2. Pharm: Antidepressants and Bipolar Disorder
1/13
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
14 Terms
Classification of depression
Reactive: secondary in response to stimuli such as grief, illness, drugs/alcohol → 60% of all depressions
Endogenous: genetically determined inability to experience ordinary pleasure or cope with ordinary life events
Antidepressant mechanisms for serotonin and norepinephrine
Noradrenergic receptors
In depression monoamine (NE, serotonin & dopamine) neurotransmission is reduced
As a response, its receptors on the other side of the synaptic cleft are upregulated to increase uptake of the monoamines
What antidepressants do is block norepinephrine transporters (NET) that reuptake leftover NE, that way they can stay in the cleft for longer
At first, alpha2 autoreceptors have a negative feedback that prevents NE from being released into the synaptic cleft
After some desensitization, NE release becomes normal again
Results in increased cAMP → increased krebs, Increased BDNF → increases neurogenesis → antidepressants take effect
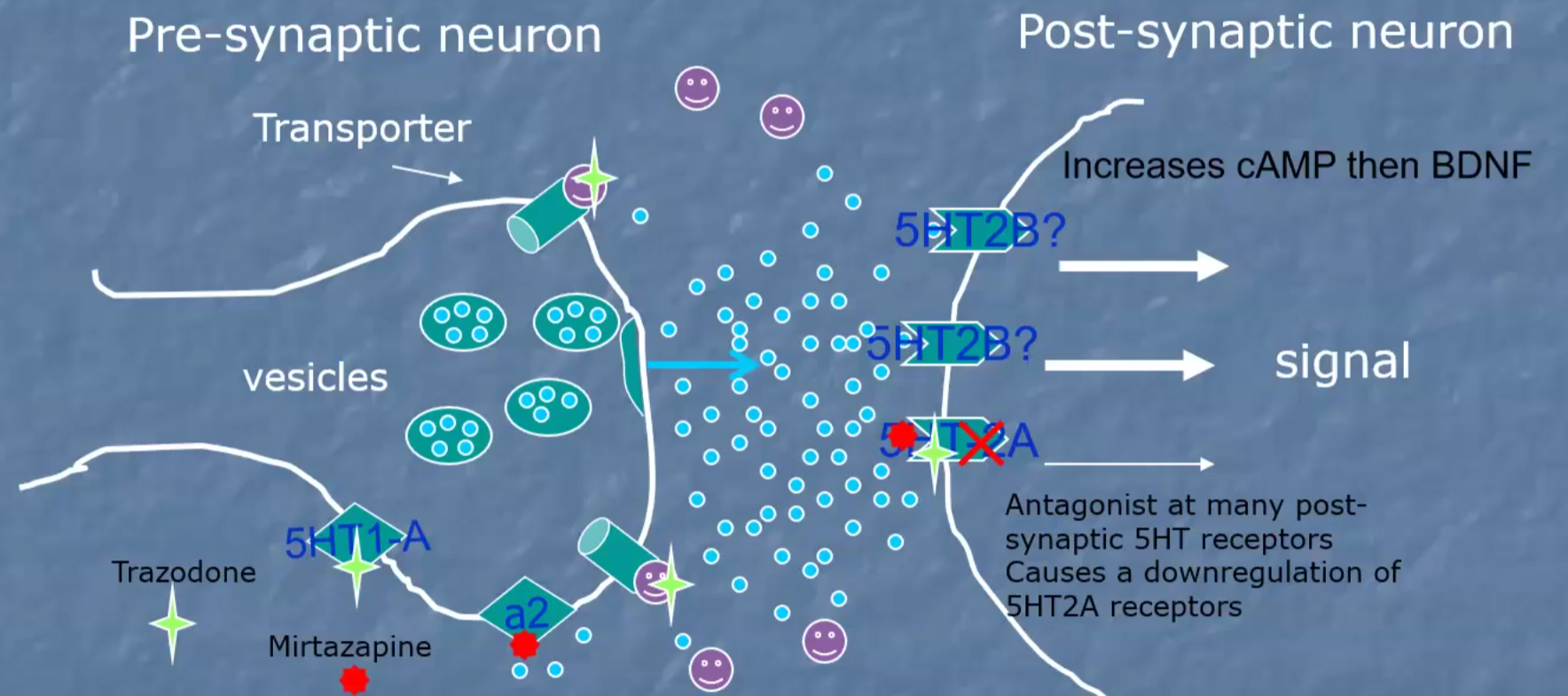
Serotonergic receptors
In depression monoamine (NE, serotonin & dopamine) neurotransmission is reduced
As a response, its receptors on the other side of the synaptic cleft are upregulated to increase uptake of the monoamines
What antidepressants do is block serotonin transporters (SERT) that reuptake leftover serotonin, that way they can stay in the cleft for longer
At first, 5HT1A autoreceptors have a negative feedback that prevents serotonin from being released into the synaptic cleft
After some desensitization, serotonin release becomes normal again → antidepressants take effect
Results in increased cAMP → increased krebs, Increased BDNF → increases neurogenesis → antidepressants take effect
What pain drug reduces the effect of antidepressants by more than 10%?
