Celiac Trunk, Development of Midgut & Hindgut and their Derivatives
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
derivatives of foregut
-esophagus
-stomach
-liver
-gallbladder
-pancreas
-duodenum (only part proximal to entrance of the bile duct approximated by green line)
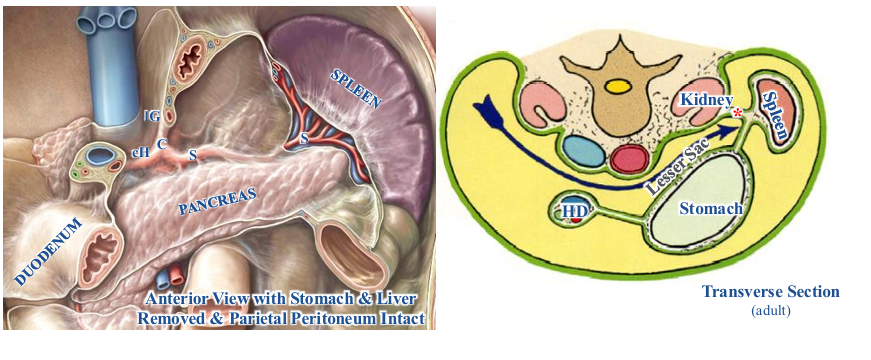
how do vessels and nerves get to GI tract?
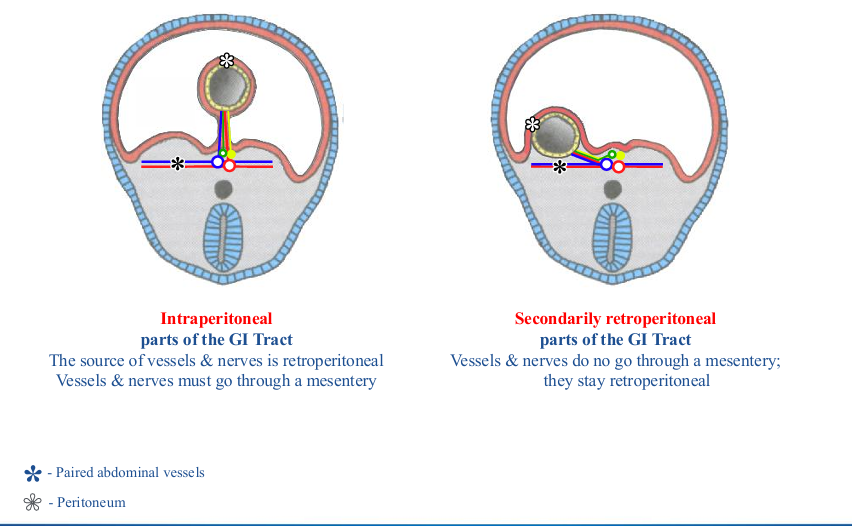
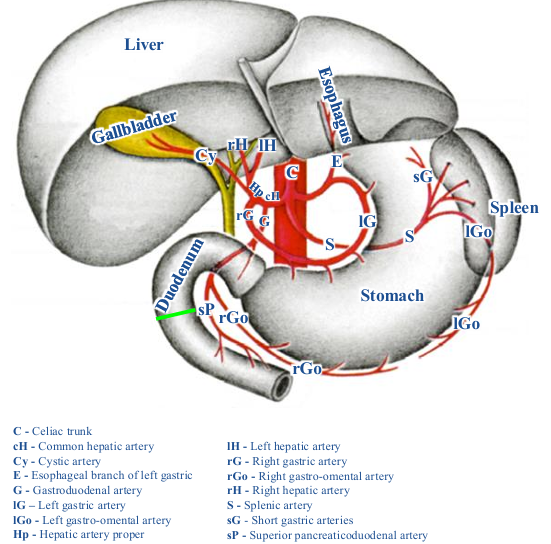
retroperitoneal vessels
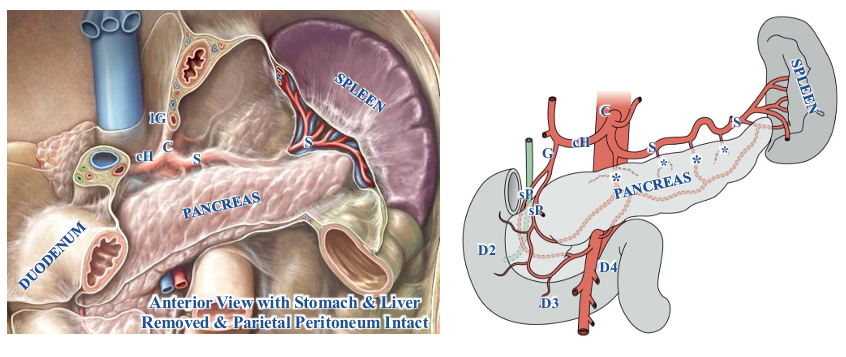
-abdominal aorta and celiac trunk are primarily retroperitoneal
-celiac trunk quickly trifurcates into common hepatic, splenic, and left gastric arteries
-all of some of the common hepatic, splenic, and left gastric arteries are initially retroperitoneal
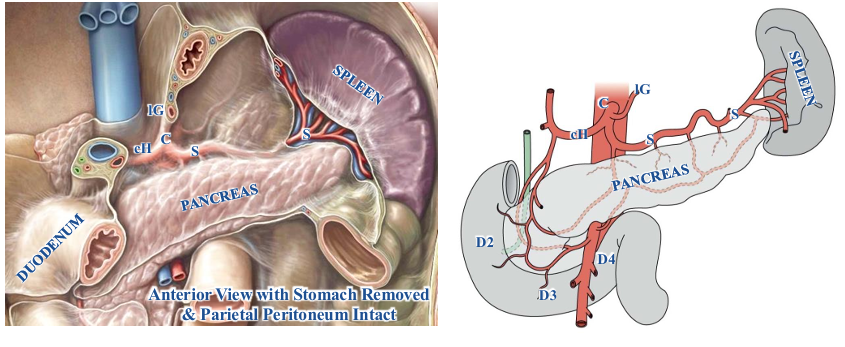
retroperitoneal vessels to secondary retroperitoneal organs
-secondarily retroperitoneal organs are supplied by arteries that stay retroperitoneal
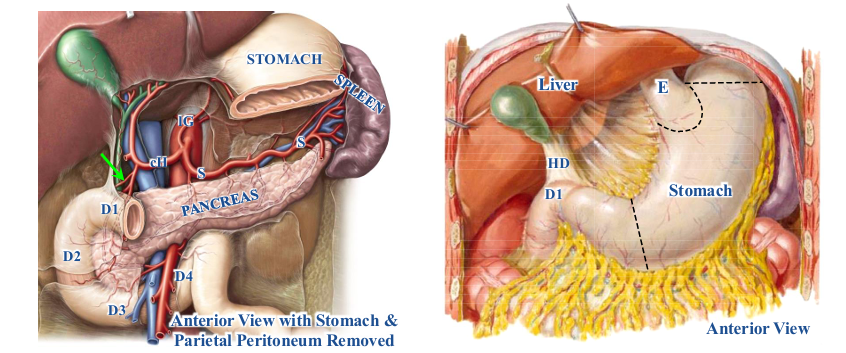
-duodenum (2nd, 3rd, and 4th parts) and pancreas (head and neck): supplied by superior pancreaticduodenal arteries (branches of gastroduodenal artery)
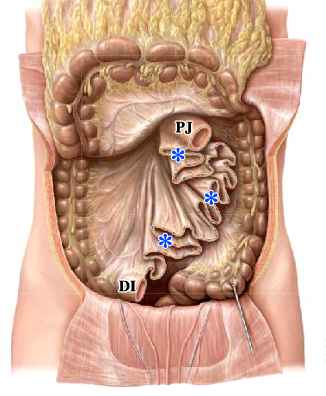
-pancreas (body): supplied by branches of splenic artery (asterisks)
retroperitoneal vessels to intraperitoneal organs- stomach
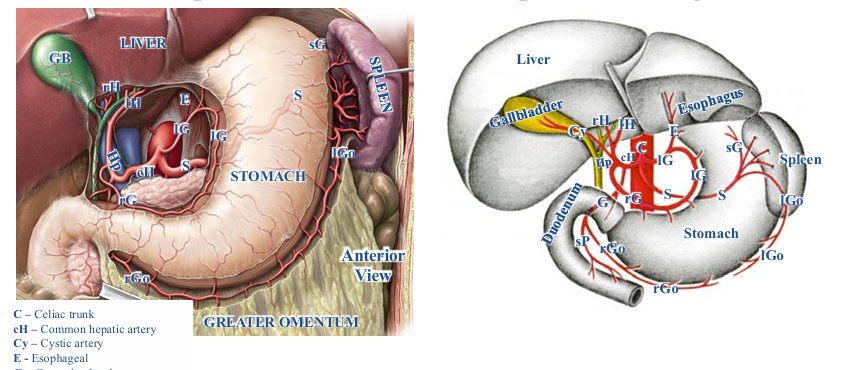
