infection and the immune system
1/31
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
32 Terms
Pathogens
microorganisms / infectious agents that cause disease
different forms of microorganisms / infectious agents
viruses
bacteria
fungi/yeast
protozoa
helminths
prions
how do we acquire infections?
transmission can be by physical contact, ingestion, inhalation, via vectors or breaching skin defences
microorganisms exploit mucosal sites (respiratory, gastrointestinal and urogenital tracts) for transmission
the skin acts as a barrier. breaches (abrasions, cuts) can make the host vulnerable to infection. biting insects can acts as vectors for disease transmission by bypassing the skin defence barrier.
mucosal immunity is highly specialised and very important for protection against infection, developing mucosal vaccines has been challenging
what makes microorganisms harmful?
a combination of factors, some of which are microbe-specific (virulence factors), others are host-specific (inflammation)
microorganisms evolve and adapt to their hosts and vice-versa. such adaptations can be site-specific and/or host specific (intra-host or inter-host)
intra-host
the immune system might ‘ignore’ microorganisms at one anatomical site, but react to them at another.
e.g. commensals ignored in the gut, but stimulate very strong inflammatory immune responses if they spread to other anatomical locations (ruptures of the gut wall)
inter-host
microorganisms that cross species barriers may not produce disease in one host but can in another and even be lethal
inter-species transmission: zoonotic infections
humans and animals share common ecosystems hence their health is intrinsically linked (One health). this provides opportunities for infections to spread from animals to humans (zoonoses) and vice-versa (reverse zoonoses).
this can occur via ingestion, physical contact, aerosols, environmental contamination.
when pathogens jump species barriers to establish infections in different hosts, the outcome is unpredictable
evolutionary host-pathogen adaptations
bats have constitutive interferon activity that suppresses viral infections (innate immunity)
bats also have unusually large naive antibody repertoires which dont require rapid affinity maturation for limiting viral replication (adaptive immunity)
selective pressures and transmission opportunities determine the survival and expansions of virus mutations. mutations selected for in one host species can have implications for disease pathogenesis in a different species
host adaptation of viruses
virus mutations are randome and can enhance transmission, virulence or immune evasion, depending on selective pressures and opportunities (including human behaviours). effective surveillance is key to protecting public health in a globalised society
CFRs - case fatality ratio
most CFRs are estimates. they depend on methods used to record deaths and the strategies for diagnosing infection rates within the population
CFRs can influence perceptions of risk versus hazard
individual human behaviours then impact on disease transmission and uptake of control strategies such as vaccination which subsequently affect populations
lessons from smallpox vaccine
success with smallpox vaccination was due in part to the efficacy of the vaccine at inducing herd immunity and to the fact that variola virus can only infect humans (there is no animal reservoir) - pathogen dependence on a single host is a potential achilles heel
using microorganisms for vaccination - benefits and risks
live-attenuated vaccines usually work well because they induce strong immunity, but they carry the risk due to their live nature, particularly for immuno-compromised individuals
dead or subunit vaccines (using part of the microorganism) are usually safer, but often dont work as well as live-attenuated vaccines, require effective adjuvants to stimulate strong protective immunity
we can genetically engineer ‘benign’ microorganisms to deliver a component of a disease-causing microorganism for vaccine-induced protection: viral vectors
co-evolution with microorganisms
our immune system expects to be challenged and may become dysregulated if not exposed to microorganisms
it might not be the presence of microorganisms but their absence thats cause disease
microbial flora
antibiotics have saved countess lives but need to be used carefully (antimicrobial resistance)
disrupting the natural microbial flora with antibiotics can lead to opportunistic yeast and fungal infections
roles of the immune system
controlling infections
killing tumours
immune pathology
graft rejection
metabolic diseases
what is the immune system?
