Human Anatomy & Physiology: The Heart and Circulatory System
1/131
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
132 Terms
What are the two main circuits of the heart?
The pulmonary circuit and the systemic circuit.
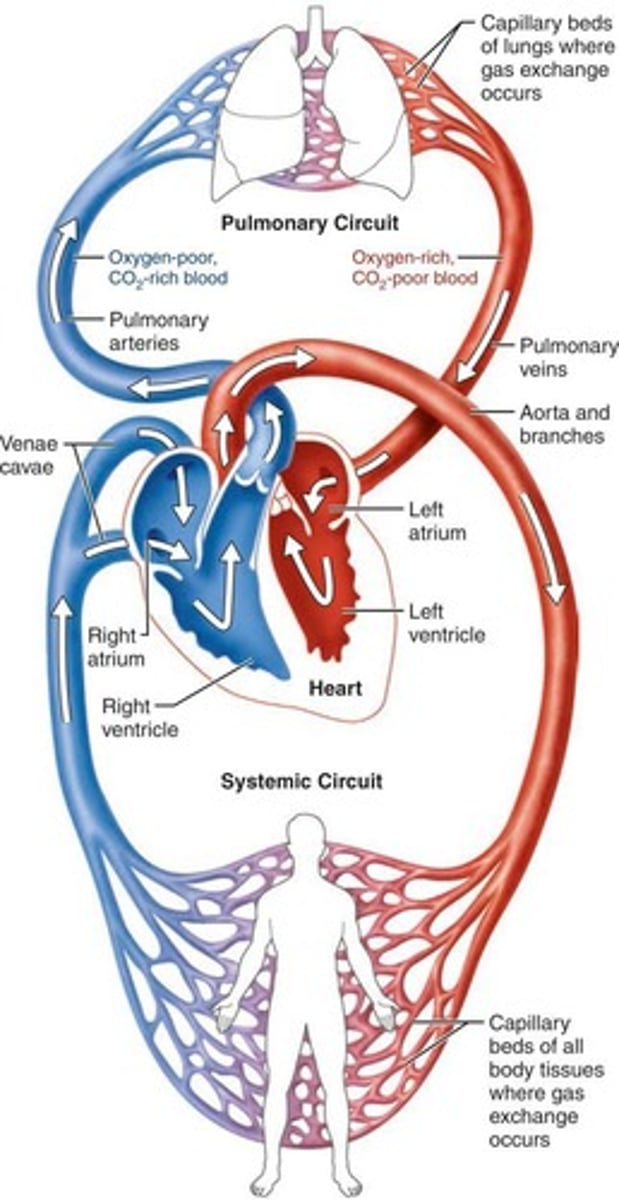
What type of blood does the right side of the heart receive and where does it pump it?
The right side receives oxygen-poor blood from body tissues and pumps it to the lungs.
What is the function of the pulmonary circuit?
It carries blood to and from the lungs to eliminate CO2 and pick up O2.
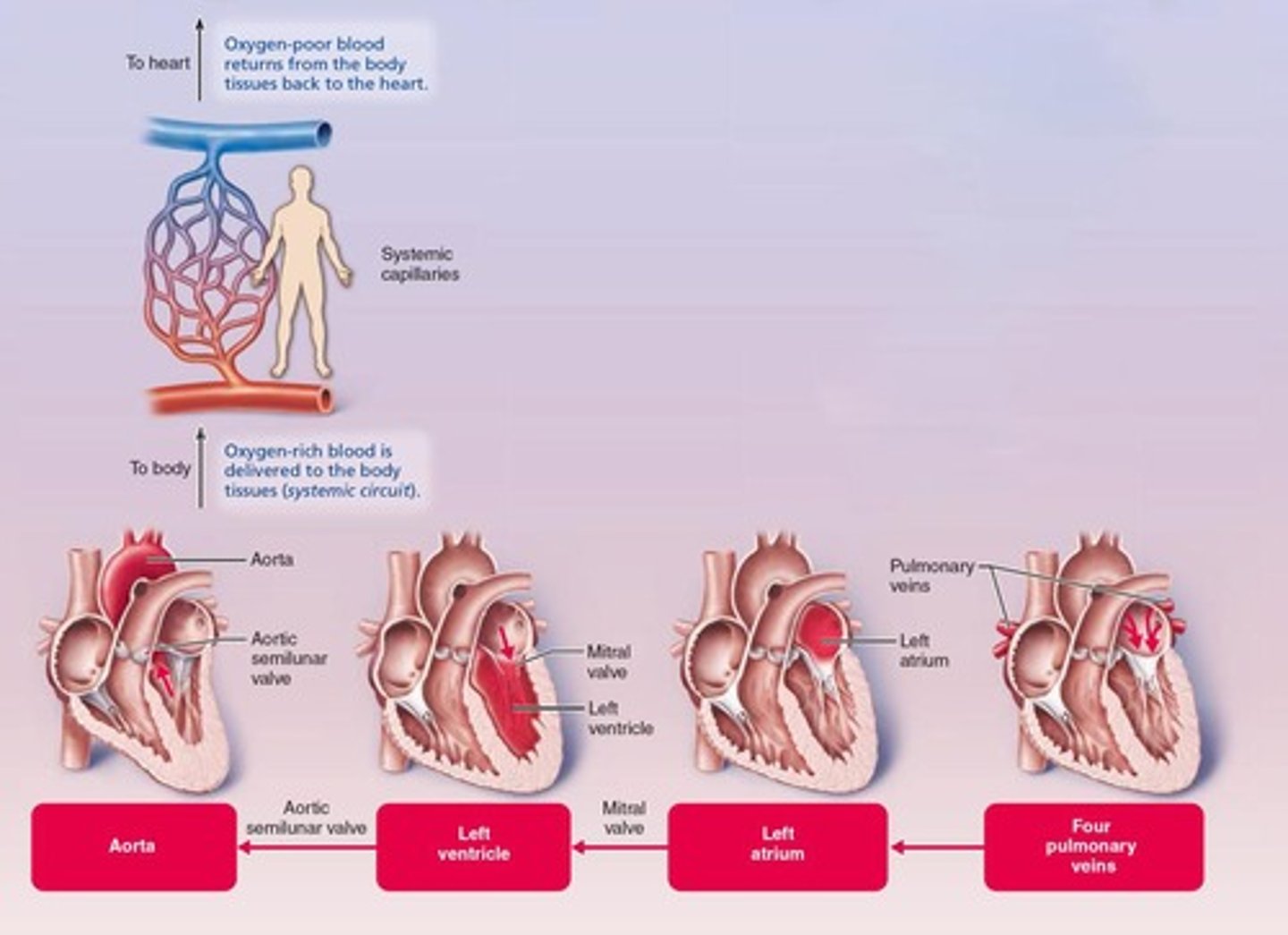
What type of blood does the left side of the heart receive and where does it pump it?