-intraperitoneal organs supplied by arteries that must go through a mesentery
-greater curvature- supplied by right and left gastro-omental arteries, branches of the gastroduodenal and splenic arteries respectively; right and left gastro-omental arteries go through greater omentum
-lesser curvature- supplied by right and left gastric arteries, branches of hepatic artery proper and celiac trunk; go through hepatogastric part of lesser omentum
-fundus- supplied by short gastric arteries, branches of splenic artery; go through the gastrosplenic ligament
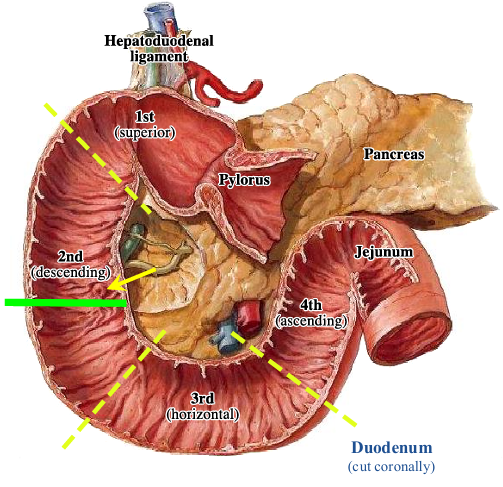
retroperitoneal vessels to intraperitoneal organs- duodenum (first part)
-supplied by supraduodenal artery (green arrow) that can be a branch of either the hepatic or gastroduodenal arteries that go through the hepatoduodenal ligament
retroperitoneal vessels to intraperitoneal organs- liver and gallbladder
-liver: supplied by right and left hepatic arteries, branches of the hepatic artery proper; all go through hepatoduodenal ligament (red arrows; part of lesser omentum) to reach the liver
-gallbladder: supplied by cystic artery (white arrow) that is usually a branch of the right hepatic artery; goes through the hepatoduodenal ligament (part of lesser omentum)
retroperitoneal vessels to intraperitoneal organs- spleen and pancreas
-spleen and pancreas (tail): supplied by splenic artery that goes through the splenorenal ligament (red asterisk)
