4 - Frank-starling mechanisms and myocardial contractility
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
42 Terms
What is the MAIN function of the cardiovascular system? (3)
To transport blood (oxygen, nutrients, waste products, chemical messengers) to and from body tissues
So that the nutrients, wastes, etc can be exchanged between the blood and the tissues
So that one part of the body, can tell the other part of the body what to do!
How does the body deliver the ‘right amount’ of blood to those capillaries?
By maintaining the ‘right’ blood pressure
Cardiac output
The heart needs to pump the ‘right amount’ of blood
Total peripheral resistance
The arterioles need to have the ‘right’ radius
Blood pressure calculation
Blood pressure = CO x TPR
Sometimes we need cardiac output to go up. For example when we exercise, it can go from 5 L/min up to 20-25 L/min! How can this happen? Which of the following will help increase cardiac output when we exercise? (select all that apply)
A. Decrease preload
B. Increase afterload
C. Increase heart rate
D. Increase stroke volume
E. Increase total peripheral resistance
C. Increase heart rate
D. Increase stroke volume
Draw this out
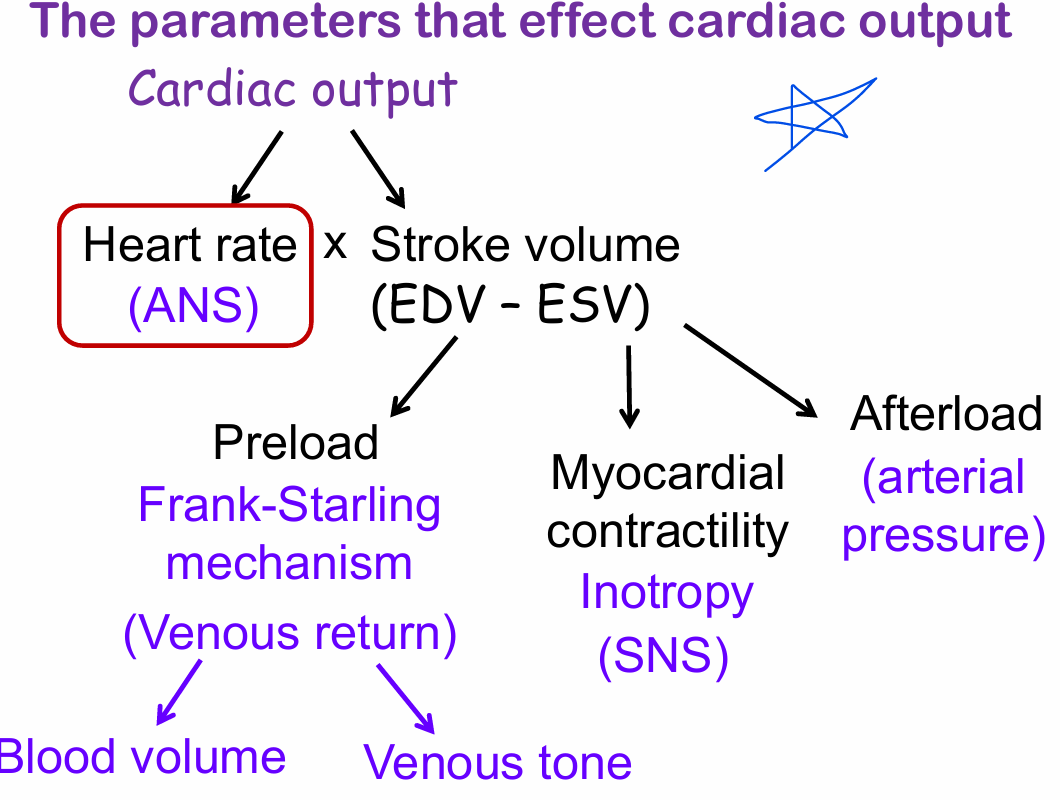
Control of heart rate by the ANS
To increase HR - Decrease PSNS, increase SNS
To decrease HR - Increase PSNS, decrease SNS
What is the inherent rate of the SA node?
100 bpm
If a person’s resting heart rate is 72 bpm, this is because:
A. They have high parasympathetic tone
B. They have high sympathetic tone
A. They have high parasympathetic tone
How does the PSNS lower heart rate? Releases acetylcholine which binds to and activates:
A. Beta 1 receptors on the SA node which decreases phase 0 slope
B. Beta 1 receptors on the SA node which decreases phase 4 slope
C. M receptors on the SA node which decreases phase 0 slope
D. M receptors on the SA node which decreases phase 4 slope
E. N receptors on the AV node
D. M receptors on the SA node which decreases phase 4 slope
EPI and NE activate B1 → increase HR
Depolarization phase controls
Conduction velocity (especially important in AV node)
Pacemaker potential controls
Heart rate (Especially important in the SA node)
What effect will parasympathetic stimulation have on cardiac output?