The left side receives oxygenated blood from the lungs and pumps it to the body tissues.
What is the function of the systemic circuit?
It carries blood to and from body tissues to deliver O2 and pick up CO2.
What are the receiving chambers of the heart?
The right atrium and left atrium.
What are the pumping chambers of the heart?
The right ventricle and left ventricle.
What is the role of the left ventricle in the cardiovascular system?
It pumps oxygenated blood into the aorta for distribution to the body.
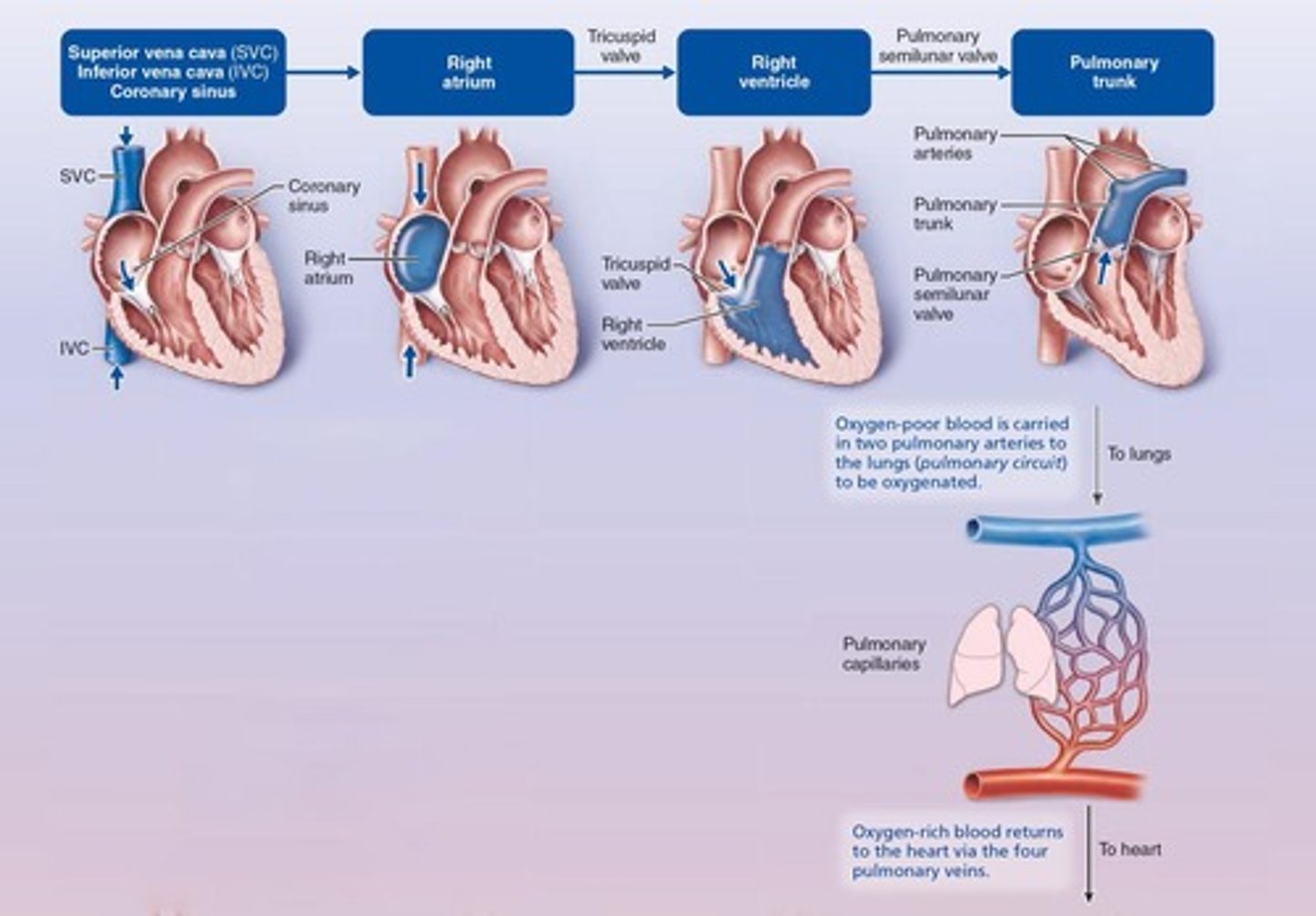
What is the role of the right ventricle in the cardiovascular system?
It pumps oxygen-poor blood into the pulmonary trunk for delivery to the lungs.
How do the workloads of the right and left ventricles compare?
Both ventricles move equal volumes of blood, but the left ventricle has a greater workload due to pumping into a longer, high-resistance systemic circuit.
What is the structure of the right ventricle compared to the left ventricle?
The right ventricle is crescent-shaped and pumps into a shorter, low-pressure pulmonary circuit, while the left ventricle is cylindrical and pumps into a longer, high-pressure systemic circuit.
What is angina pectoris?
Thoracic pain caused by a deficiency in blood delivery to the myocardium, leading to temporary lack of oxygen.
What is a myocardial infarction (MI)?
A prolonged coronary blockage causing areas of myocardial cell death, replaced with noncontractile scar tissue.
Why is damage to the left ventricle considered the most serious?
Because it is responsible for pumping oxygenated blood to the entire body, and damage can severely affect overall circulation.