NSAIDs
Acute poisoning by TCA is life threatening at how many grams?
At 2g, so prescribe less so they can’t use it to commit suicide
Antidepressant uses
Major Adult depressive disorder
Enuresis children and geriatric
ADHD non responsive to stimulants
Severe anxiety disorders
PTSD
Psychosomatic disorders
Neuropathic pain
COPD and apnea
Premature ejaculation
Migraine prophylaxis
SSRI’s
MOA
Pharmacokinetics
Use
Variations
MOA: immediate and irreversible blockage of 5HT (SERT) which are GPCRs except 5HT3 (causes GI effects) and 5HT2C (causes agitation and restlessness)
Pharmacokinetics: strongly binds plasma proteins so HL is long 7-100hrs
Use: 1st line for depression
Variations:
Fluoxetine (Prozac): prototype
Use: Major depressive disorder/ BPD, OCD, Bulimia, Panic/anxiety, approved for >8 for depression and >7 for OCD,
Adv fx: headache, induced libido, GI problems, UR infections, Myalgia (1-2%), neonates may have withdrawals, slow elimination
Contraindications: may prolong QT, do not combine with MAOIs (serotonin syndrome), rash/lupus-like syndrome
Paroxetine: antimuscarinic, weak NET inhibitor
Use: more calming/sedating than others
Adv fx: increased male sexual dysfunction, significant withdrawals
Sertraline (Zoloft):
Use: PTSD, Premenstrual dysphoric disorder and social anxiety disorder
Most used due to least interactions
Weak dopamine transporter (DAT) inhibitor so good for low energy patients
Adv fx: QT prolongation
Citalopram:
Use: elderly and hot flashes
Adv fx: racemic mixture has antihistaminic actions and can increase QT
Escitalopram (Lexapro): citalopram’s more potent S-enantiomer
Use: no antihistaminic effect, no QT, pure SERT inhibition
Adv fx: few observed
Not Pure SSRI’s
Vortioxetine: partial agonist at 5HT1B ( slightly decreases release by pre-synaptic), agonist at 5HTA1( blocks release in presynaptic/desensitizes but increases mood in post-synaptic) and antagonist at 5HT3 + 5HT7 (reduces nausea+anx+cognitive dulling , improves, mood, sleep and cognitive flexibility)
Use: improves cognition independent of Major depression Disorder and cause less weight gain
Trazodone→ Serotonin Antagonist (weak 5HT2A and 5HT2C) and reuptake Inhibitor (SERT) → “SARI”
Use: Highly sedating so used as hypnotic, use higher dose for antidepressant or combine with a true SSRI or SNRI, reduces anxiety, insomnia and sexual side-effects
Vilazodone → Serotonin Partial Agonist (stimulates 5HT1A receptors) and Reuptake Inhibitor (blocks SERT) → “SPARI”
Use: improves sexual dysfunction side effects
Heterocyclics, 2nd an 3rd generation antidepressants; Atypical antidepressants
Bupropion:
MOA: higher affinity to DAT and some NET action (acts like an amphetamine)
Metabolites block NET and increase NE
Use: little to no sedation, muscarinic effects and decreases sexual dysfunction → depression, ADHD, smoking cessation
Contraindications: seizure disorders and aggravation of psychosis
Mirtazapine
Mirtazapine: stimulates 5HT/NE receptors to release due to antagonism of alpha 2 autoreceptors
MOA: Antagonizes 5HT and 2C post-synaptic receptors → sedating effects and weight gain
Combined with SNRI’s, it is called California rocket fuel
SNRI’s
MOA: All increase DA, NE and 5HT in prefrontal cortex and can be used to treat neuropathic pain due to adrenergic effects
Venlafaxine:
MOA: at low doses acts like SSRI, very low histaminic, muscarinic or adrenergic effects → must increase dose for NET effect
Use: GAD, Social anxiety, panic disorder, severe depression, Off-label for Diabetic neuropathy
