Chapter 1-3 Intro pharm
1/53
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
54 Terms
Pharmacology
Study of drugs
Pharmacodynamics
Action of drugs on living tissue
What the drug does to the body
(Mechanism, effects, dose response etc)
Pharmacokinetics
How drugs are processed in the body (ADME)
What the body does to the drug
Pharmacotherapeutics
Study of drugs in treating disease
Pharmacy
Preparing and dispensing medication
Posology
Study of the amount of drugs required to produce a therapeutic effect
Toxicology
Study of harmful effects of drugs on living tissue
What is ADME?
Absorption
How the drug enters
Distribution
Where the drug travels (tissues, organs)
Metabolism
How the liver metabolizes the drug
Excretion
How the kidney gets rid of the drug —> urine
What is a drug?
Substance given to a living organism to produce a change in function
Drug — Medication used for diagnosing, curing, or treating disease. Both chemical and biological properties
Water, metal, insecticides etc.
What are physical and chemical properties of a drug?
Drug properties determines the effects on the body
Chemical: Structure
Physical: Solubility (water, fat), selectivity, affinity for receptors, metabolism
All drugs produce more than 1 effect
Where do drugs come from?
Animals
Premarin (horse urine for estrogen)
Plants
Foxglove (lowers HR)
Poppy (morphine)
Microorganisms (bacteria)
Chemical synthesis (man-made)
Drugs will have 2 effects..
Therapeutic
Undesirable
Difference between therapeutic effect, side effect, adverse effects, and toxic effects
Therapeutic effect
Intended use
Side effect
Unintended use / Undesirable effect / Tolerated
More nuisance than harmful (dry mouth)
Adverse effects
Harmful or damage to organs when used for long time
Diarrhea, vomitting
Toxic effect
Extremely life threatening
Anaphylaxis
Drug indication and contraindication
Indication
Therapeutic use of drug —> Why drug is used
Ex: Insulin —> manage diabetes
Contraindication
Why the drug should NOT be used
Ex: Liver disease can’t take aspirin (bleeding)
What are the 4 drug interactions? (I—ASS—A)
Incompatibility
Precipitate before administration
Additive effect
2 drugs, same biological response, same mechanism of action
1 advil (50%) + 1 aleve (50%) = 100%
Summation
2 drugs, same biological response, different mechanism of action
Zantac + Prilosec (H2 blockers)
Synergism
2 drugs combined together enhance each other for greater effect
Alcohol + sleeping pills = 110% enhancement
Antagonism
1 drug blocks another
Opioids + narcan
Biological response: (end goal of drug)
Mechanism of action: how the drug is produces its effects
Describe the mechanism of action, site of action, receptor site, agonist, antagonist
Mechanism of action: How drug produce pharmacological effect
Does it block an enzyme, activate a receptor? etc.
Site of action: Where the drug exerts its therapeutic effect
Location (blood vessels, lungs)
Not always known
Receptor site
Site where drug binds to receptor
Agonist
Produces a drug action
Antagonist
Block other drugs from producing an effect
Competitive antagonism
competes with same receptor
What is the dose response relationship?
Dose: Amount of drug given to produce an effect
Response: Effect from dose
Effective dose (ED50)
Produces 50% of max therapeutic effect
Dose where 50% of population experience therapeutic effect
Used to compare potency between drugs
A drug gives 100% pain relief at 80mg.
60mg give 50% relief. In this case, the ED50 is 60mg, even though that’s not half the dose (or strength) — it's the dose that gives half the effect.
Purpose of the dose response curve?
Drug is proportional to dose (drug increase, response increase)
Helps compare the potency between drugs
Potency
ED50 of drug A is 10 mg
ED50 of drug B is 20 mg.
Therefore, drug A is twice as potent as drug B.
Twice the concentration of drug B is needed to produce the same response as drug A.