A. Have no effect on cardiac output
B. Increase cardiac output
C. Decrease cardiac output
C. Decrease cardiac output
CO = HR x SV
The Frank-Starling mechanism (5)
Increase venous return →
Increase the volume of blood in the ventricle at the end of diastole (end diastolic volume (EDV)) OR increase preload
Stretch the chamber wall
Stretch the myocytes
Myocytes respond by increasing force of contraction
What is preload?
The load or how much the wall of the ventricle is stretched at the end of diastole
The Frank-Starling mechanism result with filaments (2)
Greater overlap of thin and thick filaments
Filaments or cross bridge cycling are more sensitive to increases in intracellular Ca++
Frank-Starling Mechanism Ventricular-Function Curve
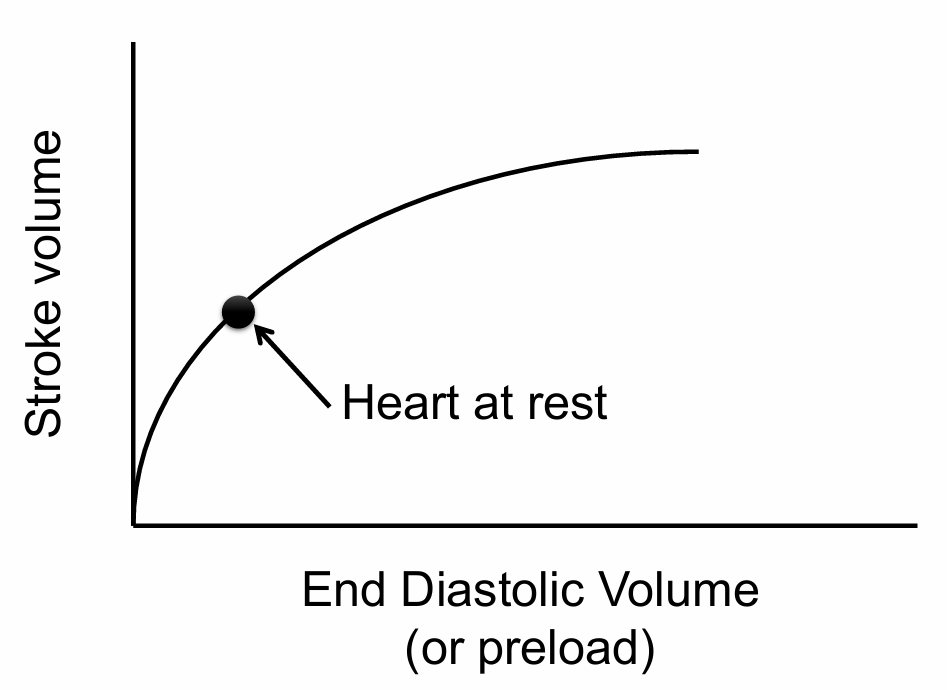
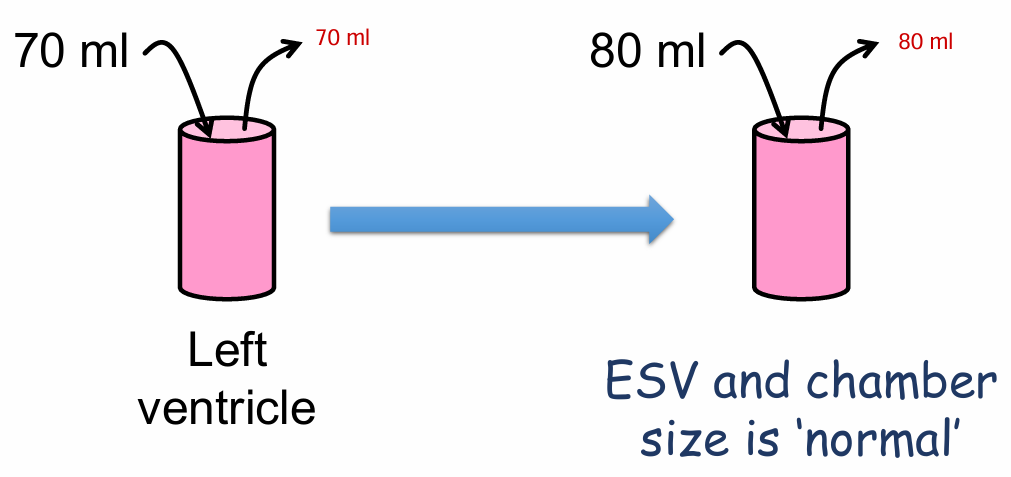
Because of the Frank-Starling mechanism, in a healthy heart, venous return =
