Lecture 12: Renal III Aspects of Renal Water Excretion and Conservation
1/65
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
66 Terms
Why is creatinine always expected in urine?
because 100% of filtered creatinine is excreted
Water intake sources
the water we drink and food we eat
What do we lose fluid to?
- Metabolic production
- Insensible loss and sweat
- The bulk of fluid loss is from urine and fecal waste
Why do we need to concentrate urine?
Humans are not surrounded by water at all times therefore we need to conserve water, we can do so by concentrating urine.
The longer the loop of Henle,
the more concentrated urine is
2 types of nephrons
cortical (85%)
juxtamedullary (15%)
Countercurrent mechanism
Occurs when fluid flows in opposite directions in two adjacent segments of same tube with hair pin turn
Countercurrent multiplier
interaction of filtrate flow in ascending/descending limbs of nephron loops of juxtamedullary nephrons
- Multiply the osmolality within the loop of Henle
Countercurrent exchanger
blood flow in ascending/descending limbs of vasa recta
Role of countercurrent mechanisms
- Establish and maintain osmotic gradient (300 mOsm to 1200 mOsm) from renal cortex through medulla
- Allow kidneys to vary urine concentration
Loop of Henle: descending limb
- Freely permeable to H2O
- H2O passes out of filtrate into hyperosmotic medullary interstitial fluid
- Filtrate osmolality increases to ~1200 mOsm
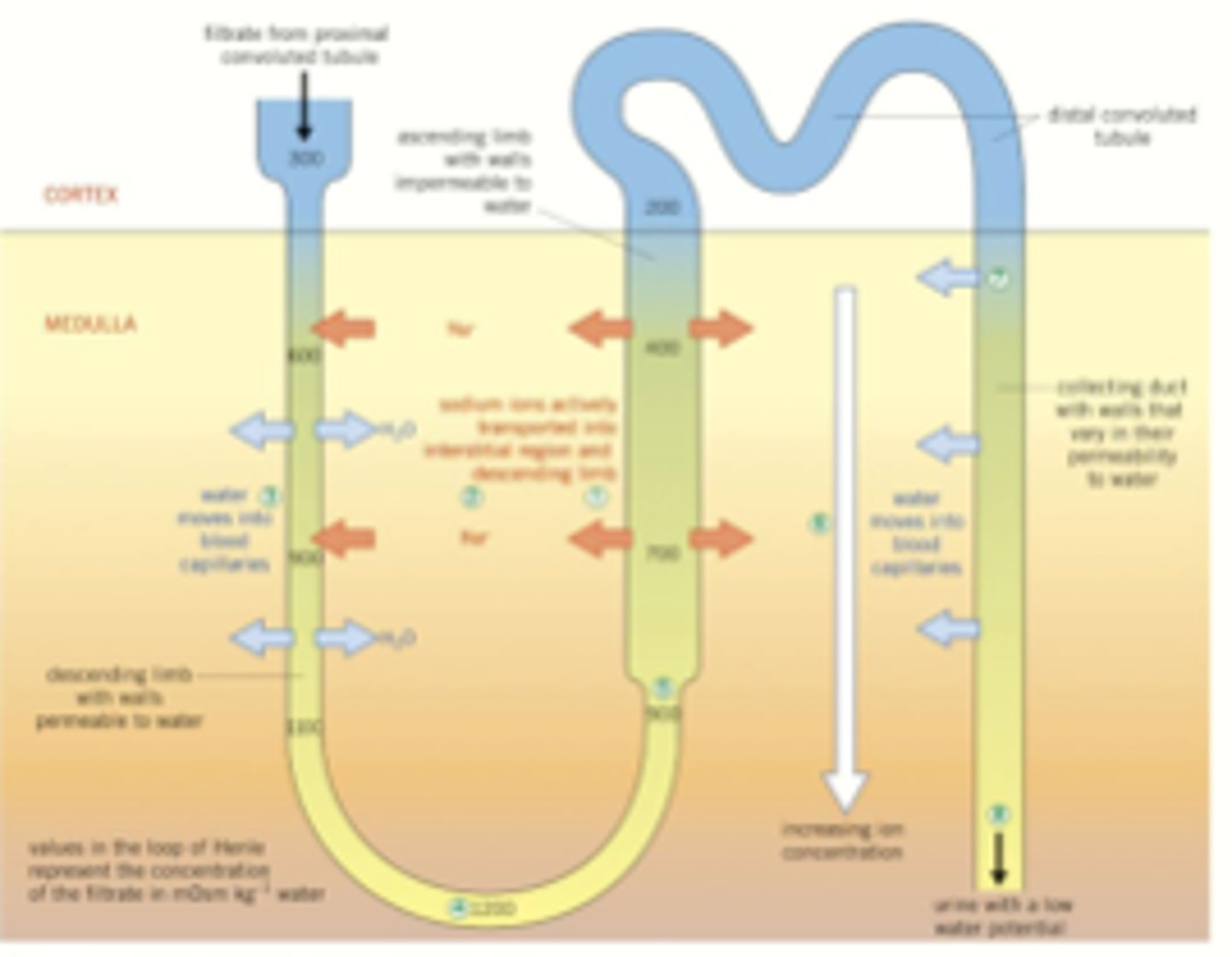
Loop of Henle: ascending limb
- Impermeable to H2O
- Selectively permeable to solutes
- Filtrate osmolality decreases to 100 mOsm
Solute permeability of ascending
Na+ and Cl- actively reabsorbed in thick segment; some passively reabsorbed in thin segment
What region of nephrons creates the osmotic gradient?
Long nephron loops of juxtamedullary nephrons
The countercurrent multiplier depends on which three properties of the nephron loop to establish the osmotic gradient.
- Fluid flows in opposite directions (countercurrent) through two adjacent parallel sections of a nephron loop.
- The descending limb is permeable to water, but not to salt.
- The ascending limb is impermeable to water, and pumps out salt.
There is a constant ___mOsm difference between the two limbs of nephron loop and between the ascending limb and interstitial fluid