20/10 = 2x more potent
Ceiling effect
Increasing dose doesn’t increase effects
Nothing past 100% — Will cause toxic effects
Time plasma concentration curve
Drug dose in blood over time (time response)’
3 parts to curve
Onset of action
Drug first start working
Duration of action
Time the drug continues to product its therapuetic effect (effective range)
Termination of action
Therapeutic effect wears off — not effective range
Purpose
Used to predict frequency of when drug is administered to keep effective drug response (duration of action)
Shows the concentration of drug over time
Whats the 2 FDA guidelines for drugs? Drugs are tested on ______ first before humans
Safety
Efficacy
Why? Flipper baby incident
Animals

What is LD50?
Lethal dose at 50% (first test)
Dose that kills 50% of animals tested
Dose where 50% of population would die from the drug
Purpose
Predict safety of drug OR how toxic it is
Therapeutic index (TI)
TI = LD50 / ED50 =
Bigger TI = safer drug
bc need higher dose to product toxicity
Margin between therapeutic and lethal dose
→ TI = 10 means lethal dose is 10x higher than effective dose (safe)
→ TI = 2 means lethal dose is 2x higher than effective dose (risky)
Tells you how safe a drug is
Whats the goal of drug therapy?
To achieve therapeutic effects without producing any harmful effects
Controlled substances (5 schedules)
Regulate dispensing of drugs that have potential for abuse
Schedule I – Drugs with high abuse potential and no accepted medical use (heroin)
Schedule II - Drugs with high abuse potential and accepted medical use (morphine)
Schedule III – Drugs with moderate abuse potential and accepted medical use (tylenol)
Schedule IV — Drugs with low abuse potential and accepted medical use (valium)
Schedule V – Drugs with limited abuse potential and accepted medical use
How are drugs named? What is the difference between generic names, brand names and chemical names?
Generic names
Official, simplified, nonproprietary, FDA approved
Brand name
Pharmaceutical company / trademark (product) / proprietary
Chemical name
IUPAC — molecular structure
Which biological factor affects drug action?
Dosage
Routes of administration
ADME
Half life
Blood drug levels
Bioavailability
Genetics
3 types of drug preparations
Aqueous preparation
syrups and suspensions (solid in liquid shake)
Alcoholic preparations
Elixirs, spirits, tinctures, extracts
Solid and semi preparations
Solid most common
List the different forms of drug products (solids and semisolids)
Powder
Tablet
compressed powder
Troches and lozenges
dissolve in mouth (cough drops)
Capsules
Gelatin shell with drug powder
Delayed release product
Tablet or capsule with special coating — dissolve at different times
bypass parts of GI
Enteric coating
Type of delayed release product
Special coating to protect from stomach acid — Dissolves when reach basic pH
Irritate stomach or destroy drug
2 delayed release system for drugs?
SODAS (Spheroidal Oral Drug Absorption System)
Pellet with different coating — release at different times (delayed)
Less frequent dosing
Not affected by food or GI
GITS (Gastrointestinal Therapeutic System)
Constant release rate over time
Semi solid drug forms (topical preparations)
Cream
Emulsion of oil + water = water based
Ointment
Oil based
Suppositories
Inserted into rectum/ vag
Transdermal patches
Controlled release patch
What type of preparation are creams and ointments?
Topical preparaion
Routes of administration
Oral
Mouth
Most safe but slow
Enteral
Through GI tract
Suppositories
Parenteral
Not GI tract
Inhalation, topical, IV (injection)
Fast but can’t be withdrawn (risk of overdose)
Factors affecting absorption of drugs
Lipid solubility of drug
More lipid soluble = pass faster
Ionization
Unionized form = better absorption
pH
Acid = readily absorbed in acidic environment (stomach)
Base = readily absorbed in basic environemnt (Urine)
What is the role of drug ionization and lipid solubility in pharmacokinetics?