Desvenlafaxine: same but higher NE activity and more side effects
Duloxetine:
MOA: SERT>NET
Use: pain, depression or both → diabetic neuropathy
Milnacipran:
MOA: NET>SERT = energizing
Use: fibromyalgia
Adv effects: sweating and urinary incontinence
Tricyclic Antidepressants (TCA)
MOA: developed as antipsychotics, have mixed NE and SE reuptake, no DA → affects alpha 1 adrenergic (heart and BP), muscarinic, histaminic and voltage gated Na+ channels → many side effects
Adverse effect: Sedation, sympathomimetic, antimuscarinic, cardiovascular, Psychiatric, neurologic, metabolic, overdose can be fatal
Contraindications: do not mix with MAOI until 2 weeks after stopping (convulsions, hyperpyretic crisis, death), acute recovery period from M, heart conditions, lowers seizure threshold, withdrawals
Amitriptyline:
Use: 2nd line for depression, off-label neuropathic pain, ADHD, enuresis, social anxiety
One of the most sedating
Clomipramine
Use: OCD, depression, autism and premature ejaculation
Highly sedating
Protriptyline
Use: Depression with apathy and withdrawal, adjunct to COPD due to stimulation of central respiratory centers
Doxepin
Use: More effect on 5HT than NE → Major depression, anxiety, bipolar, alcoholism. eczema, migraine prophylaxis, insomnia (low dose)
Contraindications: do not use with glaucoma or urinary retention
Monoamine Oxidase Inhibitors (MAOI)
MOA: Block MAO from deaminating and metabolizing monoamines
Two types: MAO-A (prefers NE, Epi and 5HT) and MAO-B (phenethylamine) → both metabolize DA
Pharmacokinetics: metabolized by acetylation so ½ of the population will experience slow acetylation
Drugs:
Phenelzine → A+B → irreversible (takes 2 weeks to clear)
Tranylcypromine → A+B → reversible
Selegiline → Only B → irreversible
Contraindications: do not mix with sympathomimetics (causes hypertensive crisis), no vasoconstrictors, avoid Wine, cheese, pickled herring etc (tyramine? foods), serotonin syndrome, do not use with SSRI’s, SNRI’s, Bupropion, meperidine or buspirone
Tx of hypertensive crisis → Phentolamine (alpha 2 antagonist)
Uses: Atypical, non-endogenous neurotic pts, used if pts are refractive to other drugs
Newer ADMs
Esketamine (Spravato): nasal spray
MOA: blocks NMDA receptors (antagonist)
Use: used in tx resistant patients (have tried 2 different AD), effects are present in 24rs, drug goes away but antidepressant effects are present for a longer time (short term)
Brexanolone:
MOA: Allopregnanolone analog, increase GABA-A
Use: 60r infusion to prevent post partum depression, monitor for CNS depression → very expensive
Electric convulsive therapy
Most rapid and effective way to treat severe acute depression in suicidal pts
Lithium
MOA: Alters electrochemical gradients in CNS, blocks release of DA and glutamate but stimulates serotonin and GABA, downregulates NMDA receptors, increases 5HT synthesis, G-protein de-coupling → basically a bunch of things that ultimately decreases monoamine neurotransmission
Pharmacokinetics:
Distributes in total body water, crosses BBB, 95% eliminated in urine but decreased Na+ (hyponatremia) increases its reabsorption and may cause toxicity
HL: 20-24 hrs
Small therapeutic index so serum levels should be monitored
Off-label tx for Bipolar
Valproate (1st line), Carbamazepine or Lamotrigine (maintenance) → for mania
Cariprazine → only drug approved for both manic and depressive phases
Risperidone (antipsychotic) , Haloperidol, Lurasidone
Valproate (antiepileptic) → Increases GABA