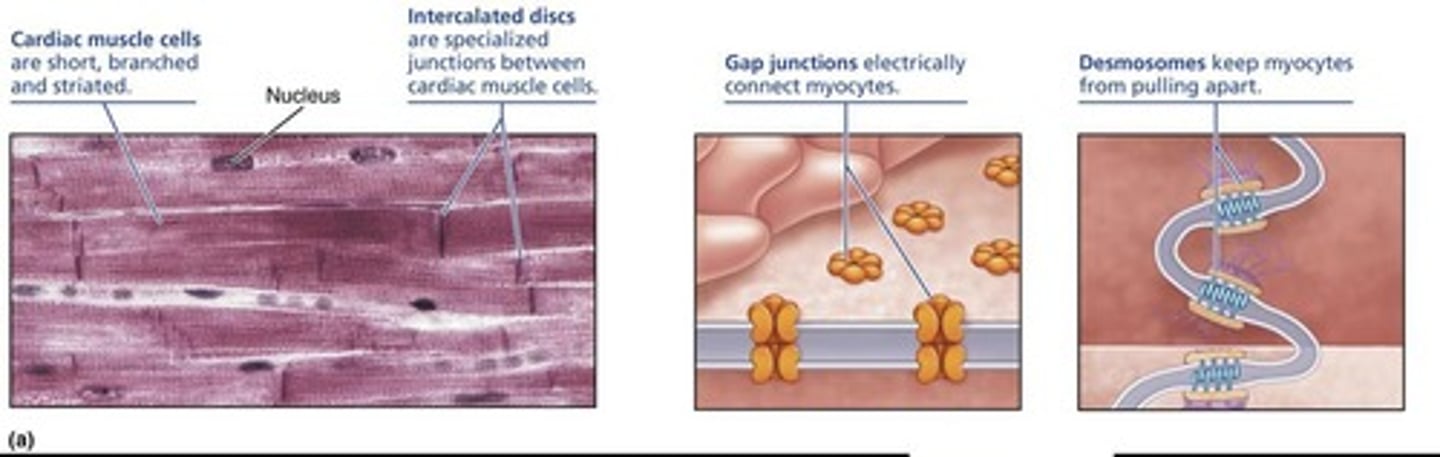
What anatomical feature connects cardiac muscle cells into a functional syncytium?
Intercalated discs.
How does cardiac muscle differ from skeletal muscle in terms of contraction?
Cardiac muscle is striated like skeletal muscle but has unique anatomical features that reflect its blood-pumping role.
What mechanism do cardiac muscle cells use to contract?
The sliding filament mechanism.
What are the characteristics of the pulmonary arteries?
They carry oxygen-poor blood to the lungs.
What are the characteristics of the pulmonary veins?
They return oxygenated blood to the left side of the heart.
What are the characteristics of systemic arteries?
They carry oxygenated blood to body tissues.
What are the characteristics of systemic veins?
They return oxygen-poor blood to the right side of the heart.
What is the relationship between the thickness of the left and right ventricle walls?
The left ventricle walls are three times thicker than the right ventricle walls.
What is the significance of the coronary arterial circulation?
Blockage can lead to serious conditions such as angina pectoris and myocardial infarction.
What are the characteristics of cardiac myocytes?
Cardiac myocytes are short, fat, branched, and interconnected, with one (sometimes two) centrally located nuclei.
What type of connective tissue fills the intercellular space in cardiac muscle?
Endomysium, which is loose connective tissue with many capillaries.
What is the function of intercalated discs in cardiac muscle?
Intercalated discs contain desmosomes that hold cells together and gap junctions that allow ions to pass cell-to-cell, enabling the myocardium to behave as a functional syncytium.
What is the significance of large mitochondria in cardiac muscle cells?
Numerous large mitochondria (about 35% of cell volume) provide resistance to fatigue.
What are the components of myofibrils in cardiac muscle?
Myofibrils are composed of sarcomeres, which include Z discs, A bands, and I bands.
How does muscle contraction begin in cardiac muscle?
Muscle contraction is preceded by a depolarizing action potential (AP).
What is the role of calcium ions in cardiac muscle contraction?
Calcium ions (Ca2+) bind to troponin to initiate the sliding filament mechanism during excitation-contraction coupling.
What distinguishes cardiac muscle cells from skeletal muscle cells?
Some cardiac muscle cells are self-excitable, with about 1% being pacemaker cells that spontaneously depolarize, unlike skeletal muscle which requires neural input.
What is the intrinsic cardiac conduction system?
It is a network of noncontractile (autorhythmic) cells that initiates and distributes impulses to coordinate depolarization and contraction of the heart.
What are pacemaker potentials?
Pacemaker potentials are unstable resting potentials in cardiac pacemaker cells that continuously depolarize, drifting slowly toward threshold.
What occurs during the depolarization phase of cardiac action potentials?
At threshold (about -40 mV), Ca2+ channels open, leading to a huge influx of Ca2+ and the rising phase of the action potential.
What happens during repolarization of cardiac pacemaker cells?
Ca2+ channels close and K+ channels open, causing an efflux of K+ that makes the interior of the cell membrane more negative.
