Psych 3501 Exam 3: Cognitive Behavior Therapy
1/23
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
24 Terms
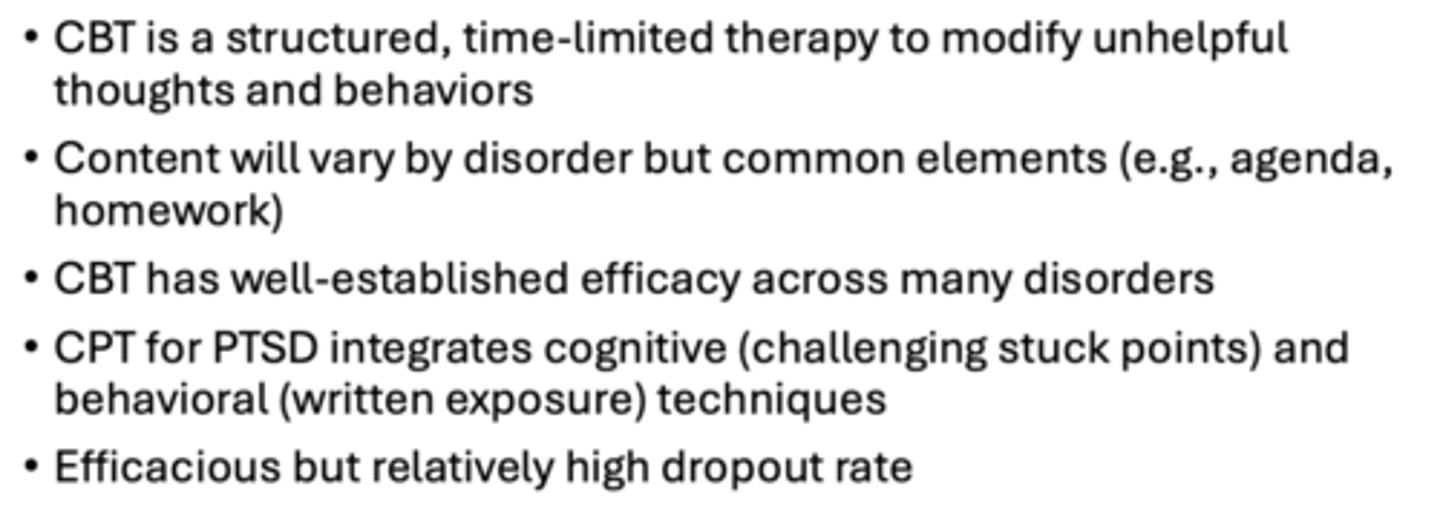
Cognitive behavior therapy (CBT)
Structured: every session of CBT generally follows the same format
Time-limited: 12-20 session in general
Present-focused: targeting on current thought patterns/behaviors
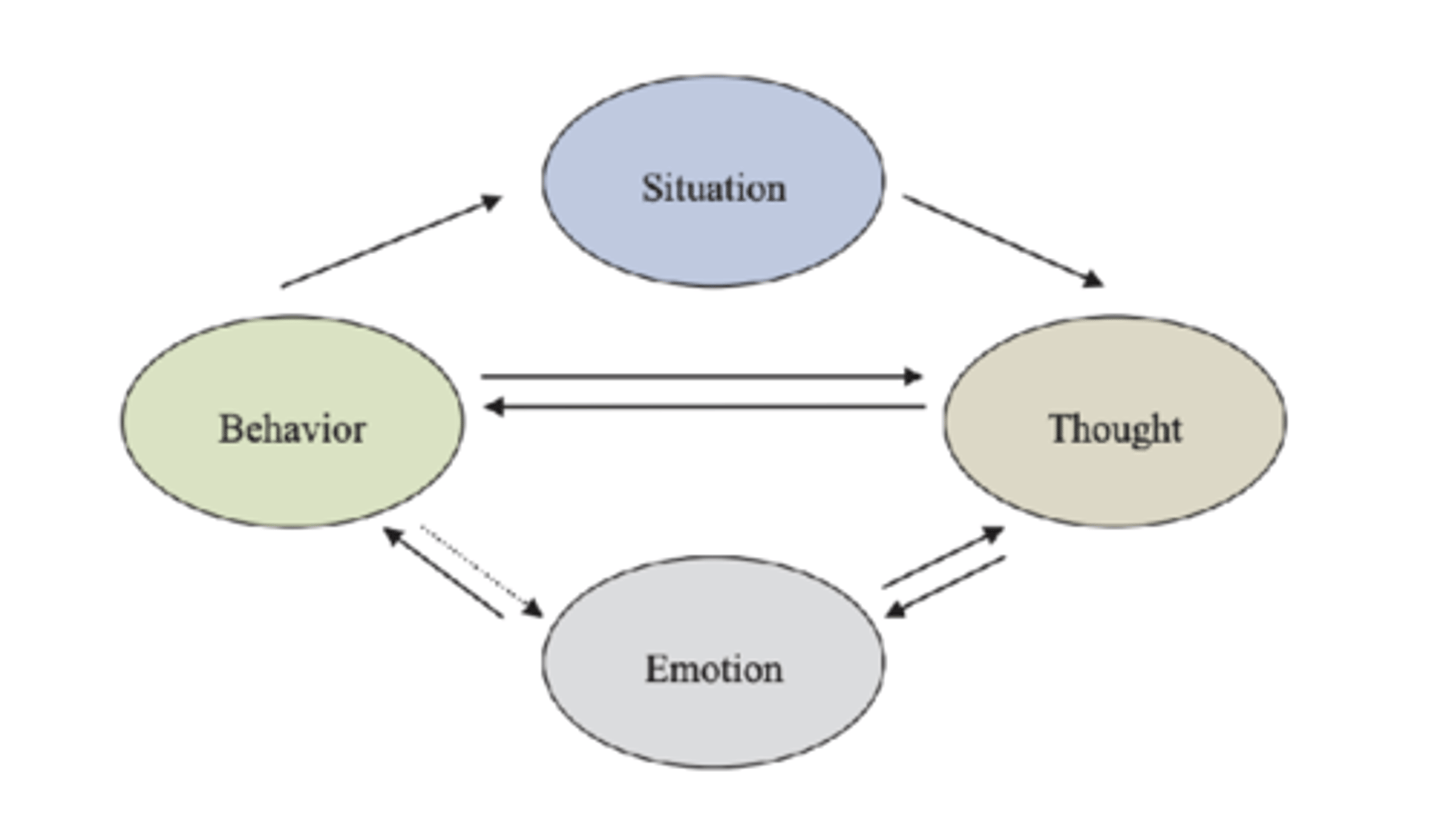
CBT Goals
Develop strategies to modify dysfunctional thinking patterns or cognitions ("C")
Develop strategies to modify maladaptive emotions and behaviors ("B")
CBT Skills
help the client develop a new set of skills to reduce symptoms and to maintain in the long-run through collaboration
Increase awareness of thoughts and emotions
Identify how situations, thoughts, and behaviors influence emotions
Improve emotions by changing thoughts and behaviors
- Collaboration is important