Ionization and lipid solubility affect the speed and rate of drug transportation
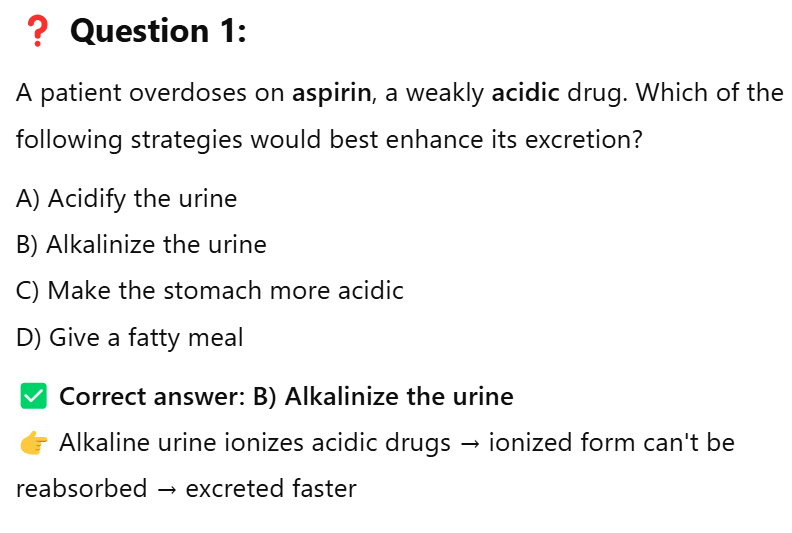
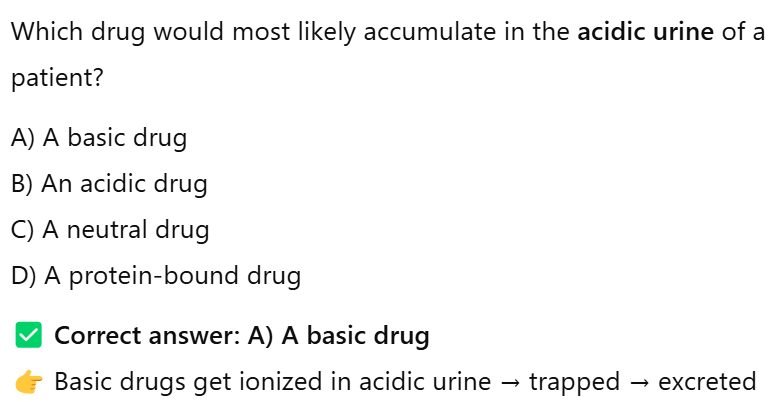
What conditions do acidic and basic drugs prefer and why?
Acidic drugs
Prefer acidic
Stays unionized in stomach
Becomes ionized in urine
Basic drugs
Prefer basic
Stays unionized in urine
Becomes ionized in stomach
Unionized = easily diffuse through phospholipid bilayer, more lipid soluble
Ionized = can’t pass through membrane —> excreted
Different ways drugs can cross cell membrane
Passive diffusion
High to low concentration
Facilitated diffusion
Passive through protein channel
Active transport
Use ATP — Low to high
What factors affect distribution of drugs?
Plasma protein binding
Only free unbound drugs (not attached to plasma protein) can cause pharmacological response
Bounded drugs = Inactive drug protein complex (can’t cross membrane)
Blood flow
Organs with higher blood flow —> drugs delivered faster
High blood flow (Liver, kidney, brain)
Low blood flow (Adipose tissue) except for lipid soluble drugs
Blood brain barrier (BBB)
Lipid soluble drugs easily pass through
Restricts water soluble
What is metabolism? What organ? DMMS? First pass effect?
Metabolism: Chemical alteration of drugs in the body
Aka Biotransformation
Chemically altered before excreted by kidneys
Liver does metabolism
Drug microsomal metabolizing system (DMMS)
Enzyme in liver
Convert lipid soluble drugs —> water soluble (to be excreted)
First pass effect
After oral administration, all drugs are absorbed into portal circulation
Reducing concentration or amount of drugs
Take drug —> absorbed in GI —> enters portal circulation —> Liver metabolism (greatly reduces amount of drugs entering blood stream)
Reduces bioavailability
All oral drugs enter portal circulation
Enzyme induction
Repeated use of drug, liver makes more enzymes
Result: Faster drug metabolism
What routes of administration bypass the liver (first pass?)