venous drainage of foregut derivatives
-pattern of veins closely matches arteries with respect to drainage of esophagus, stomach, duodenum, pancreas, and spleen
-veins do NOT drain to inferior vena cava directly; they joint to form the hepatic portal vein
-veins draining intraperitoneal parts of gut also run through mesenteries to reach the portal vein
-portal vein goes through the hepatoduodenal ligament to reach the liver
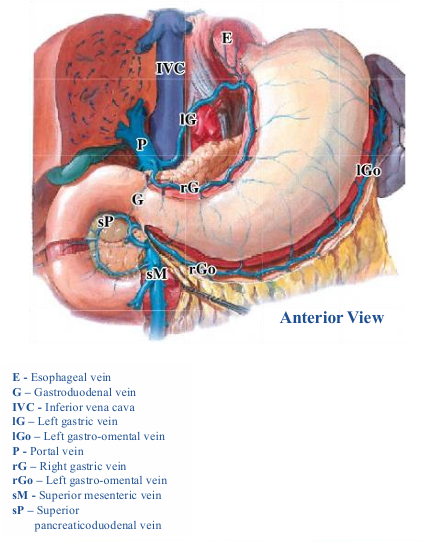
venous drainage of foregut derivatives- drainage
-all veins from foregut derivatives drain into the portal vein along with the blood from the midgut and hindgut derivatives
-usually, the inferior mesenteric vein drains into the splenic vein and the splenic & superior mesenteric veins joint to form the portal vein
-pattern is variable- inferior mesenteric vein may join at intersection of superior mesenteric and splenic veins
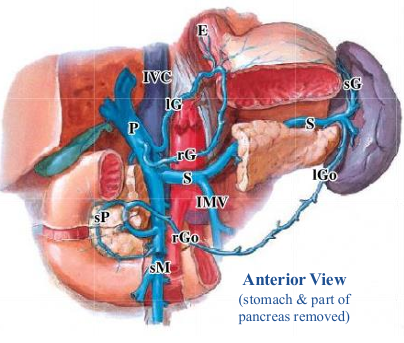
anatomical planes
-planes: a way to standardize locations in abdomen using the vertebral column as a ruler
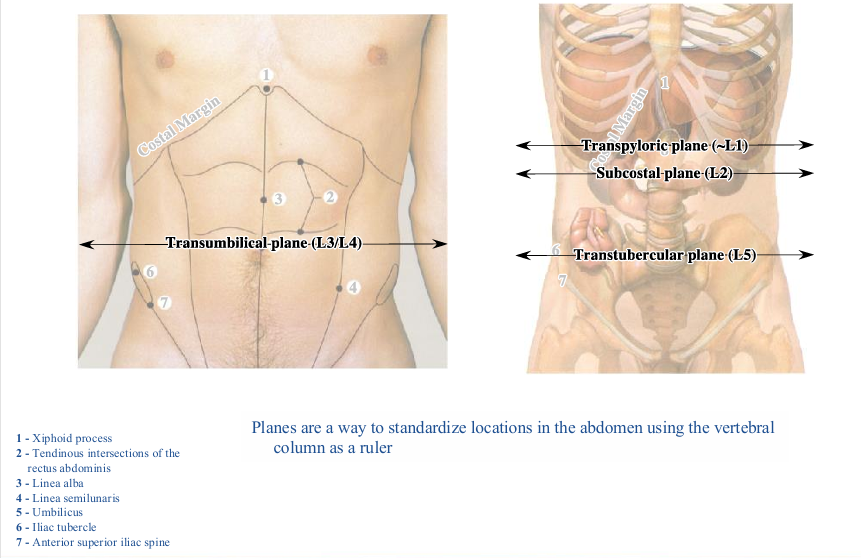
innervation of anterior abdominal wall
-skin of anterior abdominal wall supplied by anterior (A) and lateral (L) cutaneous branches of ventral rami of spinal nerves T7 through L1
-dermatome T10 at level of umbilicus