a range of cells working together as a team
the immune challenges
detect a vast array of different pathogens
distinguish between harmful (pathogens) and harmless (food, pollen) exposures
respond rapidly and eliminate invading pathogens using the appropriate killing mechanism
control the strength of the response to limit immune-mediated damage
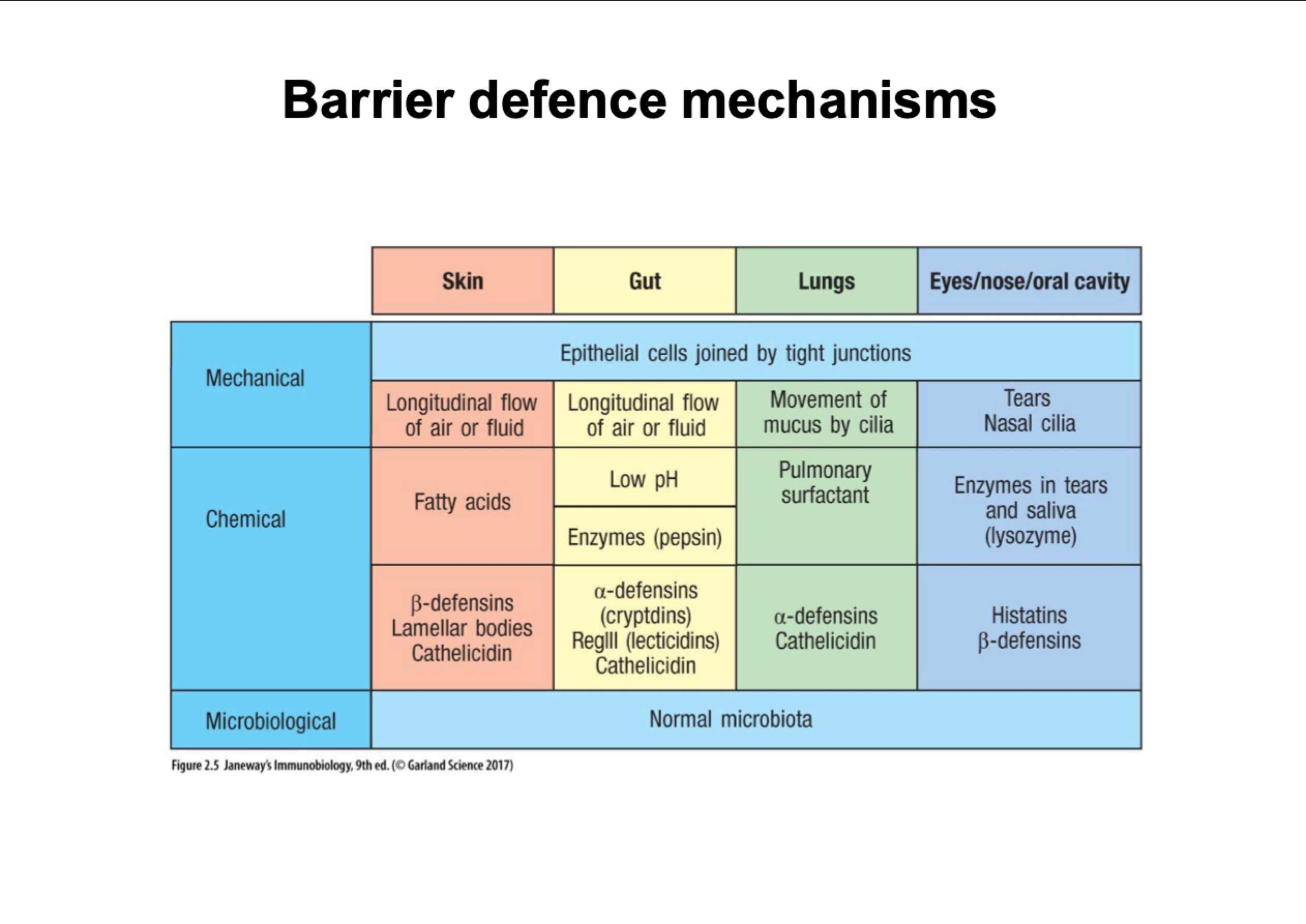
barrier defence mechanisms
tight junctions stop things getting between cells
cilia waft upwards, pushes anything that gets in lungs
stomach low ph, acid destroys bacteria
tears have lysozymes that break down bacterial cell walls
how do pathogens penetrates the barriers
skin breaks, wounds/burns
animal bites
insect bites
parasites burrow through skin
mucosal barriers
placenta
lungs
STDs
faecal-oral
food
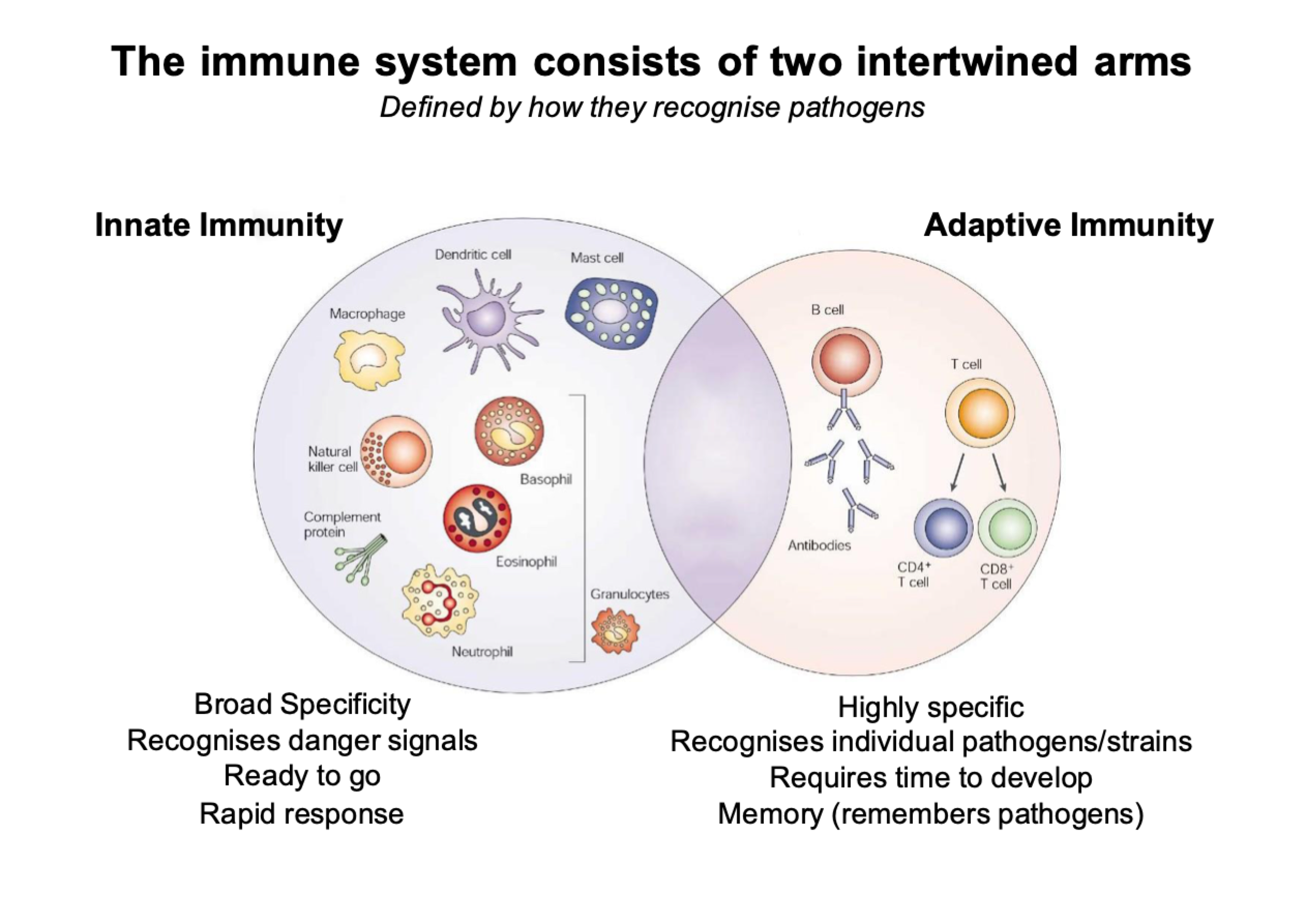
innate and adaptive immunity
the immune system consists of two intertwined arms
innate immunity is our first line of defence:
broad specificity
receptor recognise danger signals
rapids responses
can tell the class or type of virus