- What sets CBT apart: teaching skills & homework to reinforce skills learned
- Focused on skill acquisition
General session structure
Symptom check
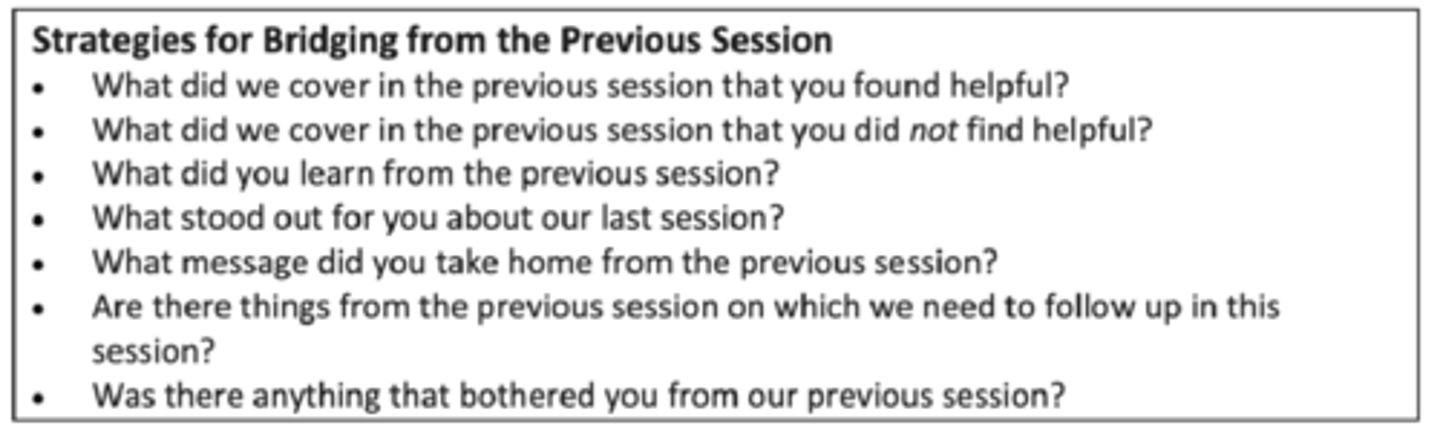
Bridge from previous session: linking today to what you did last time
Agenda setting: what we are going to do today
Homework review
Agenda items: go through
Assign homework
Session summary and feedback
Symptom check
Brief assessment: the level of symptom severity the client is presenting today
Goals:
Track progress over time
Make progress explicit to client: the client can see symptom decrease
Alerts therapist to symptoms that require immediate attention
Bridge from previous session
Identify negative reactions
Make sure goals are met
Identify agenda items to put on the current session
Agenda setting
Collaborative process to identify topics for session
- “What do you want to discuss/accomplish today?”