-downward trajectory of ventral rami of thoracic and lumbar spinal nerves explains why T10 dermatome includes the umbilicus yet the umbilicus is considerably inferior to T10 vertebrae and the transumbilical plane is at vertebral level L3/L4
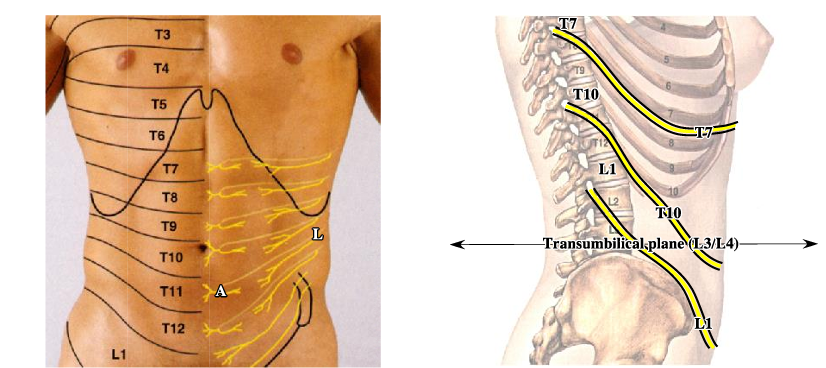
anatomical regions
-regions: used to describe the location of structures
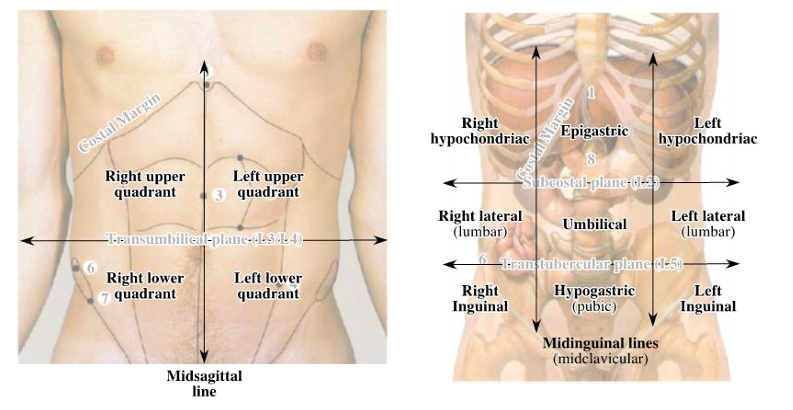
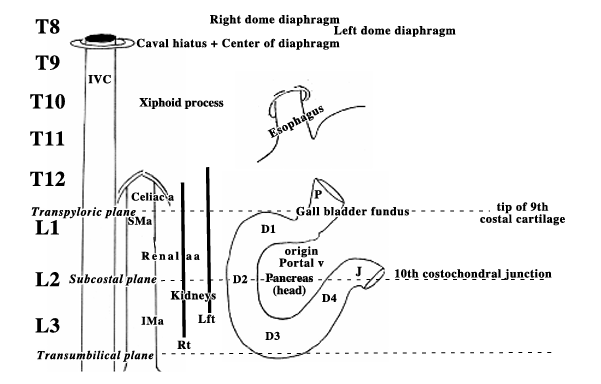
relationship of organs and vessels to vertebral column
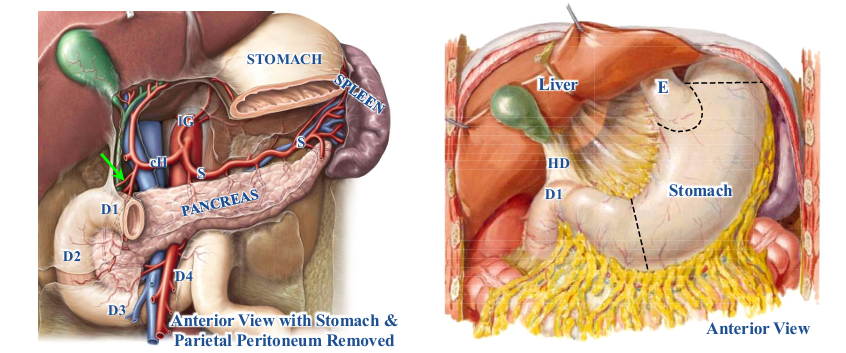
-structures at T10: esophageal hiatus, xiphoid process
-structures at T12: aortic hiatus, celiac trunk
-structures at L1: pyloric sphincter
blood supply of midgut and hindgut
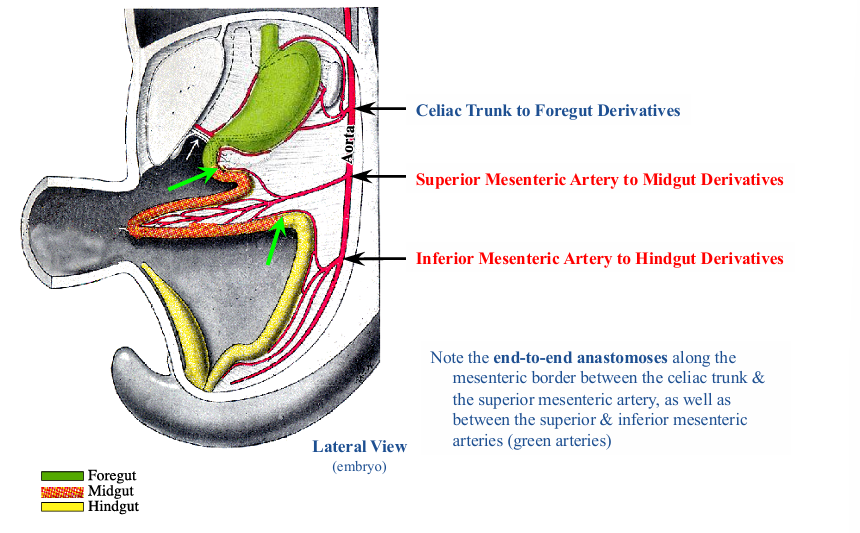
derivatives of midgut and hindgut
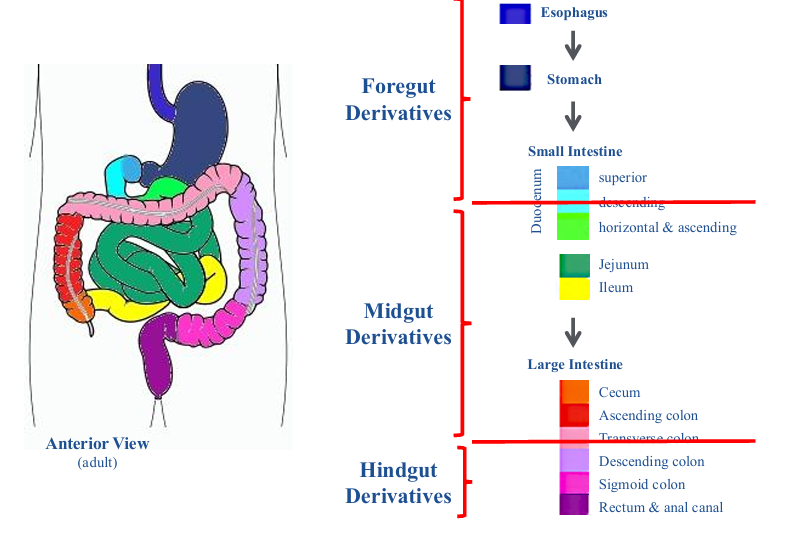
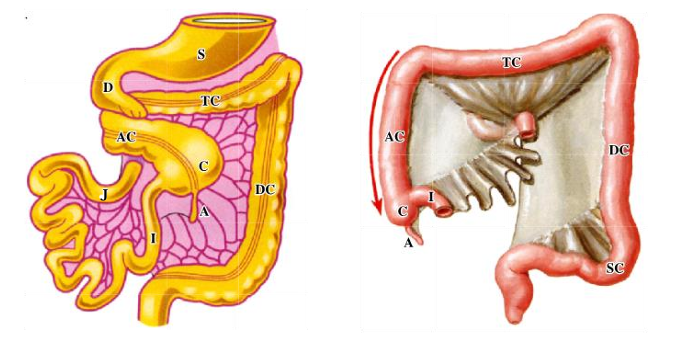
derivatives of midgut
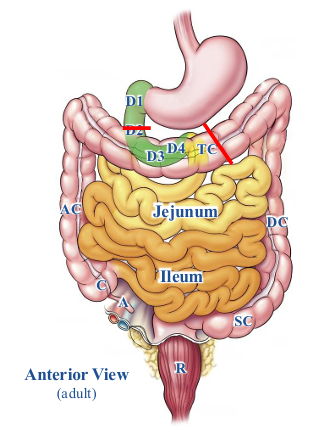
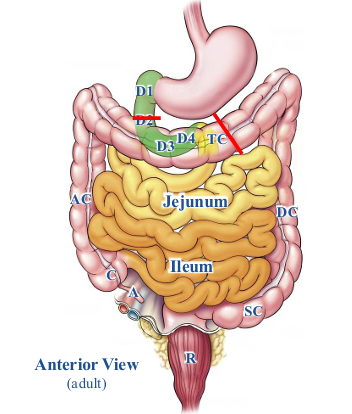
-duodenum (distal to entrance of bile and main pancreatic ducts; red line)
-jejunum and ileum
-cecum
-appendix
-ascending colon
-transverse colon (proximal 2/3; black line)
-secondarily retroperitoneal: duodenum and ascending colon
derivatives of hindgut
-transverse colon (distal 1/3; black line)
-descending colon
-sigmoid colon
-rectum
-anal canal (superior part)
-epithelium of bladder and urethra
