Homestasis
1/81
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
82 Terms
Homeostasis
The process of keeping the environment inside the body fairly constant. The body’s cells are surrounded by fluid, and its composition and temperature must be maintained in narrow limits.
the stimulus–response–feedback model
Stimulus: A change in environment.
Receptor: Stimulus detected by sensory cells.
Modulator: A control center processes the messages from receptor.
Effector: Muscles or glands recieve message from modulator.
Response: Effector organs bring about appropriate reactions.
Feedback: The response changes original stimulus.
Negative feedback - dynamic equilibrium and tolerance limits
Reduces or eliminates the stimulus that caused it. Returns the body to a steady state. The fluctuation is called dynamic equilibrium. The point around which conditions fluctuate is the set point. Tolerance limits are the upper and lower limits between which the levels fluctuate.
Cellular respiration
Glucose is energy for cell activities. Energy released from glucose through this.
Glucose + Oxygen → Carbon Dioxide + Water + Energy
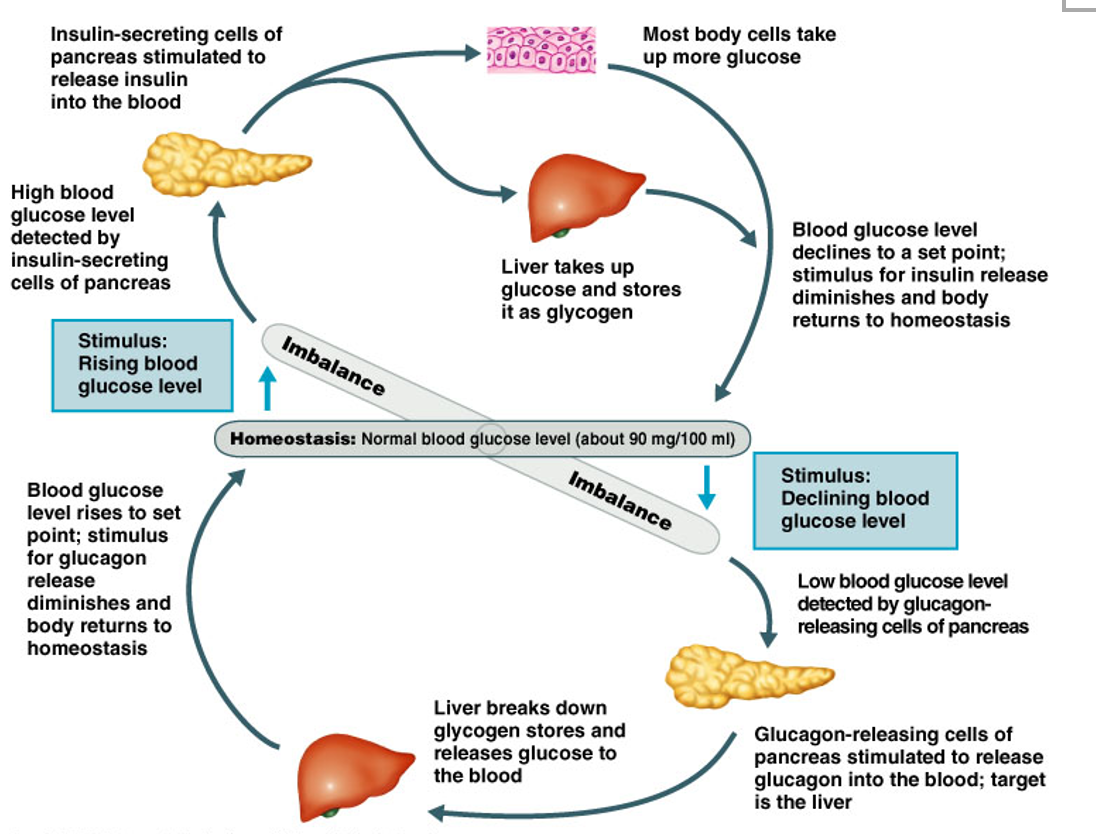
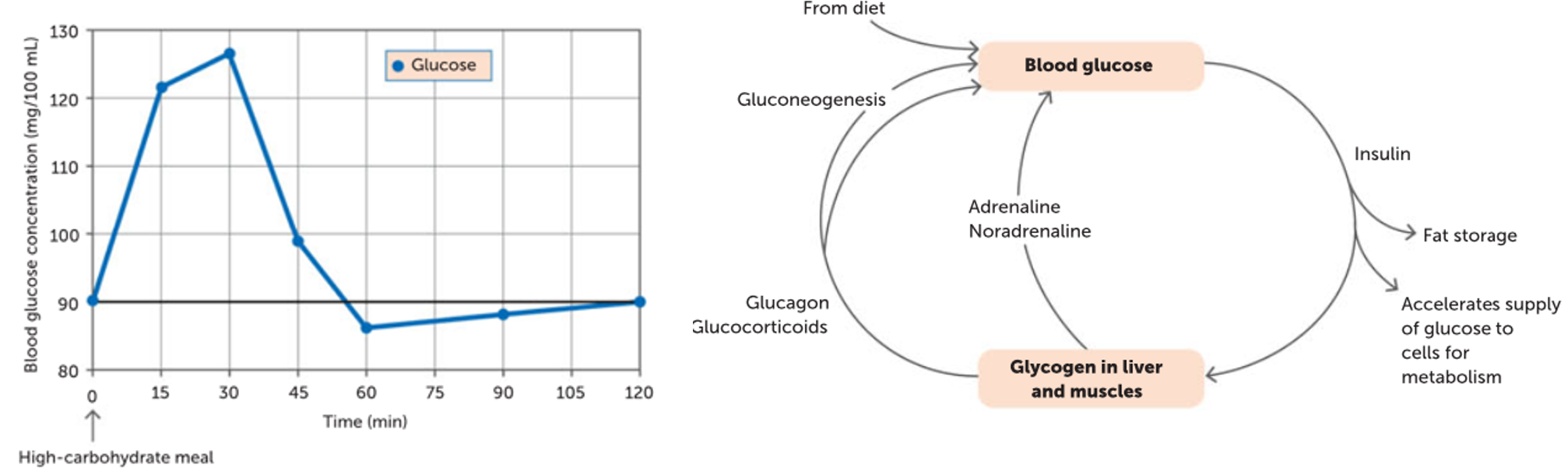
Normal blood glucose levels are between 4-6 mmol/L (90mg/100ml)
Glucose storage
After a meal, blood glucose concentration can rise and excess glucose must be removed and stored between meals.
