PSYC 367: Quiz 3
1/137
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
138 Terms
photoreceptors
light sensitive receptors in the retina that initiate the act of seeing through producing chemical signals - two types: rods and cones
rods
a photoreceptor specialized for night vision
have more than cones (95% of photoreceptors), absent from centre of fovea
nocturnal animals have all-rod retinas
all have the same photopigment, so can’t signal differences in colour
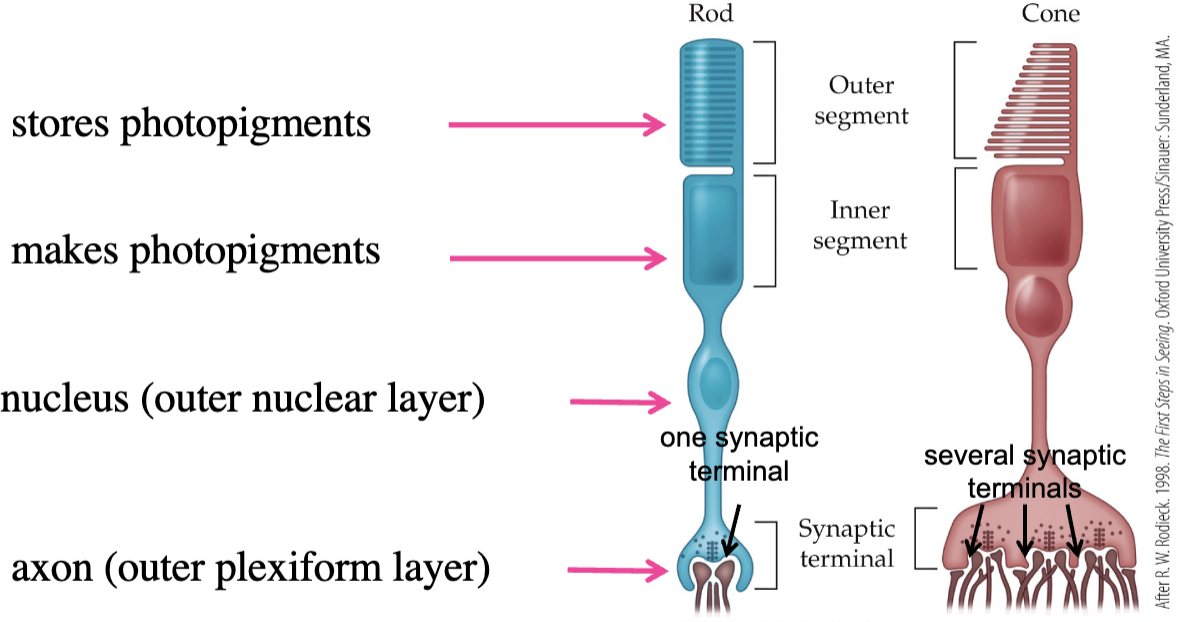
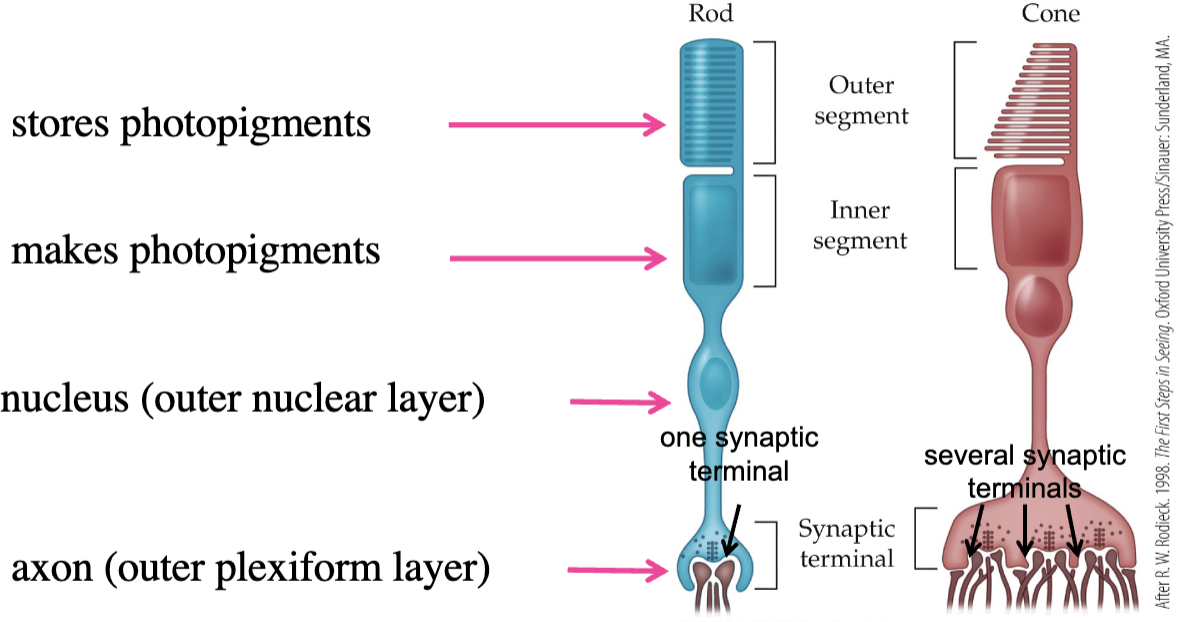
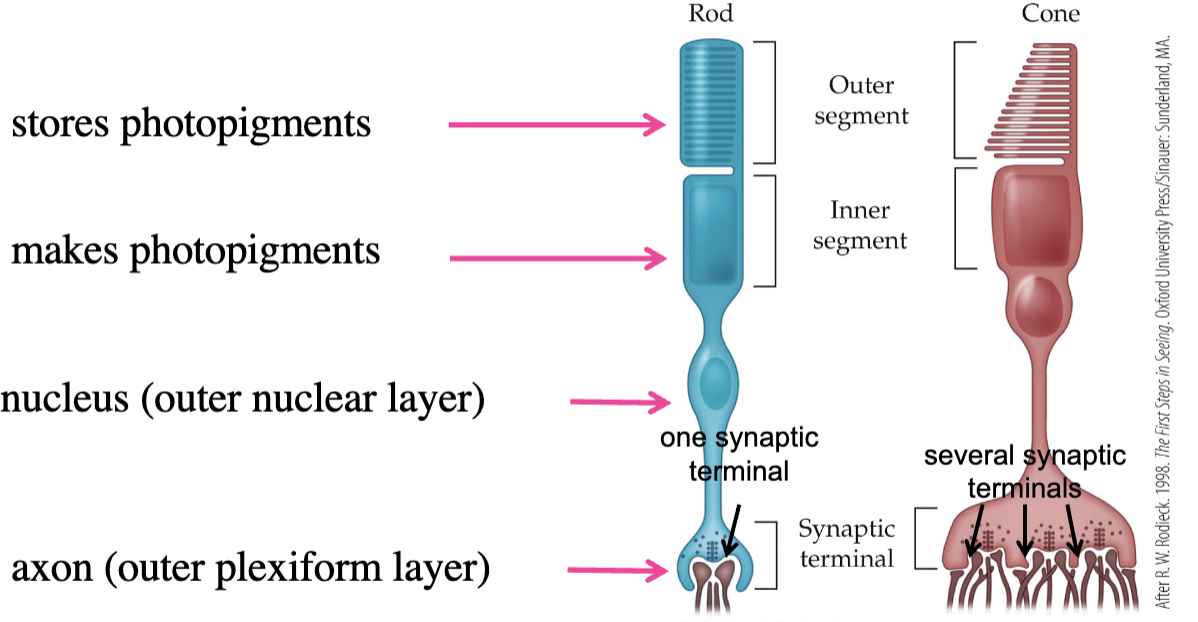
rod structure
outer segment: stores photopigments
inner segment: makes photopigments
nucleus
axon (in one synaptic terminal)
contain rhodopsin
synaptic terminals in photoreceptors
each synaptic terminal admits 2 horizontal cells and at least 1 bipolar cell
cones
photoreceptor specialized for daylight vision, fine visual acuity, and colour (central vision - trusted more than peripheral)
less of them (4-5 million)
most concentrated at centre of fovea (smaller and more tightly packed)
require brighter illumination (central vision is almost blind in dark environments)
have 3 different photopigments (opsins) that signal colour according to long, medium, or short wavelength
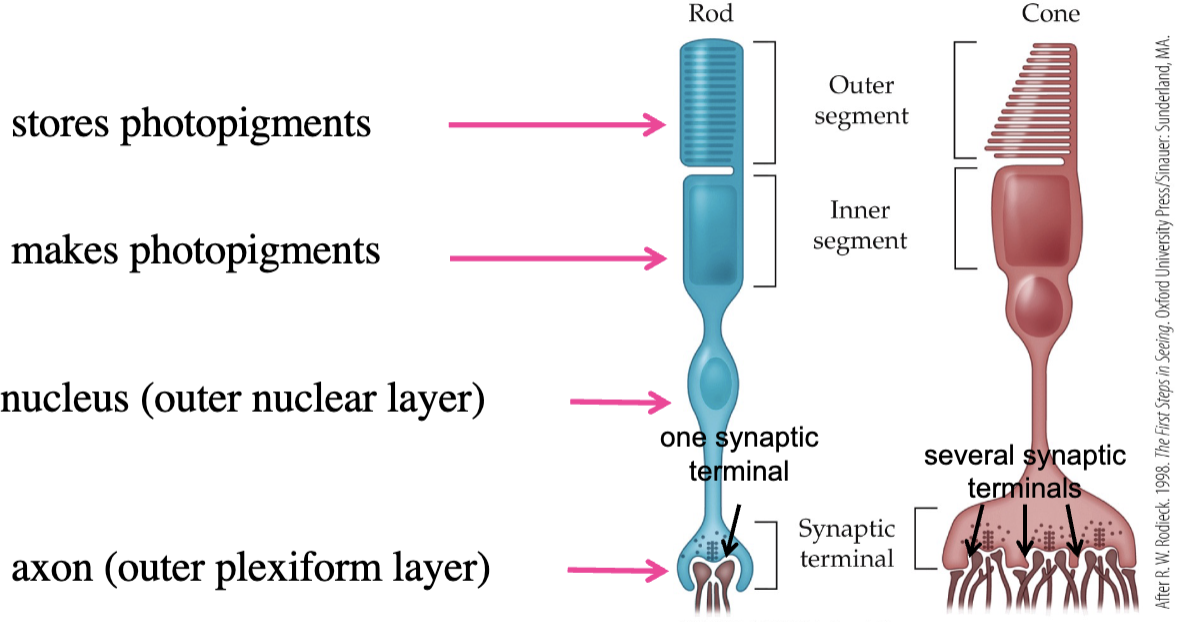
cone structure
outer segment: stores photopigments