-secondarily retroperitoneal: descending colon and rectum
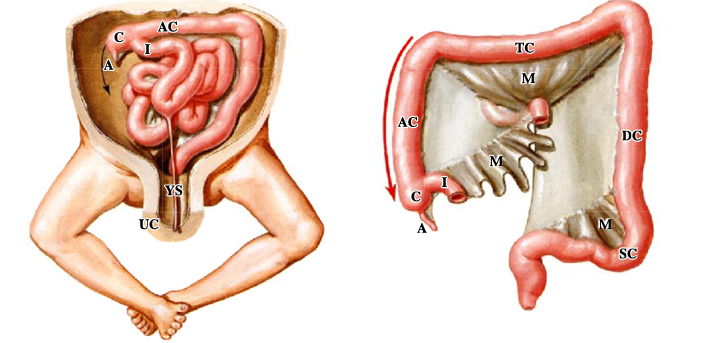
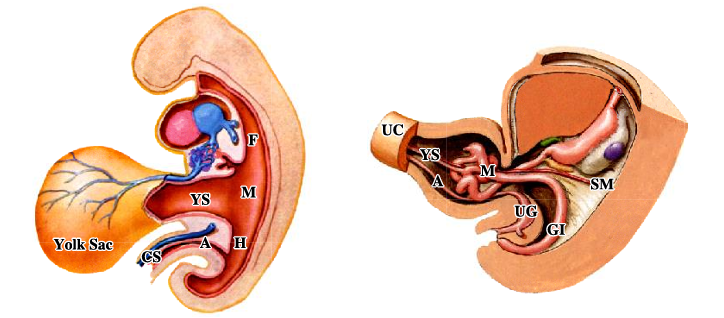
midgut development
-midgut: supplied by superior mesenteric artery, herniates into the umbilical cord during the embryonic period
-midgut returns to abdominal cavity early in the fetal period and rotates
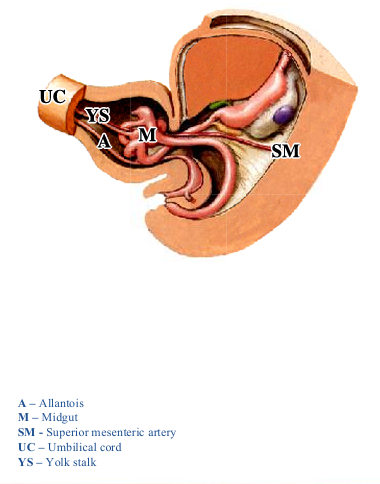
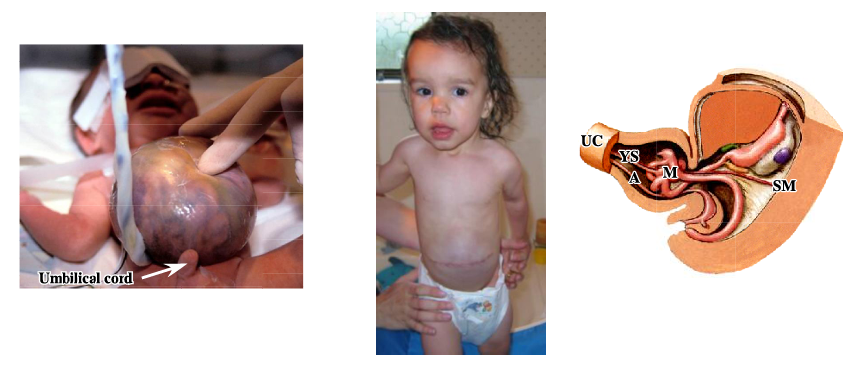
if midgut fails to return to abdominal cavity,
-baby is born with an omphalocele
-intestines are covered with a layer of parietal peritoneum
-occurs in 1 out of 5000 births
-following surgical repair, children do not have an umbilicus, but one can be made by a plastic surgeon
rotation of gut
-after midgut has returned to abdomen, both the midgut and hindgut derivatives rotate
-certain parts of gut fuse with the posterior abdominal wall resulting in secondarily retroperitoneal organs; process called fixation of gut
-jejunum, ileum, transverse colon, and sigmoid colon retain their mesentery
-ascending colon may attach to posterior wall before finishing its rotation in which case the cecum and appendix may remain in a subhepatic location
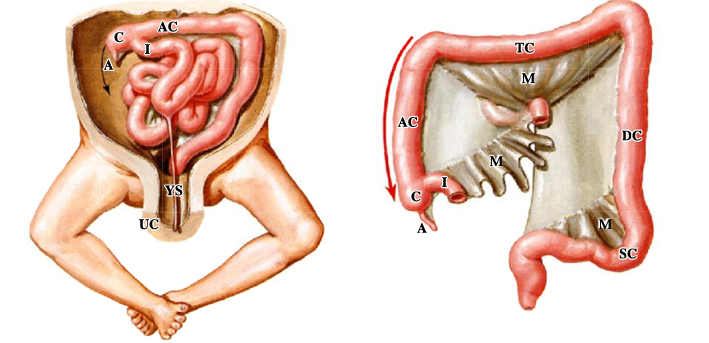
complications with rotation of gut
-improper rotation can result in volvulus (twisting) that can cause obstruction as well as a compromised blood supply resulting in ischemia and subsequent necrosis
