Pcol Exam 1 Flashcards
1/117
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
118 Terms
Pharmacology
The study of how drugs affect physiological function
Drugs
exogenous chemicals administered to affect biological functions substances used to diagnose, prevent, treat or cure disease
Ligand
something that binds to something else
has affinity (how well something binds to something else, usually via number of chemical bonds or strength of the bonds)
Target
what drug binds to → mostly proteins, enzymes, transporters, ion channels
drug are usually designed to have high affinity for this to elicit a biological response.
Draggability
refers to the target itself
how easy it is to design a drug that does what is wanted at target
agonist
substances that activates receptors (many drug mimics this)
Antagonist
ligand that binds to receptor and prevents activation
voltage acitvated, ligand gated
Channels can be ____ or ____
into, depolarize, positive
Na+ moves ___ cell and _______ cell, making it more ____
into, depolarize, positive
Ca+ moves ____ cell and ____ cell, making it more ____
out of, hyperpolarize, negative
K+ moves ____ cell and ____ cell making it more ______
into, hyperpolarize, negative
Cl- moves ____ cell and ____ cell making it more ______
Enzyme
coverts substrate to product
inhibit
____ enzyme will lead to increase substrate amount and decreased product amount
activate
_____ enzymes will lead to decrease substrate and increased product amount
into or out of
a transporter or a pump moves substances _____ cell
inhibit
inhibiting a transporter or pump will ____ movement across membrane
increase
activating a transporter or pump will ____ movement across membrane
agonist + receptor → autophosphorylation → activation of cellular signaling
List the tyrosine kinase receptor pathway
agonist + receptor (inside cell) → transport to nucleus → activation of gene transcription and translation
List the nuclear hormone receptor pathway
agonist + receptor (7-TM) → G-protein activation → generation of second messenger → activation of cellular signaling
List the G-protein coupled receptor
allow cell to cell communication
what is role of receptor
adenyl cyclase → cAMP → Protein kinase A → increase protein phosphorylation
Gs binds to b-adrenergic receptor. List rest of pathway
phospholipase C → diaglycerole → protein kinase C
phospholipase C → IP3 → Ca2+ release
Gq binds to mGluR receptor and leads to an increase protein phosphorylation and activate calcium binding proteins. List rest of pathway
adenyl cyclase → cAMP → protein kinase A → decreased protein phosphorylation
Gi binds to Dopamine D2. List rest of inhibition pathway
decrease protein phosphorylation and open K+ channels
Gi does 2 important things
hyperpolarize
Gi opens K+ channels
because K+ is higher in cell → K+ dumps out of cell and cell becomes _____ (cell more negative and less active)
IP3 and DAG, enzymes
____ are second messangers are produced by _____
basal state
when no agonist are present
inactive
____ receptors are more energetically favorable
active
G-proteins binds to ____ receptors ONLY
more ligand + active receptor complexes are formed
More agonist = more [R*L] complexes are formed, what does [R*L] mean
they will shift into active receptors
As more [R*L] forms, what happens to inactive receptors
inverse agonist
____ binds preferably to inactive receptors
agonist
preferential affinity
if ligand has 100-300x higher affinity for active receptor
inverse agonist
preferential affinity
if ligand has 100-150x higher affinity for inactive receptor
partial affinity, 100x
10x affinity for active is not selective enough → ____
____x affinity is the cutoff
partial agonist
_______ binds to both active and inactive receptors with reduced efficacy compared to a full agonist
can have a higher affinity for an active receptor but a lower efficacy than a full agonist.
neutral antagonist, inverse agonists
Antagonists: used to reduce response of endogenous agonists
graded response
numerical value such as (HR= beats/min, BP=millimeters of mercury, glucose level = mg/dL)
quantal response
yes or no (did this drug kill an animal, did drug prevent pregnancies?)