cardiac output
What might happen if the Frank- Starling mechanism doesn’t work? For example, with heart failure? (3)
ESV and chamber size is larger than normal
It cannot stretch anymore
Blood backs up in the veins
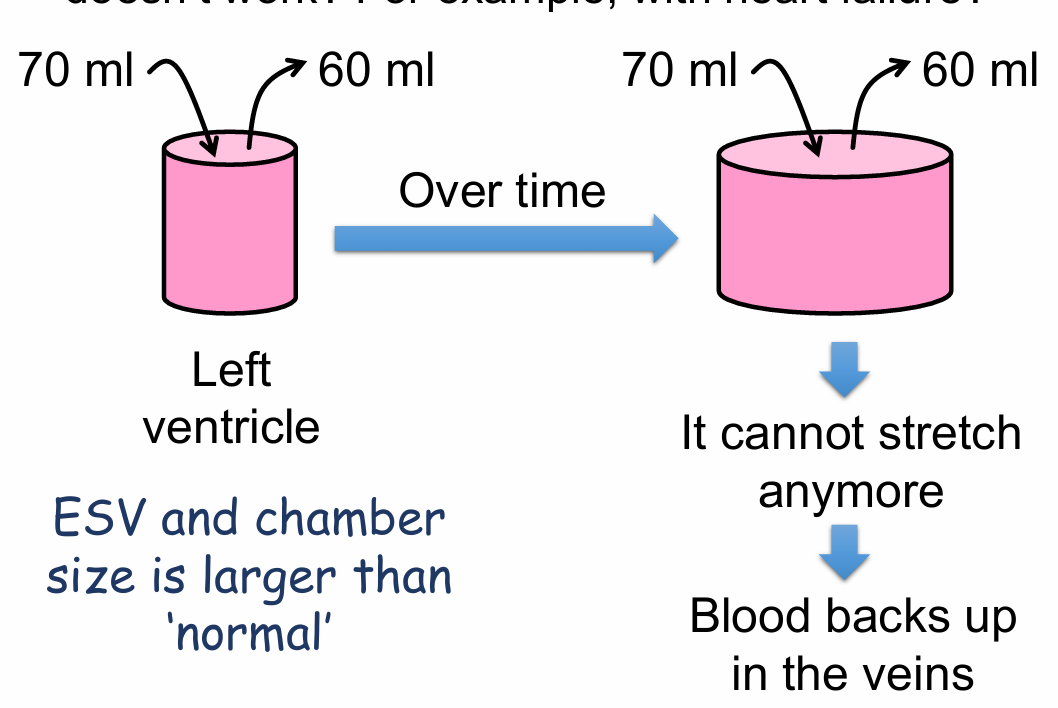
Remember, the heart has a right and left pump. When one of the pumps (i.e. ventricles) fail and the Frank-Starling mechanism doesn’t work:
Blood backs up in the veins supplying that side of the heart This increases venous pressure, which ‘pushes’ fluid into the tissue causing edema
Left heart failure will cause:
Pulmonary edema
Edema from left heart failure (2)
Left heart failure: Too much blood in left ventricle
Blood backs up in the left atria then the pulmonary veins
Edema from right heart failure
Right heart failure: Too much blood in right ventricle
Blood backs up in the right atria and then the systemic veins
What affects venous return?