inner segment: makes photopigments
nucleus
axon - in the several synaptic terminals
photoreceptor synaptic terminals
specialized structures for contacting other retinal neurons - horizontal and bipolar cells
photoreceptor outer segments
contain photopigment molecules
photoreceptor inner segments
makes visual pigments, each one a specific structure that absorbs a certain wavelength and also captures light photons with chromophore
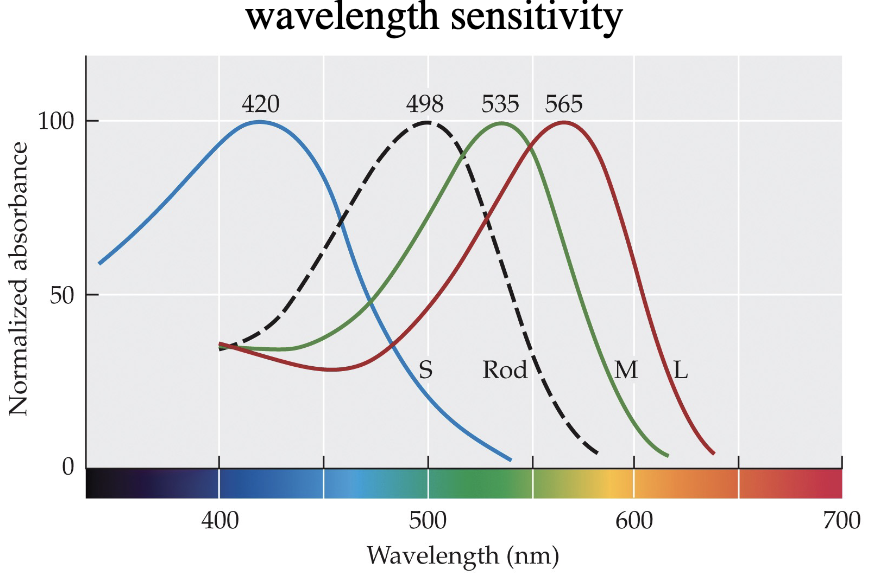
3 different cone types
short wavelength-sensitive cones (S-cones)
medium wavelength-sensitive cones (M-cones)
long wavelength-sensitive cones (L-cones)
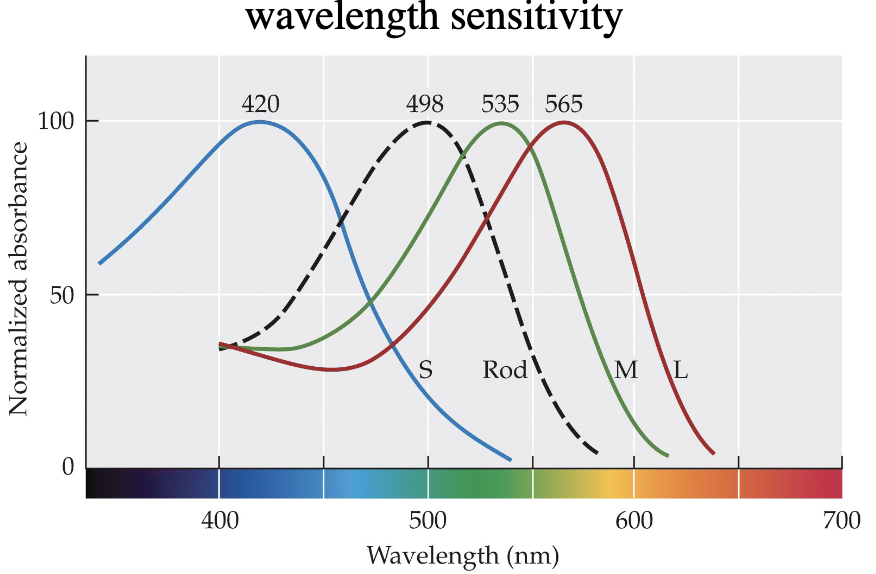
S-cones
most absorbent wavelength at 420 nm - 5-10% of of cone population
essentially missing from fovea centre
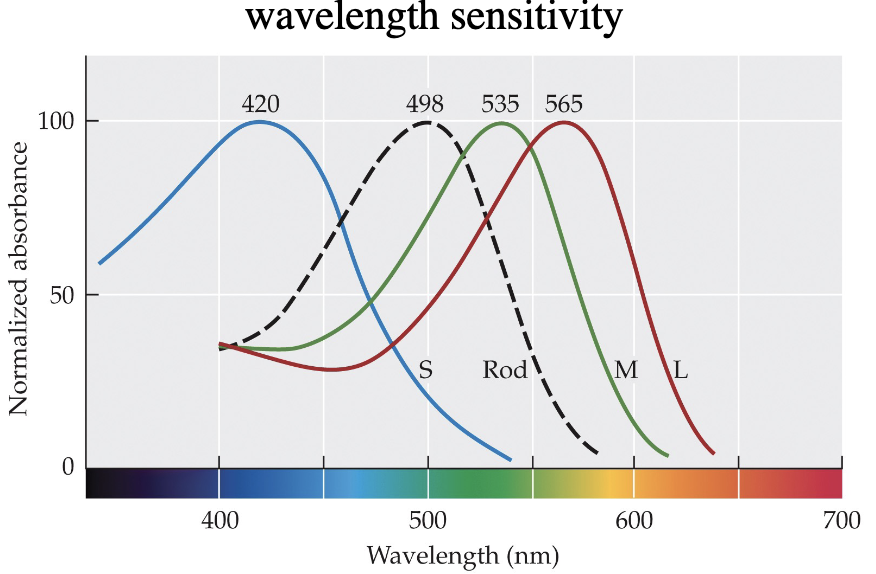
M-cones
most absorbent wavelength at 535 nm - in fovea, less than L-cones
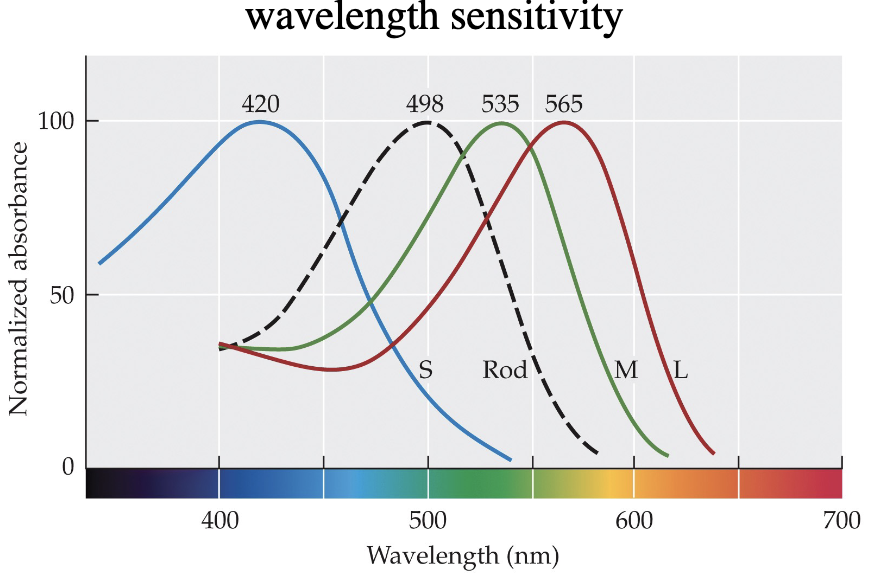
L-cones
most absorbent wavelength at 565 nms - in fovea, more than M-cones
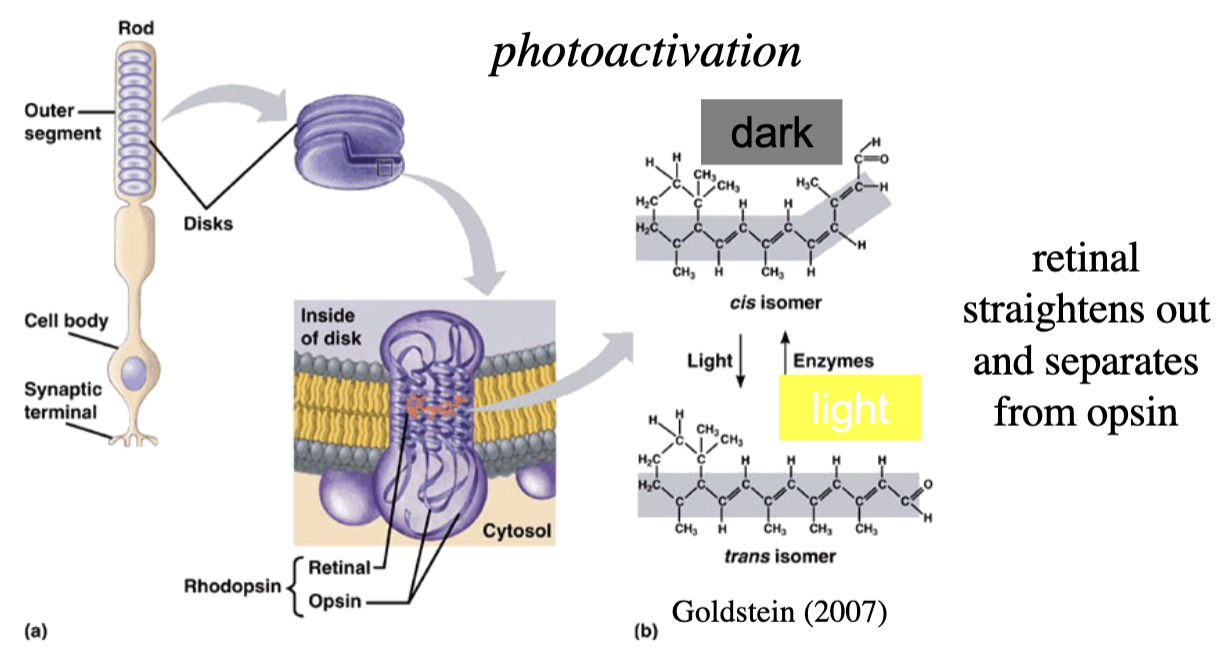
rhodopsin
visual pigment (1/4 in the retina) found in rods, mainly in membranous discs in outer segment
consist of a protein (opsin) connected to a light-sensitive chromophore (retinal)
other 3 or in cones
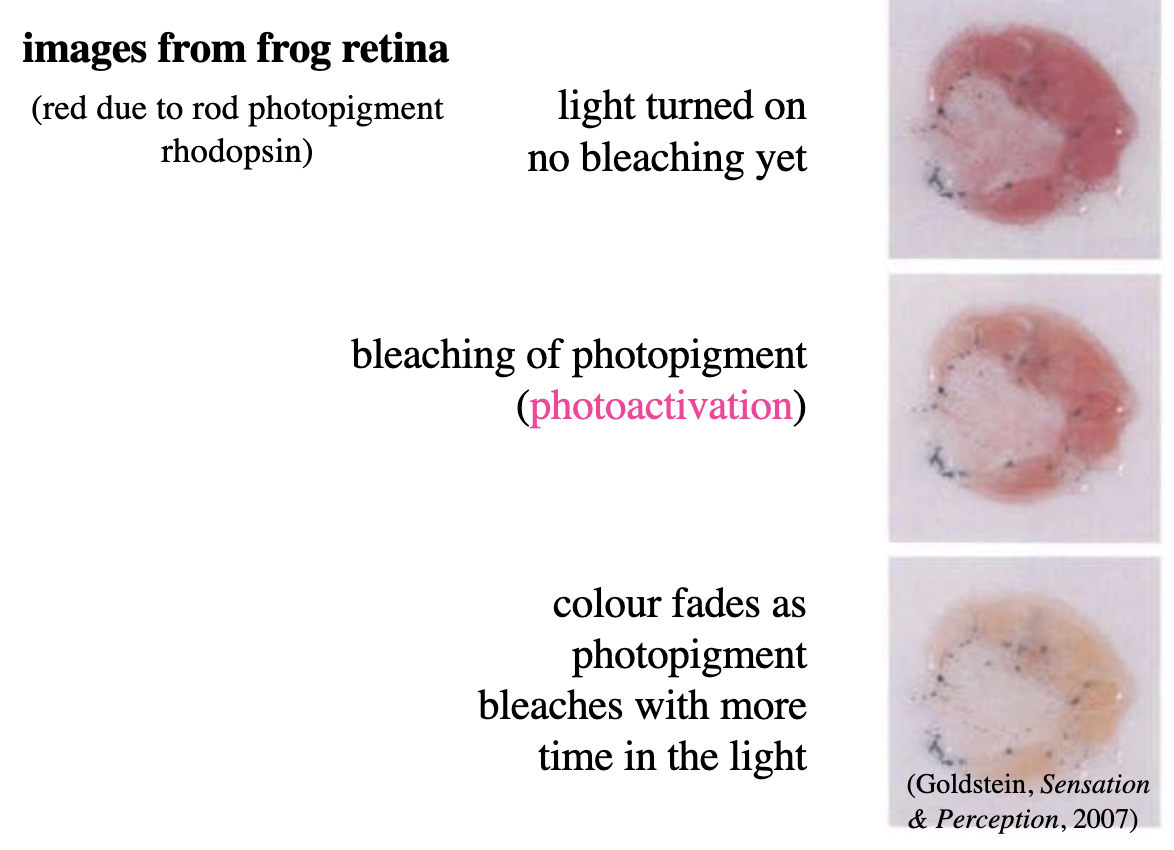
what happens when a photo meets the photoreceptors?