Glucose is stored as glycogen. Able to store about 500g of glycogen: 100g in the liver, 400g in skeletal and muscle cells

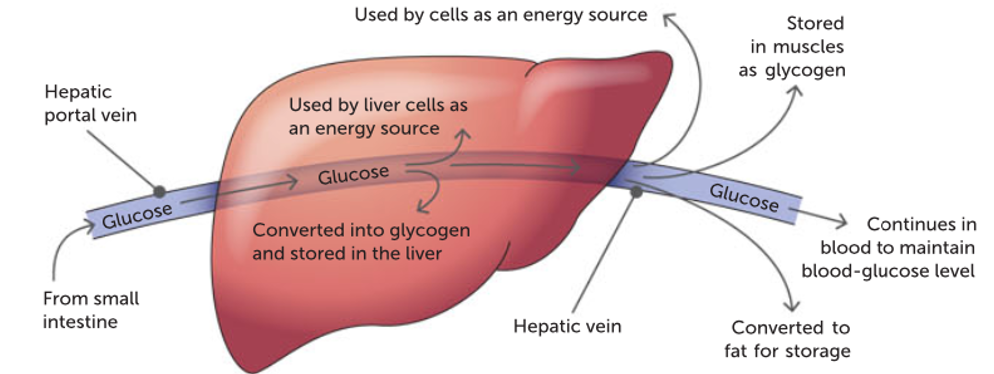
Role of the liver
Converts glucose to glycogen and vice versa. The hepatic portal vein brings sugar-rich blood directly from the small intestine to the liver. The breakdown of products are absorbed into the blood capillaries of the villi of the small intestine.
The liver can:
1) Remove glucose from the blood to provide liver with energy
2) Remove glucose from the liver and/or muscles and converted into glycogen for storage.
3) Circulate glucose around the body for cells to absorb and use as energy.
4) Convert excess glucose and glycogen into fat for long-term storage.
Glycogenesis
The process where glucose molecules are chemically joined in long chains to form glycogen.
Stimulated by pancreatic hormone insulin. Glycogen in muscle cells provides the glucose required for activity.
Glycogenolysis
The process of converting glycogen in liver and muscle cells back into glucose when glucose levels are low.
Stimulated by pancreatic hormone glucagon. Glycogen stored in the liver is a short-term energy supply. Provides energy for about 6 hours.
Gluconeogenesis
Process where glucose is made from fats (lipids) and amino acids in the liver.
Involves the breakdown of lipids in a process called lipolysis
Lipogenesis
A process where excess glucose can also be converted into fat.
Role of the pancreas
Contains islets of Langerhans – hormone secreting cells. Two types:
-Alpha cells: Secrete glucagon = increase blood sugar.
-Beta cells: Secrete insulin = decrease blood sugar.
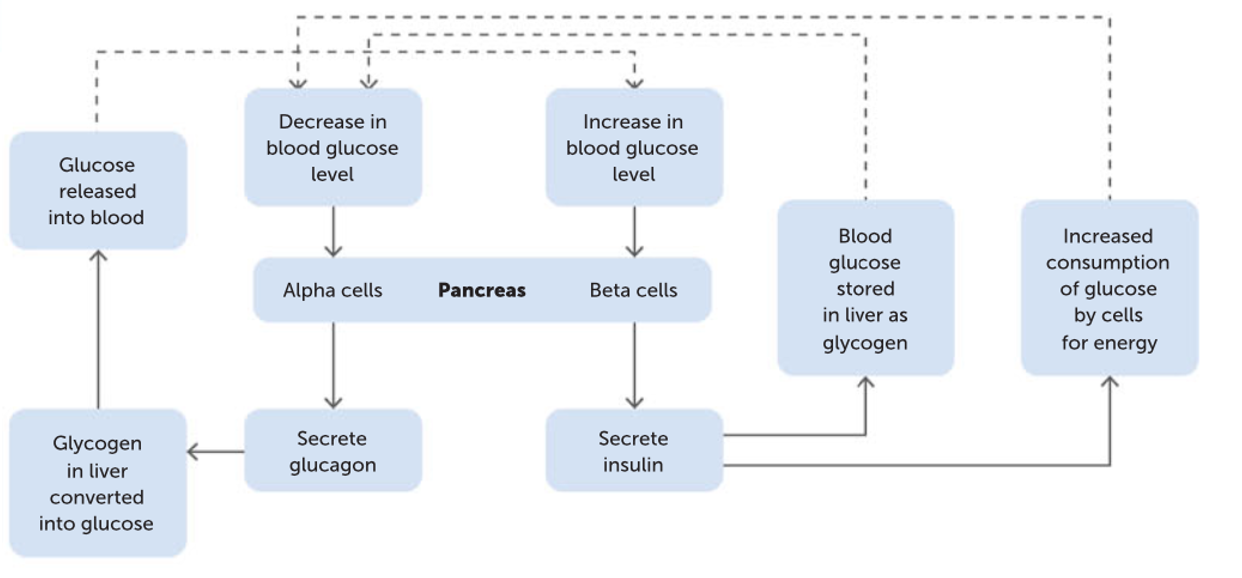
Role of the pancreas: low blood glucose
Stimulus – low blood glucose levels.
Receptor – chemoreceptors in the alpha cells of the islets of Langerhans.
Modulator – Alpha cells in the islets of Langerhans secrete glucagon.
Effector - Promotes glycogenolysis and gluconeogenesis in the liver.
Response– blood glucose levels increase.
Feedback – negative
Role of the pancreas: high blood glucose
Stimulus– high blood glucose levels
Receptor– chemoreceptors in the beta cells of the islets of Langerhans
Modulator– Beta cells in the islets of Langerhans secrete insulin
Effectors- promotes entry of glucose into cells
- promotes glycogenesis in liver and muscles
- promotes fat storage (lipogenesis)
- promotes protein synthesis
Response – decrease in bloods glucose levels
Feedback- negative
Pancreas feedback loop
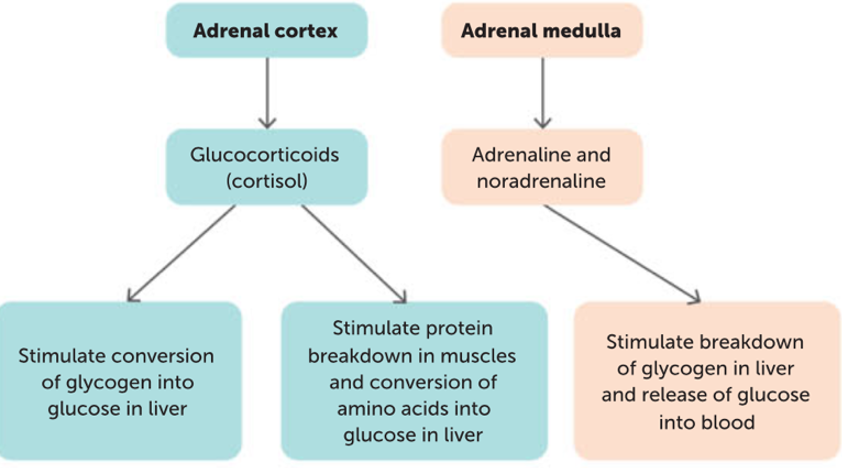
Adrenal glands
Above the kidneys, composed of 2 parts:
-The outer adrenal cortex
-The inner adrenal medulla
Produces the hormone glucocorticoids by the cortex, and adrenaline and noradrenaline by the medulla.