potency
efficacy is “how effective” a drug is
unrelated to ____
Emax, y -axis
Efficacy is determined by
the maximum efficacy
the plateau
EC50 or ED50, x-axis
____ or ____ represents potency
the concentration/dose that produces 50% of maximal response
Kd
equilibirum dissociation constant
describes affinity of ligand for receptor
high
low KD = _____ affinity
low
high KD = ___ affinity
additivity
1+1=2
synergy
1+1=3
potentiation
1+0=2
additive
agonist with 2nd substance increases response
synergistic
2 agonist combined = GREATER than additive effect
potentiation
agonist + inactive leads to a response MORE than agonist on its own
competitive antagonist
dose response curve shift to right and Emax is not reduced
effect can be overcome with higher dose of agonist
higher dose of antagonist = needs even higher dose of agonist for a response
reversible competitive antagonism
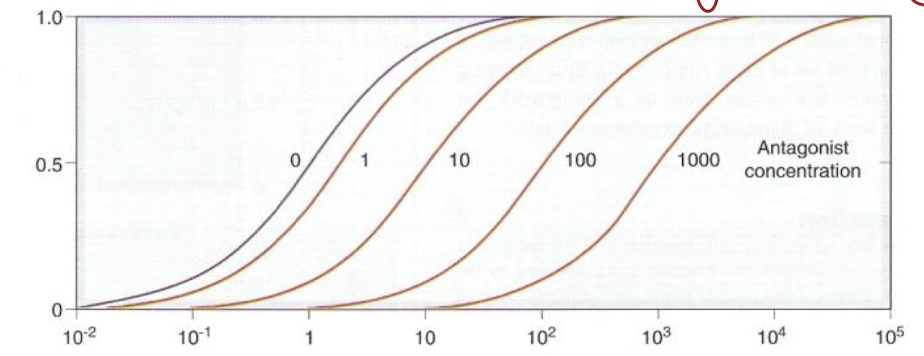
irreversible noncompetitive antagonism
Competitive antagonists, reversible
______ are usually ________ because they bind to the exact same site on a receptor that the natural molecule (the agonist) would. This is the active site. The binding is typically non-covalent, meaning it's a temporary interaction, like a magnet.
Competition for the Active Site: The antagonist and the agonist are like two people trying to sit in the same chair. Whichever one is present in a higher concentration, and has a higher affinity (stronger attraction) for the chair, will win the spot.
Overcoming the Antagonist: Because the binding is reversible, you can overcome the antagonist's effect by simply increasing the concentration of the agonist. If you flood the area with enough agonists, they will eventually outcompete the antagonists and activate the receptors.
Analogy: Think of a key (agonist) and a master key (competitive antagonist) trying to get into the same lock (receptor). The master key doesn't open the lock, but it occupies the keyhole. However, if you have enough regular keys, you can eventually displace the master key and open the lock.
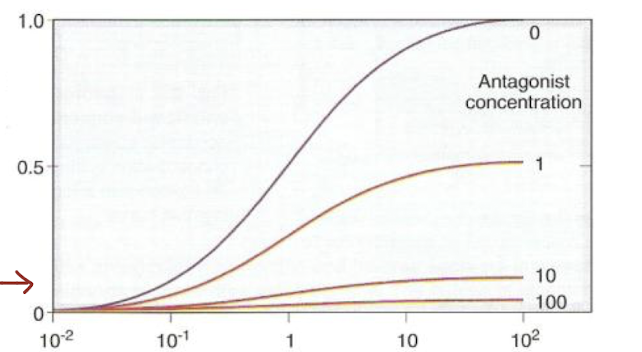
Noncompetitive antagonists, irreversible
________ are often ________ because they don't compete for the active site. Instead, they bind to a different location on the receptor, called an allosteric site.
Change in Shape: When the noncompetitive antagonist binds to the allosteric site, it causes a change in the overall shape of the receptor. This conformational change is often permanent or long-lasting due to the formation of strong, sometimes covalent (irreversible) bonds.
No Competition: The key difference is that they are not competing with the agonist. The agonist can still bind to its active site, but because the receptor's shape has been altered, it can no longer be activated.
Overcoming is Not Possible: You cannot overcome the effect of a noncompetitive antagonist by increasing the agonist's concentration. The receptor is effectively "broken" or deactivated, and no amount of agonist will fix it. The only way for the receptor to become functional again is for the cell to create a new receptor.
Analogy: This is like someone gluing a piece of wood to the inside of the lock's mechanism. The key (agonist) can still go into the keyhole (active site), but no matter how many keys you try, you can't turn the lock because the internal mechanism is permanently blocked.
are non-therapeutically favored because
too high dose, too high response
cant administer agonist to reduct effect
selectivity
the relative affinity for a ligand + target in comparison to some other protein
high affinity
drug is designed to bind to target
low selectivity
drug has high affinity to other proteins in the body as well
high selectivity
drug has low affinity to other proteins but high affinity to target
specific
A ____ drug would ideally have an effect on only a single, unique target. Specificity is a theoretical ideal that is rarely, if ever, achieved in practice. A truly specific drug would bind to its target and nothing else, regardless of the dose. It's a binary concept: a drug is either specific or it's not. Since all drugs have the potential for some level of off-target binding, the term "specificity" is generally avoided in favor of "selectivity”
LD50/ED50 or ED50 (adverse effect)/ED50 (therapeutic effect)
therapeutic index
high affinity, high selectivity
drugs prefer ____ and ____
20nM because low # means higher affinity
a drug with 400 nM and 20 nM affinity, which one has higher affinity?
