immunodeficiency and HIV
1/39
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
40 Terms
immune system - refresher
Immune system:
Innate (ex: phagocytes, complement)
Adaptive (ex: T cells, B cells)
Central role to protect against microbial pathogens
Compromised defence if one or more components absent or deficient
Immunodeficiency results in
increased susceptibility to infection by specific classes or types of microbes
Repeated or unusual infections is an indication of immunodeficiency
Primary immunodeficiency
Genetically determined or result of developmental anomalies
Inherited, congenital, and rare
Secondary immunodeficiency
Acquired.
Caused by disease or an immunosuppressive treatment
More common.
genetic primary immunodeficiencies
Autosomal or…
X-linked (sex chromosome)
Gene deletions rearrangements, polymorphisms (SNPs)
Biochemical or metabolic primary immunodeficiencies 3
Adenosine deaminase deficiency (T cells)
Purine nucleoside phosphorylase deficiency (T cells)
Developmental arrest (B cells, T cells, Phagocytes
complement deficiency - primary immunodeficiency
complement deficiency - General increased susceptibility to bacterial infections, especially Pneumococcus, Streptococcus and Neisseria
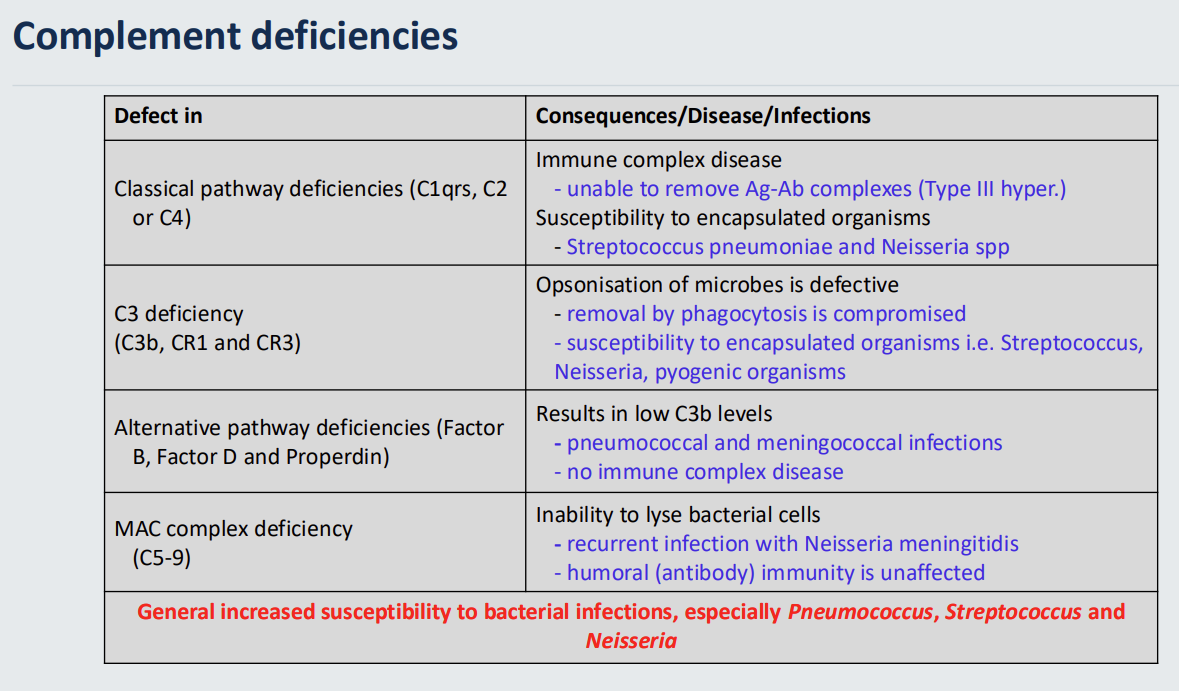
Classical pathway deficiencies (C1qrs, C2 or C4)
Immune complex disease
unable to remove Ag-Ab complexes (Type III hypersensitivity)
Susceptibility to encapsulated organisms
Streptococcus pneumoniae and Neisseria spp
C3 deficiency (C3b, CR1 and CR3)
Opsonisation of microbes is defective