Adrenal cortex
Stimulated to secrete hormones by adrenocorticotropic hormone (ACTH) from the anterior pituitary gland. The hormones secreted are glucocorticoids, including cortisol:
-Regulates carbohydrate metabolism ensuring energy is provided to cells
-Stimulates glycogenolysis
-Increase the rate of gluconeogenesis
- Promote the mobilisation of fatty acids from adipose tissue
-Allows muscle cells to shift from using glucose to fatty acids for metabolic energy.
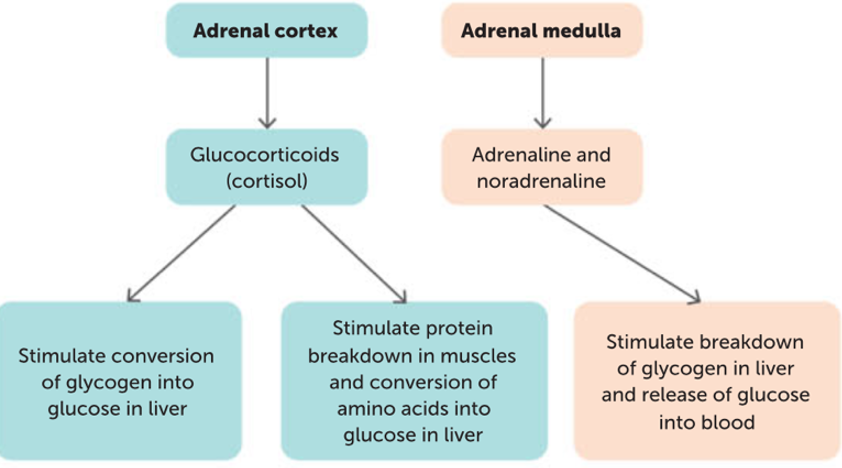
Adrenal medulla
Secretes adrenaline and noradrenaline, hormones that produce the same effects as the SNS. This includes increase of blood glucose (glycogenolysis) and counteracts the effects of insulin. Stimulates the production of lactic acid from glycogen in muscle cells where they can be used by the liver to manufacture glucose.
Blood glucose homeostasis
Normal glucose in blood is between 4-6 millimoles per liter. Equal to 90mg/100mL. Blood glucose homeostasis relies on the contribution of the liver, pancreas and adrenal glands, working in an integrated manner.
Thermoregulation
The regulation of body temperature to keep the body’s core temperature within its tolerance limits.
Body temperature tolerance limits
Set-point for is around 36.8°C with tolerance limits around 36.5 to 37.5 °C. Optimum for cellular reactions (enzyme function)
Hypothermia
Temperature less than 35 °C. The metabolic rate is so low that heat production is unable to replace the heat lost and body temperature continues to fall.Can cause death
Hyperthermia
Temperature above 37.5. Affects cells as it can cause protein degeneration (enzymes) and cell death. When the temperature and humidity are high, it is difficult for the body to lose heat by radiation or evaporation. Body temperature rises and the regulatory mechanisms cease = heat stroke.
Heat exhaustion: Extreme sweating and vasodilation to lose heat. Loss of water in sweating reduces the volume of blood plasma and vasodilation reduces resistance to blood flow. Blood pressure is reduced and output of blood from the heart decreases
Heat production
A constant human body temperature is achieved by a balance between heat gain (input) and heat loss (output)
During exercise and strenuous activity, the increase in metabolic rate generates more heat than is needed. Carbs, proteins and lipids we eat contain energy in the form of chemical bonds, and energy is released in the form of heat during cellular respiration.
Metabolic rate
The rate at which energy is released by the breakdown of food.
Increases when stressed due to noradrenaline increasing cell activity. For each1º C increase in temperature, the rate of biochemical reactions increases by 10%.
Central thermoreceptors
Located in the hypothalamus. Detect the temperature of the internal environment.
Peripheral thermoreceptors
Found in skin and some mucous membranes. Detect temperature changes in the external environment. Sends information to the hypothalamus. 2 types:
Cold receptors: sensitive to temperatures cooler than the neutral skin temperature. Found in higher concentrations in the skin than warm receptors as they are needed to survive when we are cold.
Warm receptors: sensitive to temperatures warmer than neutral skin temperature. Found in deep tissues (e.g muscle and viscera).
Role of the Skin in Temperature Regulation
About 85% of excess body heat is lost through the skin. Changes in the skin can speed up or slow down the rate at which heat is lost from the body
Methods of heat transfer
Conduction
Convection
Radiation
Evaporation
Conduction
Transfer of heat by direct contact between particles.
Heat is transferred from particle to particle, results in heat gain or heat loss. Eg sitting on a metal seat/slide
Convection
The transfer of heat by the movement of a liquid or a gas (a fluid).
Occurs when the fluid is heated and becomes less dense and moves away taking the heat with it, results in heat gain or heat loss. Eg The use of a fan
Radiation
The transfer of heat by infrared radiation being emitted by objects.
No direct contact with source and energy is transferred in waves. Can result in heat gain or heat loss. Eg Radiation from the sun
Evaporation
The process of a liquid forming a gas, which absorbs heat energy.
This requires energy which results in cooling, results in heat loss only. Eg sweating
Preventing Body Temperature from Falling
If cold receptors are stimulated they send a message to the hypothalamus and it brings about changes so body temperature is maintained by:
-Reducing heat loss
-Increasing heat production
The body can respond by:
- Physiological changes (changes in body functioning)
- Behavioral changes (conscious changes)
Reducing heat loss body responses
PHYSIOLOGICAL:
Vasoconstriction
Reduction in sweating
BEHAVIOURAL:
Conscious changes
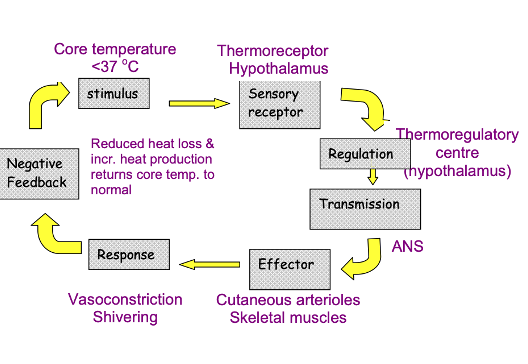
Preventing Body Temperature from Falling: Physiological changes: Vasoconstriction
Arterioles in the skin carry heat from the core of the body. When low temperatures are detected, the hypothalamus sends messages to smooth muscle surrounding arterioles, causing them to constrict, reducing blood flow and reducing heat transfer from the skin.
