Drug Receptors and Pharmacodynamics: Key Concepts and Classifications
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
68 Terms
What is pharmacodynamics?
The actions/effects of the drug on the body.
What determines the classification of a drug?
The pharmacodynamics of the drug.
What is a drug receptor?
A component of a cell or organism that interacts with a drug and initiates the chain of events leading to the drug's observed effects.
What do receptors determine in pharmacology?
The quantitative relations between dose or concentration of drug and pharmacologic effects.
How do receptors select drug molecules?
They are selective in choosing a drug molecule to bind to, avoiding constant activation by promiscuous binding.
What happens to a receptor upon binding a drug?
It changes its function, altering the function of the biologic system to produce a pharmacologic effect.
What are the four classifications of receptors?
1. Regulatory proteins, 2. Enzymes, 3. Transport proteins, 4. Structural proteins.
What characterizes regulatory proteins as drug receptors?
They mediate the action of endogenous chemical signals like neurotransmitters and hormones.
What is the role of enzymes in drug receptor interaction?
They are inhibited or activated by binding a drug, such as dihydrofolate reductase for methotrexate.
What is an example of a transport protein receptor?
Na+/K+ ATPase, the membrane receptor for digitalis.
What is an example of a structural protein receptor?
Tubulin, the receptor for colchicine.
What are effectors in pharmacodynamics?
Molecules that translate the drug-receptor interaction into a change in cellular activity.
What is a common example of an effector?
Adenyl cyclase.
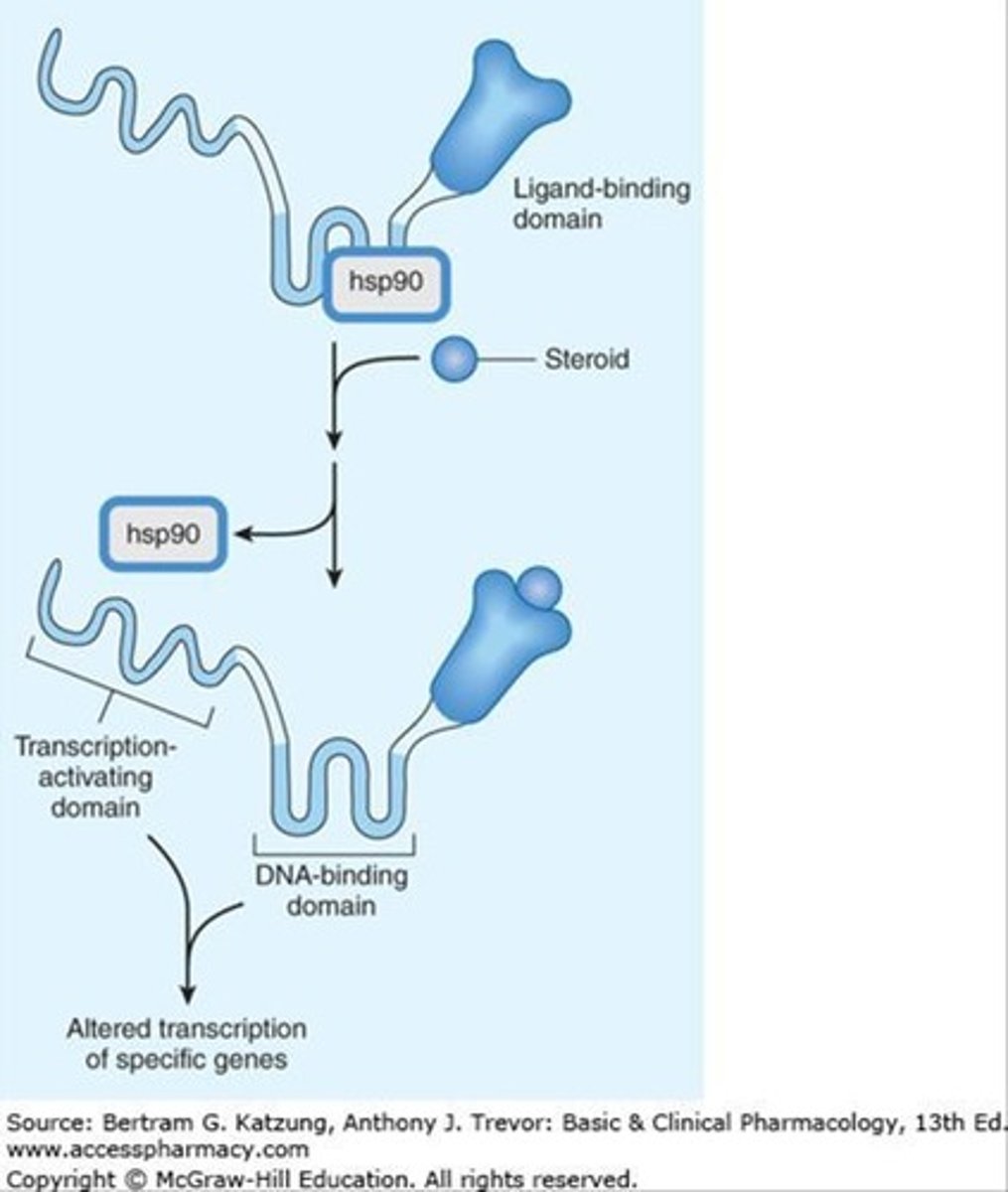
What is the first basic transmembrane signaling mechanism?
Lipid soluble drug crossing the plasma membrane and acting on intracellular receptors (e.g., steroids).
What is the second basic transmembrane signaling mechanism?
Transmembrane receptor protein with enzymatic activity regulated by a ligand binding to the extracellular domain.