removal by phagocytosis is compromised
susceptibility to encapsulated organisms i.e. Streptococcus, Neisseria, pyogenic organisms
Alternative pathway deficiencies (Factor B, Factor D and Properdin)
Results in low C3b levels - defective phagocytosis
pneumococcal and meningococcal infections
no immune complex disease - as there is no antibody involvement
MAC complex deficiency (C5-9)
Inability to lyse bacterial cells
recurrent infection with Neisseria meningitidis
humoral (antibody) immunity is unaffected
primary immunodeficiency - phagocytosis deficiencies
intrinsic deficiencies - deficiencies in the actual cells that perform the phagocytosis functions
General increased susceptibility to bacterial and fungal infections of skin and mucosal tissues
Treatment: antibiotics or bone marrow transplant (gene therapy)
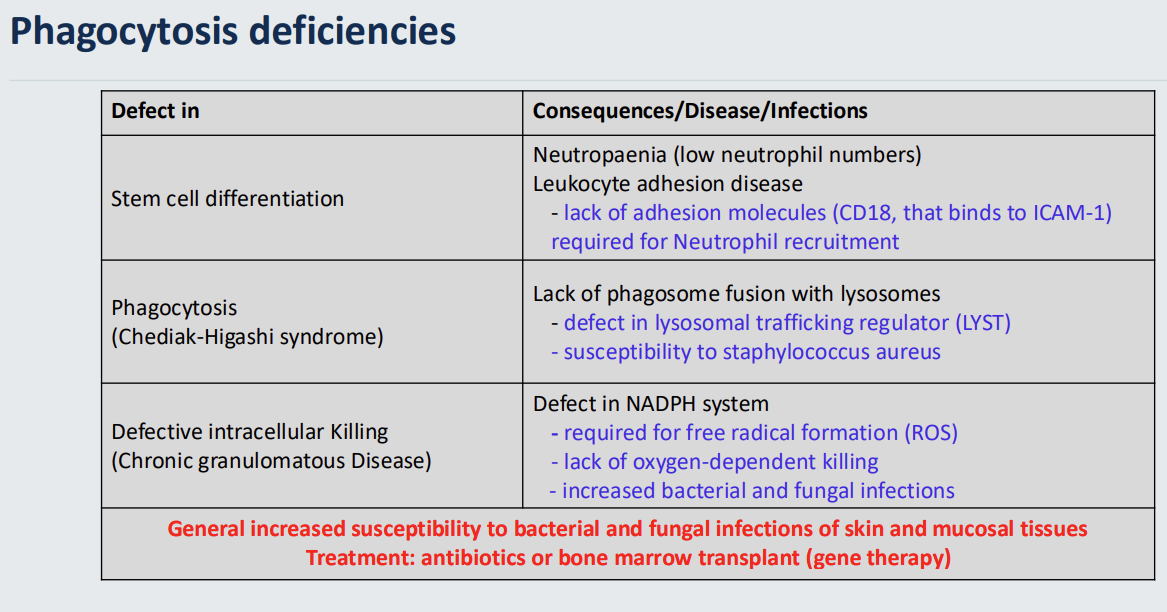
treatment for phagocytosis therapies
antibiotics or bone marrow transplant(gene therapy)
primary immunodeficiency - Stem cell differentiation -
Neutropaenia (low neutrophil numbers)
Leukocyte adhesion disease
lack of adhesion molecules (CD18, that binds to ICAM-1 in epithelial cells - oveming of neutrophils) required for Neutrophil recruitment
primary immunodeficiency - phagocytosis (Chediak-Higashi syndrome)
Lack of phagosome fusion with lysosomes
defect in lysosomal trafficking regulator (LYST) - organism will not be killed
susceptibility to staphylococcus aureus
primary immunodeficiency - Defective intracellular Killing (Chronic granulomatous Disease)
Defect in NADPH system - required for free radical formation (ROS) → lack of oxygen-dependent killing