Photoactivation: absorbed by a molecule of rhodopsin in outer segment of rod → transfers energy to chromophore portion of visual pigment molecule
biochemical cascade of events resulting in closing of cell membrane channels that normally allow ions to flow into rod’s outer segment
opsin
determines which wavelengths photopigment absorbs
chromophore
captures light photons and protein (opsin)
photoactivation process
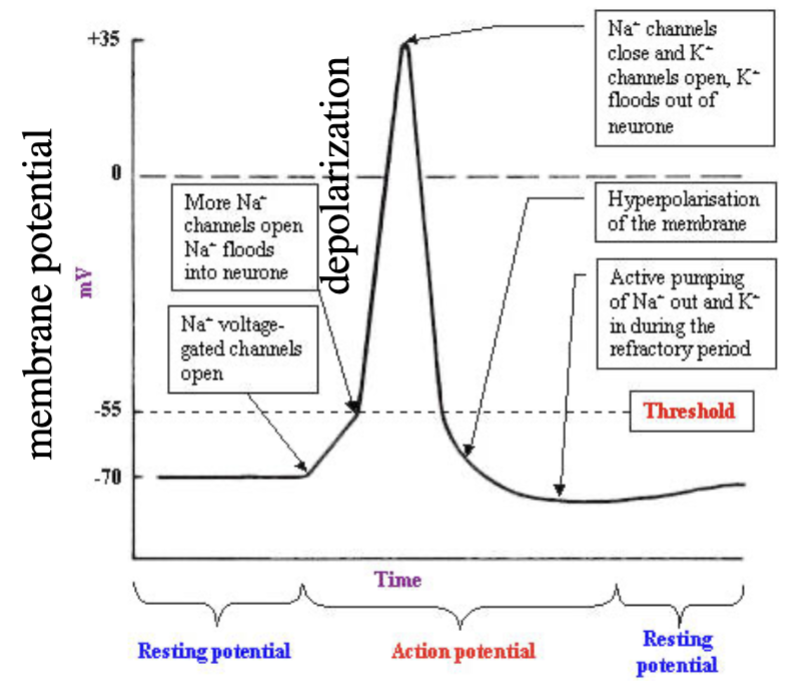
activated by light, photoreceptors become hyperpolarized, leads to transduction (process by which light is transformed into electrical activity)
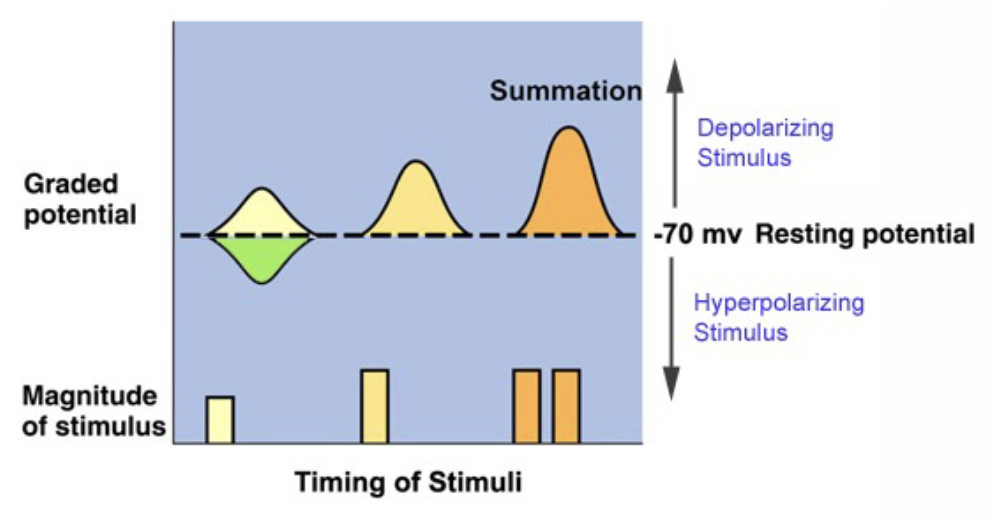
changes in photoreceptor activation communicated by bipolar cells in form of graded potentials
light transduction
hyperpolarization: imbalance of electrical current between inside and outside of rod outer segment causes closing of cell membrane channels, inside is more negatively charged
closes voltage-gated calcium channels at synaptic terminals
reduces concentration of glutamate released in synapse
signals to bipolar cells that rod has captured a photon
potentials are graded (instead of the all-or-none in nervous system)
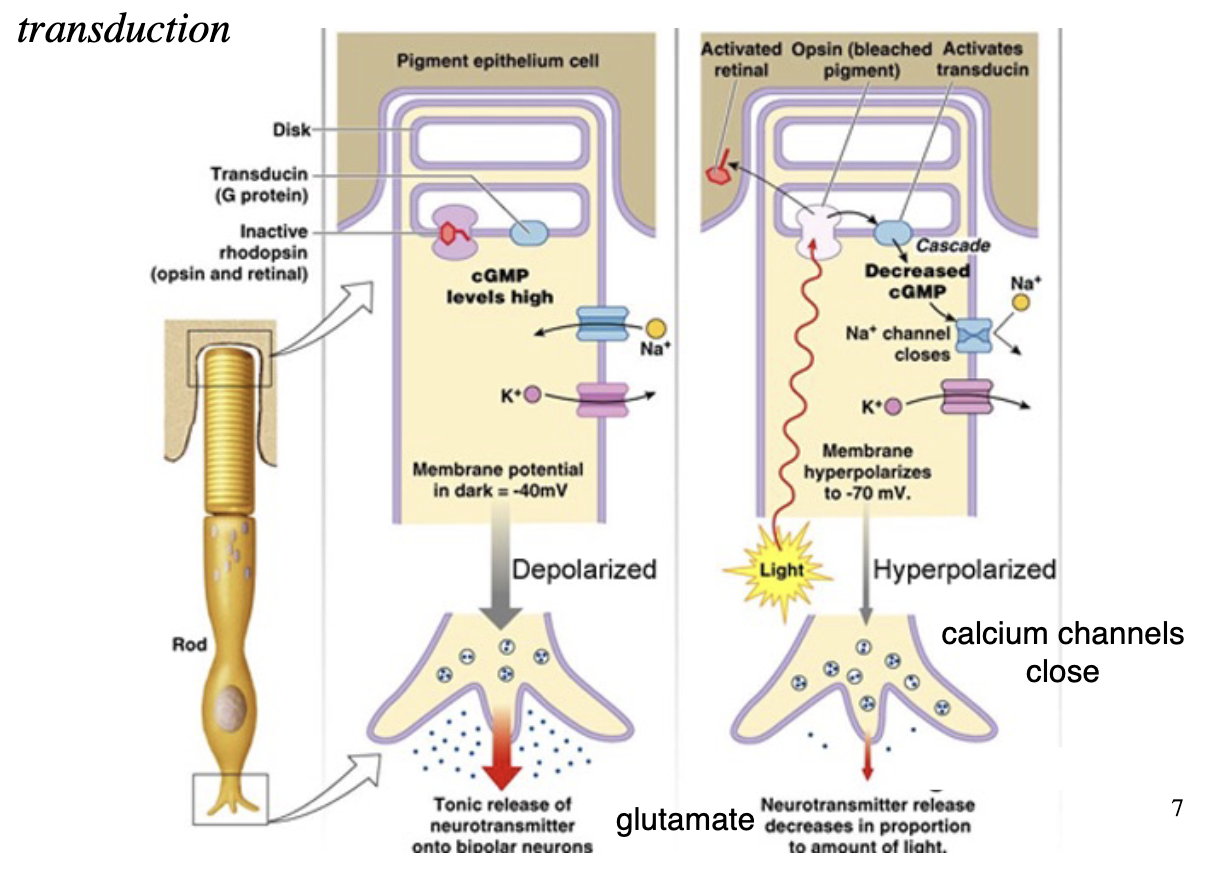
photoreceptor activity in the dark
cyclic GMP keeps sodium flowing (-40mV membrane potential)
glutamate is released into synaptic cleft and binds to bipolar cell membrane receptors
photoreceptor activity with light absorption
deactivation of cGMP closes sodium channels
photoreceptor hyperpolarizes (-70mV)
calcium channels close; glutamate concentration reduced
the more light entering the retina, the faster the photopigments are used up and the fewer photopigments there are to process more light
graded potential
slow change in membrane potential; varies in size (not all-or-nothing)
occurs in photoreceptors, bipolar cells, horizontal cells
pupil diameter
ranges from 2 (bright light) to 8 (darkness) mm
duplex vision
scotopic (rod-mediated, more sensitive in dim light) and photopic (cone-mediated, less sensitive vision in bright light)
similar to indoor and outdoor film in a camera
cones much less sensitive than rods in dim light
rod response saturates in bright light (rhodopsin bleached)
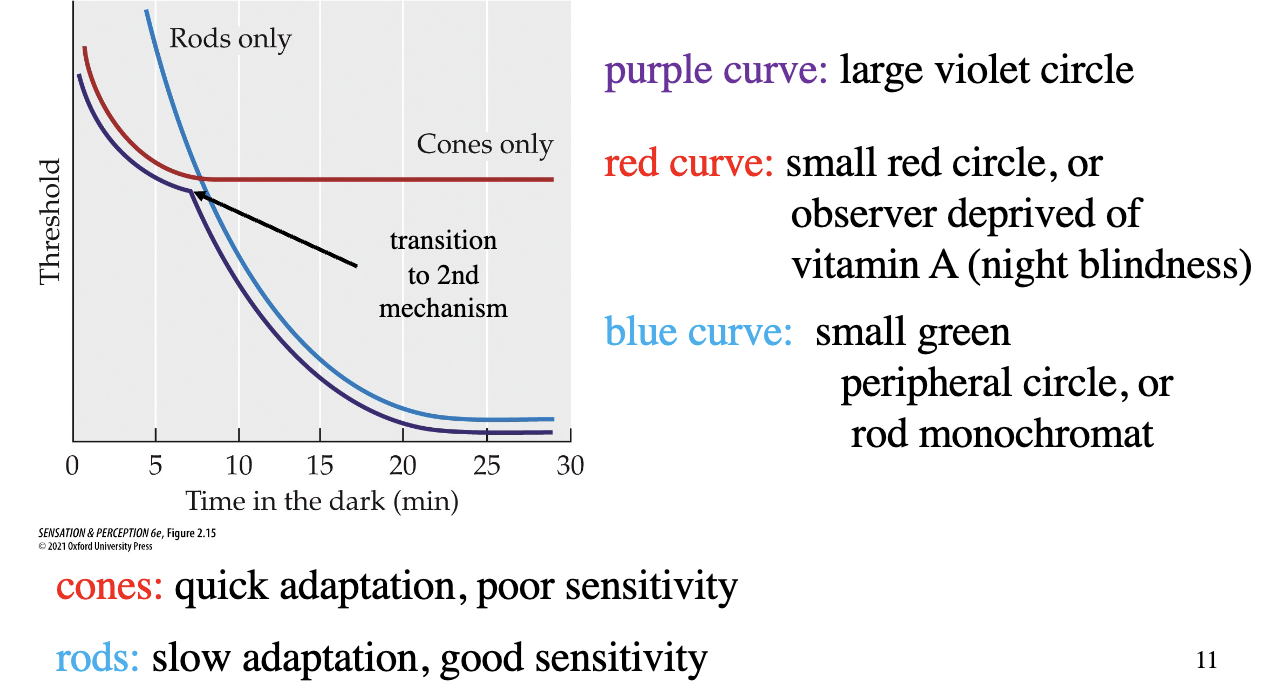
adapting to light and dark conditions (Hecht, Haig & Chase, 1937)
participant adapts to bright light → lights then turned off - frequently measure absolute threshold for circles for 30 mins (large violet circle, small red circle, small green peripheral circle)
cones: quick adaptation (then saturation), poor sensitivity
rods: slow adaptation, good sensitivity
purple curve = change in threshold intensity to detect a spot (represents the more sensitive of the rods or cones at a given time)
ways the visual system adapts to changes in illumination
pupil size
photopigment regeneration
duplex retina
neural circuitry (ganglion cells measuring difference in light intensity between central and peripheral vision
horizontal cells
run perpendicular to photoreceptors and make contact with nearby photoreceptors and bipolar cells
enable lateral inhibition (signals that reach retinal ganglion cells are based on differences in activation and creates their centre - surround receptive field)
amacrine cells
run perpendicular to photoreceptors in retina