Peripheral vasoconstriction also decreases heat loss due to heat transfer in the extremities.
Preventing Body Temperature from Falling: Physiological changes: Reduction in sweating
The evaporation of sweat uses energy and cools the body so a decrease in sweating decreases heat loss.
Preventing Body Temperature from Falling: Behavioural changes
Putting on a more clothing.
Sheltering from the wind.
Curling up into a ball to reduce surface area so less area for heat exchange to occur.
Eating/drinking warm food.
Increasing heat production body responses
PHYSIOLOGICAL
Increase of metabolic rate (adrenal medulla)
Increase of metabolic rate (thyroid gland)
Shivering
BEHAVIOURAL
Increased voluntary activity
Increasing heat production: Physiological changes: Increase of metabolic rate (adrenal medulla)
Stimulation by sympathetic nerves releases adrenaline and noradrenaline. Brings about an increase in cellular respiration which leads to an increase in heat production. Useful when there is rapid heat loss
Increasing heat production: Physiological changes: Increase of metabolic rate (Thyroid gland)
Hypothalamus causes anterior pituitary to release more TSH. Thyroid releases more thyroxine into the blood, increasing metabolic rate resulting in greater heat production. Slower to have an effect but longer lasting.
Increasing heat production: Physiological changes: Shivering
A reflex triggered in response to low temperatures. Skeletal muscles produced rhythmic muscle tremors that occur at a rate of around 10 to 20 contractions per second. Increased muscular activity results in the generation of heat as a byproduct. The heat produced by the muscles is released as heat.
Increasing heat production: Behavioural changes: Increased voluntary activity
Running on the spot
Rubbing hands together
Preventing Body Temperature from Rising
When the weather is warm or when we exercise, the heat produced by metabolism is greater than needed and must be lost from the body by increasing heat loss or by decreasing heat production
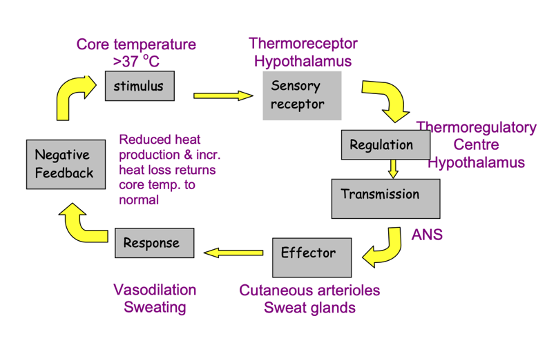
Increasing heat loss body responses
PHYSIOLOGICAL
Vasodilation
Sweating
BEHAVIOURAL
Conscious changes
Increasing heat loss: Physiological: Vasodilation
Dilation of arterioles in the skin increases blood flow to the skin’s surface. Skin becomes red, surface temperature rises and there is greater heat loss through radiation and convection
Increasing heat loss: Physiological: Sweating
Liquid sweat absorbs heat from the body so that it can be vaporized (turned into a gas). As the sweat absorbs heat from the body, the body cools down. Sweating is only effective in environments that are dry.
Increasing heat loss: Behavioural
Removing clothing
Turning on a fan
Increasing surface area by spreading out to increase the area that heat can be lost from
Decreasing heat production body responses
PHYSIOLOGICAL
Decreased metabolic rate
-Bought on by the reduction of the hormone thyroxine from the thyroid gland. A long-term response.
BEHAVIOURAL
-Decreased voluntary activity.
Main role of water in the body
Transporting substances from one area to another
Facilitating movement across membranes
Being the site of chemical reactions
Makes up around 50% of adult mass for females and 60% in males.
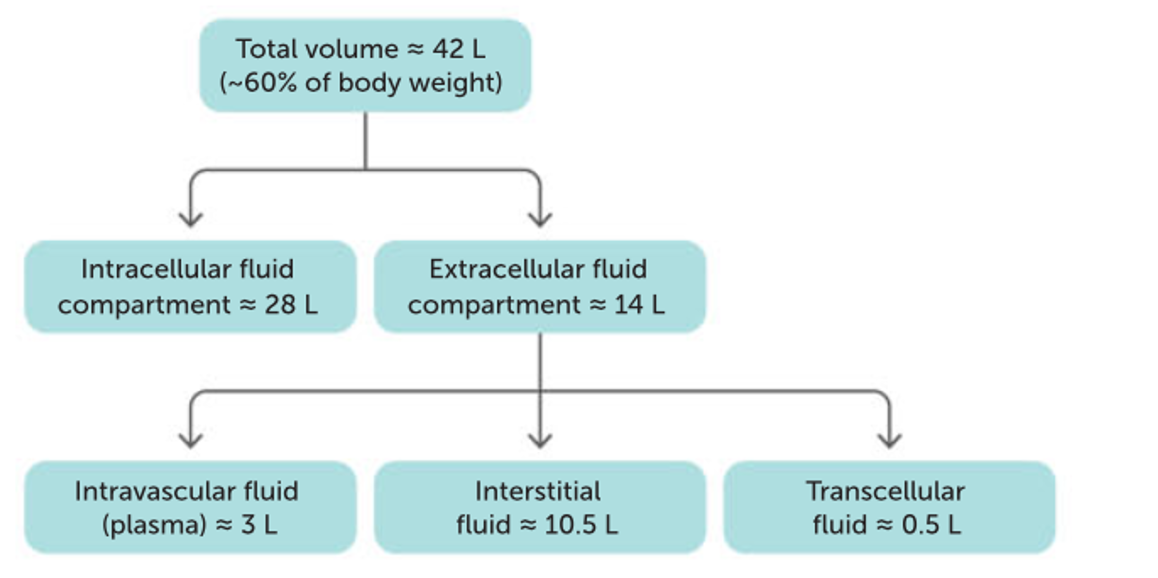
Distribution of body fluid
Extracellular fluid includes:
-Intravascular fluid: Blood plasma within blood vessels.
-Interstitial /tissue fluid: Fluid between cells.
-Transcellular fluid: Fluid in specific body regions
Osmosis
The movement of water from an area of high-water concentration to a region of low water concentration. Allows water to move through plasma membranes.
Plasma is separated from the interstitial fluid by capillary walls, and there’s a relatively free exchange of materials. Osmotic concentration difference between intracellular and extracellular fluid don’t last long.
Osmotic pressure
The tendency of a solution to take in water.