increased bacterial and fungal infections
primary immunodeficiencies - humoral/antibody deficiencies
Recurrent extracellular bacterial infections (Pneumococcus, Streptococcus, Haemophilus, mainly encapsulated bacteria) Treatment: life-long or periodic gamma globulin injections
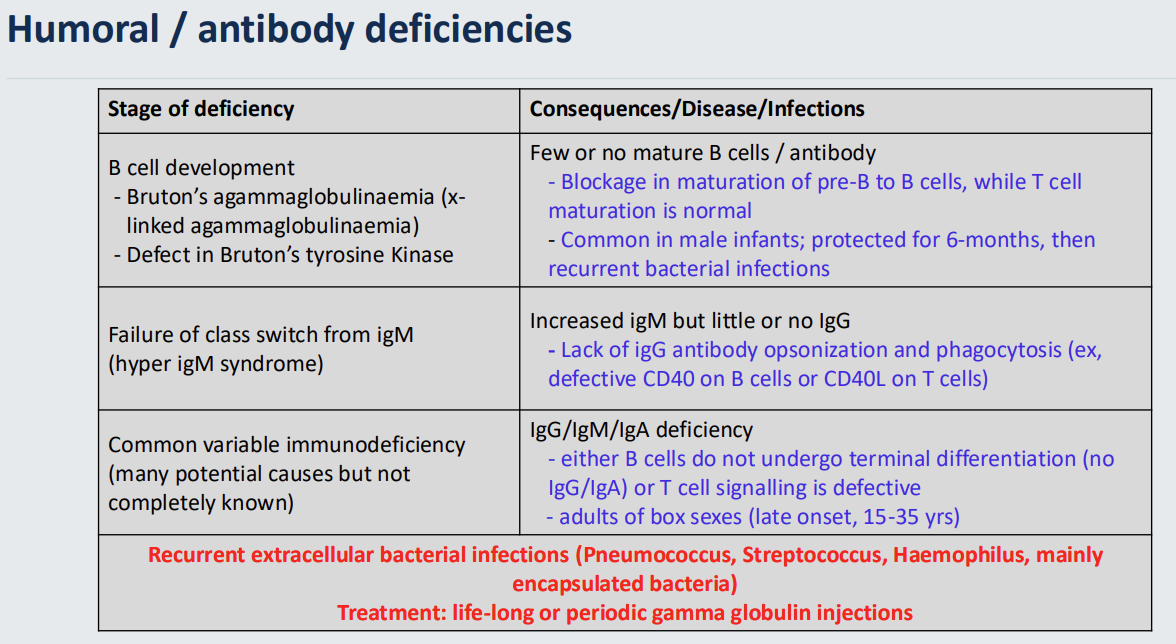
humoral/antibody deficiency treatments
Treatment: life-long or periodic gamma globulin injections
primary immunodeficiencies - B cell development - 2 examples
Bruton’s agammaglobulinaemia (xlinked agammaglobulinaemia)
Defect in Bruton’s tyrosine Kinase
Few or no mature B cells / antibody
Blockage in maturation of pre-B to B cells, while T cell maturation is normal
Common in male infants; protected for 6-months, then recurrent bacterial infections
humoral/antibody deficiencies → Failure of class switch from igM (hyper igM syndrome)
Increased igM but little or no IgG - Lack of igG antibody opsonization and phagocytosis (ex, defective CD40 on B cells or CD40L on T cells)
defects in opsonisation
both T and B cells can be affected
humoral/antibody deficiencies - Common variable immunodeficiency (many potential causes but not completely known)
IgG/IgM/IgA deficiency - either B cells do not undergo terminal differentiation (no IgG/IgA)
or T cell signalling is defective - adults of box sexes (late onset, 15-35 yrs)
affects both B and T cells
T cell deficiencies - primary immunodeficiency
Opportunistic infections (viruses, fungi, parasites, bacteria).
Often fatal in early years of life.