synapse horizontally between bipolar and retinal ganglion cells
implicated in contrast enhancement and temporal sensitivity (detecting light patterns that change over time)
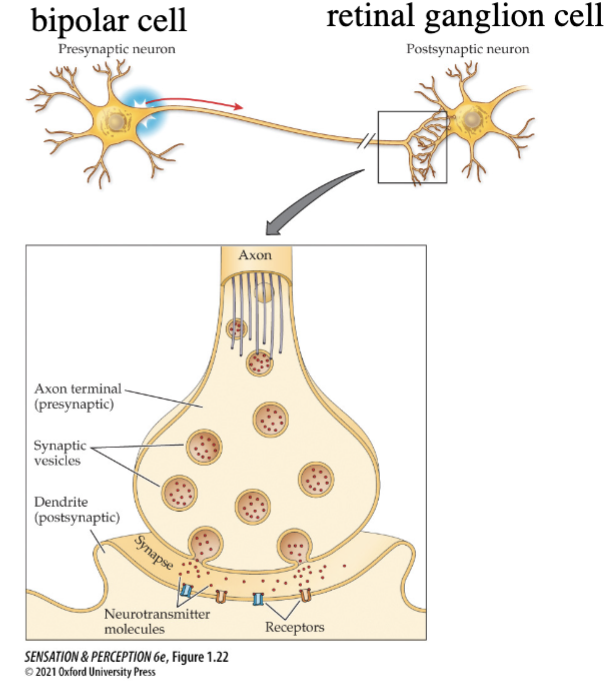
bipolar cells
intermediaries between photoreceptors and ganglion cells
synapses with 1+ rods or 1+ cones and with horizontal cells → then with ganglion cells
depolarize with increase in photon catch by photoreceptors due to opening of positive ion channels
increase rate of neurotransmitter release
diffuse bipolar cells
synapses with multiple photoreceptors (up to 50) (convergence)
ON midget bipolar cells
depolarizes to an increase in photon catch by photoreceptors in central retina
increase rate of neurotransmitter release
connect to cones in fovea
receive input from 1 cone per bipolar cell → pass to single ganglion cells (why images in this part of retina are the clearest)
OFF midget bipolar cells
hyperpolarizes in response to an increase in light captured by cones
connect to cones in fovea
1 cone per bipolar cell → pass to single ganglion cells
neural transmission between a bipolar cell and a retinal ganglion cell
Bipolar cell depolarizes
Glutamate released into synaptic cleft
Ion channels open
Retinal ganglion cell depolarized
depolarization happens with more light in ON cells and less light in OFF cells
action potential
rapid depolarization - occurs in amacrine cells and retinal ganglion cells
cells when lights are on
ON bipolars (midget or diffuse): depolarize/increase nt release, ON-centre retinal ganglion cells fire more action potentials
OFF bipolars (midget): hyperpolarize/decrease nt release, OFF-centre retinal ganglion cells fire fewer action potentials
cells when lights are off (luminance)
ON bipolars: hyperpolarize/decrease nt release, ON-centre retinal ganglion cells fire fewer action potentials
OFF bipolars: depolarize/increase nt release, OFF-centre retinal ganglion cells fire more action potentials
mighet retinal ganglion cells/P ganglion cells
project to parvocellular LGN layers
small cell bodies, short dendrites, thin axons
70% of ganglion cells in retina
synapse with midget bipolar cells
high visual acuity, colour, shape processing, poor temporal resolution, but good spatial resolution
work best in high luminance
contrast info
parasol/M retinal ganglion cells
project to magnocellular layers of LGN
larger cell bodies, long dendrites, thick axons
10% of ganglion cells in retina
synapse with diffuse bipolar cells
motion processing (how an image changes), excellent temporal resolution but poor spatial resolution
work best in low luminance, low acuity

bistratified/K retinal ganglion cells
project to koniocellular layers of LGN
small or large cell bodies and dendritic fields, intermediate axons
10% of ganglion cells in retina
synapse with diffuse or midget bipolar cells
intrinsically photosensitive/melanopsin-containing retinal ganglion cells (4th type of retinal ganglion cells)
involved in pupil reflexes, circadian rhythms - stimulated by blue light = reduced melatonin production in evening which reduces sleepiness (brightness discrimination/contrast detection)
<5% of retinal ganglion cells
photopigment melanopsin on dendrites
peak absorption at 480 nm
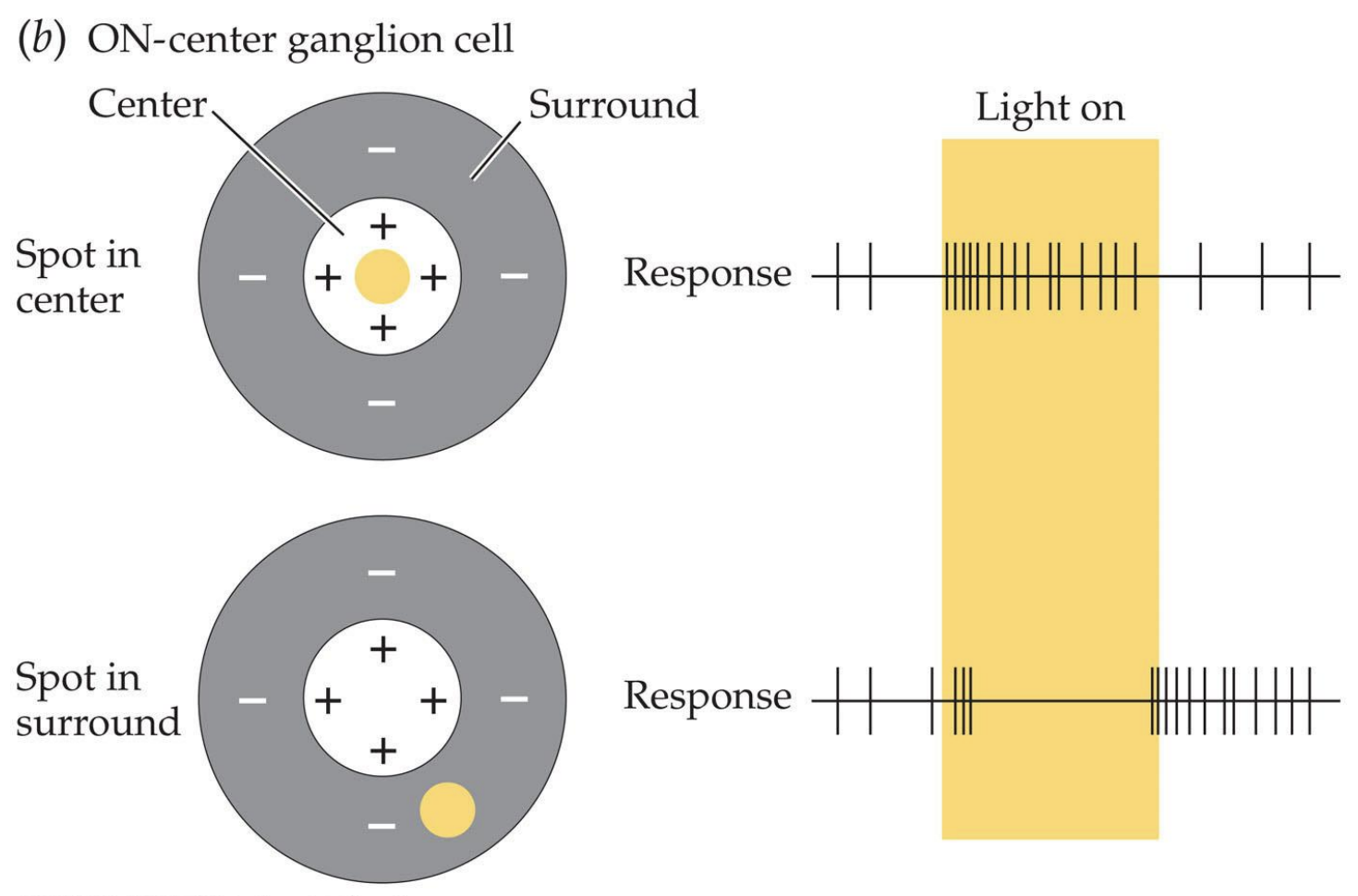
receptive field