What is the third basic transmembrane signaling mechanism?
Transmembrane receptor that binds and stimulates a protein tyrosine kinase (e.g., insulin).
What is the fourth basic transmembrane signaling mechanism?
Ligand-gated transmembrane ion channel which regulates the opening of the ion channel (e.g., GABA).
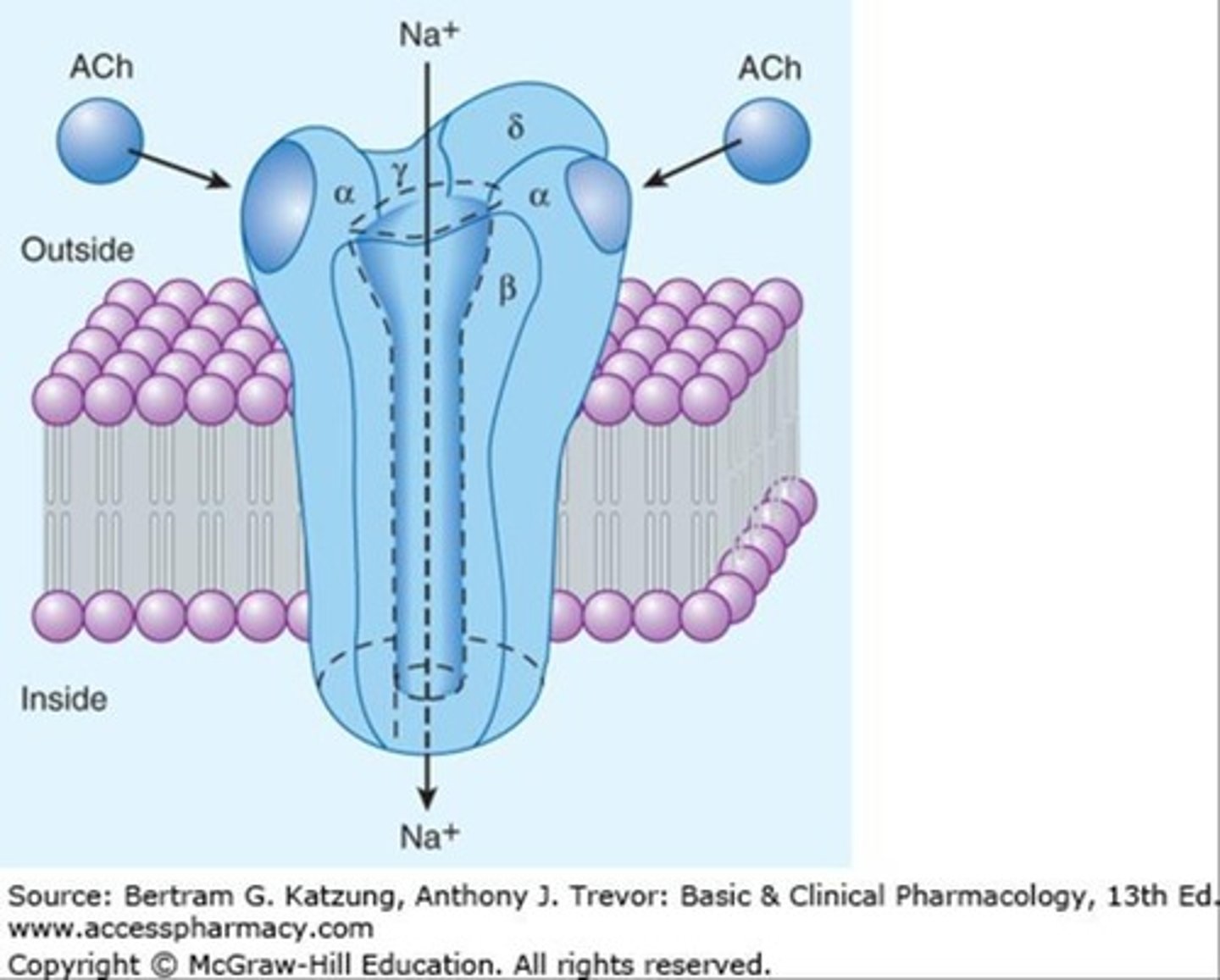
What is the fifth basic transmembrane signaling mechanism?