Treatment: bone marrow transplant (gene therapy)
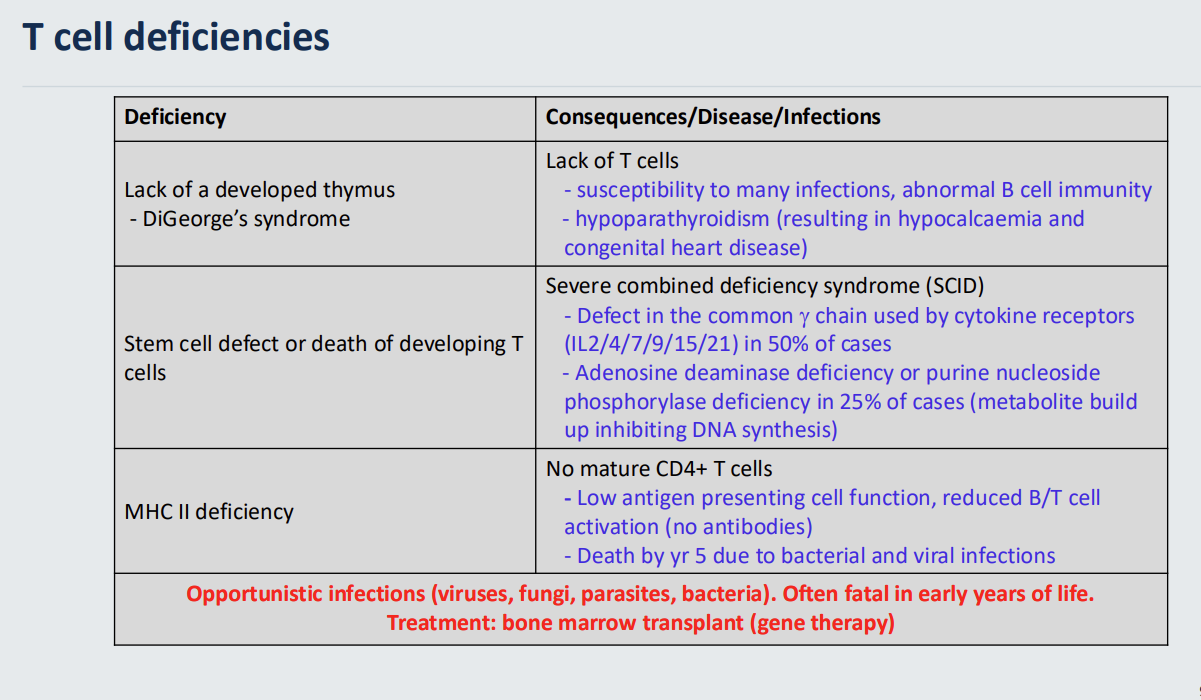
T cell deficiency - treatment
Treatment: bone marrow transplant (gene therapy)
T cell deficiency - Lack of a developed thymus - DiGeorge’s syndrome
Lack of T cells - susceptibility to many infections→abnormal B cell immunity as T cells activate B cells
hypoparathyroidism (resulting in hypocalcaemia and congenital heart disease)
T cell deficiency - Stem cell defect or death of developing T cells
Severe combined deficiency syndrome (SCID) - Defect in the common gamma chain used by cytokine receptors (IL2/4/7/9/15/21) in 50% of cases - Adenosine deaminase deficiency or purine nucleoside phosphorylase deficiency in 25% of cases (metabolite build up inhibiting DNA synthesis)
T cell deficiencies - MHC II deficiency
No mature CD4+ T cells
Low antigen presenting cell function, reduced B/T cell activation (no antibodies)
Death by yr 5 due to bacterial and viral infections
Clinical features of Immunodeficiencies 8
Chronic and recurrent infections
Unusual microbial agents
Incomplete responses to treatment
Skin lesions, warts
Diarrhoea