region on retina and corresponding region in visual space in which visual stimuli influence neuron’s firing rate - neuron firing rate increases when light shines on the specific spot
ganglion cell rf size determined by number of photoreceptors connected to that neuron (through bipolar cell)
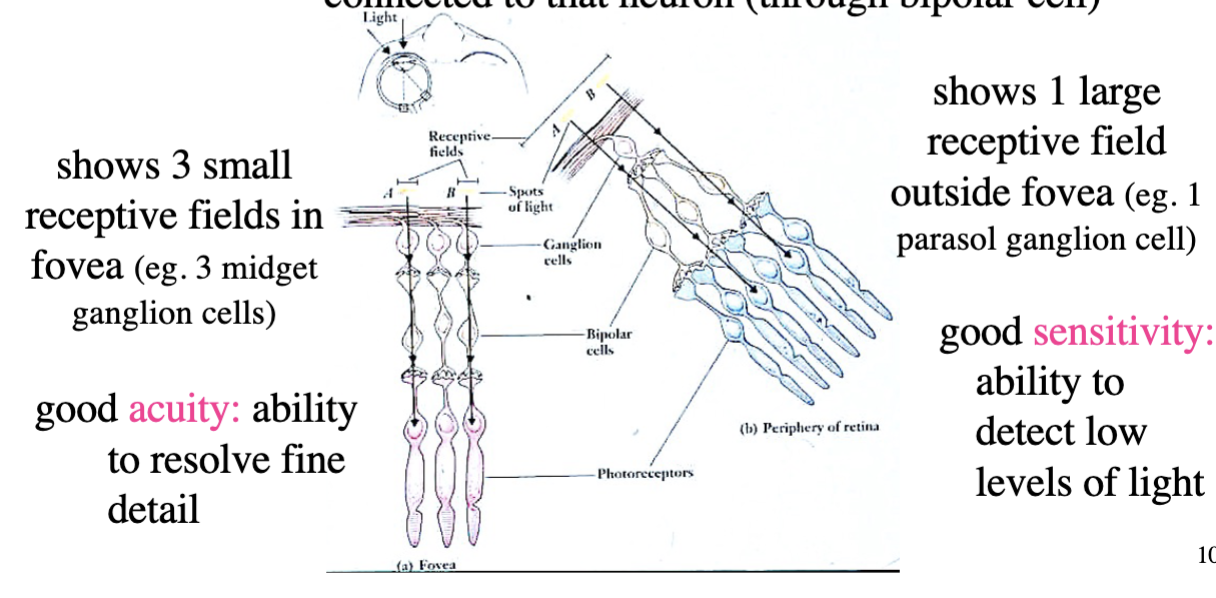
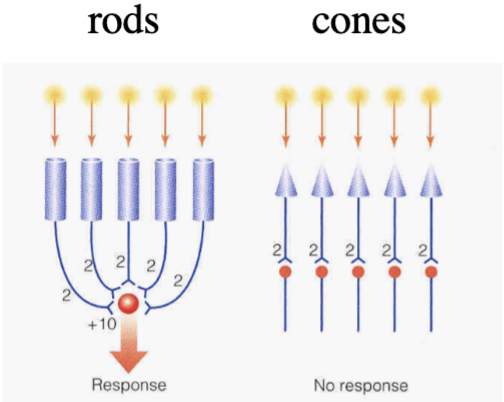
receptive field convergence
convergence of rods onto ganglion cells yields high sensitivity
lack of convergence in cones yields high acuity
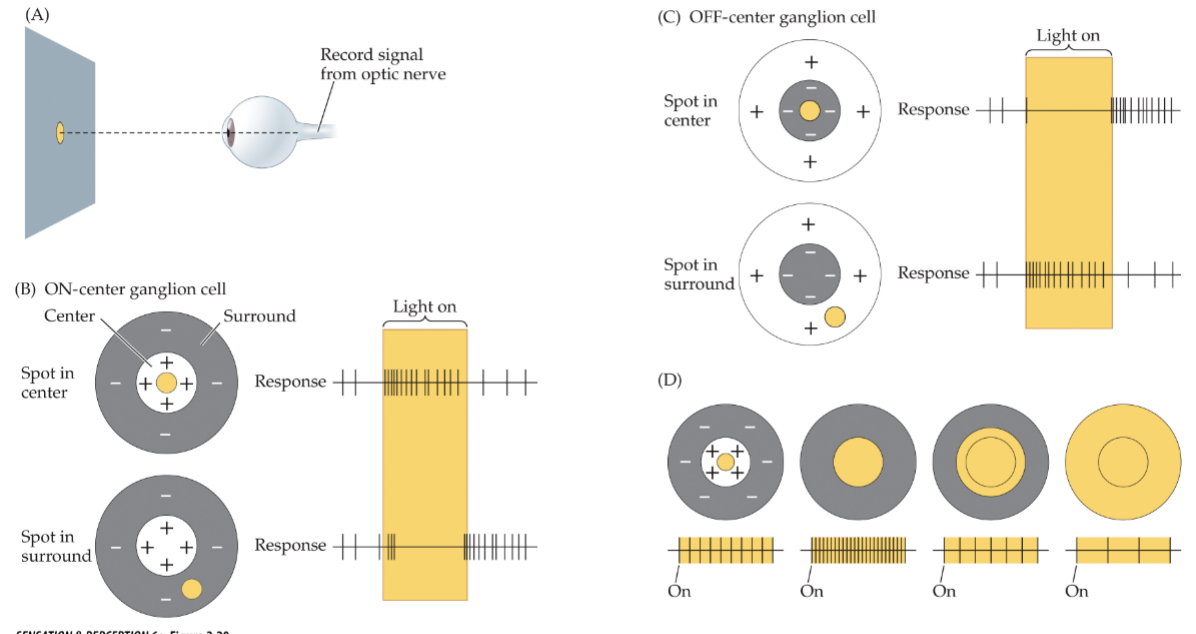
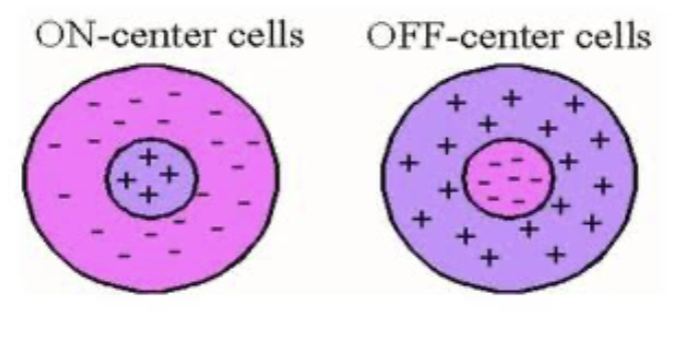
ON-centre ganglion cell
a cell that increases firing in response to an increase in light intensity in its receptive-field centre - neuron fires more when light is shone directly in the centre, fires less when light is shone in peripheral (spatial opponency)
+ regions = light increases action potentials (excitation)
- regions = light decreases action potentials (inhibition)
centre size determined by photoreceptor connections through bipolar cells
surround size determined by photoreceptor connections through horizontal cells
OFF-centre ganglion cell
a cell that increases firing in response to a decrease in light intensity in its receptive-field centre - neuron fires more when light hits peripheral of cell, less when it hits the centre
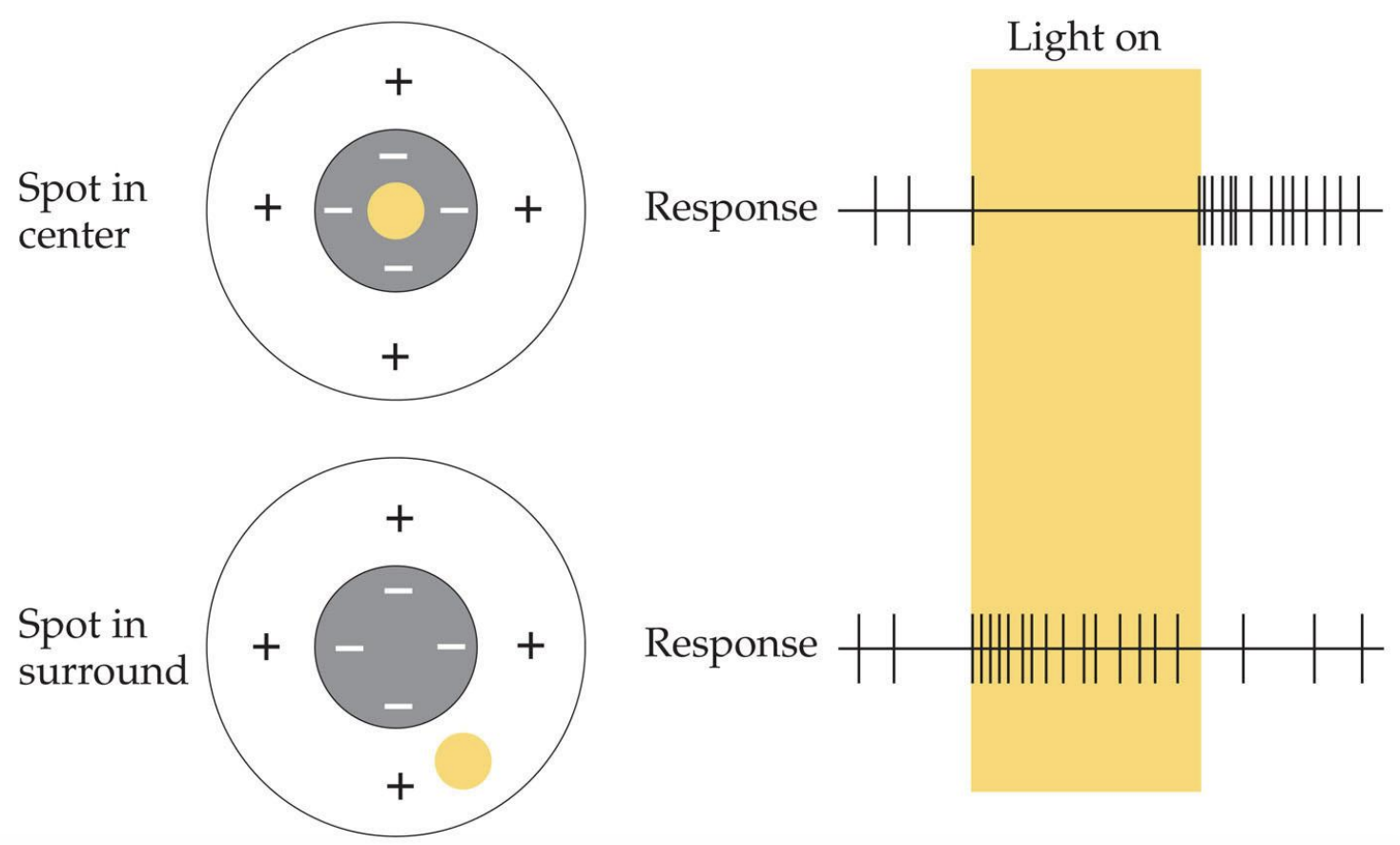
size of light and neuron firing
cell fires fastest when size of light matches size of excitatory centre, reduces rate when spot of light begins to encroach on its inhibitory surround
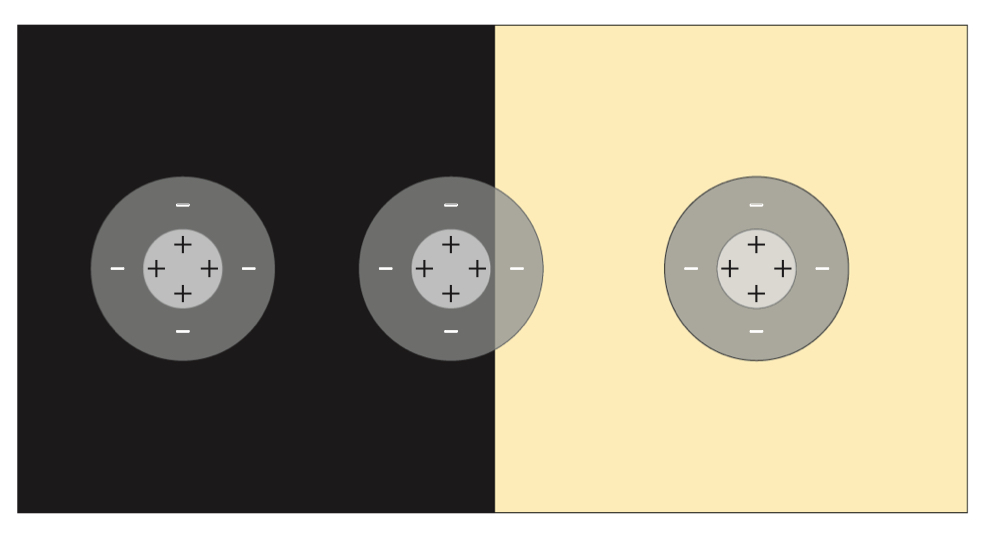
lateral inhibition
cells are more sensitive to differences in intensity of light in centre and in surround, less affected by average intensity of light
luminance variations
tend to be smooth within objects and sharp between objects - helps to emphasize object bpundaries
receptive fields in M, P, and K-ganglion cells
M-cells have smaller receptive fields than P and K-cells
M and P-cells have spatial opponency
K-cells have centres only (ON and OFF responses)
M-cells are the most senitive
retinal ganglion cells temporal responses
M-cells = sustained response: lasts entire time light is on or off in ganglion cell receptive field
P-cells = transient response: brief response at onset and/or offset of light in ganglion cell receptive field
K-cells = sustained OR transient response at onset and offset of light in receptive field
Describe 3 new technological developments that may lead to
treatments for age-related macular degeneration or retinitis
pigmentosa.
prosthetic retina - may replace damaged photoreceptors
Gene therapy - improve functioning in surviving photoreceptors
Chemical therapies - convert retinal ganglion cells into photoreceptors
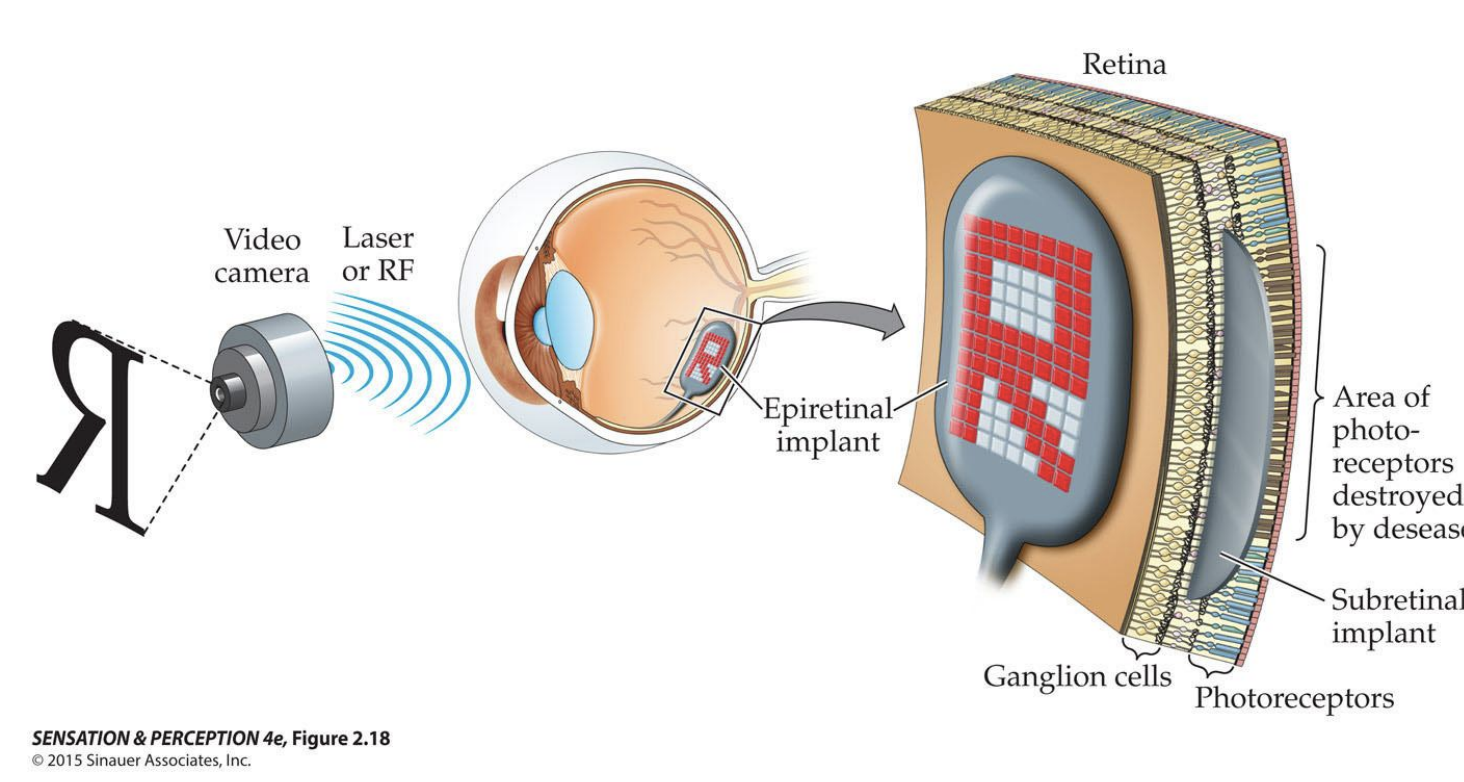
age-related macular degeneration
disease associated with aging that affects the macula - gradually destroys sharp central vision, making it difficult to read, drive, and recognize faces
retinitis pigmentosa
progressive degeneration of the retina that affects night vision and peripheral vision - commonly runs in families and can be caused by defects in a number of different genes
Discuss how lateral inhibition allows retinal ganglion cells to highlight contrast and discount ambient light intensity.