90% of oral medication is metabolized and destroyed by the liver before it reaches the heart
Venous system (injection / IV)
Nasal (goes to veins)
Rectum/ transdermal patch (skin)
Different methods of drug excretion. Where can drug excretion occur and what state must the drug form be in to facilitate excretion
Methods of excretion
Renal excretion (Kidneys → Urine)
Filtered by glomerulus in kidneys
Reabsorbed back except urinary waste
Must be in ionized and water soluble form
GI excretion (Fecal)
Reabsorbed back into enterohepatic pathway
Liver → Bile → Intestines → Blood → Liver (repeat) (L—BIB)
Recycling of drugs/ substances
Prolong drug effects and increase half life
Respiratory excretion
Lungs, breathing, alcohol
Anesthetic gases not metabolized by lungs
Sweat, saliva, tears, bodily fluids
Placenta through pregnancy
→ Must be ionized form
How does half life relate to drug response?
Half life
Time it takes for blood concentration of drug to fall to half of its original level
Importance
Determine frequency of drug administration
Relate to drug response (body’s response to drug)
Longer half life = stays in body longer
Shorter half life = doesn’t stay in body as long
Need more dosing
What are the 2 factors that affect half life and blood drug levels? (ME)
Metabolism
How fast liver breaks down
Slow liver = Slow metabolism = longer half life
Excretion
Slow kidney = drug stays longer = longer half life
How does blood drug levels relate to drug response?
Blood drug levels
Concentration of drugs in blood
Dependent on ADME
Relate to drug response
Too little = not effective
Just right = therapeutic effect
Too high = toxic
Goal is maintain therapeutic range
How does bioavailability relate to drug response?
Bioavailability
How much drugs gets absorbed into the blood
Relate to drug response
High bioavailability = More drug is available to exert on body
Low bioavailability = Needs more doses for therapeutic effect
Ex: Expensive pee
Factors that influence bioavailability? DRIG + absorption factors
Drug formation (lipid/ water sol)
Route of administration
Individual variations
GI absorption (Movement, pH, food)
Individual variation factors (AW—GG—EPPP)
Age
Weight
Gender and body fat
Genetics
Emotional state
Placebo
Presence of disease
Patient compliance
Define loading dose and maintenance dose. What is the purpose of a loading dose?
Need higher blood drug levels
Loading dose
Initial dose to give therapeutic range (jumpstart)
Maintenance dose
Dose after loading dose to maintain therapeutic range
Factors for pediatric drug administration and how it affects pharmacokinetics.
Teratogenic risk (drug causes birth defects during pregnancy)
Breastfeeding
Drugs pass onto milk
FDA category X
Contraindicated drugs for pregnancy
Teratogenic risk
How it affects pharmacokinetics
Faster drug processing in kids
Dosing is based on weight, not age
Chronic drug use and tolerance
Chronic drug use
Using drug repeatedly over time
Tolerance
Repeated administration decreases drug effect
What are the 2 types of tolerance?
Metabolic tolerance
Caused by Enzyme induction (body makes more enzymes)
Drug metabolized more quickly
Pharmacodynamic tolerance (aka Down regulation)
Caused by decrease in receptors
Fewer receptors drug can bind to = weaken effect
Takes longer to occur
Differentiate between drug dependency vs drug addiction
Drug dependency
Relying on drug to feel normal or function (well being)
Can be..
Physical
Body needs drug to avoid withdrawal
Psychological
Person craves and believes they can’t function w/o drug
Unpleasant feeling (not smoking tobacco for short time)
Drug addiction
Dependence is severe and compulsive
Interrupts ADL (activities of daily living)