Recurrent abscesses
Autoimmunity
Failure to thrive
Secondary Immunodeficiencies 6
Therapeutic drugs (cancer chemotherapy, radiation therapy, post-transplant immunosuppression)
Infection (HIV/AIDS)
Metabolic / chronic disorders (ex: diabetes)
Malnutrition
aging
Burns/trauma (loss of immunoglobulin via damaged skin)
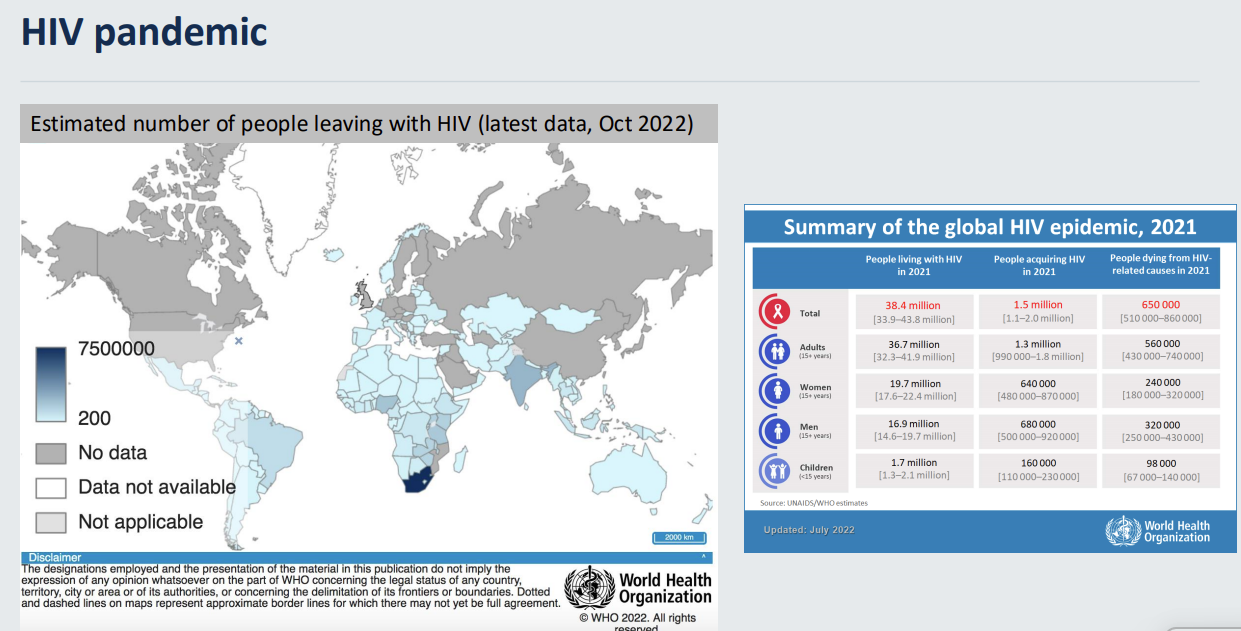
HIV pandemic
38.4 million people currently living with HIV
1.5 million new infections in 2021
0.5 million deaths in 2021
Human Immunodeficiency virus
Causative AIDS agent
Baltimore virus classification: Group VI (ssRNA virus with a DNA intermediate)
Hallmarks: Reverse transcription (RNA -> DNA) and chromosomal integration
once they merge from cell - envelope delved from plasma membrane - as it matures it will form a core with a characteristic conical shape
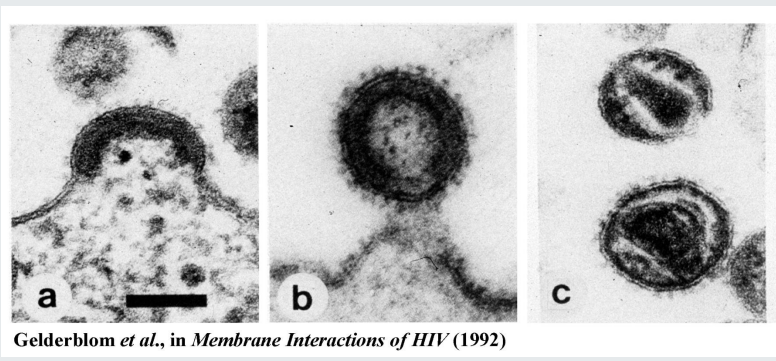
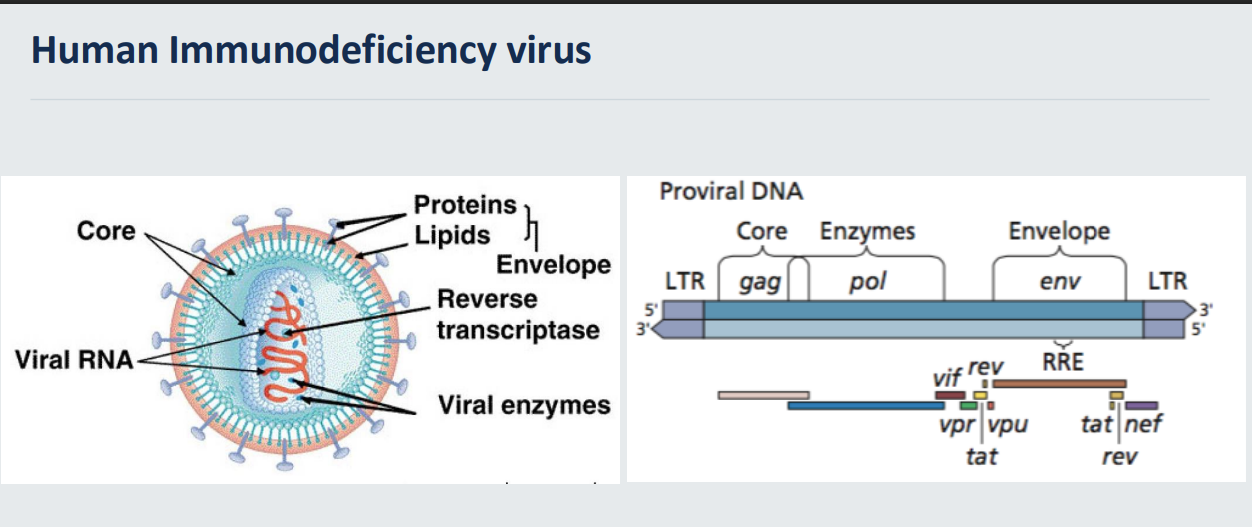
outer layer/envelope
core→ protein capsid
viral genome and viral enzymes
pro vial DNA that is integrated into the host - long terminal repeats
gag - structural proteins
pol - viral enzymes - reverse transcriptase and viral integrase → originals are present in the virus to begin with