enhances contrast by shaping ganglion cell receptive field to emphasize differences in light intensity between adjacent areas of the retina - make’s ganglion cell’s response to a boundary between light and dark stronger
responds primarily to relative changes in light intensity rather than absolute levels - allows visual system to focus on changes or patterns in visual scene, rather than overall brightness
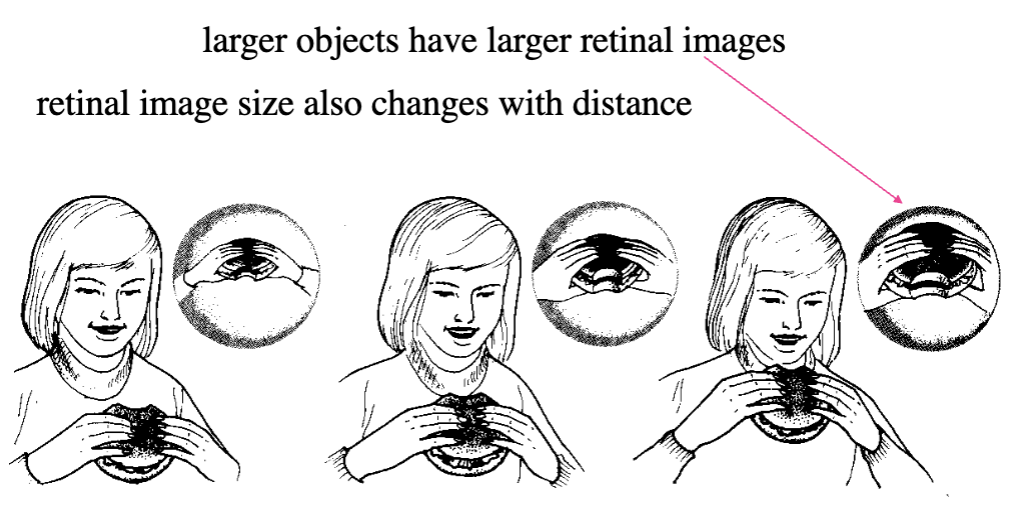
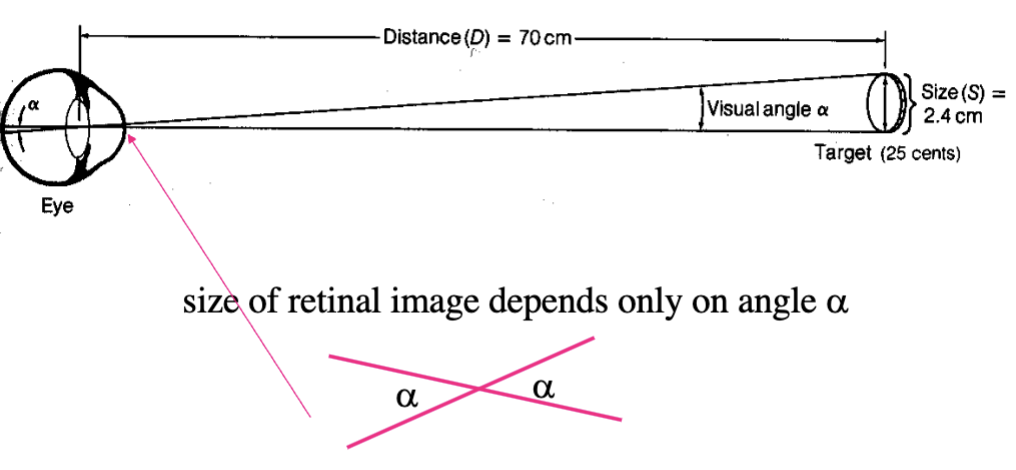
visual angle
measure of retinal image size that depends on physical size of object and object’s distance from eye (retinal image size also changes with distance)
formed by lines going from ex. top and bottom of a stripe cycle, passing through the centre of the lens and ending on the retina
measuring visual angle
divide the size of cycle by viewing distance at which you ca barely see a difference between two objects → take arctangent of this ratio
cycle
for grating, a pair consisting on one dark bar and one bright bar
size of visual angle
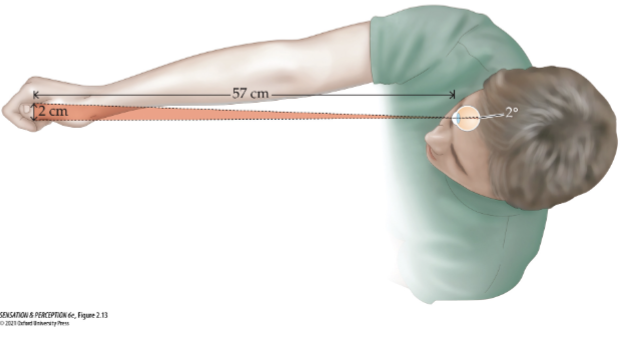
measured in degrees of arc - 60 minutes of arc in 1 degree
1 degree is ~0.3 mm on retina
Rule of thumb: 1 cm object at 57 cm away subtends 1 degree (index finger at arm’s length)
visual acuity
ability of visual system to resolve fine spatial detail - smallest resolvable visual angle
depends on separation distance of photoreceptors from each other/convergence of receptors on each ganglion cell
worse in peripheral vision because more cones converge on each other
central vision is slower at responding to light - foveal cones have longer axons = denser packing
minimum visible acuity
smallest objects one can detect - ex. can see a dark wire against a bright background when they subtend an angle of 0.5 arc second (0.00014)
why is minimum visible acuity so small?
optics of the eye spread the image of the line, making it wider on the retina
fuzzy retinal image of the line casts a shadow that reduces the light on a row of cones to levels that is just detectably less than rows of cones on either side
Snellen ration (20/20) - visual acuity
numerator is viewing distance of 6m (20 ft) - optical infinity (lens relaxed in emmetropic eye)
denominator calculated for each person based on size of smallest letter they can correctly identify (distance at which a person with normal vision can identify letters_
normal = read line of bard of letters that subtend 1 min of arc from 6m viewing distance (6/6)
6/3 = better than normal (can read at 6 meters what normally read at 3)
6/12 = worse than normal (can read at 6 meters what normally read at 12)
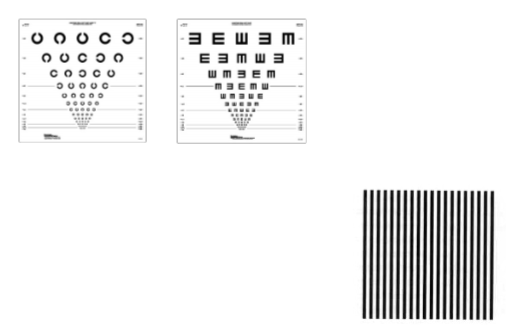
testing visual acuity on people not familiar with English language
Landolt Cs: where is the gap in the C
Tumbling Es: what direction are the E prongs facing
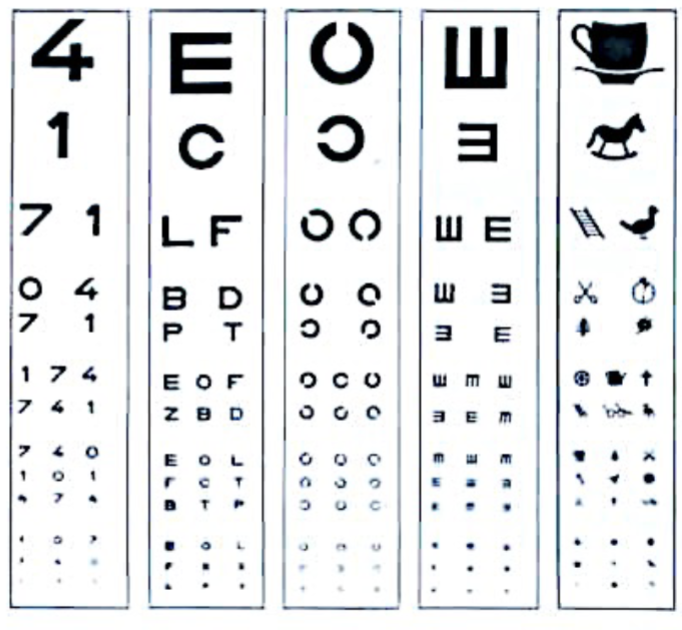
recognition acuity
requires identification - letters, numbers, shapes
angular size of smallest feature that one can recognize or identify
normal if you can identify letters with a 1 min of arc stroke width (0.017 degree)
many people can see smaller letters
depends on photoreceptor properties + higher cortical factors

resolution acuity
does not require identification, finest high-contrast detail that can be resolved - Landolt Cs, tumbling Es, grating acuity (stripe width)
often better than recognition
depends on photoreceptor properties (density and convergence)
ex. can resolve black and white stripes when one cycle subtends angle of approximately 1 min of arc
visual acuity is best when
mediated by the cones in the fovea
foveal viewing: 0.5 mins of arc between cone centres vs. 0.75+ mins of arc between rod centres outside fovea - no convergence of photoreceptors onto retinal ganglion cells and fit nicely into acuity limit of 1 minute of arc (2 cones per cucle)
photopic light conditions
vertical meridian asymmetry
we have better acuity a fixed distance below the midline of the visual field than above - acuity falls off more rapidly along vertical midline (horizontal and vertical asymmetry
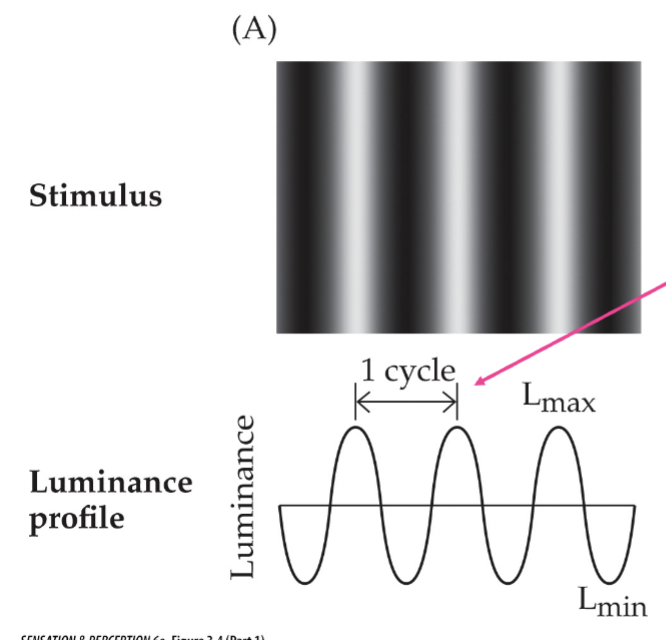
contrast sensitivity is measured by
sinewave grating - used to assess spatial vision over a range from very coarse to very fine detail, sinusoidal change in intensity across pattern
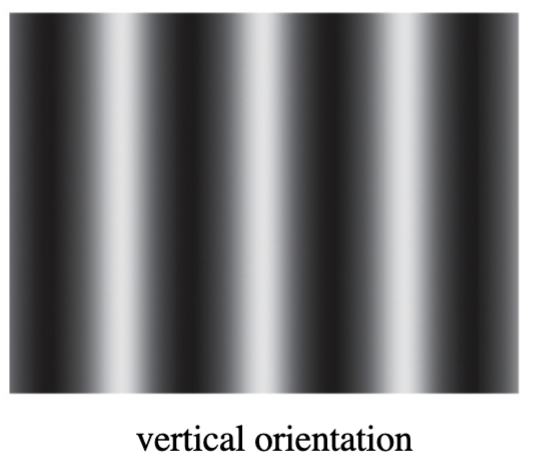
sinewave grating varies in
spatial frequency: # of cycles in 1 degree of visual angle
contrast: luminance difference between light (Lmax) and dark (Lmin) bars
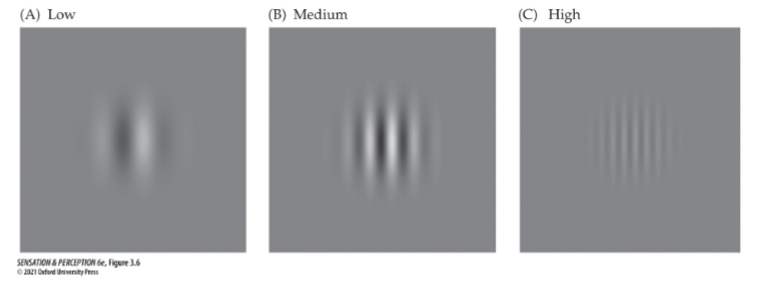
different spatial frequencies
low, medium, high
phase
position of grating relative to some fixed position (measured in degrees)
which parameters differ in the 2 left gratings and in the 2 right gratings?