The greater the difference in osmotic concentrations between two solutions, the greater the osmotic pressure.
LOW OSMOTIC PRESSURE: A low salt and a high-water concentration
HIGH OSMOTIC PRESSURE: A high salt and a low water concentration.
Body fluid concentrations need to be maintained to maintain osmotic pressure so that cells can receive nutrients and get rid of wastes
Exchange of nutrients and wastes
Takes place between the intravascular fluid and the interstitial fluid. At the arterial end of the capillary there is a mass flow of plasma and nutrients from the bloodstream into the interstitial fluid because blood pressure is greater than osmotic pressure. At the venous end of the capillary there is a mass flow of tissue fluid containing wastes into the blood stream because the blood pressure is less than the osmotic pressure.
Maintaining fluid balance and metabolic water
Fluid gain must equal fluid loss if the composition of body fluids is to be kept fairly constant. Most body fluid is obtained from water that is either taken in as a liquid or contained in food.
Metabolic water: A small amount of water obtained as a by-product of respiration within cells.
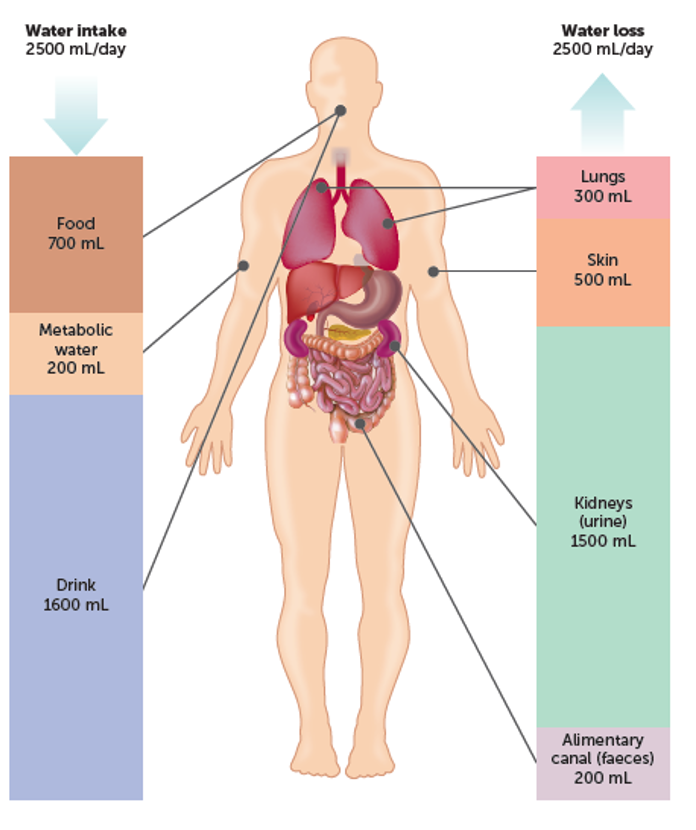
Excretion
The removal of the waste products of metabolism from the body.
Lungs: carbon dioxide.
Sweat glands: water with by-products of metabolism - salts, urea, lactic acids.
Kidneys: urea.
Kidneys
The ureter leaves each one and drains into the urinary bladder which empties through the urethra. Only water loss from the kidneys can be regulated to achieve a constant concentration of dissolved substances in the body fluids. Play a major role in regulating the composition of body fluids.
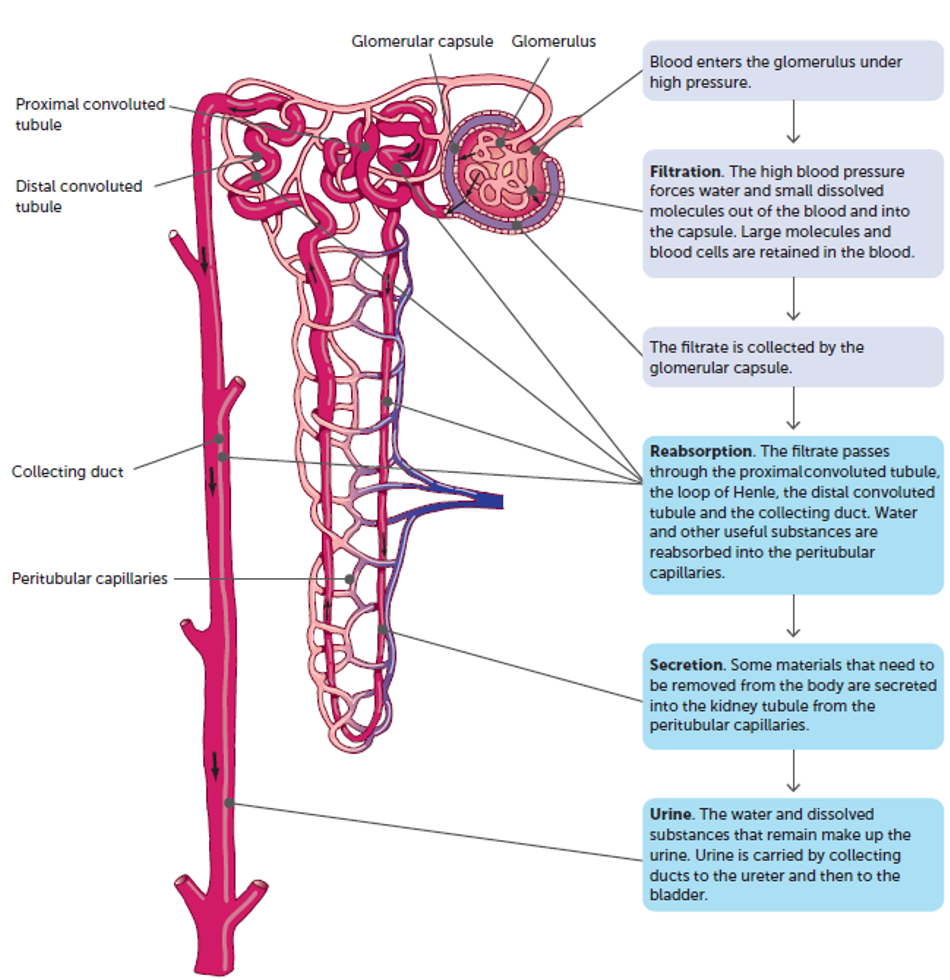
Kidney: Nephrons
Each kidney contains about 1.2 million microscopic units called nephrons.
The nephrons are the functional units of the kidney and carry out its role in excretion and water regulation
Urine formation stages
The water dissolves substances that remain make up the urine. The concentration of the urine can be altered depending on the water concentration in the body.