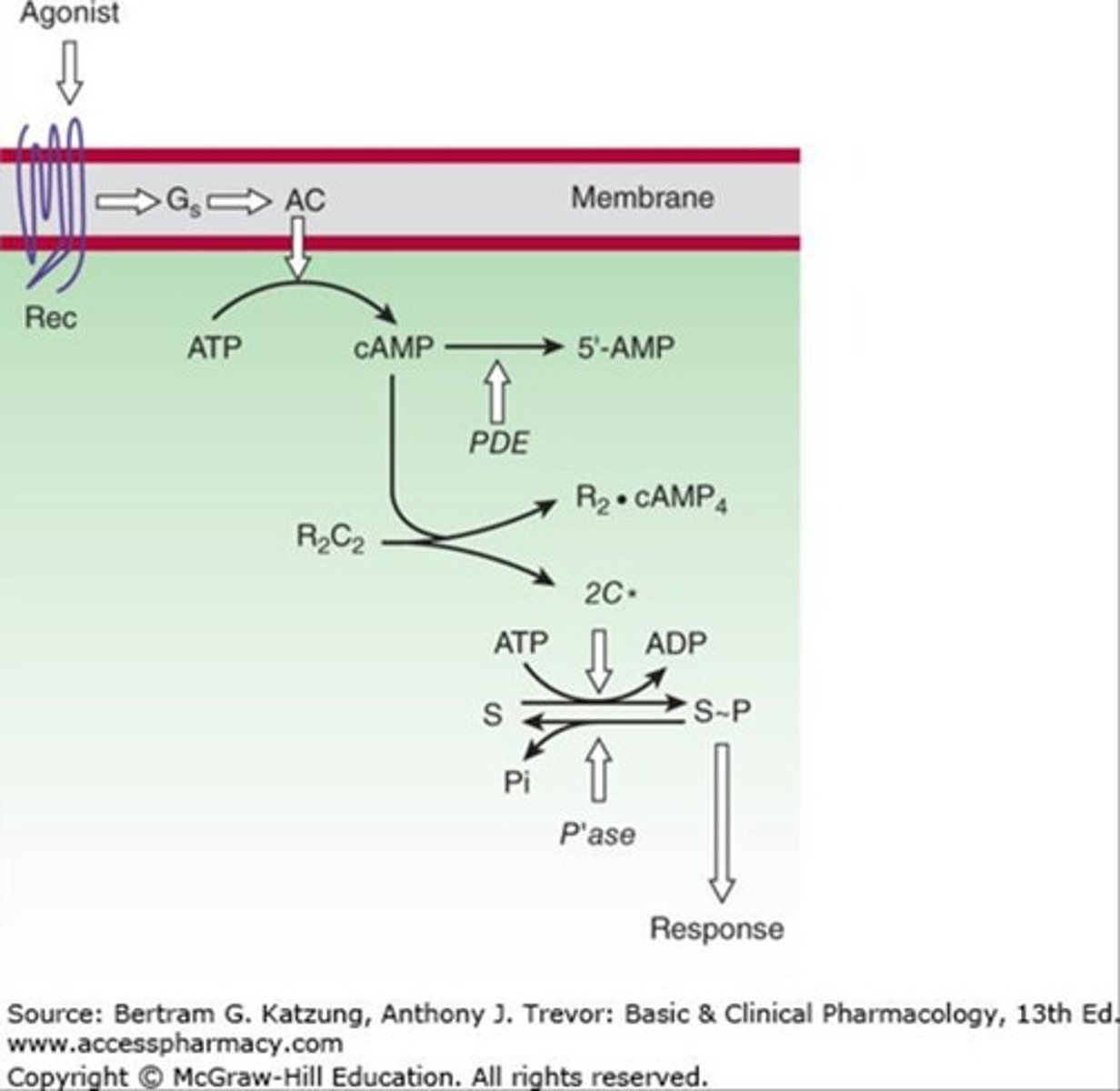
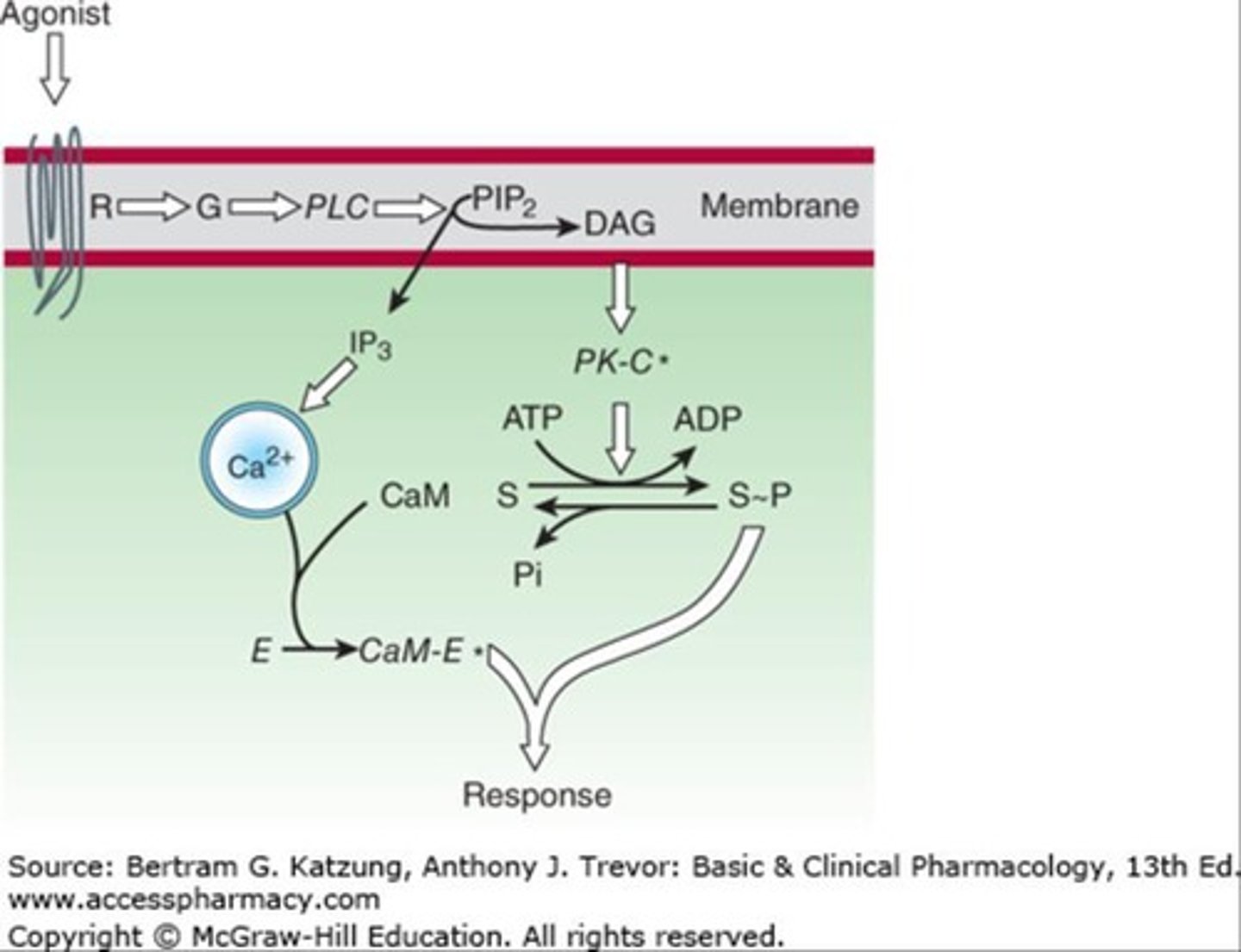
Transmembrane receptor coupled with an effector enzyme by G protein, modulating production of an intracellular second messenger.