2 left: contrast and phase
2 right: orientation and spatial frequency
contrast detection threshold for sinwave gratings is a function of
spatial frequency - most sensitive to intermediate spatial frequencies (~6 cycles/degree
steep falloff due to neural factors
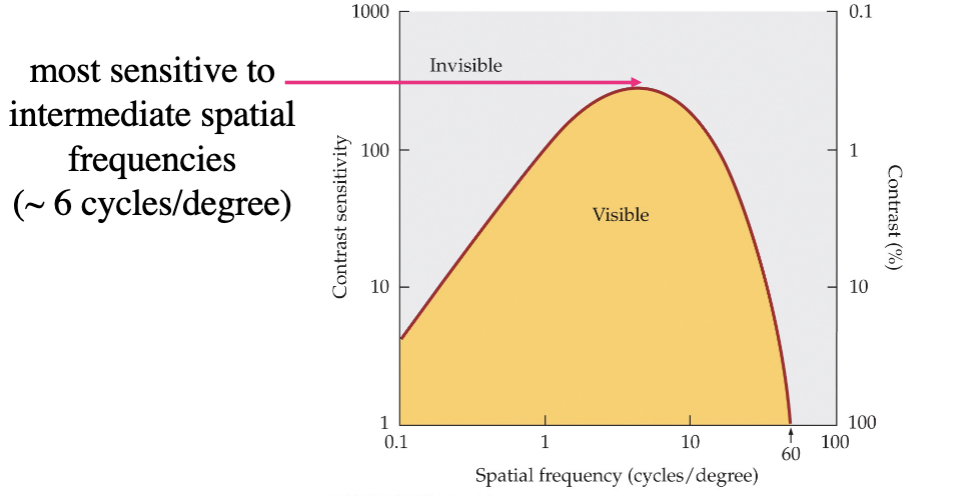
as contrast goes down and spatial frequency goes up
sensitivity gets higher
contrast sensitivity
reciprocal of (Lmax - Lmin)/(Lmax + Lmin) → divide that answer by 1
contrast of 100% = sensitivity of 1
why does our sensitivity drop off as frequency reaches 60 cycles/degree?
high spatial frequencies transmitted poorly due to
optics: eye can’t transmit higher spatial frequencies
anatomy: spacing of cones
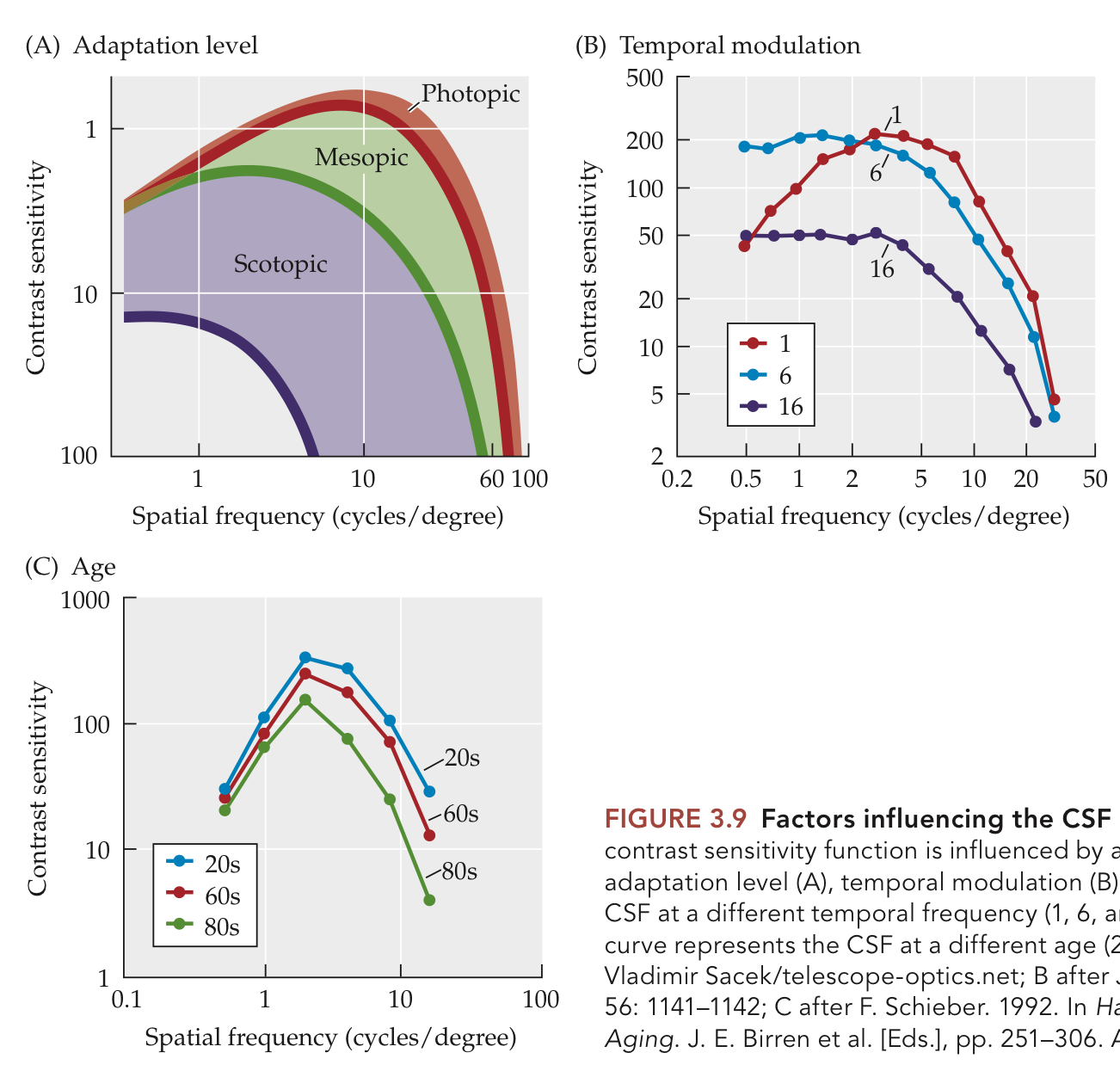
factors that influence exact form of CSF
adaptation level of eye
Temporality modulation of targets (how it varies over time)
age and refractive state of individual
when do retinal ganglion cells give the best response?
when width of receptive field centre matches the specific width of the grating bars and the phase fills the receptive field perfectly
different neurons respond to different spatial frequencies; fewer tuned to low
respond weakly when spatial frequency is too low or too high
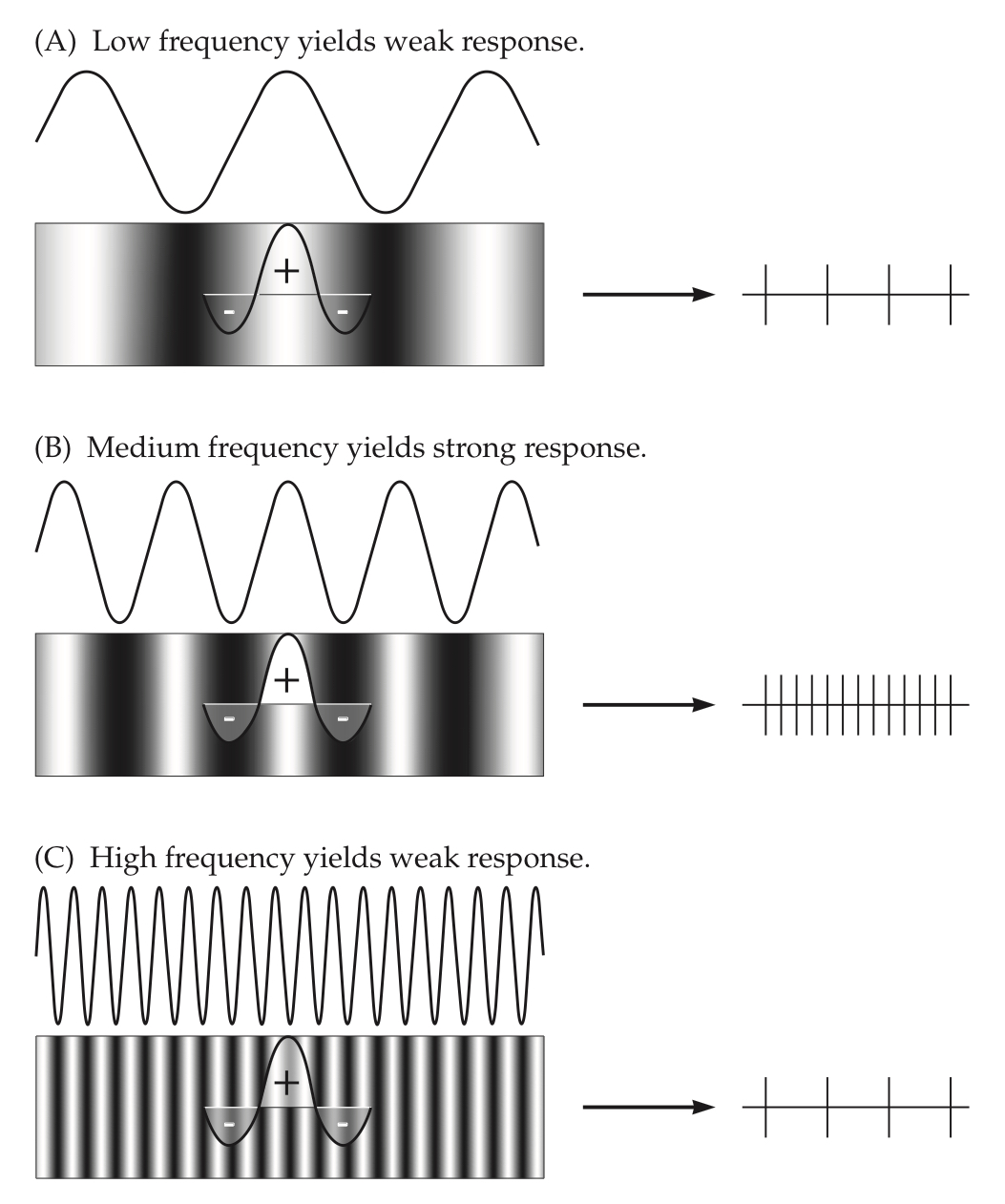
why do respond to sine wave gratings the most?
although pure sine waves are rare, all objects have some edge that may or may not be fuzzy - visual system breaks down images into components that essentially are sine wave gratings (same as the Fourier analysis in the auditory system)
track how often changes from light to dark occur over a region of space (spatial frequencies)
spatial frequency
number of light/dark changes across 1 degree of a person’s visual field
why is contrast sensitivity low at low spatial frequencies?
