12. Infectious diseases of dogs & cats characterised by natural focality (leptospirosis, lyme borreliosis, tick encephalitis, ehrlichiosis, ....)
1/50
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
51 Terms
What is natural focality in the context of disease?
A pathogen that is a part of an ecosystem and spreads under favourable conditions, geographically and seasonally limited.
What are examples of diseases with natural focality?
Leptospirosis
Borreliosis
Ehrlichiosis
Tick encephalitis
Tularaemia
Anaplasmosis
Bartonellosis/Cat scratch fever
Q fever
Which diseases with natural focality are zoonotic?
Leptospirosis
Borreliosis
Tularaemia
Bartonellosis/Cat scratch fever
Q fever
What is the natural focality of leptospirosis?
Seasonal in temperate areas (more when heavy rainfall thrives in moist conditions, autumn) & year- round in tropical climates
More common in areas where rats are found (urine)
What is the treatment for leptospirosis?
Doxycycline
What type of transmission characterises all tick-transmitted diseases?
Natural focal transmission
What are the peak seasons for tick-borne diseases in temperate areas?
Spring (nymphs) and summer/autumn (adults)
What is the causative agent of Lyme disease (Borreliosis)?
Borrelia burgdorferi sensu lato (Borrelia burgdorferi sensu stricto, Borrelia afzelli, Borrelia garinii)
How is Borreliosis transmitted?
Tick nymphs (Ixodes ricinus, Dermacentor)
What is the pathogenesis of borreliosis?
Bacteria in tick saliva → are injected into hosts via tick bite → replicate in skin → enter bloodstream - bacteraemia & fever → pass into lymphatic system → immunocomplexes form → cartilage & bone → arthritis & bone destruction. Also spread to kidneys, CNS, heart
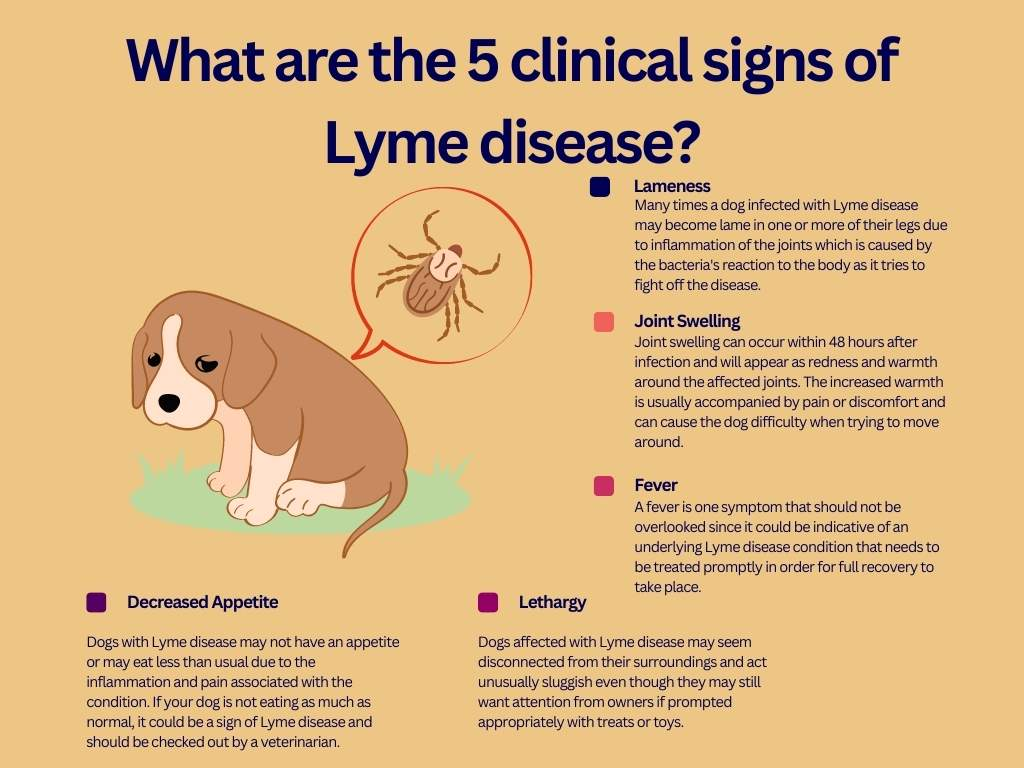
What are some clinical signs of Borreliosis?
General → fever, lethargy, inappetence, swollen lymph nodes
Skin → local irritation
Polyarthritis → lameness, swollen painful joints.
CNS → meningitis, seizures, & facial paralysis
Renal → Characterised by uraemia, hyperphosphatemia, & severe protein-losing nephropathy
What are differential diagnoses for borreliosis?
Babesiosis (musculoskeletal), leptospirosis (kidney), rabies (CNS), anaplasmosis (joint pain)
How is Borreliosis diagnosed?