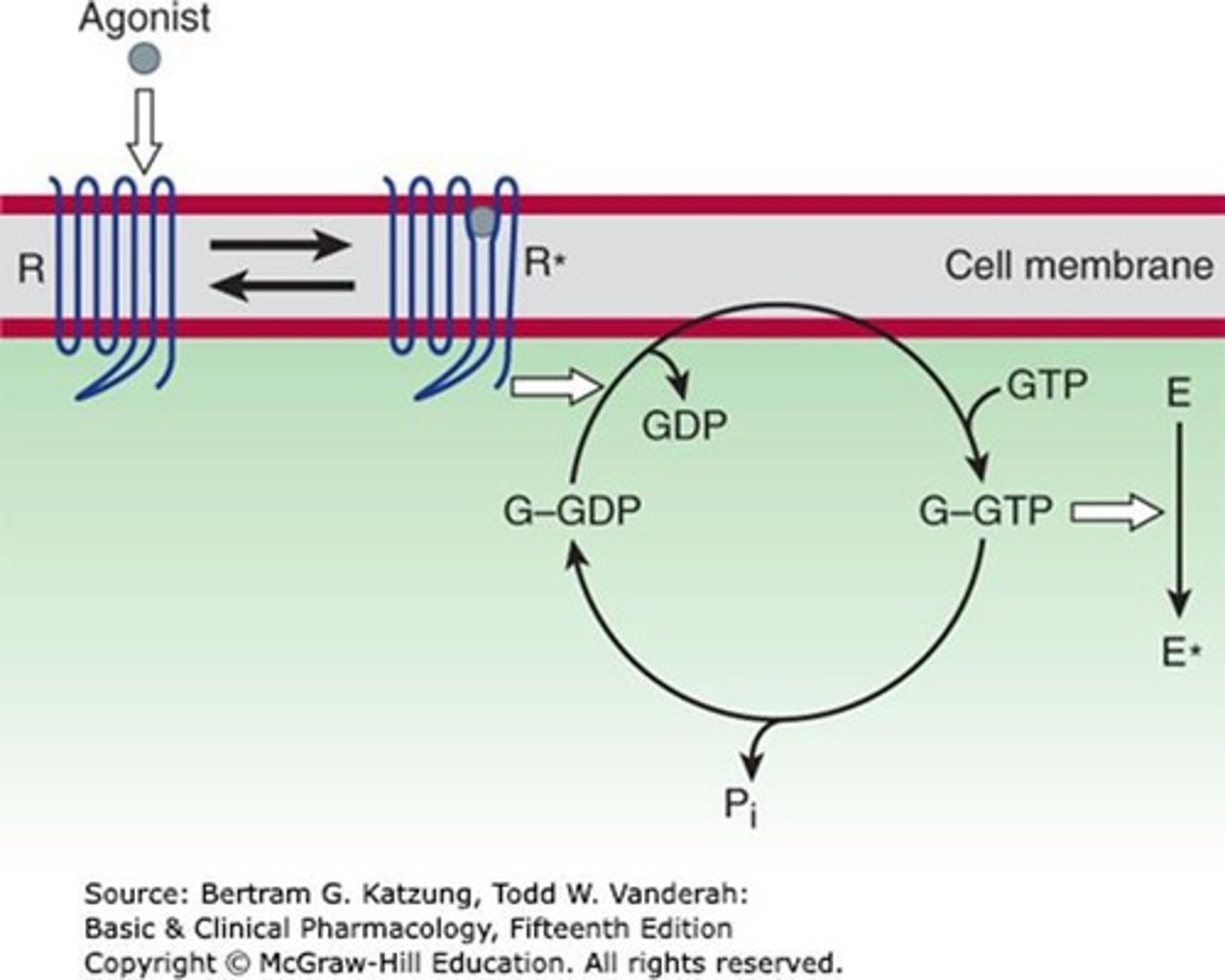
What is cAMP and its role in pharmacodynamics?
Cyclic adenosine monophosphate mediates hormonal responses and mobilizes stored energy.
What role do calcium and phosphoinositides play in signaling?
They bind to receptors linked to G proteins and stimulate membrane enzyme phospholipase C.
What is cGMP?
Cyclic guanosine monophosphate, a second messenger with few signaling roles in certain cell types.
What effect does cGMP have on vascular smooth muscles?
It causes relaxation through a kinase-mediated mechanism.
What does a graded dose-response curve measure?
The response of a receptor-effector system against increasing drug concentration.