buys time until adaptive response kicks in
innate cells kick in first then works in partnership with adaptive cells
Adaptive immunity:
highly specific
recognises individual pathogens/strains
requires time to develop
memory (remembers pathogens)
B and T cells
slow
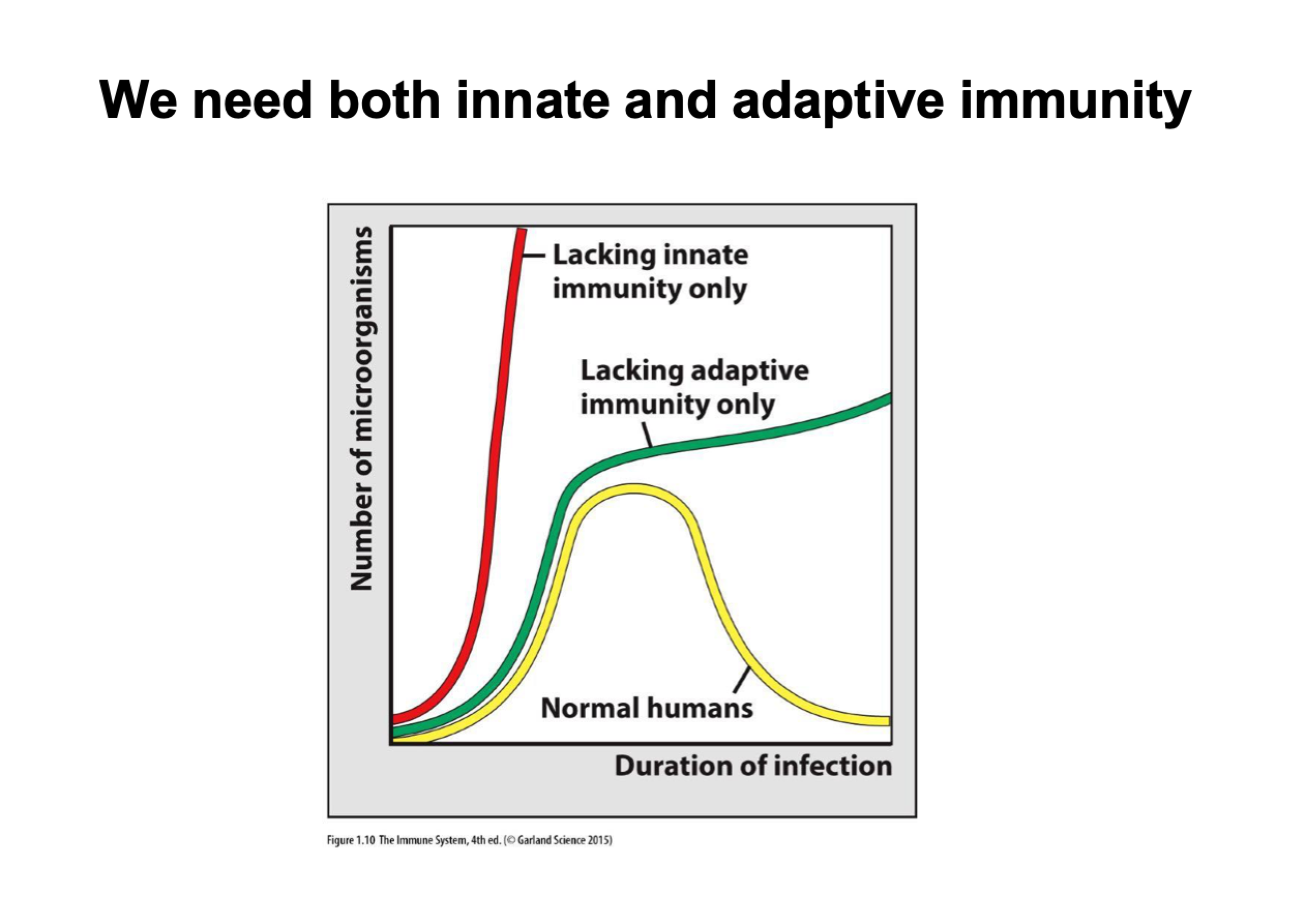
necessity of innate and adaptive immunity
we need both innate and adaptive immunity
absence of innate immunity - die quickly as theres nothing to respond to infection
absence of adaptive immunity - might be fine if infection dose is low, higher dosage of infection will result in death
functions if innate immunity
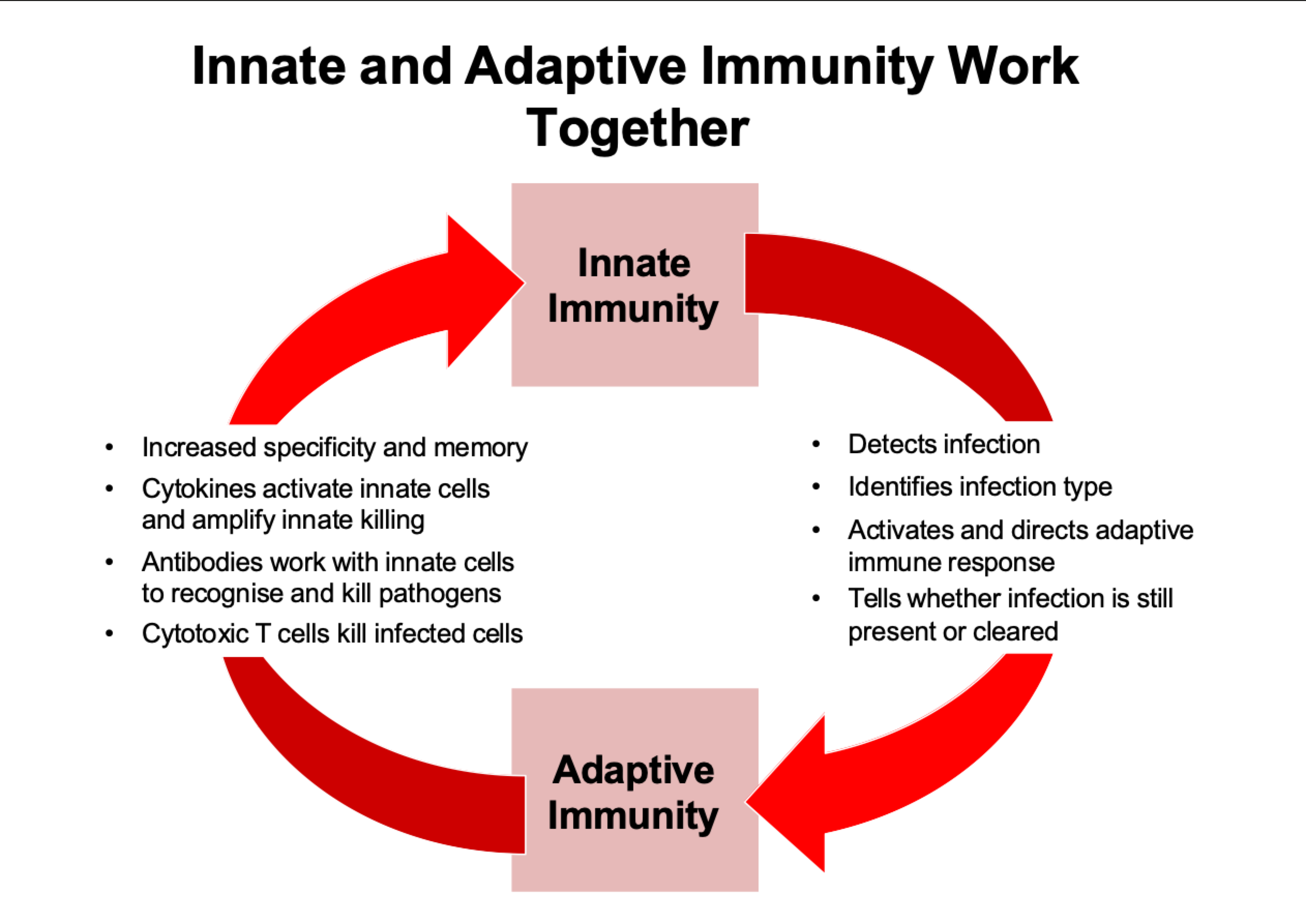
senses and responds to danger signals (infection & damage)
always on, always ready to respond instantly
communicates danger to other cells of innate and adaptive immunity
recruits immune cells to infection site (inflammation)
tells adaptive immune cells when to respond
cellular and biochemical killing mechanisms
innate killing mechanisms
phagocytosis - engulf bacteria and digest