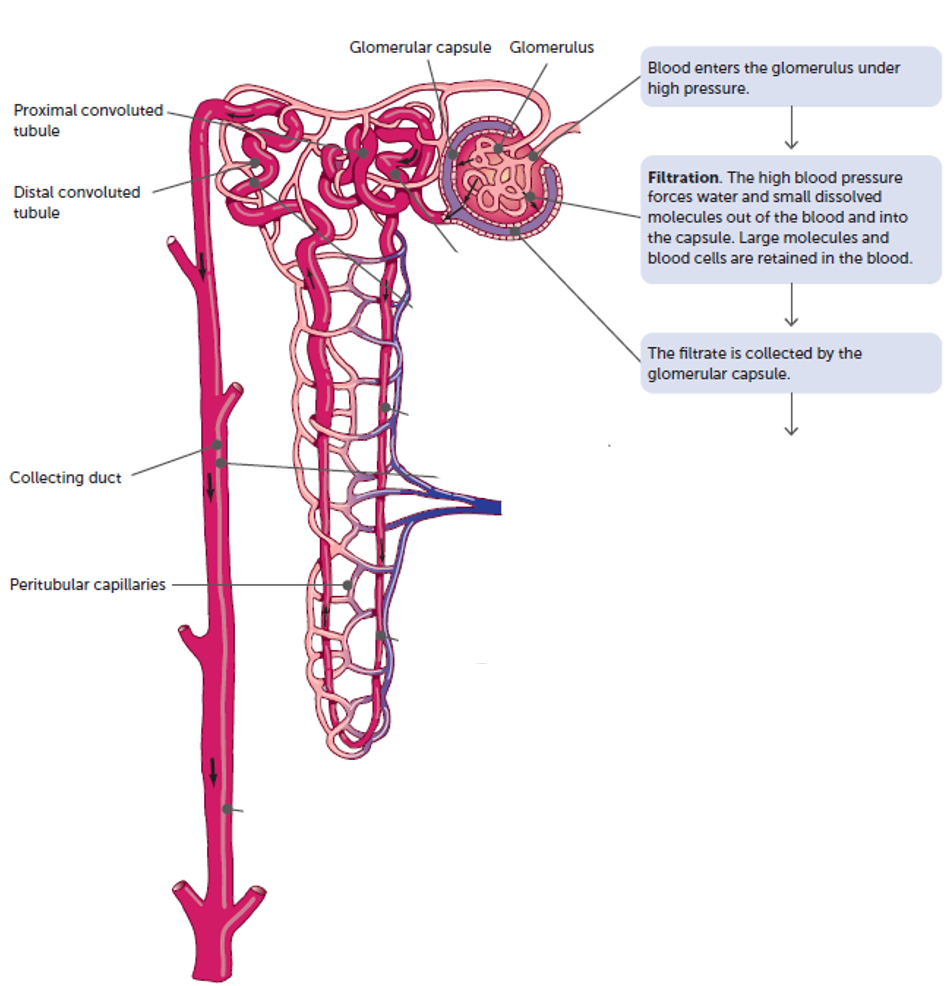
Filtration
Selective reabsorption
Tubular secretion
Kidneys: Urine formation: Step 1
Filtration.
Occurs in the renal corpuscle
High blood pressure forces water and small dissolved molecules out of the blood and the filtrate is collected by the glomerular capsule.
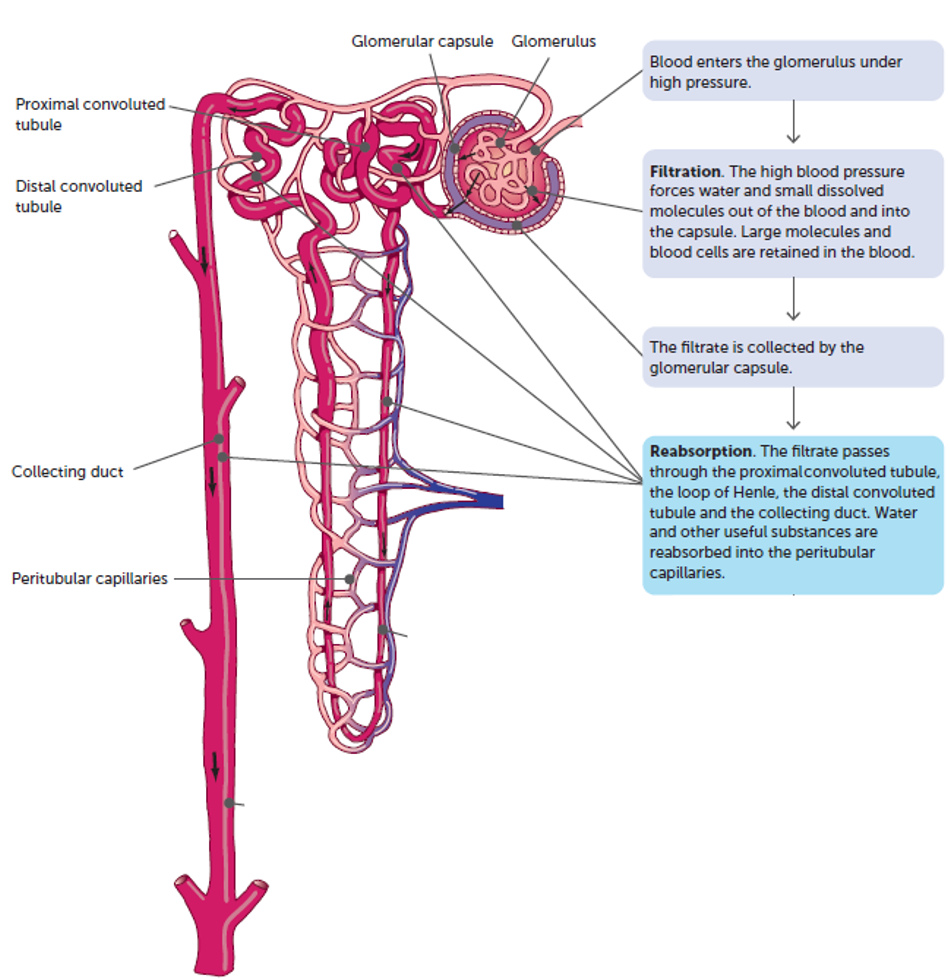
Kidneys: Urine formation: Step 2
Selective reabsorption.
Occurs in the proximal convoluted tubule, loop of Henle, distal convoluted tubule and collecting duct
Water and other useful substances are reabsorbed back into the bloodstream via the peritubular capillary network that surrounds the nephron
Kidneys: Urine formation: Step 3
Tubular secretion.