Models a systematic approach to problems
- Good problem-solving model to clients
Provides structure to session
Use agenda items to meet treatment goals and facilitate skill development
Homework review
Reinforce importance of between-session practice
- Always check in to show client that it’s important
Assess skill acquisition
- What did you learn from the homework? What impact?
- Opportunity to reinforce the CBT principles
May be brief or take most of the session
Dealing with noncompliance
- Identify barriers: too challenging? Too time-consuming?
Agenda items
Address in order of importance agreed upon by client and therapist
Therapist identifies CBT principles underlying each problem
Uses problems to teach CBT skills
Assign homework
Essential component of CBT
Reinforce in-session learning
Practice skills in real life
Collaboration fosters compliance
- The client comes up with ideas for homework
- Also test for their understanding of the session
Good homework assignments set clients up for success
- E.g., thought record: did it one time in session so the client understands how to do it
- Realistic, plausible
Concrete goals
Break down to exactly what you are asking them to do
Session summary and feedback
goal: knowledge check, address misunderstandings
Summary initially by therapist, later by client
What was the most helpful thing that we discussed in today's session?
What will you take away from this session?
Unaddressed agenda items
Feedback from the client
CBT application and efficacy
Efficacious for almost every disorder that has been assessed
For all different disorders, good response rates for CBT, better than controls
CBT: the "gold-standard" for psychotherapy
1. CBT is most researched psychotherapy
2. No other psychotherapy shown to be systematically superior to CBT
- May be not significantly different, but no evidence of "better"
3. CBT theoretical models/mechanisms of change most researched, consistent with current neuroscience paradigms of human mind and behavior
- E.g., information processing; learning and memory
Cognitive Processing Therapy (CPT)
Specific CBT psychotherapy for PTSD
Impact statement
Write down what your traumatic experience means to you. Why do you think it occurred? How did it impact your thoughts, perceptions and beliefs about yourself, others, and the world in general?
Goal: to understand the meaning of the trauma to the client without getting into details yet