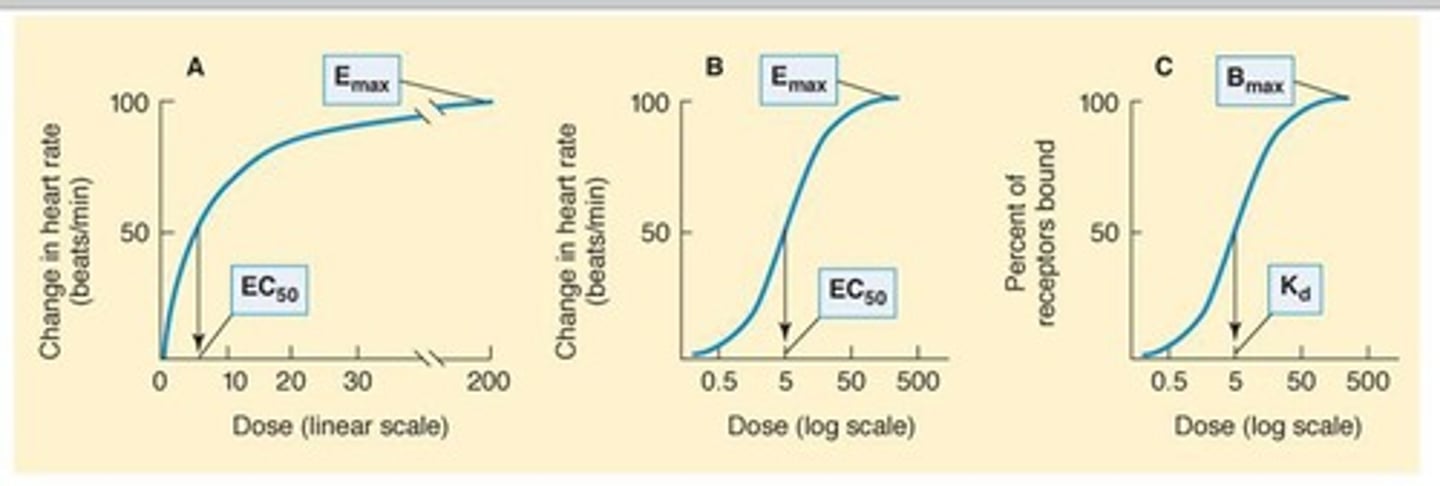
What shape does a graded dose-response curve typically take?
A sigmoid curve.
What do Emax and EC50 represent in a dose-response curve?
Emax is the maximal response produced by a drug, and EC50 is the concentration that produces 50% of the maximal effect.
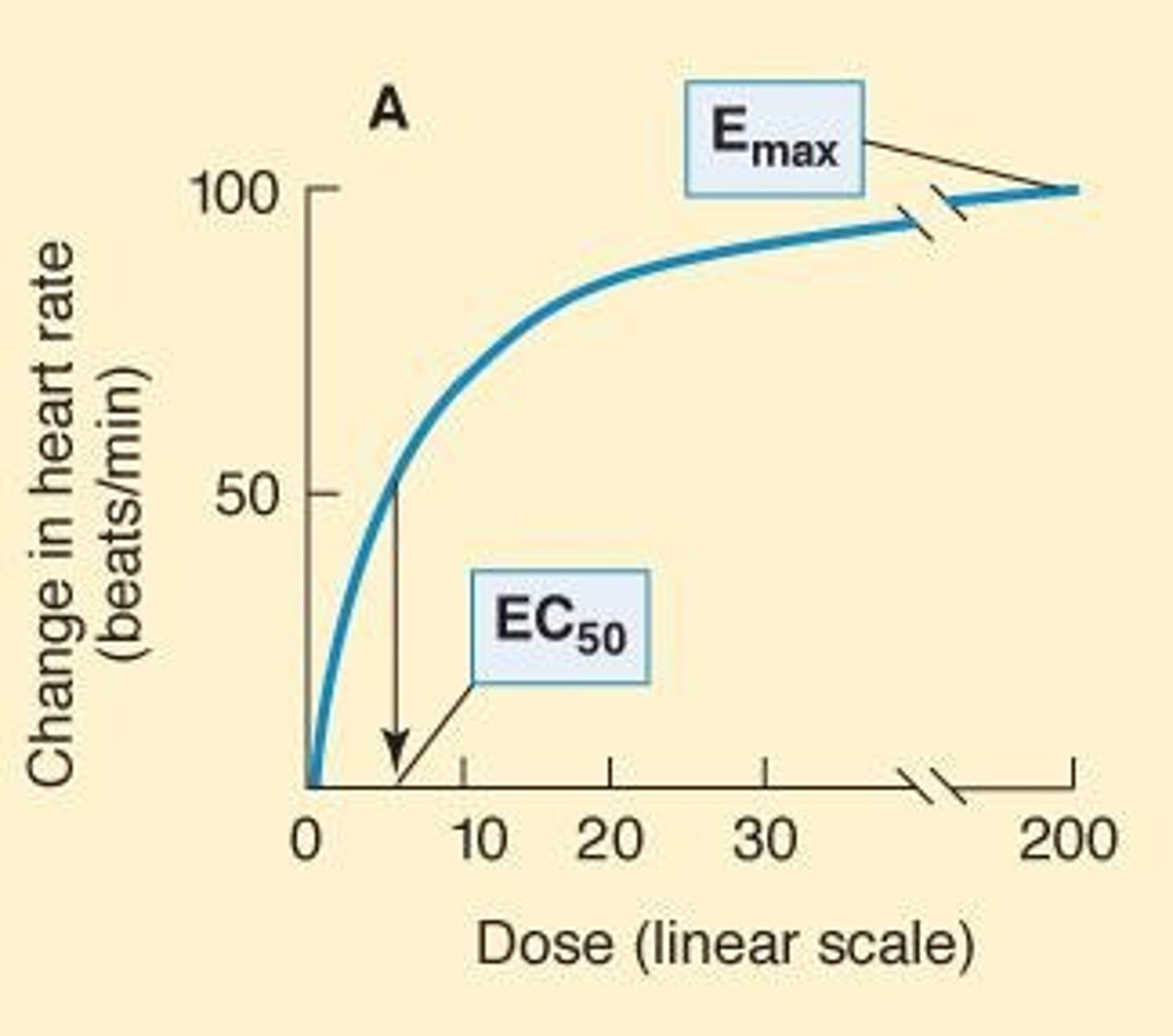
What does a smaller EC50 indicate about a drug?