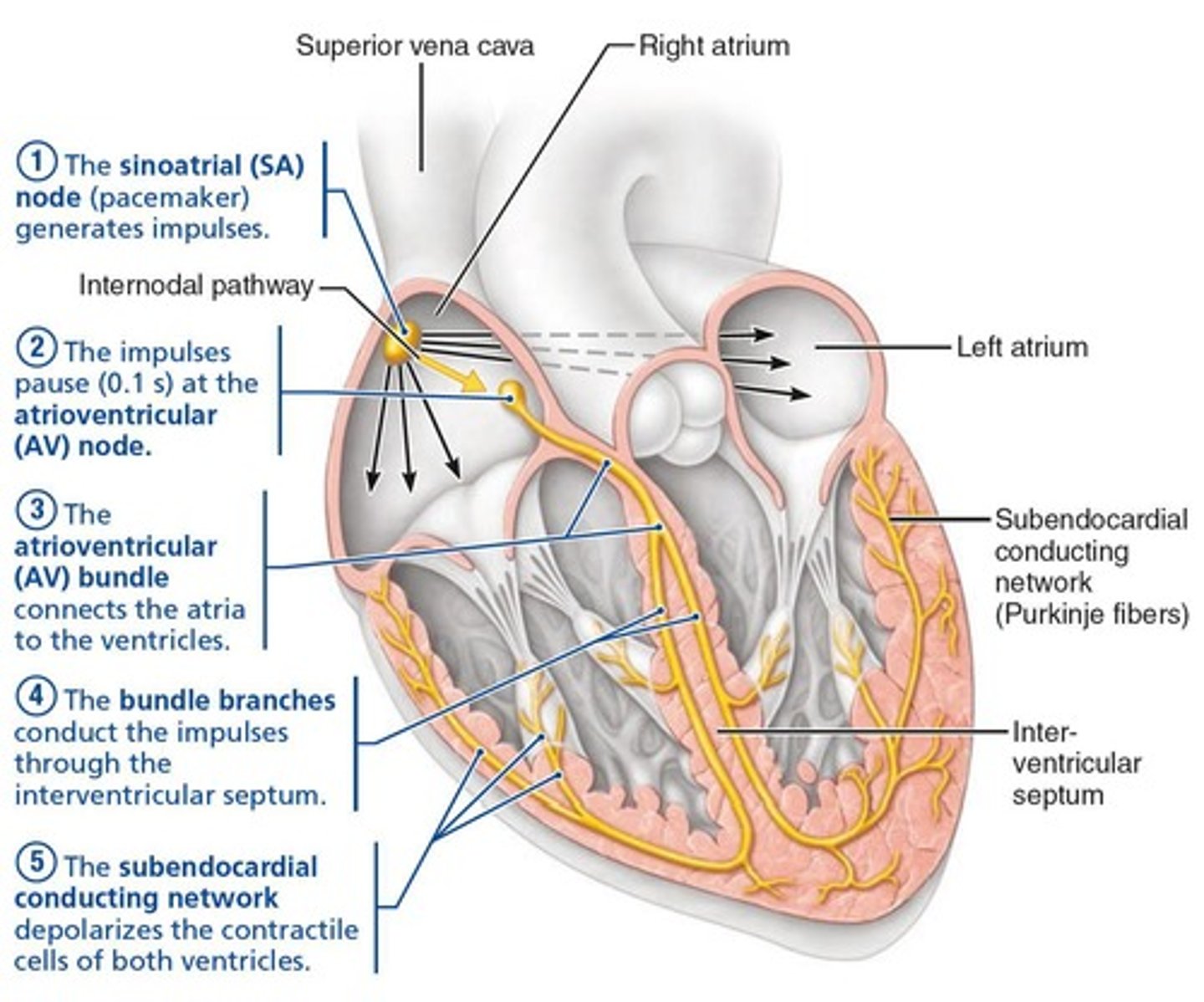
What is the sequence of excitation in the intrinsic conduction system of the heart?
The sequence is: Sinoatrial node → Atrioventricular node → Atrioventricular bundle → Right and left bundle branches → Subendocardial conducting network (Purkinje fibers).
How long does it take for impulses to pass across the heart in the conduction system?
It takes approximately 0.22 seconds.
What is the role of gap junctions in cardiac muscle?
Gap junctions allow for the transmission of action potentials without additional neural stimulation.
What percentage of cardiac myocytes are contractile cells?
About 99% of cardiac myocytes are contractile cells responsible for contraction.
What is the function of the autonomic nervous system in relation to the heart?
The autonomic nervous system adjusts the basic heart rhythm (rate) as needed.
What initiates the depolarization of the entire heart?
The spontaneous depolarization of pacemaker cells initiates the depolarization of the entire heart.
What is the main difference in the excitation-contraction coupling between skeletal and cardiac muscle?
In cardiac muscle, some cells are self-excitable and do not require neural input for contraction.
What is the significance of the fibrous skeleton in cardiac muscle?
The fibrous skeleton connects cardiac muscle to the endomysium, providing a structure for muscle cells to pull against.
What are the three phases of action potential in cardiac pacemaker cells?
The three phases are: 1) Pacemaker potential, 2) Depolarization, 3) Repolarization.
What causes the interior of cardiac pacemaker cells to become more positive during the pacemaker potential?
The closing of K+ channels and the opening of slow Na+ channels cause Na+ influx, making the interior more positive.
What is the function of the Sinoatrial (SA) node?
It acts as the heart's pacemaker, generating impulses at about 75 beats per minute and setting the heart's rhythm.
Where is the Sinoatrial (SA) node located?
In the right atrial wall below the entrance of the superior vena cava.
How does the impulse generated by the SA node spread through the heart?
The impulse spreads via gap junctions across the atria and to the AV node through the internodal pathway.
What is the role of the Atrioventricular (AV) node?
It delays impulses by about 0.1 seconds to allow for atrial contraction before ventricular contraction.
Where is the Atrioventricular (AV) node located?
In the inferior interatrial septum, above the tricuspid valve.
What is the inherent rate of the AV node in the absence of SA node input?
50 beats per minute.
What is the Atrioventricular (AV) bundle also known as?
The bundle of His.
What is the significance of the AV bundle?
It is the only electrical connection between the atria and ventricles.
What do the right and left bundle branches do?
They continue the conduction path down the interventricular septum after the AV bundle splits.
What is the function of the subendocardial conducting network (Purkinje fibers)?
It provides a complete path down the interventricular septum to the apex and then up the ventricular walls, facilitating ventricular contraction.
What is the rate of depolarization for the AV bundle and subendocardial conducting network without AV node input?
About 30 beats per minute.
How long does it take from initiation at the SA node to complete ventricular depolarization?
Approximately 0.22 seconds.
How does the autonomic nervous system modify the heartbeat?
Through cardiac centers in the medulla oblongata, with the cardioacceleratory center increasing heart rate and force of contraction, and the cardioinhibitory center decreasing heart rate.
What role does the sympathetic nervous system play in heart function?