Serology (ELISA Ab, IFAT), SNAP test 4Dx plus
What is the treatment for Borreliosis?
IV ATB: Doxycycline, amoxicillin, azithromycin for 4 weeks minimum
Supportive care (colloids, fluids)
Symptomatic treatment (NSAIDs)
How is borreliosis prevented?
Antiparasitic drugs
Decrease population density of ticks
Vaccination (1st: 12 weeks; 2nd: +2-3 weeks; booster: annual)
What is the causative agent of Ehrlichiosis?
Ehrlichia canis
What are other names for ehrlichiosis?
Canine haemorrhagic fever
Canine pancytopenia
Tick bite fever
How is Ehrlichiosis transmitted?
Brown dog tick (Rhipicephalus sanguineus)
What is the pathogenesis of ehrlichiosis?
Bacteria infect & phagocytes (monocytes & neutrophils) → replicate until cell bursts → bacteria infect RBCs & replicate → cause haemolysis → results in severe anaemia, widespread blood clotting (DIC), severe multiple organ failure
What are some clinical signs of Ehrlichiosis?
Acute: fever, anorexia, lethargy, lymphadenopathy, thrombocytopenia. This phase begins 1-3 weeks after exposure. Most dogs recover at this point, but others progress to the subacute & chronic phases
Subacute: hypergammaglobulinemia (polyclonal or sometimes monoclonal gammopathy), thrombocytopenia & anaemia usually subclinical, but can last months to years. May be eliminated or progress to chronic.
Chronic: lethargy, weight loss. Mortality can be high in dogs that progress to the chronic stage of disease.
NB: PANCYTOPENIA, BONE MARROW SUPPRESSION & HAEMORRHAGES
How does Ehrlichiosis affect red blood cells?
Destroys bone marrow → non-regenerative anaemia
Which breed is more predisposed to the more severe, chronic form of ehrlichiosis?
German shepherds
How is Ehrlichiosis diagnosed?
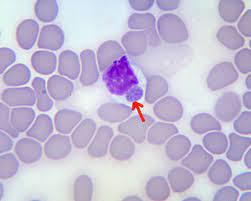
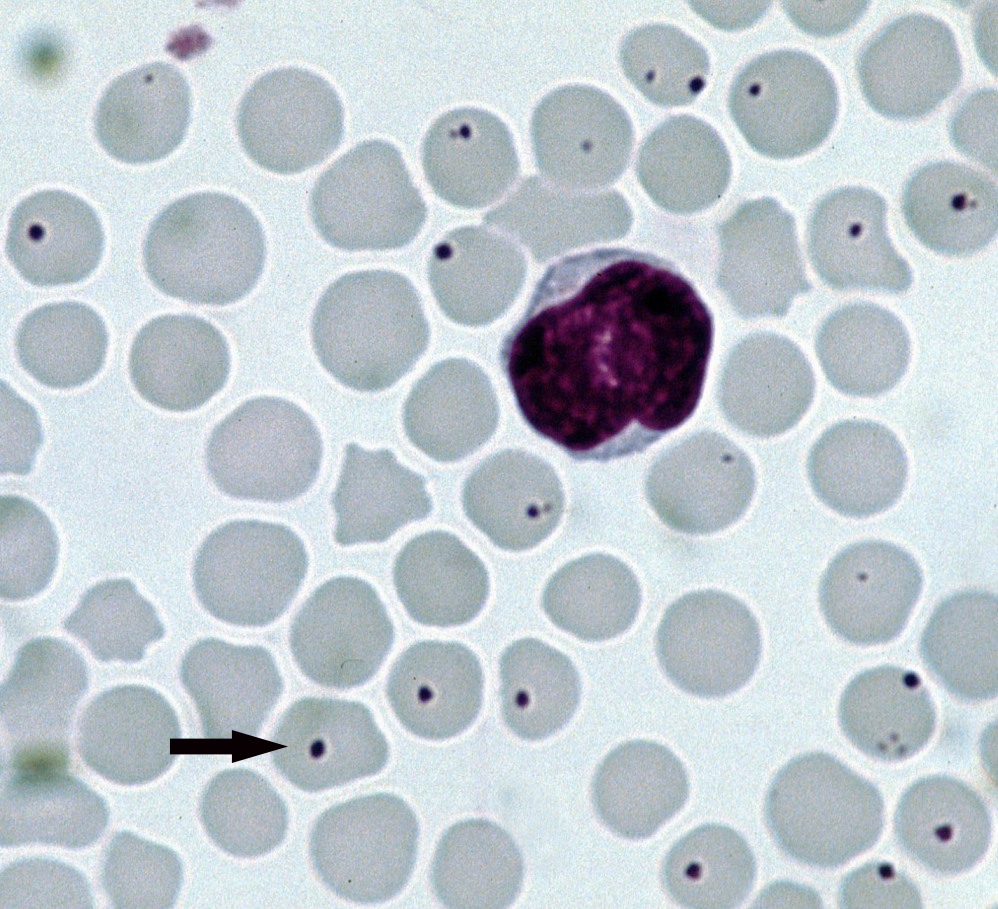
Serology (ELISA - Ab), PCR, blood smear (morulae inclusions in monocytes; rare)
What is the treatment for Ehrlichiosis?