killing of infected cells - NK cells identify infector or tumour, cells tell them to commit apoptosis
secretion of cytotoxic granules - fired out to microbes and kills them
complement proteins - punches holes causing them to explode
adaptive immunity
adaptive immunity consists of T cells and B cells
T and B cells can recognise a huge range of proteins and molecules (called antigens) with a high degree of specificity
their specificity for the pathogen makes the immune response more effective
identifying and expanding the T and B cells that recognise the pathogen takes time, which is why adaptive immunity is slow
T and B cells can remember previous encounters with pathogens (immune memory)
3 types of T cell
helper T cells (Th cell):
coordinate immune responses
amplifies innate immunity
talks to other cells
regulatory T cells (Treg cells):
turn-off immune responses
counter part to helper cells, turns off immune responses when not needed
cytotoxic T cells (CTL):
kill infected cells
B cells
B cells produce antibodies that:
are highly specific to individual pathogens
neutralise pathogen molecules e.g. toxins
mark pathogens for destruction by other immune cells
link innate and adaptive killing mechanisms
immune memory
adaptive memory is specific to the original pathogen
adaptive memory responses are faster and bigger
adaptive memory combines specificity with speed
innate and adaptive immunity work together
cytokines
cytokines are chemical messengers (like hormones)
many different cytokines with different functions
target any cells with relevant receptor
allow one cell to signal to many cells
cells dont need to be in contact
can act locally or systematically
cell to cell communication
use receptor/ligand pairs on cell surface
many different receptors and ligands with different functions
cells have to be in contact and have correct receptor/ligand pairs
allows very precise communication between individual cells
lymph nodes and spleen
specialised sites where immune responses are coordinated
focal points for immune cell communication
play a very important role in initiating adaptive immune responses