It indicates greater potency.
What is Bmax?
The total number of receptor sites occupied by a drug.
What does KD stand for in pharmacodynamics?
Equilibrium dissociation constant, indicating the concentration of drug required to bind 50% of receptors.
What does a smaller KD signify?
Greater affinity of the drug for its receptor.
What happens to the dose-response curve when a low concentration of antagonist is present?
The curve shifts to the right, but the maximal response is preserved.
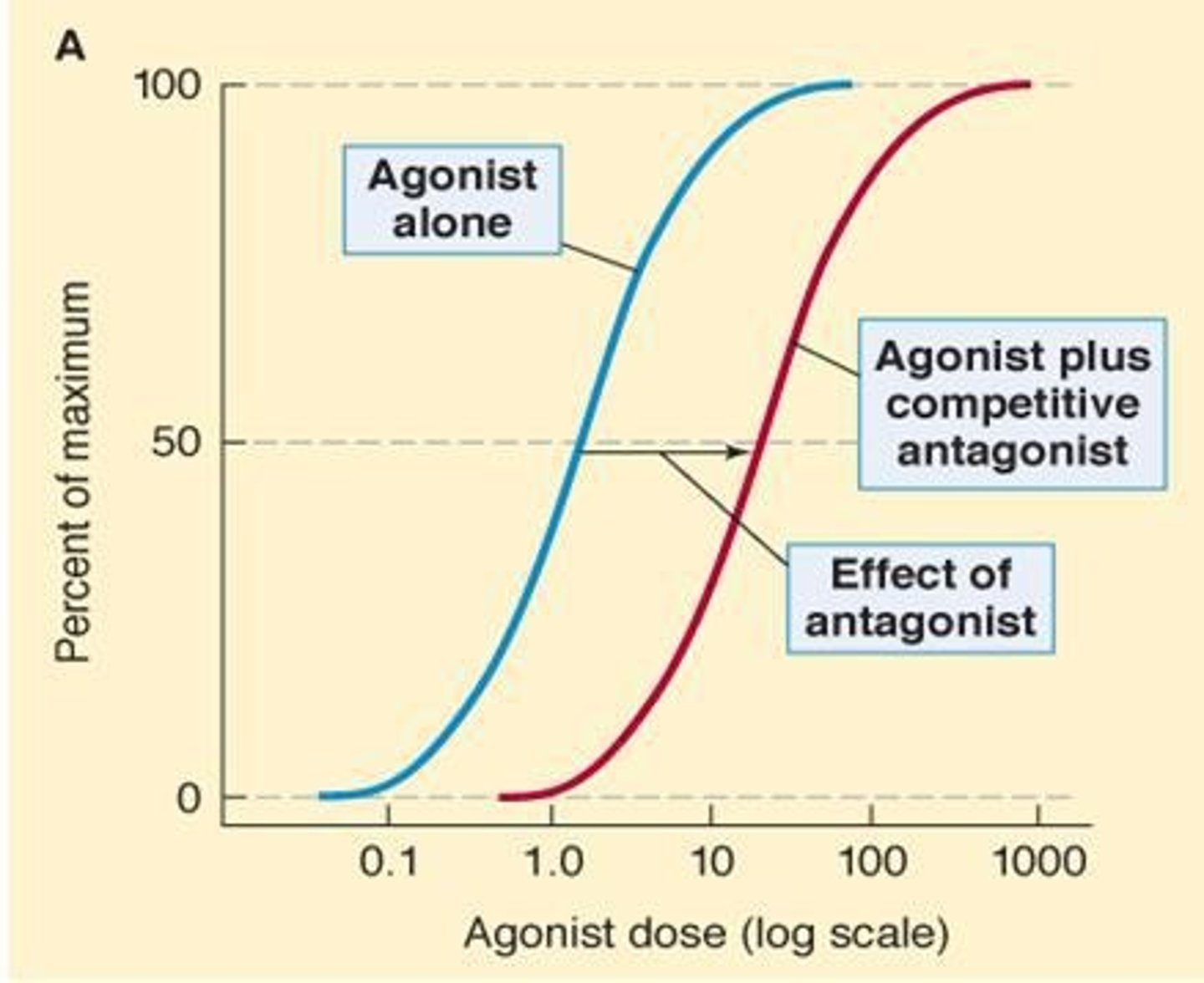
What occurs when a larger concentration of antagonist is used?
The available receptors are no longer sufficient to mediate an undiminished maximal response.
What is the effect of high concentrations of antagonist on receptor availability?
They reduce the number of available receptors, diminishing the maximal response.
What is pharmacodynamics coupling?
The transduction process between receptor occupancy and the production of specific effects.
What are spare receptors?
Receptors that allow maximal drug response at less than full receptor occupancy.
How does the presence of spare receptors affect drug response?
Drugs with low binding affinity can produce a full response even at low concentrations.
What is the relationship between EC50 and KD with spare receptors?
KD is greater than EC50 when spare receptors are present.
What are inert binding sites?
Non-regulatory molecules that bind drugs without causing detectable changes in biological function.
What role do inert binding sites play in pharmacodynamics?
They buffer drug concentration and bound drugs do not contribute to the concentration gradient for diffusion.