mechanism of action
how drug works
therapeutic effects
reason why give drug
indications
disease state to give drug
side effects
an effect other than therapeutic effects
adverse effect
an effect other than therapeutic effect that causes a bad/undesirable response
contraindications
reason why NOT to give drug
toxic
what happens with high level of drug
usually an exacerbation of what drug does
too much drug is administered or too little drug is leaving the body
allergic
involves immune system → it recognizes drug as harmful
idiosyncratic
we dont know why patient responses a certain way to drug → reason usually has to do with patient’s genetics
fetopathic
kills fetus in uterus
teratogenic
leads to deformity in fetus when born m
mechanism based side effects
due to drug binding to targets its designed to bind but target is in many different parts of the body
ex; drug may bind to different target (position wise)
off target side effect
caused by drug binding to something else (selectivity problem)
potent
a drug with high affinity for its target would be more _____ than a drug with low affinity for same target
dissociation (activation) of Gs - activation of adenylate cyclase- activation of PKA
what is the correct order for following activation of Gs-coupled receptor
off-target adverse effect
an _____ is due to poor selectivity of a drug
affinity
the KD is a measure of a drug’s ____
hydrophilic
How does a metabolite differ from a parent drug?
metabolite is made more ______ and is usually less active than the parent drug.
- stays in nephron to be eliminated via urine
biotransformation (same as Metabolism): body's ability to convert lipophilic drug to metabolite
Substrate → product is same as drug → metabolite
cytochrome p450, hydrophilic
Phase I metabolism involves ______ family enzymes → metabolize endogenous substances, synthesize some molecules or breakdown exogenous substances
simple reactions to make phase I metabolism more _____
transferases
Phase II Metabolism involves the enzyme ____ (enzyme that transfer or attach hydrophilic endogenous and large substances onto phase I metabolites
so they can be eliminated from the body b/c theyre so hydrophilic so little chance of being reabsorbed
first pass metabolism
how much metabolism occur on first pass through liver
drug is given orally = absorbed from GI to travel to liver (where phase I metabolism occurs before entering systemic circulation)
high first pass metabolism
drug is good substrate for enzyme so very little parent drug is going to come out into bloodstream
low first pass metabolism
drug is NOT good substrate for enzyme so most parent drug is going to come out into bloodstream after it first pass through liver
decrease
increase bioavailability, ____ first pass metabolism
increase
decrease bioavailability, ____ first pass metabolism
very little gets into bloodstream
drug with high first pass metabolism means _____
drug cannot be given orally or give super high oral dose
oral bioavailability, Fpo
% of parent drug that reaches circulation (as parent drug, NOT metabolite) following oral administration
oral absorption and first pass metabolism
what are the two factors that oral bioavailability depends on
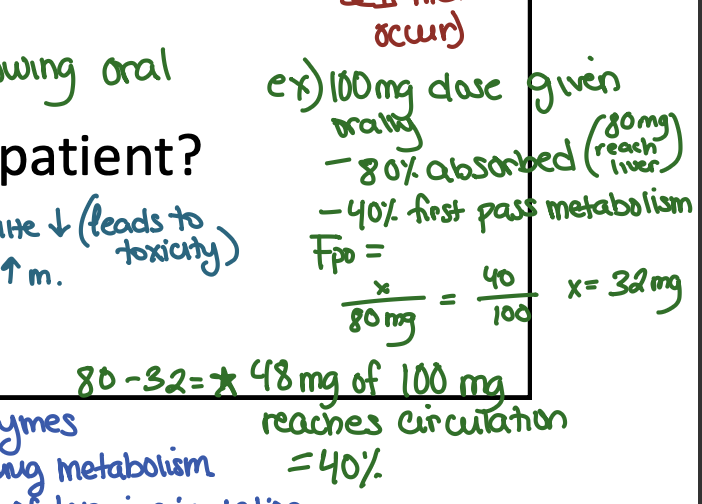
48
if 100 mg of a drug is given and 80% absorbed, 40% first pass metabolism, what is Fpo
TOXICITY
Why can metabolism differ between patients or within the same patient?
disease status: liver disease (liver is site to drug metabolism and status means reduced metabolism)
age: newborns (will have undeveloped complements of enzymes and will not metabolize well) vs elderly (above age of 65 loses 1 of hepatocytes yearly = less or metabolism = increased drug level and metabolites = _____
prodrugs
low drug level, increase metabolites
inhibition of metabolic enzymes
how does metabolism contribute to drug-drug interactions?
enzyme inducers
leads to sub-therapeutic responses
enzyme inhibitors
leads to increase in drug level and toxicity