-volvulus not only a developmental problem; can occur throughout life
congenital midgut abnormalities
-midgut returns to abdominal cavity, but the yolk stalk can persist resulting in a variety of congenital defects
A) mildest form: presence of an ileal (Meckel’s) diverticulum- NOT the appendix; present in approximately 2% of the population on the antimesenteric border of the ileum usually within 12 inches of the ileocecal junction
B) remnant of yolk stalk may still be attached to umbilicus
C) in the most problematic and rarest situations, the yolk stalk may still be patent providing egress for ileal contents
development of hindgut
-hindgut initially a single tube
-as development proceeds, hindgut becomes subdivided into anterior urogenital tube (future bladder and urethra) and a posterior gastrointestinal tube (distal 1/3 of transverse colon through superior anal canal)
-UG and GI tubes each have separate openings to the outside, the urethra and anal canal, respectively
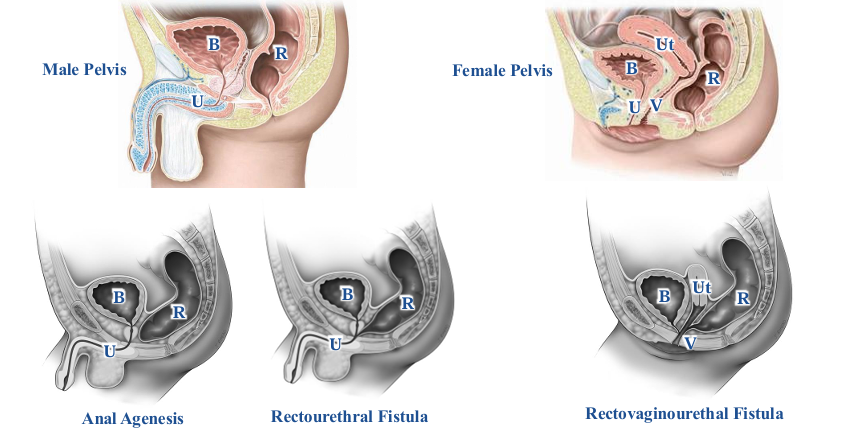
congenital hindgut abnormalities
-variety of congenital abnormalities that are a result of an incomplete subdivision of hindgut
-fistula = an abnormal connection between two hollow spaces
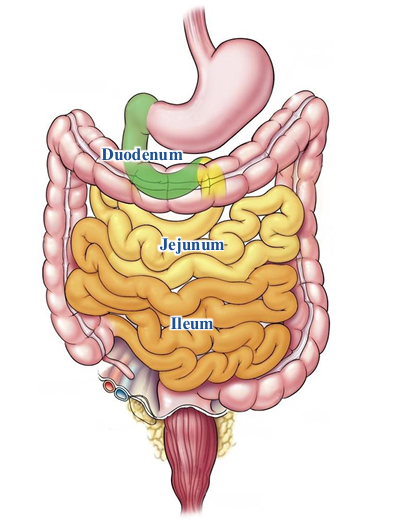
small intestines
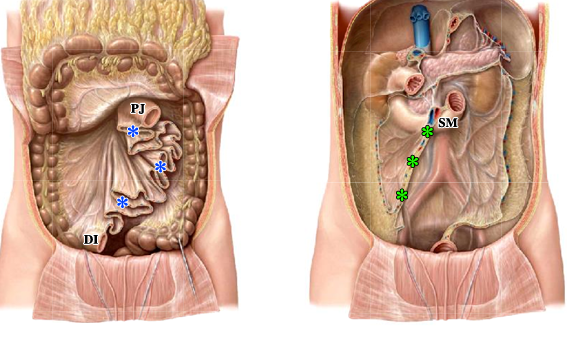
duodenojejunal junction