Some materials such as drugs and some ions that need to be removed from the body are actively secreted into the kidney tubule from the peritubular capillaries
Controlling water levels
As water is lost, the plasma becomes more concentrated and has a higher osmotic pressure, causing water to move from the interstitial fluid into the plasma by osmosis. Osmoreceptors in the hypothalamus detect this, and then responses are triggered to increase water content and lower osmotic pressure
Hormonal control of fluid regulation: Kidneys: Antidiuretic hormone
~99% of water water filtrated through the glomeruli in the nephron in the kidneys is reabsorbed.
Passive reabsorption through osmosis: proximal convoluted tubule and Loop of Henle.
Active reabsorption : distal convoluted tubule (DCT) and collecting tubule/duct
The level of active reabsorption is controlled by the hormone ADH (antidiuretic hormone). Produced in the hypothalamus and released from the posterior pituitary and controls the permeability of the walls of the DCT and collecting duct.
Kidneys: Hormonal control: Antidiuretic hormone: increased ADH
Response to low plasma water levels.
Causes increases permeable of kidney tubules to water. Water leaves tubules and enters capillary networks (bloodstream), decreasing osmotic pressure of blood.
Decreased water in kidney tubules = increased concentration of materials remaining (more concentrated urine)
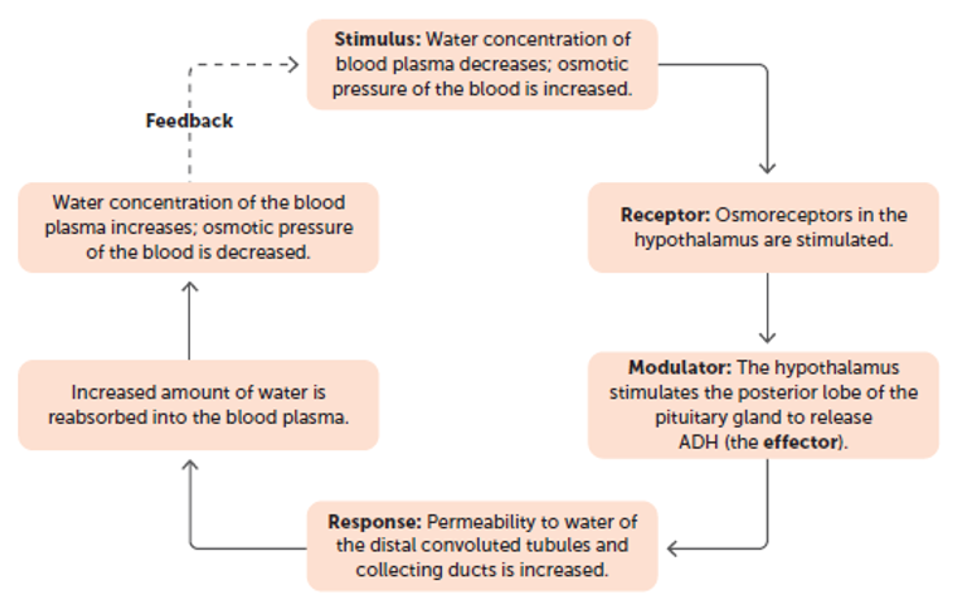
Hormonal control of fluid regulation: Kidneys: Antidiuretic hormone: Decreased ADH
Response to high plasma water levels
Causes decreased permeable of kidney tubules to water. Less water leaves tubules and enters capillary networks (bloodstream). Decrease in water concentration in the blood so increased osmotic pressure of blood
Increased water in kidney tubules = decreased concentration of materials remaining (more dilute urine)
Hormonal control of fluid regulation: Kidneys: Aldosterone
Secreted by the adrenal cortex in response to:
-Decrease in concentration of sodium ions in blood
-Decrease in blood volume
-Decrease in blood pressure
- Increase in the concentration of potassium ions in the blood.
Acts on DCT and collecting ducts to increase the amount of sodium ions reabsorbed into the bloodstream and the amount of potassium ions secreted into the urine. Using the sodium-potassium pump there is a net movement of ions into the blood.
-Water then moves into the blood via osmosis
- Increases water level in the blood/decreases osmotic pressure.
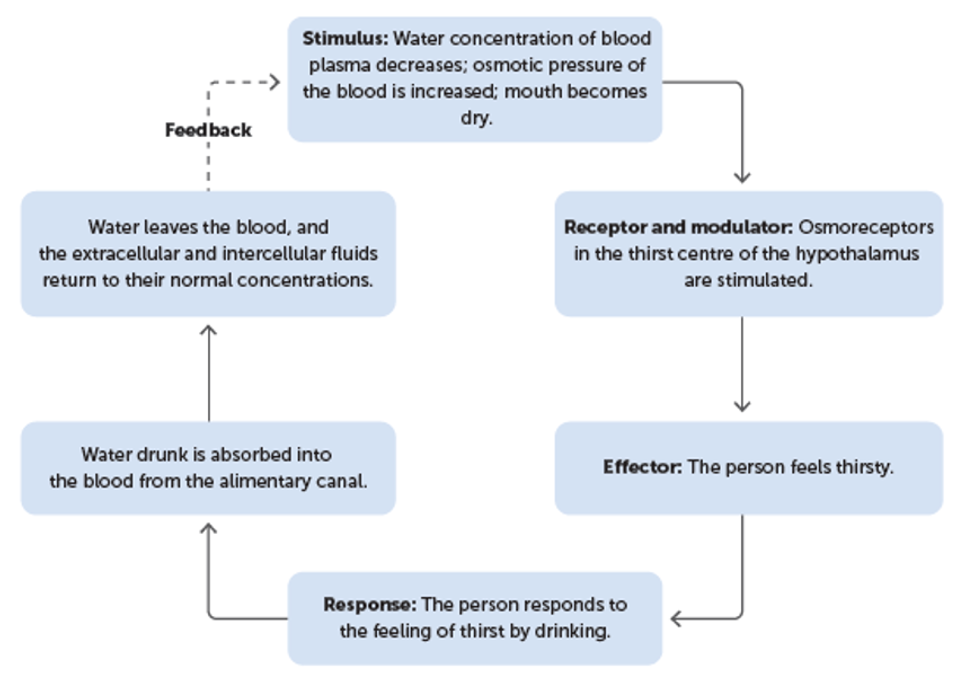
Nervous control of fluid regulation: Thirst response
In addition to regulating water loss in urine, the level of water in the body can be increased by taking in more fluid. It is a conscious response in which a person response to a feeling of thirst.
Osmoreceptors stimulate the thirst center in the hypothalamus, prompting a person to drink water.
Too little water – dehydration
Occurs when water loss exceeds water intake. Symptoms become noticeable when a person has lost ~2% of their normal body water, including severe thirst, low blood pressure, dizziness and headache.
On a cellular level, the low levels of water in the extracellular environment causes water to move out of the cells due to osmosis, causing them to shrink.