env - envelope
rav and tat - regulatory proteins
accessory proteins enhance viral infection
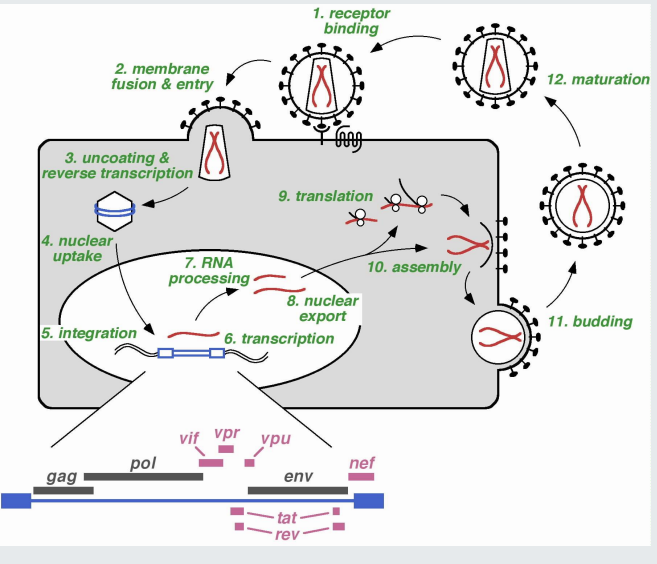
Human Immunodeficiency virus life cycle and cell entry 11
receptor binding - viral envelope protein interacts with CD4 and co-receptors - CCR5 or CXCR4
Fusion of viral membrane with target cell membrane
uncoating and reverse transcription via viral RT enzymes
nuclear entry
integration into host chromosomes
transcription
RNA processing
nuclear export
translation
assemble of progeny
budding
virus only has 9 proteins - many of these steps require host proteins
Cellular infection by HIV - attachment factors
Heparan Sulphate Proteoglycans
Galactosylceramide
alpha3beta7 integrin
DC-SIGN
relatively non specific
not essential
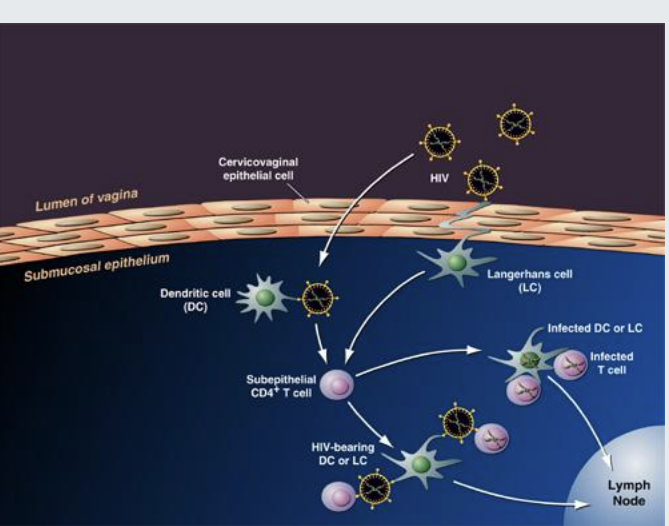
Cellular infection by HIV - receptor
CD4 - requires co receptors
Cellular infection by HIV - coreceptors
CCR5 (macrophages and DCs dendritic cells/langerhans cells) - antiviral that bind to CCR5 can be used in antiretroviral medicine
CXCR4 (T cells including subepithelial Tcells)