-foregut/midgut boundary (green line): just distal to entrance of bile duct, the major duodenal papilla (yellow arrow), within the 2nd (descending) part of duodenum
-2nd (descending), 3rd (horizontal), and 4th (ascending) parts of duodenum are all secondarily retroperitoneal
-4th (ascending) part of duodenum is continuous with the jejunum at the duodenojejunal junction
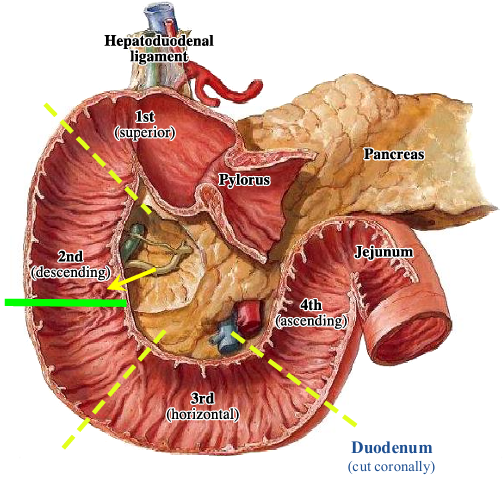
duodenojejunal junction tether
-tethered to body wall by band of skeletal tissue from the right crus of diaphragm, the suspensory ligament (of Treitz)
-duodenojejunal junction located at level of subcostal plane (L2)
-mesentery of jejunum begins at duodenojejunal junction (asterisk indicates torn mesentery)
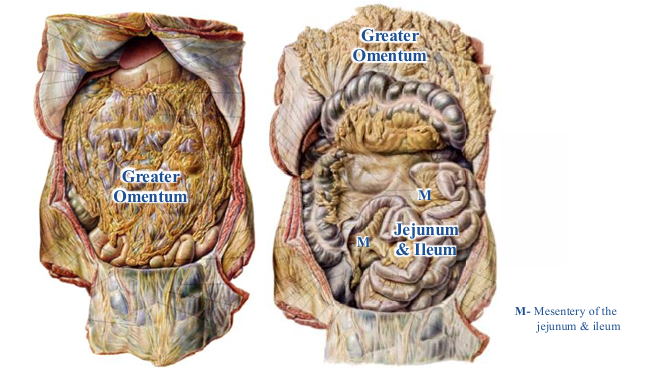
mesentery of jejunum and ileum
-must reflect greater omentum to see
-jejunum and ileum intraperitoneal because they are suspended by a mesentery for their entire length
-mesentery of jejunum and ileum also referred to as “the” mesentery- vessels and nerves run through it
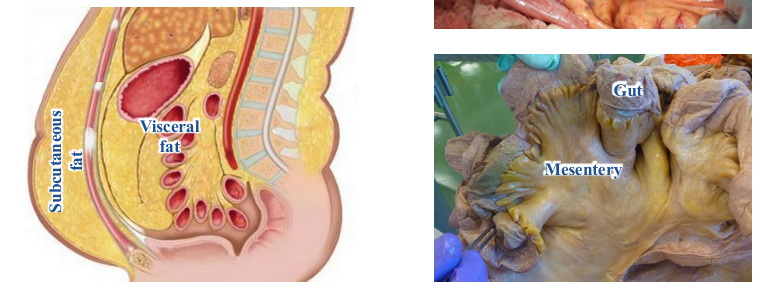
jejunum and ileum mesenteries- vessels and fat
-vessels can be seen in mesentery of individual with a minimal amount of visceral fat
-subcutaneous and visceral fat differ significantly
-subcutaneous fat produces a higher proportion of beneficial molecules (leptin and adiponectin) and visceral fat a higher proportion of molecules with potentially deleterious health effects (cytokines, precursor to angiotensin and retinol-binding protein 4)