Use the impact statement to identify stuck points
Stuck points
Unhelpful, maladaptive thoughts that keep the client “stuck” from recovering
Thoughts about why the trauma happened
Thoughts about self, others, the world have changed because of the trauma
Often an “if…then…” structure
- E.g., if I had been paying attention, no one would have died
Often have extreme language
- E.g., I am damaged forever because of the assault
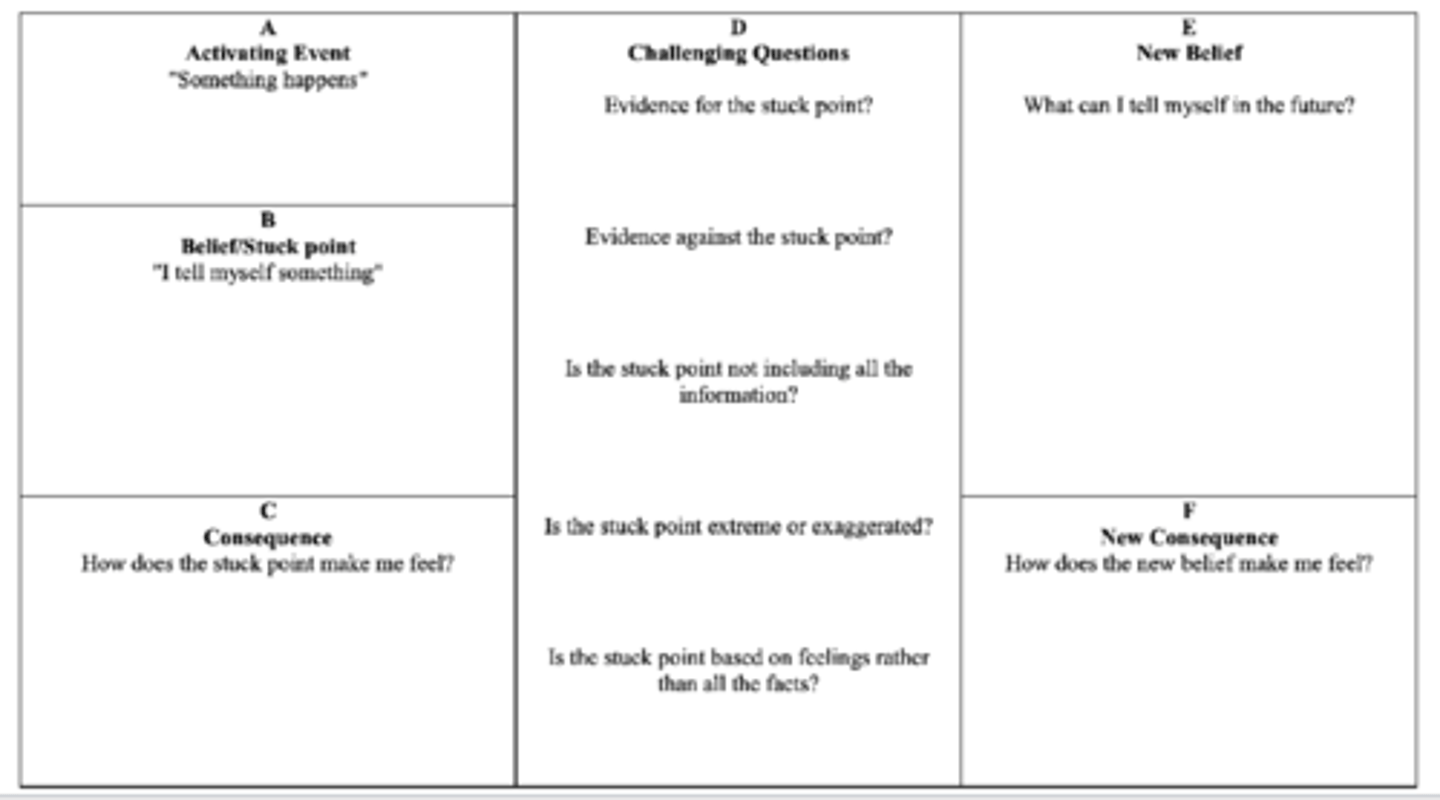
Challenging stuck points
Evidence for and against?
Is the stuck point missing information?
Does the stuck point include black/white thinking?
Does the stuck point originate from a reliable information source?
Does the stuck point conflate possible with likely?
A-B-C analysis
Similar to thought record
A: activating event
B: belief/stuck point
C: consequence
Written trauma account
Around session 3-4, not directly jump in
Full written account of the trauma with sensory details
Read account daily (homework)
Read account in session with emotion expression
- Reliving experience
Rewrite with more detail
- The first draft is usually thin on details
- As exposure increases, they are able to increase more details, making the exposure more robust
Goal: engage with the fear stimulus, anxiety goes up, and learn that you can tolerate it, so it goes back down, eventually for the client to be able to discuss the event without the impact
Efficacy of CPT for PTSD
Comparing CPT to waitlist control/placebo: large effect size
Comparing CPT to another evidence-based psychotherapy for trauma: small significant difference better than the other psychotherapy
Conclusion: efficacious as treatment for PTSD
Is the exposure piece needed?
There is no significant difference in CPT outcomes with or without the written exposure
Significantly lower symptom reduction in military compared to non-military
Rates of dropout from CPT
CPT comparing to other treatments for PTSD
Relatively higher than other treatment, but not dramatically so
Dropout higher for military compared to non-military clients
Predictors of dropout
Factors in-session that are predictive of dropout:
Physiological distress: higher distress associated to lower dropout
Avoidance: higher avoidance associated to higher dropout
Cognitive emotional processing: higher processing associated to lower dropout
Engaging -> getting a desired effect
Summary