Doxycycline (4 weeks if resistant thrombocytopenia)
What is the causative agent of Tick-borne encephalitis?
Tick-borne encephalitis virus (TBEV), Flaviviridae
How is Tick-borne encephalitis transmitted?
Ticks (Ixodes spp.) with transstadial and transovarial transmission
What is the pathogenesis of tick-borne encephalitis?
Virus replicates at site of infection → enter lymphatic system + bloodstream → viremia → transport to CNS → replicates in neurons → cause neuronal necrosis
What are some clinical signs of Tick-borne encephalitis?
70-80% are asymptomatic. Clinical cases are usually characterised by a biphasic course.
1st Phase: nonspecific symptoms like fever, fatigue, muscle ache, headache & nausea.
2nd Phase: correlates w/ viral invasion of CNS like meningitis (fever, headache), encephalitis (drowsiness, confusion, sensory & motor abnormalities) or meningoencephalitis. High WBCs in blood & CSF.
What are differential diagnoses of tick-borne encephalitis?
Rabies, distemper, Aujeszky’s
How is Tick-borne encephalitis diagnosed?
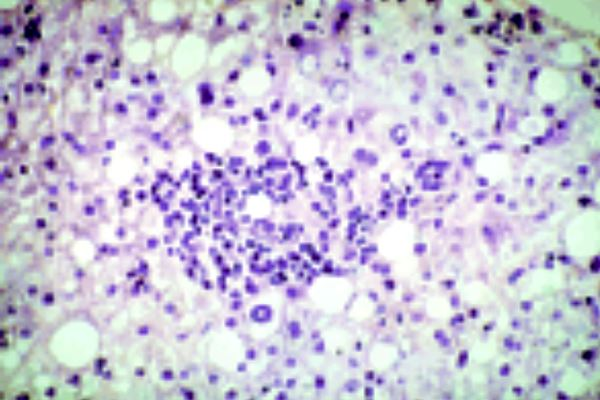
History, clinical signs, serology (VNT, ELISA [IgM Ab]), RT-PCR, histology (perivascular cuffing, disseminated meningoencephalitis)
What is the treatment for Tick-borne encephalitis?
Symptomatic treatment
Anti-inflammatory drugs → corticosteroids, NSAIDs, paracetamol, prednisolone
Sedation → diazepam.
IV fluid → restore electrolytes lost due to vomiting.
Mannitol → decreased excessive fluid accumulation in the brain
What is the prevention against tick-borne encphalitis?
Tick control and vaccination
What is the causative agent of Tularemia?
Francisella tularensis
Where is tularaemia found?
Most countries of the northern hemisphere → N. America, N.Europe, Asia, N. Africa, with some areas being completely free.
Endemic/natural focality → dead rodent infects drinking water.
How is Tularemia transmitted?
Arthropods (mosquitoes, deer flies, ticks), ingestion, inhalation
What are some clinical signs of Tularemia?
Cats: fever, lethargy, septicaemia
Dogs: rare, poor appetite, lethargy, mild fever
What is the treatment for Tularemia?
Streptomycin, doxycycline (resistant to penicillin and sulfonamides)
What are the causative agents of Anaplasmosis?
Anaplasma phagocytophilum → infects neutrophils → anaemia and leukopenia
Anaplasma platys → infects thrombocytes → infectious cyclic thrombocytopenia in dogs
How is Anaplasmosis transmitted?
Ticks (Ixodes)
How is Anaplasmosis diagnosed?
Rapid Ab test, PCR, IFAT
What is the treatment for Anaplasmosis?
Doxycycline
What is the causative agent of Cat Scratch Fever (Bartonellosis)?
Bartonella henselae
How is Cat Scratch Fever transmitted?
Flea faeces (Ctenocephalides felis felis)
What are clinical signs of cat scratch fever?
Mild fever & muscle aches
What is the treatment for Cat Scratch Fever?
Doxycycline, amoxicillin
What is the causative agent of Q fever?
Coxiella burnetii
How is Q fever transmitted?
Ticks, lice, mites, flies, ingestion of bodily fluids/tissues from infected ruminants
What are clinical signs for Q fever?
In carnivores: asymptomatic, pregnancy loss, fever, lethargy, anorexia
How is Q fever diagnosed?
Staining of impression preparates with stamp or Giemsa
What is the treatment for Q fever?
Doxycycline (does not completely eliminate bacteria)
What is a common reservoir for Rabies, contributing to its natural focality?
Red fox