characteristics of jejunum and ileum
-difficult to distinguish jejunum from ileum unless looking at proximal jejunum or distal ileum
-jejunum and ileum approximately 15-20 feet in length
-jejunum compromises proximal 2/5, ileum the distal 3/5
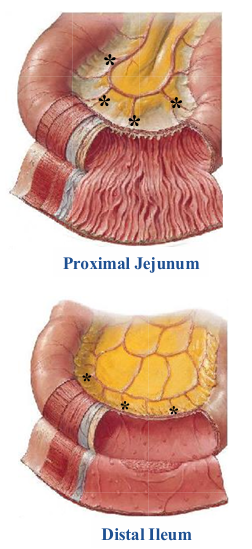
proximal jejunum v. distal ileum
-proximal jejunum: has a thick wall, many circular folds of its mucosa, relatively long straight arteries (vasa recta; black asterisks)
-distal ileum: has a thin wall, few if any circular folds of mucosa, numerous lymphoid nodules that are best seen histologically, relatively short straight arteries (vasa recta; black asterisks)
-straight arteries (vasa recta) essentially end arteries; blockage can result in ischemia and subsequent necrosis
appearance of mesentery between jejunum and ileum
-ruffled appearance
-presence of arteries and veins within mesentery
root of mesentery
-green asterisks
-on posterior abdominal wall
-approximately 6 inches in length; explains ruffled appearance of mesentery
-begins at duodenojejunal junction (L2) and ends at the ileocecal junction (L5) crossing from left to right
-branches of the superior mesenteric artery and vein are within root of mesentery since they provide blood supply to jejunum and ileum