How much blood is in your body (blood volume)
A person gets a huge cut and loses a lot of blood. How does that affect cardiac output? (3)
A. Decrease blood volume
A. Decrease venous return
A. Decrease cardiac output
A person quickly stands up and gets dizzy because their blood pressure drops. Normally when you stand up, the veins rapidly constrict to help return blood to the heart. What contributed to his drop in blood pressure? The veins remained dilated a little too long, which reduced venous return and:
A. Increased preload and decreased CO
B. Increased preload and increased CO
C. Reduced preload and decreased CO
D. Reduced preload and increased CO
C. Reduced preload and decreased CO
Inotropy definition
The strength of contraction at ANY GIVEN end diastolic volume (EDV) or preload
Ventricles are essentially not innervated by
the PSNS
Activation of Beta 1 receptors (by a variety of neurotransmitters or drugs – e.g. epinephrine, norepinephrine, dopamine, dobutamine) causes a ____ inotropic effect on the heart
Positive; increased contractility
What type of drugs would have a negative inotropic effect? (Select all that are correct)
A. Beta blockers (block Beta 1 receptors)
B. Calcium channel blockers
C. Potassium channel blockers
D. Sodium channel blockers
A. Beta blockers (block Beta 1 receptors)
B. Calcium channel blockers
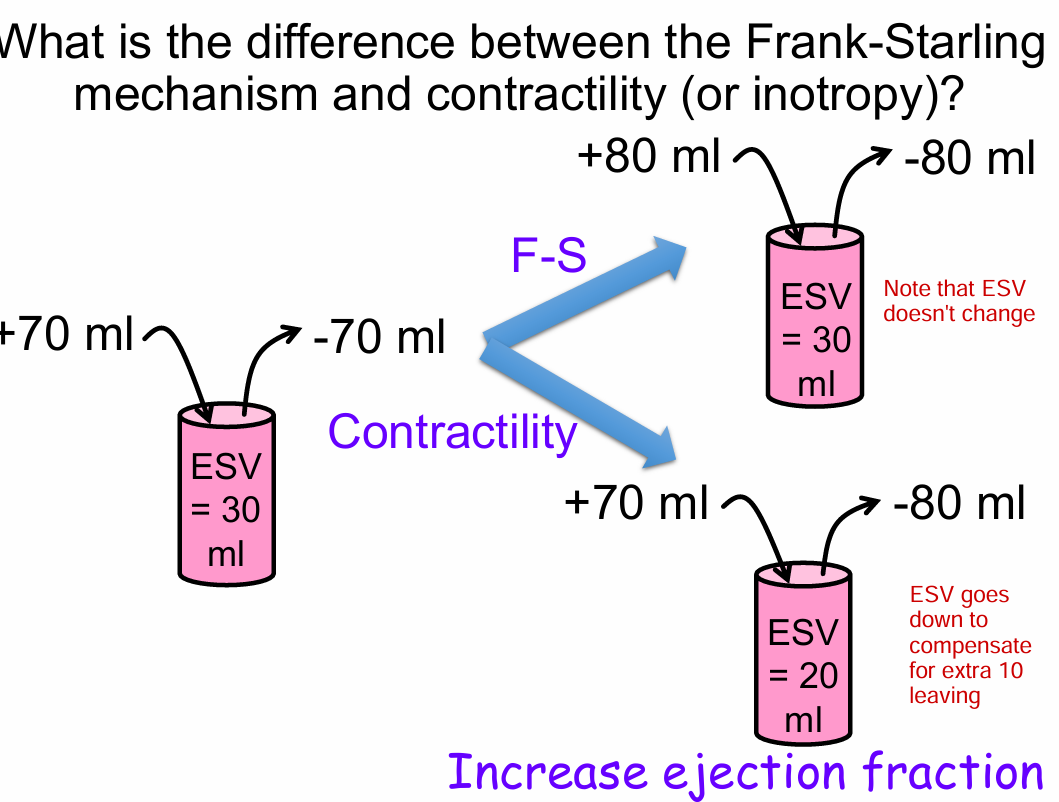
What is the difference between the Frank-Starling mechanism and contractility (or inotropy)?
Frank-Starling mechanism - An increase in preload causes the heart to contract more forcefully and squeeze out that ‘extra blood’
Increase in contractility - The heart contracts more forcefully and squeezes out a greater percentage or fraction of blood for a more complete ejection (ejection fraction)
Ejection fraction (EF) definition
the fraction of blood that is ejected from the heart with each heartbeat
Ejection fraction (EF) calculation
EF = Stroke volume / End diastolic volume (EDV)
Normal resting ejection fraction
50% - 75%
Stroke volume calculation
EDV-ESV
Why are both processes (F-S and inotropy) important? (3)
Both will cause an increased force of contraction → Increa se volume of ejected blood (stroke volume)
Sometimes you need to increase stroke volume just because preload (or end diastolic volume) has increased
Sometimes you need to increase stroke volume because of increased ‘oxygen demand by the tissues of the body’ (Contractility)
How does arterial pressure (afterload) affect cardiac output?
A. Afterload has no effect on CO
B. Increase in afterload will increase CO
C. Increase in afterload will decrease CO
C. Increase in afterload will decrease CO
Because pressure in the aorta is working against the output of the heart
Need to contract at a greater force.
Afterload definition
is the ‘load’ against which the ventricles must pump
When does a person most likely have a chronic increase in afterload?
A. Hypertension
B. Hypotension
C. Hypervolemia
D. Hypovolemia
A. Hypertension
An increase in preload (F-S) and an increase in contractility (inotropy) can both increase stroke volume and cardiac output. If everything else is held constant, which will decrease end systolic volume (ESV)?
A. Both will decrease ESV
B. Neither will decrease ESV
C. Increase in preload
D. Increase in contractility
D. Increase in contractility
Which of the following would be most effective in increasing cardiac output in a person who has heart failure?
A. Decreasing contractility
B. Decreasing heart rate
C. Decreasing afterload
D. Decreasing preload
C. Decreasing afterload