What is an agonist?
A substance that binds to a receptor and activates it to produce an effect.
What is a partial agonist?
A substance that produces less than the full effect, even when saturating the receptors.
What is an antagonist?
A substance that binds to receptors but does not activate them, blocking or competing with agonists.
What are the classifications of antagonists?
1. Competitive Antagonist 2. Irreversible Antagonist 3. Chemical Antagonist
What is a competitive antagonist?
A substance that competes with an agonist for receptor binding, increasing the agonist concentration needed for a response.
How does a competitive antagonist affect the concentration-effect curve?
It shifts the curve to higher doses horizontally, but the same maximal effect is still reached.
What is the effect of increasing agonist concentration in the presence of a competitive antagonist?
The effects of the antagonist can be overcome by adding more agonist.
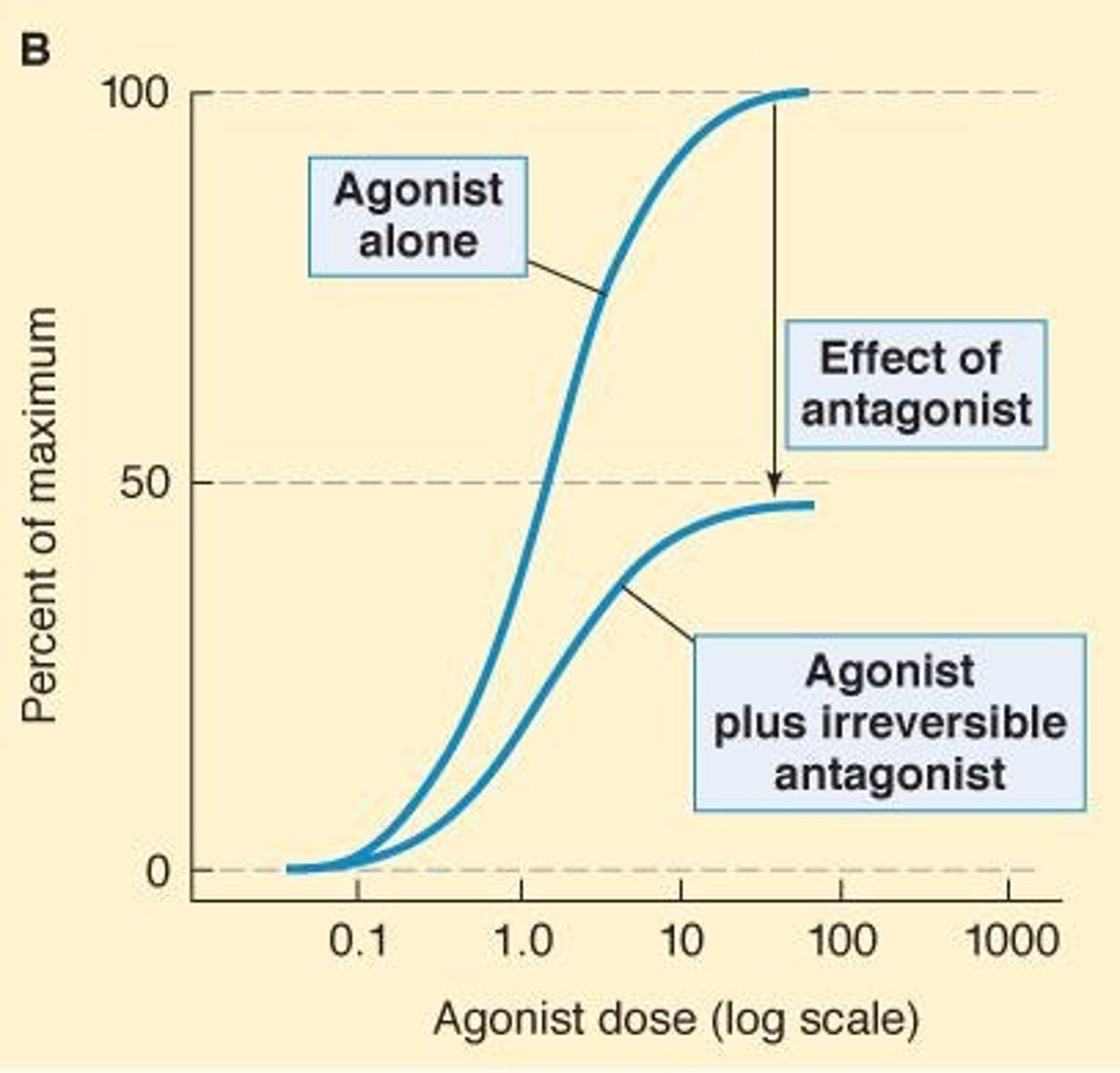
What is an irreversible antagonist?
A drug that binds to a receptor via covalent bonds, making the receptor unavailable for agonist binding.
What happens to the concentration-effect curve with an irreversible antagonist?
The curve moves downward, and Emax is not reached unless there are spare receptors.
What is chemical antagonism?
A mechanism that does not involve receptor interaction, where one drug interacts directly with another drug to negate its effects.
Give an example of chemical antagonism.
Protamine is used to counteract the effects of heparin.
What is physiologic antagonism?
A mechanism where a drug binds to a different receptor to produce effects opposite to those of the drug it antagonizes.
Provide an example of physiologic antagonism.
Glucocorticoids increase blood sugar, which is opposed by insulin.
What is receptor desensitization?
A phenomenon where the response to a drug diminishes over time despite the drug's continued presence.
What is a quantal dose-response curve?
A graph showing the fraction of a population that exhibits a specified response to increasing doses of a drug.