200mOsm
Countercurrent multiplier and mOsm difference
difference is usually 200mOsm and gets 'multiplied' along length of loop to ~900mOsm
As water and solutes are reabsorbed, what does the nephron loop do?
it first concentrates the filtrate and then dilutes
Passage of filtrate through nephron loop - step 1
Filtrate entering the nephron loop is isosmotic to both blood plasma and cortical interstitial fluid.
Passage of filtrate through nephron loop - step 2
Water moves out of the filtrate in the descending limb down its osmotic gradient.
This concentrates the Filtrate.
Passage of filtrate through nephron loop - step 3
Filtrate reaches its highest concentration at the bend of the loop.
Passage of filtrate through nephron loop - step 4
Na+ and Cl- are pumped out of the filtrate. This increases the interstitial fluid osmolality.
Passage of filtrate through nephron loop - step 5
Filtrate is at its most dilute as it leaves the nephron loop. At 100 mOsm, it is hypoosmotic to the interstitial fluid.
Role of countercurrent exchanger
Preserve medullary gradient
- Prevent rapid removal of salt from interstitial space
- Remove reabsorbed water
Where is the countercurrent exchanger located?
vasa recta
From where does water enter the ascending vasa recta?
- Descending vasa recta
- reabsorbed from nephron loop and collecting duct
The volume of blood at the end of vasa recta is ___ than the beginning
greater
What structure preserves the osmotic gradient?
Vasa recta through the countercurrent exchanger
Permeability of the vasa recta
The entire length of the vasa recta is highly permeable to water and solutes
Because the vasa recta is permeable to both water and solutes what can we say about it and the vasa recta?
the vasa recta and its surrounding interstitial fluid, the blood within the vasa recta remains nearly isosmotic to the surrounding fluid
- does NOT undo the osmotic gradient
At the beginning of the vasa recta descending limb osmolarity = 300mOsm but at the end of the ascending limb osmolarity = 325mOsm why?
because oxygen and nutrients are brought in while metabolic waste is removed
Why is blood flow to the inner medulla so low? (0.3%)
The inner medulla houses the tip of the loop of Henle where urine is the most concentrated. We have little blood flow here to prevent 'wash out' of this region.