Too much water – water intoxication
On a cellular level, excessive levels of water in the extracellular environment causes water to move into the cells due to osmosis, causing them to swell
Symptoms include lightheadness, headaches, vomiting and collapse may follow.
Regulation of gas concentrations
All cells need a constant supply of oxygen for respiration so it must be maintained at a certain level. Carbon dioxide is produced in respiration and needs to be removed from the body
Oxygen + Glucose → Carbon dioxide + water + energy
Respiratory system
Involved with the exchange of gases and the circulatory system with their transport.
Respiratory skeletal muscles - the diaphragm and the intercostal muscles - cause air to move in and out of the lungs, and need nerve impulses to initiate their contraction.
Diaphragm: stimulated by impulses from the phrenic nerve.
Intercostal muscles: stimulated by impulses from the intercostal nerve.
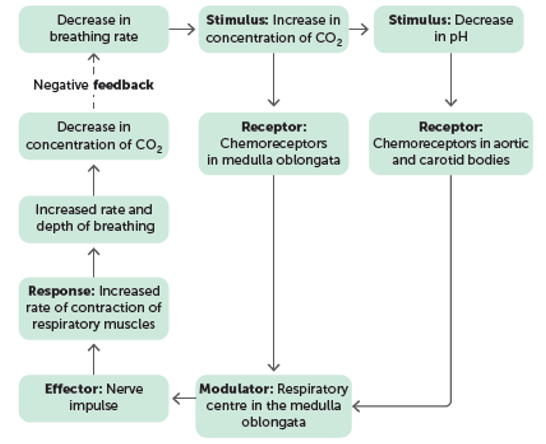
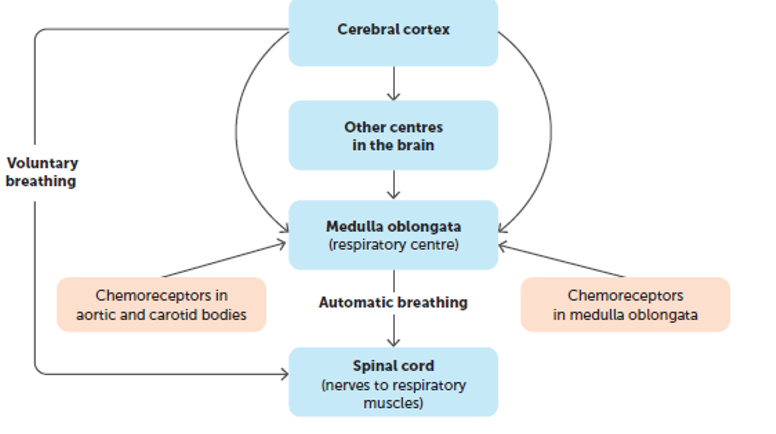
Respiratory center
Respiratory centre: controls the nerve impulses that travel to the diaphragm and intercostal muscles. Located in the medulla oblongata. Two regions that control
- Expiration: Expiratory center
-Inspiration: Inspiratory center
Peripheral chemoreceptors
Groups of cells within the walls the aortic and carotid bodies.
Sensitive to changes in the concentration of oxygen, carbon dioxide (CO2) and hydrogen ions in the blood plasma
Central chemorecpetors
Located in the medulla oblongata
Sensitive to changes in the concentration of CO2 in the blood and hydrogen ions in the CSF (Cerebrospinal fluid)
Most sensitive to CO2 concentration changes. 70-80% responsible for changes caused by increase of CO2.
Chemicals affecting breathing: Oxygen
Under normal circumstances levels of oxygen plays a little part in changing breathing rate. If concentration decreases to very low levels breathing rate will increase.
Stimulus - very low oxygen levels
Receptor – peripheral chemoreceptors
Modulator – respiratory centre in medulla oblongata sends nerve impulse along the phrenic nerve to the diaphragm and the intercostal nerve to the intercostal muscles
Effector – respiratory muscles increase the rate and depth of breathing
Response – increase gas exchange
Feedback – Increased levels of oxygen (Negative feedback)
Chemicals affecting breathing: Carbon Dioxide
CO2 concentration is the major factor in the regulation of gas concentrations. Small increases can increase breathing rate.
Stimulus –high carbon dioxide levels
Receptor – central chemoreceptors
Modulator – respiratory centre in medulla oblongata sends nerve impulse along the phrenic nerve to the diaphragm and the intercostal nerve to the intercostal muscles
Effector – respiratory muscles increase the rate and depth of breathing
Response – increase gas exchange
Feedback – decreased levels of carbon dioxide (Negative feedback)
Chemicals affecting breathing: Hydrogen ions
When carbon dioxide dissolves in the blood, it forms carbonic acid, which breaks down readily to form bicarbonate ions and hydrogen ions. Takes several minutes. An increase in the concentration of CO2 in the plasma causes an increase in H+. As H+ concentration increase, pH decreases, which stimulates chemoreceptors in the aortic and carotid bodies. Produces an immediate increase in breathing rate
Voluntary control of breathing
Humans can control their rate and depth of breathing.
Important for speech and as a protective device preventing irritating gases and water entering lungs. Comes via connections from the cerebral cortex to descending tracts in the spinal cord. Bypasses the respiratory center in the medulla oblongata
Holding our breath
Buildup of CO2 stimulates the inspiratory center of the medulla oblongata to send impulses to the respiratory muscles. We are eventually forced to take a breath whether we want to or not. You can’t die on land by holding your breath but if your brain does not get enough oxygen you can lose consciousness. Then the respiratory centre is triggered to send impulses to the respiratory muscles and you take a breath.
Hyperventilation
Rapid, deep breathing that provides more oxygen than required and remove more CO2 than necessary.
More air is breathed out (exhaled) than breathed in (inhaling). Common after strenuous exercise or can be caused by severe pain or emotional stress, resulting in less CO2 in the blood. Can trigger vasoconstriction of blood vessels to the brain which can lead to a feeling of lightheadedness. Usually correct itself as the reduction in CO2 in the blood means chemoreceptors aren’t stimulated, reducing the rate and depth of breathing until CO2 levels return to normal.
Hyperventilation - Swimming
Dangerous if occurs before swimming underwater.
Can swim under water for longer. It takes longer for CO2 levels to increase to a point that triggers the need to breathe. Levels of oxygen decrease to very low levels due to oxygen being used for respiration. This causes a person to pass out before the urge to breathe. When a breath is triggered, water can be inhaled and can lead to disorientation and drowning.
Exercise and breathing
During exercise, the contracting muscle cells require late amounts of oxygen and produce large amounts of CO2. To respond to this increased demand for gas exchange, the respiratory system increases rate and depth of breathing. The volume of air going in and out of the lungs can increase 10-20x.