physiology: fewer neurons turned to low
experimental design: harder to see grating since it only contains a few bars
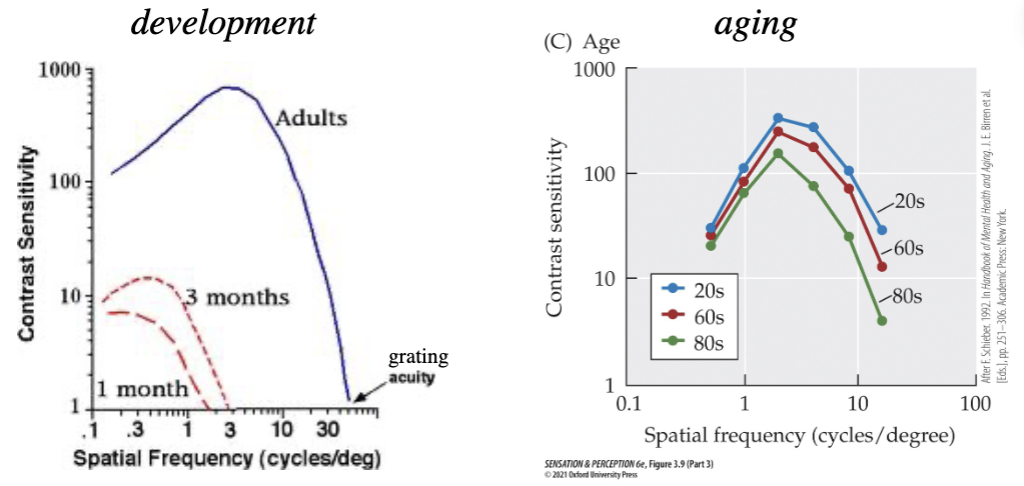
contrast sensitivity and age
during development: contrast sensitivity improves at all spatial frequencies, peak shifts to the right with age (mainly due to longer, thinner, denser cones
old age: contrast sensitivity and grating acuity decreases at high spatial frequencies, no peak shift (probably due to changes in optical properties of eye)
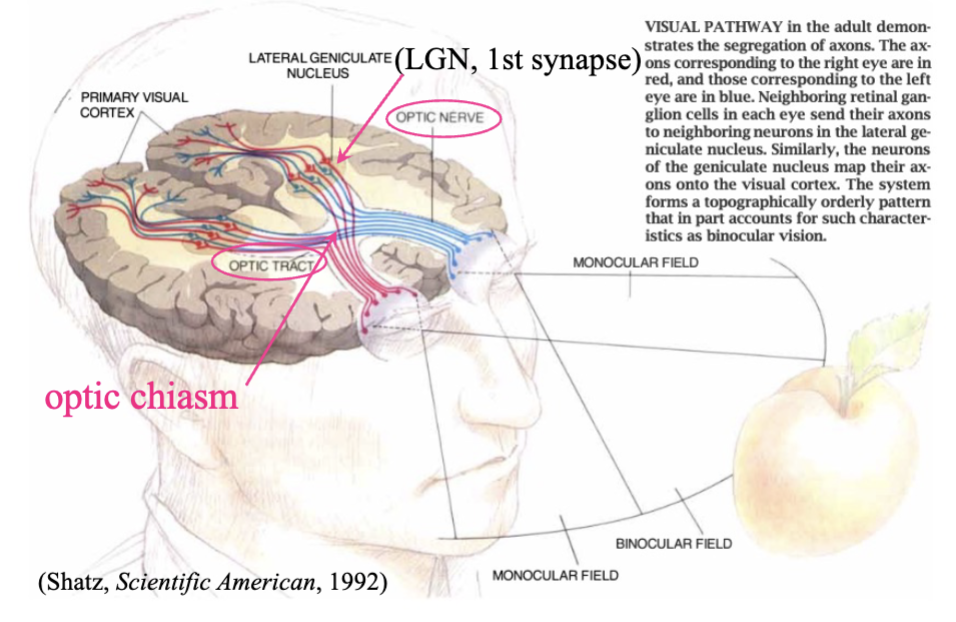
geniculostriate pathway
axons from nasal half of each eye cross over to opposite side of brain, axons from temporal half of each eye stat on same side
optic chiasm: where nerves from each eye meet
optic tract: where nerves from both eyes travel to the LGN
lateral geniculate nucleus: 1st synapse, carried by optic radiations
primary visual cortex/V1/striate cortex/area 17
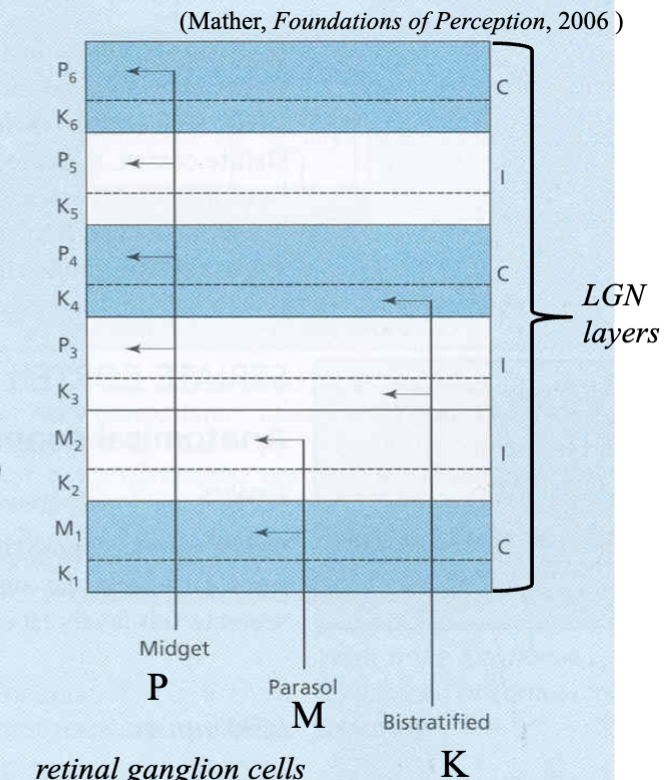
lateral geniculate nucleus (LGN) strucutre
2 magnocellular layers at bottom and 4 parvocellular layers at top - koniocellular layers in spaces between magno and parvo layers
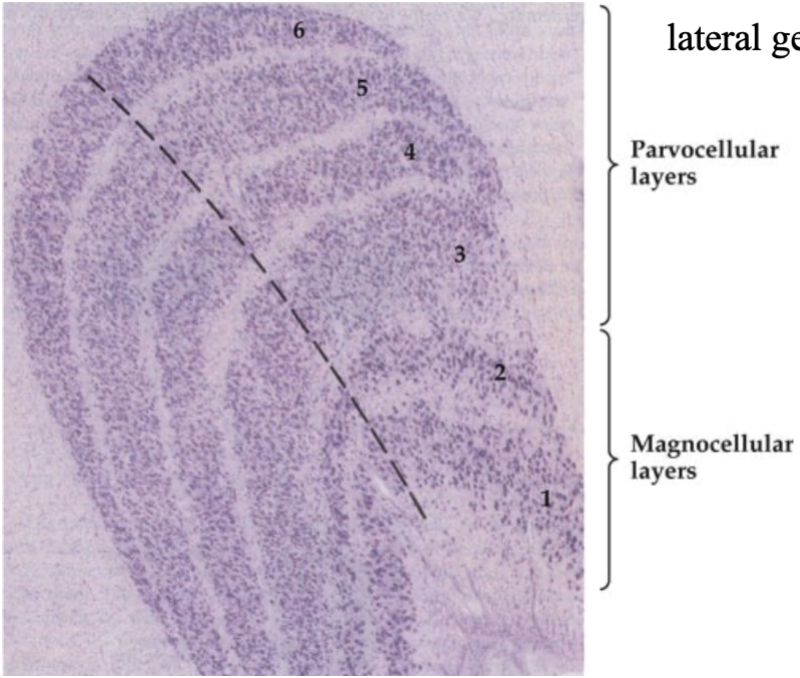
koniocellular layers
each involved in a different aspect of processing - like relaying signals from S-cones
magnocellular layers (LGN)
receive input from M ganglion/parasol cells in retina
respond to large, fast, moving objects
parvocellular layers
receive input from P ganglion/midget cells in retina
process stationary targets
lateral geniculate nucleus
structure in the thalamus that receives input from retinal ganglion cells and has input and output connections to the visual cortex - one in each cerebral hemisphere
visual input to LGN
each LGN keeps left and right eye inputs separate - left side of retina in each eye go to left LGN and right side of retina in each eye go to right LGN, but only right visual field goes to left LGN and only left visual field goes to right LGN
gets input from both eyes, it is the actual visual field that is separated again
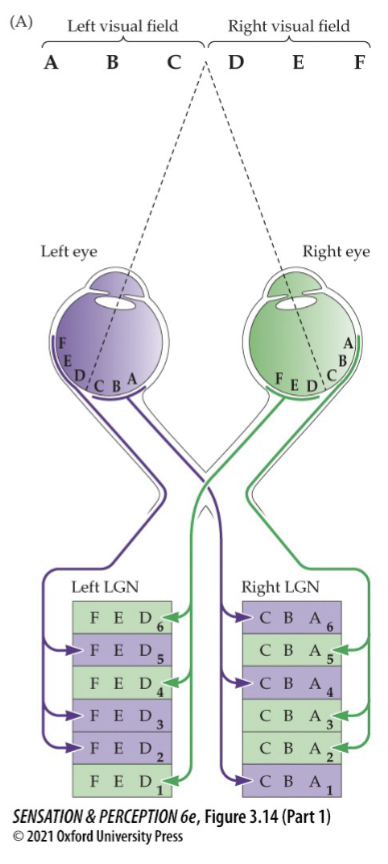
LGN layers
layers 2, 3, 5 are from ipsilateral eye (same side of body)
layers 1, 4, 6 are from contralateral eye (opposite side of body)
adjacent neurons in LGN are stimulated by adjacent points on retina or in visual field - each layer contains a highly organized map of a complete half of the visual field (topographic map)
cells synapsing in layers of the LGN
midget cells project to parvocellular (P) layers (P3, P4, P5, P6)
parasol cells project to magnocellular (M) layers (M1, M2)
bistratified cells project to koniocellular (K) layers (K3, K4 - axons from superior colliculus synapse in K1 and K2)
LGN cell receptive fields
region of visual field or part of retina on which light produces a response
primary visual cortex (V1)/area 17/striate cortex
receiving area for LGN inputs in cerebral cortex
V1 layers
6 layers: layer 1 is closest to the outer surface of the brain, layer 6 is the deepest layer
layer 4 has 3 sublayers - 4A, 4B, 4C (4C further subdivided in alpha and beta layers)
fibres from the LGN project mainly to layer 4C - magnocellular axons mostly go to 4C alpha and parvocellular axons mostly project to 4C beta
where do LGN neurons mostly project?
layer 4C in V1
magno LGN projects to V1 layer 4C alpha, further projects to V1 layer 4B and V1 layer 2/3
parvo LGN projects to V1 layer 4C beta, further projects to V1 layer 2/3
konio LGN projects to V1 layer 2/3 or V1 layer 4A
layer 2/3 further projects to layers 5 and 6, or extrastriate cortex
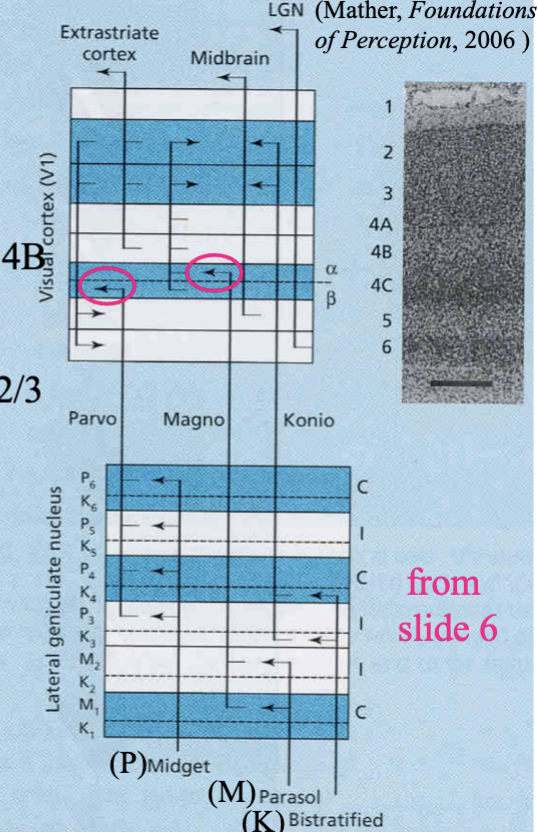
P-pathway
midget retinal ganglion cells (sustained, small rfs) → parvocellular LGN layers (sustained, small rfs) → layer 4C beta in V1 → layer 2/3 interblobs in V1 (orientation) → interstripes (orientation) in V2 → V3 → V4
K-pathway
bistratified retinal ganglion cells (large rfs) → koniocellular LGN layers (large rfs) → layer 4A and layer 2/3 (colour) in V1 → thin stripes (colour) in V2 → V4
M-pathway
parasol retinal ganglion cells (transient, large rfs) → magnocellular LGN layers (transient, large rfs) → layer 4C alpha in V1 → layer 4B in V1 (motion) → thick stripes (motion) in V2 → V3, V5
visual field
extent of visual space over which vision is possible with eyes held in a fixed position
about 190 degrees in humans
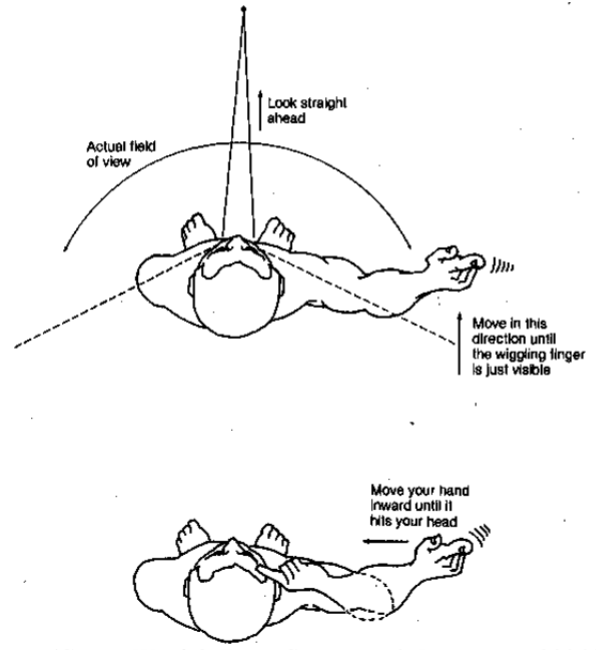
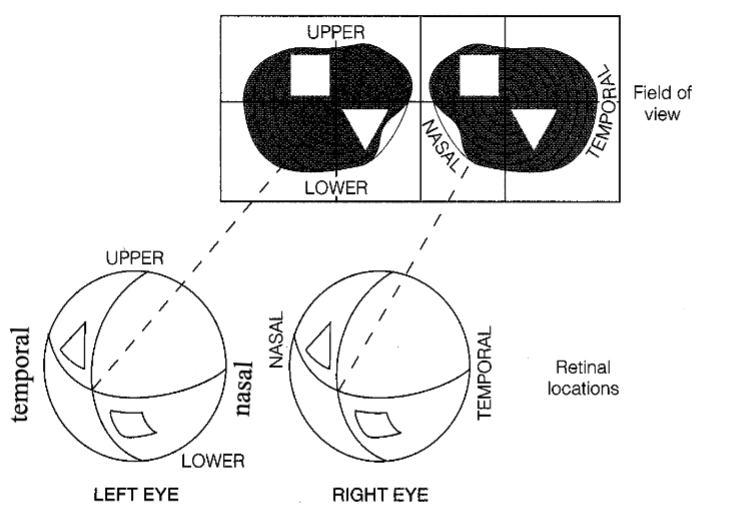
visual field representation in the eye
right visual field on nasal half of right eye and temporal half of left eye - left field on temporal half of right eye, nasal half of left eye
upper visual field on lower half of retina; lower visual field on upper half of retina
scotoma
small region of blindness in visual field due to damage in corresponding small region of retina
macular degeneration
disease of aging that damages cones in macula