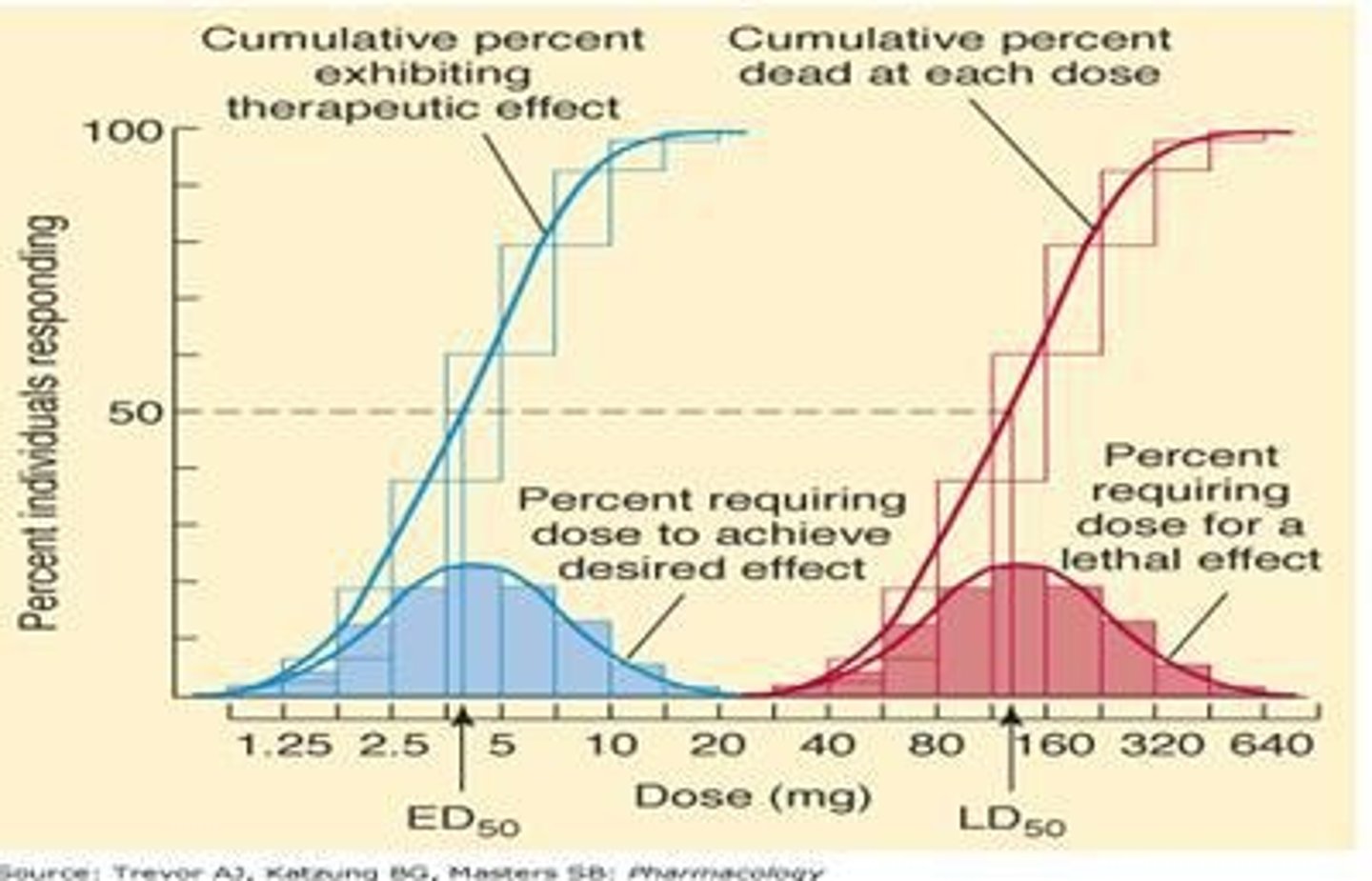
What does ED50 represent?
The median effective dose at which 50% of individuals exhibit the desired therapeutic effect.
What is the therapeutic index?
The ratio of TD50 (or LD50) to ED50, indicating the safety margin of a drug.
What is the therapeutic window?
The dosage range between the minimum effective concentration (MEC) and the minimum toxic concentration (MTC).
What does maximal efficacy (Emax) refer to?
The maximum effect an agonist can produce when administered at very high doses.
What is potency in pharmacodynamics?
The amount of drug needed to produce a given effect, often measured as EC50 in graded dose-response curves.
What is an idiosyncratic response?
An unusual or unknown response to a drug caused by genetic or immunologic differences.
What is tolerance in pharmacology?
A decreased sensitivity to a drug that develops after prolonged exposure.
What is tachyphylaxis?
A rapid decrease in response to a drug after only a few doses.
What is the overshoot phenomenon?
A rebound effect that occurs when a drug is abruptly discontinued after long-term use.
How can toxic effects be avoided in drug administration?
By giving low doses, carefully monitoring the patient, and using safer drugs.
What is down regulation in receptor pharmacology?
A decrease in the number of receptors available for binding due to prolonged exposure to a drug.
What is up regulation in receptor pharmacology?
An increase in the number of receptors available for binding, often in response to decreased ligand availability.
What is the significance of clinical selectivity in drug therapy?
It refers to the ability of a drug to act specifically on a disease while minimizing effects on other systems.
What is the relationship between beneficial and toxic effects of a drug?
Both effects can be mediated by the same receptor but may occur through different mechanisms.
How do antihistamines work on H1 and H2 receptors?
H1 blockers inhibit allergic responses, while H2 blockers reduce gastric acid secretion.