It increases heart rate and force of contraction by targeting the SA and AV nodes, heart muscle, and coronary arteries.
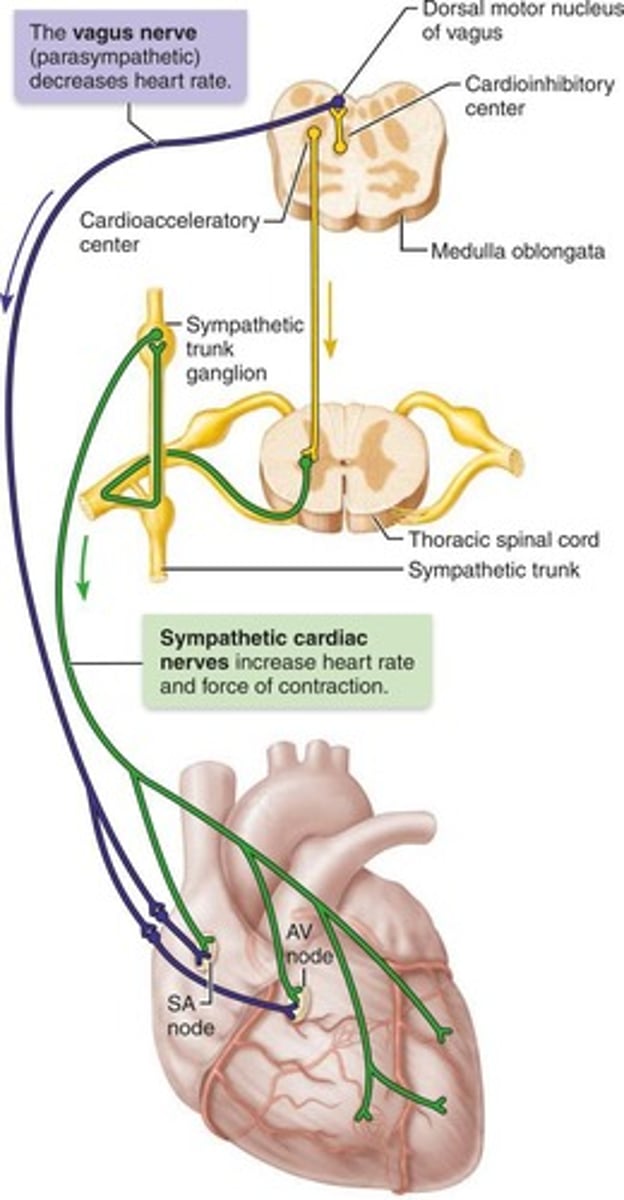
What is the effect of the parasympathetic nervous system on heart rate?
It decreases heart rate by sending signals via the vagus nerve to the SA and AV nodes.
What characterizes the action potentials of contractile cardiac muscle cells?
They have a plateau phase, which is different from skeletal muscle action potentials.
What triggers the rapid rising phase of the action potential in cardiac muscle cells?
The influx of Na+ through fast voltage-gated Na+ channels.
What happens after depolarization in cardiac muscle cells?
Slow Ca2+ channels open, prolonging the depolarized state and leading to muscle contraction.
What occurs during the repolarization phase of the action potential?
Voltage-gated K+ channels open, allowing K+ to exit the cell, which repolarizes the cell to resting membrane potential.
What happens to Ca2+ after the plateau phase of the action potential?
Ca2+ is pumped back into the sarcoplasmic reticulum and out of the cell into the extracellular fluid.
How does the action potential duration in cardiac muscle compare to that in skeletal muscle?
The action potential lasts 200+ ms in cardiac muscle, compared to 1-2 ms in skeletal muscle.
What is the benefit of the longer action potential in cardiac muscle?
It prevents tetanic contractions, ensuring the heart can fill before the next beat and allows for efficient ejection of blood.
What is an electrocardiogram (ECG or EKG)?
A graphic recording of the heart's electrical activity, representing the composite of all action potentials at a given time.
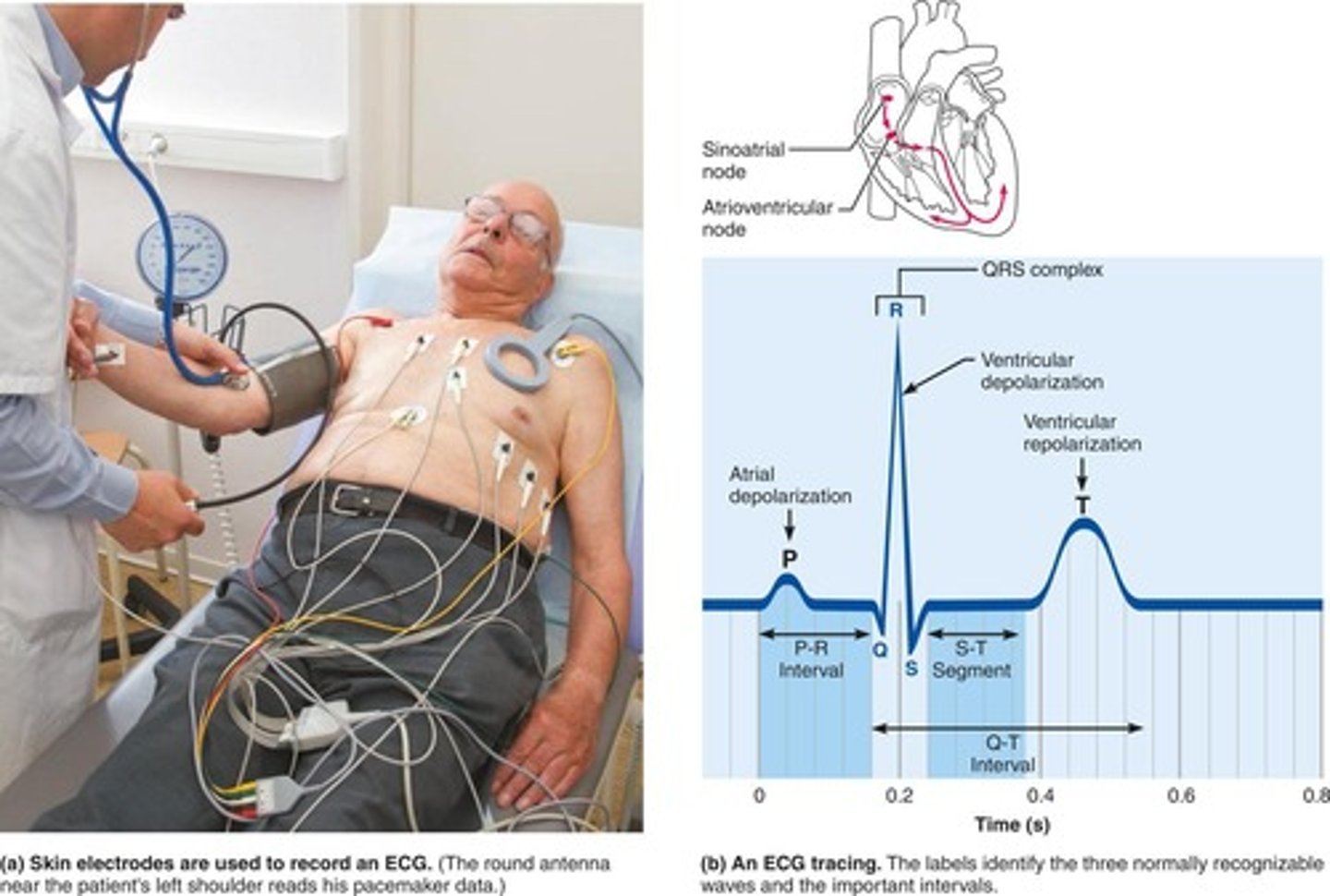
What does the P wave in an ECG represent?