Collecting duct role
it tunes how much fluid we absorb/excrete to maintain the Posm at 300.
Urea role
helps form medullary gradient (concentrate urine)
Pathway of urea in the nephron loop
Enters filtrate in ascending thin limb of nephron loop by facilitated diffusion
Cortical collecting duct reabsorbs water; leaves urea
In deep medullary region now highly concentrated urea → interstitial fluid of medulla → back to ascending thin limb → high osmolality in medulla
Source of urea for the body
dietary protein
recycled protein
Where is urea located in relation to the nephron loop?
At the tip of the loop of Henle (to facilitate urine concentration)
If we eat a lot of protein, we excrete ____ urea than if we didn't
more
The collecting duct is naturally ___. Which hormone is responsible for water and urea uptake in the collecting duct?
- constricted
- ADH
Three players of the osmotic gradient
- long nephron loops (countercurrent multiplier)
- vasa recta (countercurrent exchanger)
- collecting ducts (adjust urine osmolality)
What is the maximum osmolality the nephron loop can reach?
1200mOsm
What hormone is secreted when osmolarity of blood rises?
ADH is secreted to bring it back to normal levels
Another name for ADH
Vasopressin
Effect of vasopressin - Step 1
Blood-borne vasopressin binds with its receptor sites on the basolateral membrane of a distal or collecting tubule cell
Effect of vasopressin - Step 2
This binding activated the cyclic AMP second-messenger system within the cell
Effect of vasopressin - Step 3
Cyclic-AMP increases the opposite luminal membrane's permeability to H2O by promoting the insertion of water channels in this membrane. This membrane is impermeable to water in the absence of vasopressin.
Effect of vasopressin - Step 4
Water enters the tubular lumen through the inserted water channels and subsequently enters the blood, in this way being reabsorbed. Water exits the cell through a different water channel permanently positioned at the basolateral border.
Aquaporins
(AQP) channels that allow entry of water
Different types: AQP-3, AQP-4
Body's response to dehydration
- ADH is released to reabsorb more water
- decreased water excretion
- Thirst
What structure does ADH act on? and how?
collecting ducts increases number of water channels in principal cells
When we aren't dehydrated does ADH secretion completely stop?
No, it does decrease but we have a constant low level of ADH
Why do we have basal secretion of ADH?
To keep Posm at 300
ADH depends on what in order to be secreted?
medullary gradient and presence of urea
Consequence for severely malnourished individuals concerning ADH secretion
lack of food = lack of urea
ADH cannot be secreted
Body's response to water intake
ADH secretion is decreased because we don't need to reabsorb more water in this situation
Under what conditions would we produce dilute urine?
overhydration
Making diluted urine
Filtrate at top of ascending limb is dilute due to salt removal
in the absence of ADH the collecting ducts remain impermeable to water & very dilute urine produced
When urine is diluted does the tip of the loop of Henle become concentrated?
No, the mOsm of the tip of henle is less than that of concentrated urine
What does it mean when the tip of the loop of Henle reaches 1200mOsm?
- urine is very concetrated
- dehydration
- NO URINE will be excreted
What are the two triggers of ADH secretion?
decreased plasma volume and increased plasma osmolality
As blood volume decreases, what happens to ADH secretion?
ADH secretion increases
What % of blood volume loss triggers ADH secretion?
10%
What regulates the sodium concentration of the ECF?
ADH and thirst mechanisms
What regulates sodium concentration of the body?
ANP hormone
Renin-angiotensin-aldosterone system
ANP hormone
atrial natriuretic peptide
ANP function
ANP hormone Increases water and sodium excretion