can effect D cell which affects T cell or T cell directly
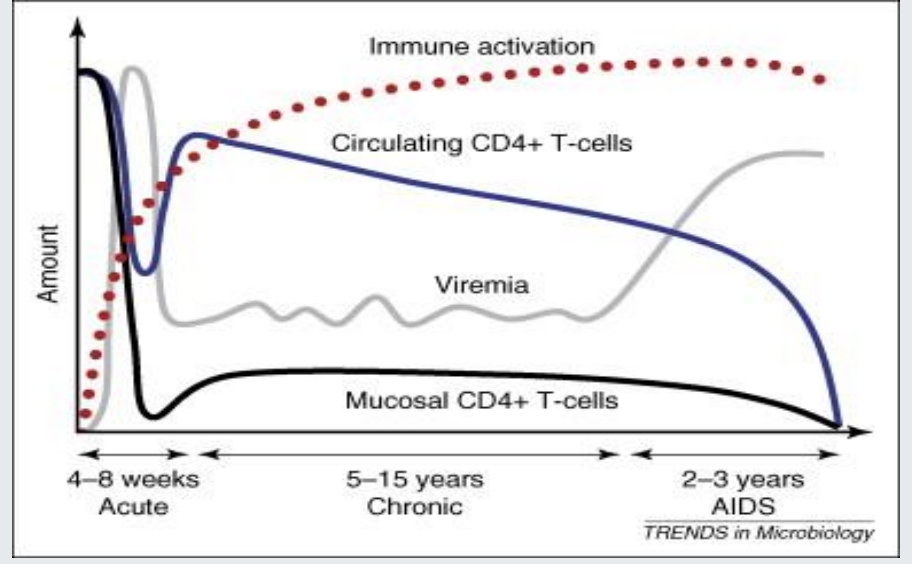
HIV - Course of infection
acute - 2-4weeks - HIV spreads throughout the body - attacks CD4 cells - highly contagious
chronic/clinical latency stage - may show no symptoms - antibodies detected - low risk of transmission if taking antiretrovirals
AIDS - CD4 depleted - CD4 count of less than 200c/ml
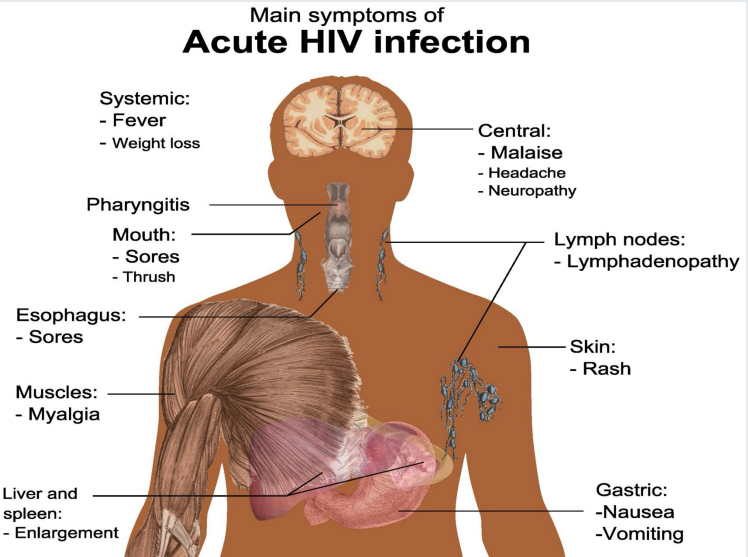
Acute HIV infection symptoms
fever
malaise
sores in mouth/oesophagus
thrush
myalgia
neuropathy
vomiting/nausea
Acquired Immune Deficiency Syndrome (AIDS) - infections and malaignancies
CD4 T cell numbers are reduced -> opportunistic infections
Infections:
Parasites (Toxoplasma spp, Cryptosporidium spp, Leishmania spp)
Bacteria (Mycobacterium tuberculosis, Salmonella spp)
Fungus (Pneumocystis carinii, Cryptococcus neoformans, Candida spp)
Viruses (Herpes simplex, Cytomegalovirus, Varicella zoster)
Malignancies:
Kaposi’s sarcoma (Human Herpesvirus 8 /Kaposi sarcoma-associated herpesvirus)
Non-Hodgkin’s lymphoma (including Burkitt’s lymphoma)
Primary CNS lymphoma
Invasive cervical cancer
Increased rates of other cancers