The depolarization of the SA node and atria.
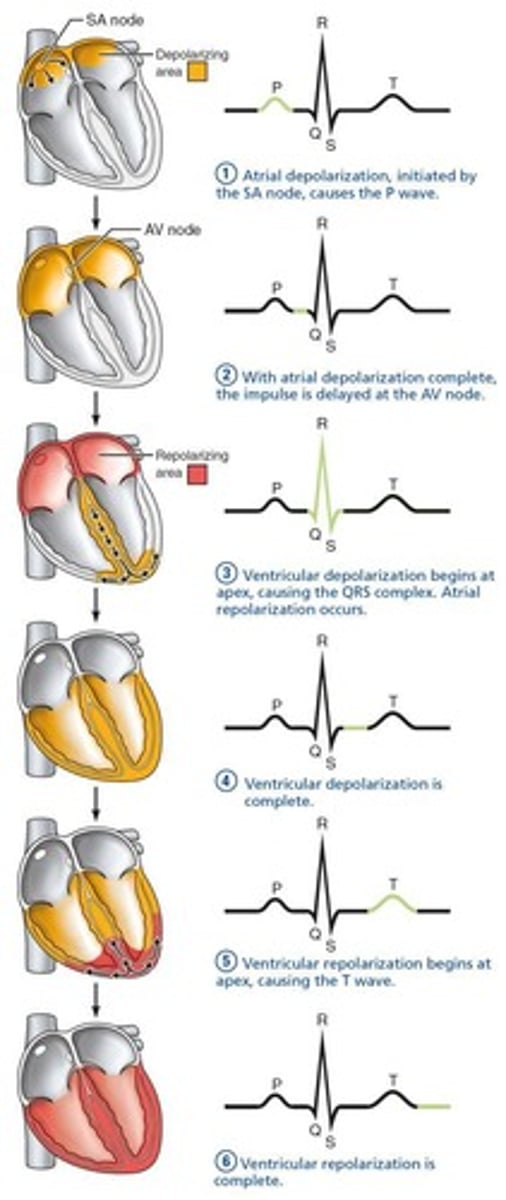
What does the QRS complex in an ECG indicate?
Ventricular depolarization and atrial repolarization.
What does the T wave in an ECG signify?
Ventricular repolarization.
What is the P-R interval in an ECG?
The time from the start of atrial depolarization to the start of ventricular depolarization.
What does the S-T segment in an ECG represent?
The entire ventricular myocardium depolarized, with cells in the plateau phase.
What is the Q-T interval in an ECG?
The time from the start of ventricular depolarization through ventricular repolarization.
What is systole in the context of the cardiac cycle?
The period of myocardial contraction.
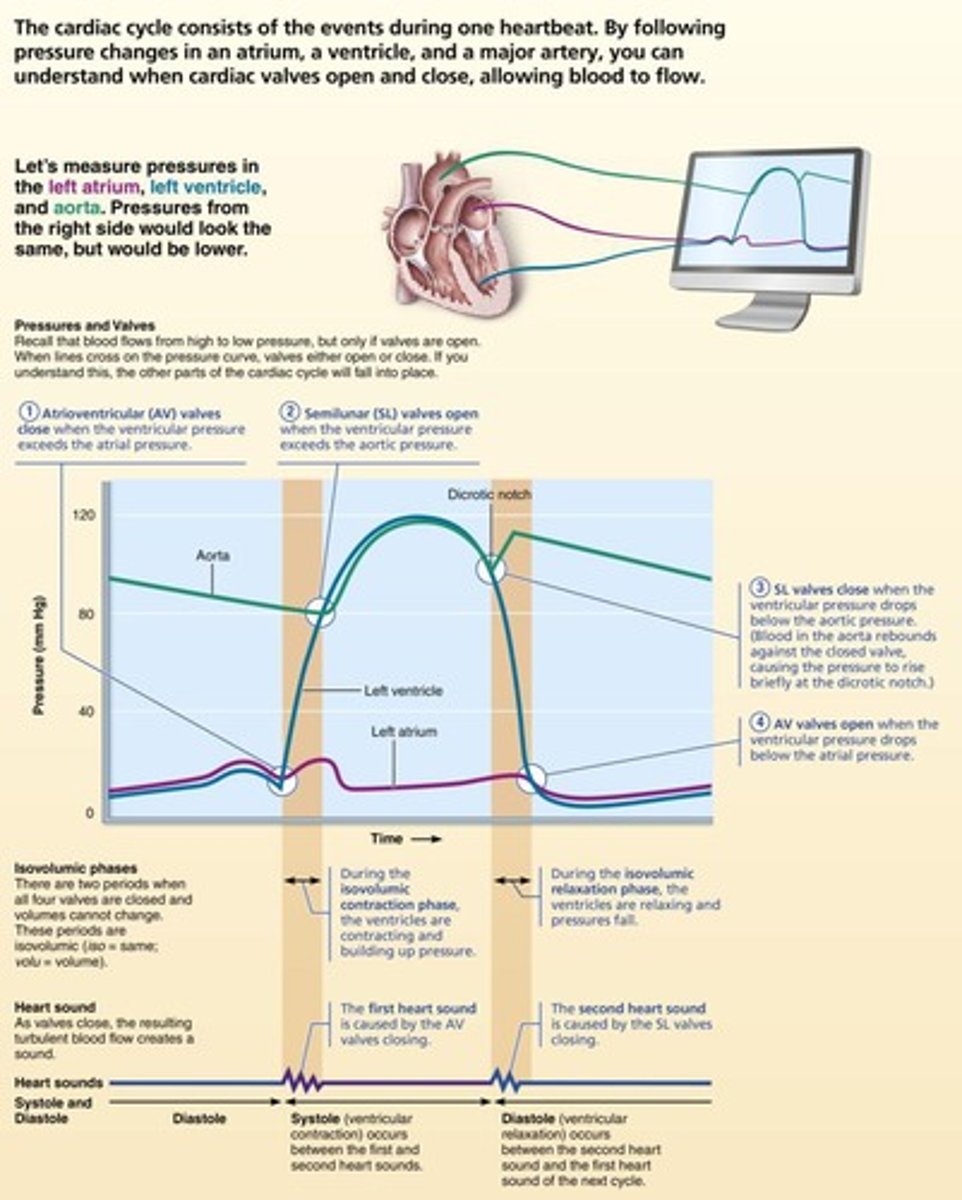
What is diastole in the context of the cardiac cycle?
The period of myocardial relaxation.
What does the cardiac cycle encompass?
All events associated with blood flow through the heart during one complete heartbeat, including ventricular and atrial systole and diastole.
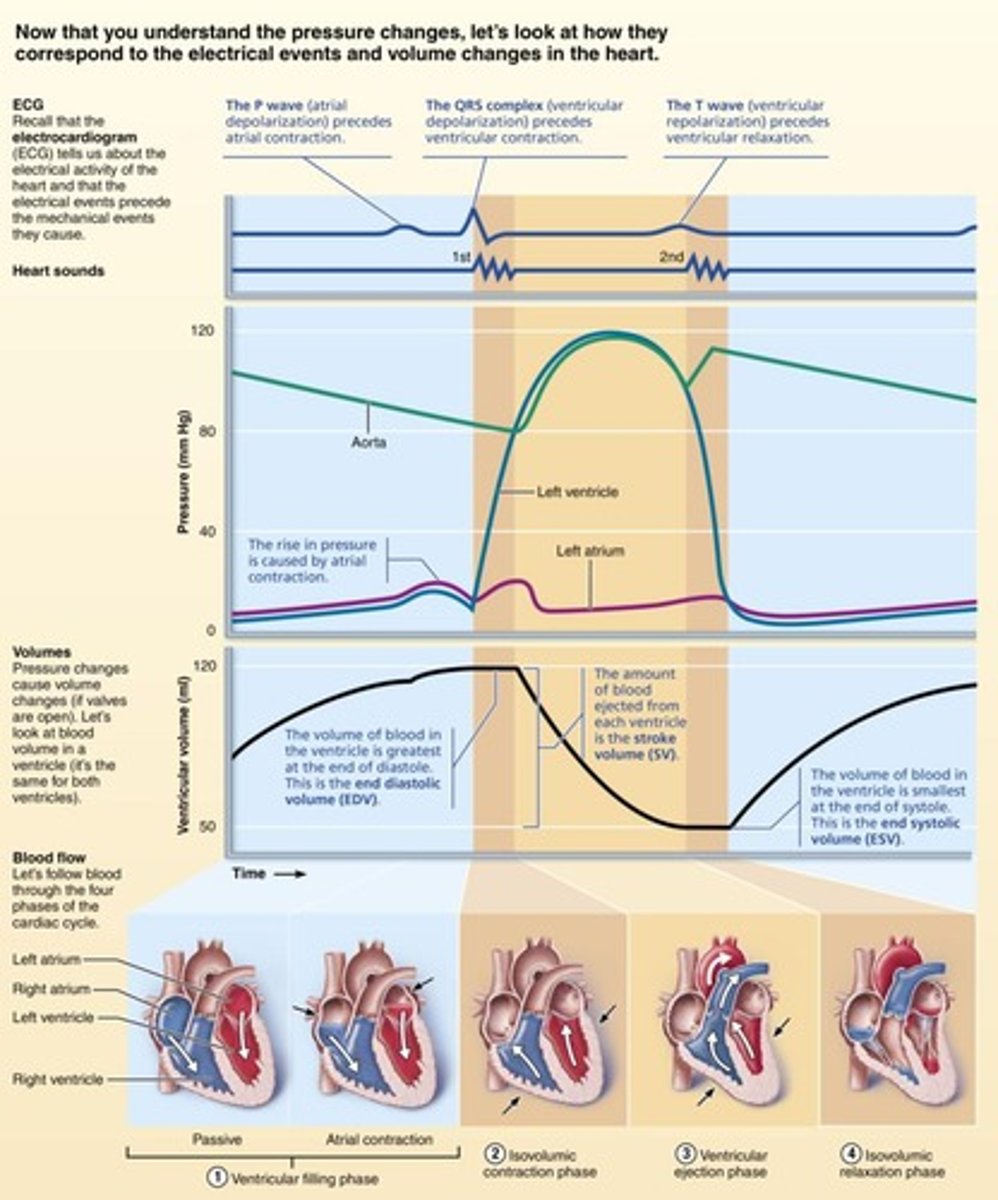
What occurs during the ventricular filling phase of the cardiac cycle?
Blood flows passively from veins through the atria into the ventricles, with atrial contraction contributing to the final filling.
What is end diastolic volume (EDV)?
The volume of blood in each ventricle at the end of ventricular diastole.
What happens during the isovolumic contraction phase?
Rising ventricular pressure causes AV valves to close, and all four valves are closed, preventing blood from entering or leaving the ventricle.
What triggers atrial systole in the cardiac cycle?
Atrial depolarization, represented by the P wave.
What is the significance of the plateau phase in cardiac muscle action potentials?
It prolongs the action potential and contraction duration, preventing tetany.
How does the cardiac cycle begin?
It starts in diastole with the atria and ventricles relaxed.
What is the role of the 12 lead ECG?
It is the most typical method of measuring voltage differences across the body to assess heart activity.
What does the QRS wave in an ECG indicate?
It indicates the depolarization of the ventricles.
What happens to the atria during ventricular systole?
The atria relax and return to diastole.
What is the relationship between the ECG waves and the heart's depolarization and repolarization?
The ECG waves represent the sequence of depolarization and repolarization of the heart.
What happens during ventricular ejection?
Once ventricular pressure exceeds arterial pressure, the semilunar (SL) valves open, allowing blood to enter the aorta and pulmonary trunk.
What are the pressures in the aorta and pulmonary trunk during ventricular ejection?
Pressure in the aorta reaches approximately 120 mm Hg, and pressure in the pulmonary trunk reaches approximately 24 mm Hg.
What occurs during isovolumic relaxation?
Following ventricular repolarization, the ventricles relax, causing a drop in ventricular pressure that triggers the closing of the SL valves.
What is end systolic volume (ESV)?
The volume of blood remaining in each ventricle after systole ends.
What is the dicrotic notch?
The closure of the aortic SL valve raises aortic pressure as backflow rebounds off closed valve cusps, creating a dicrotic notch.
What happens when atrial pressure exceeds ventricular pressure?
The atrioventricular (AV) valves open, allowing blood to flow from the atria to the ventricles.
How long does each cardiac cycle last at a heart rate of 75 beats per minute?
Each cardiac cycle lasts approximately 0.8 seconds.
What are the durations of atrial systole and ventricular systole?
Atrial systole lasts about 0.1 seconds, and ventricular systole lasts about 0.3 seconds.
What is the quiescent period in the cardiac cycle?
The quiescent period is the total heart relaxation phase, lasting about 0.4 seconds.
What is cardiac output (CO)?
Cardiac output is the amount of blood pumped out by each ventricle in one minute.
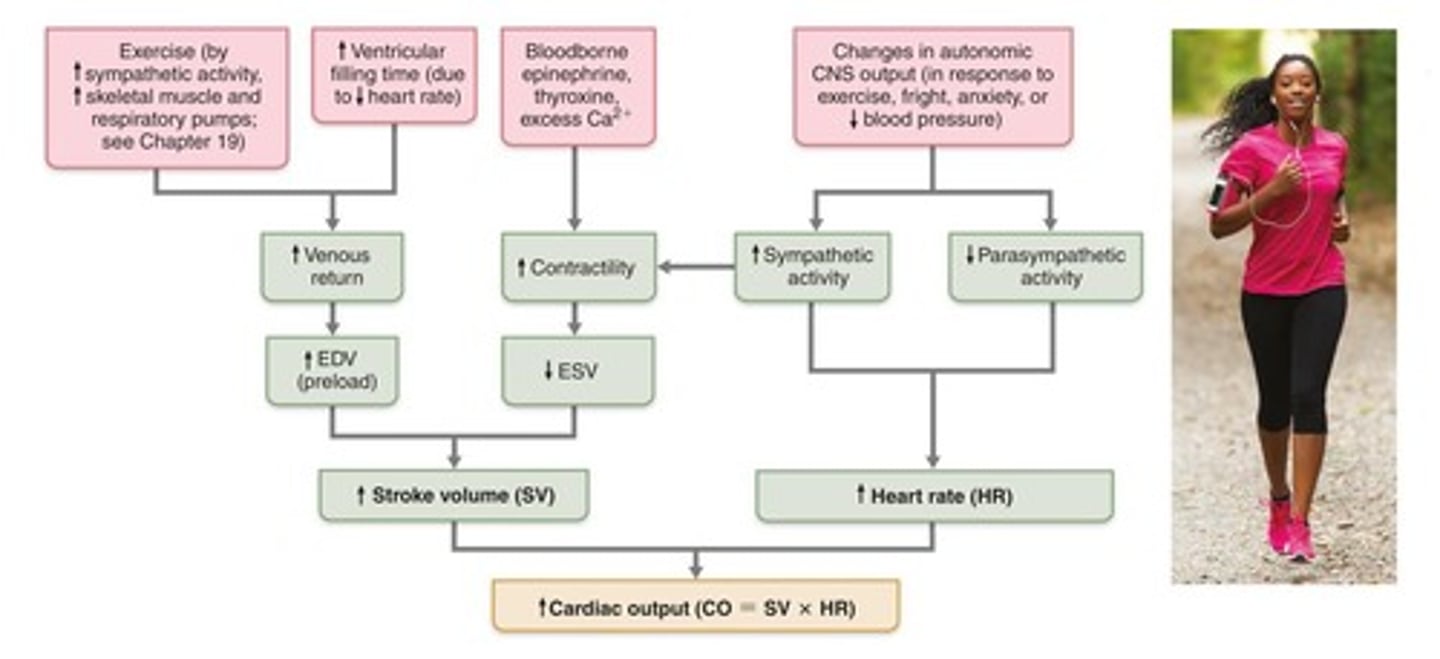
How is cardiac output calculated?
Cardiac output is the product of heart rate (HR) and stroke volume (SV).
What are the average resting values for heart rate and stroke volume in adults?
The average resting heart rate is 75 beats per minute, and the average stroke volume is 70 ml per beat.
What is the average cardiac output for an adult?
The average cardiac output is about 5.25 liters per minute.