NRS 326: Elimination/Detoxification and Final Exam
1/75
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
76 Terms
Pressure of urine in the bladder stimulates special sensory nerve endings, called stretch receptors, in the bladder wall when there's about 250-450 mL of urine in adults (50 to 200 mL for children)
What causes initial stimulation to urinate and how many mL are in the bladder when this occurs?
Blood Urea Nitrogen: 8 - 20 mg/dL
(*think of a BUNion which usually happens on the feet, there are 5 toes which is about 8 and there are 20 toes total so 8-20...)
BUN range
Serum Creatinine: 0.6 - 1.3 mg/dL
(creatiNINE= 0.9 is right in the middle of the range: 0.6-1.3)
Serum creatinine range
Below 15 ml/min = Kidney failure
Above 60 ml/min = okay
Above 90 ml/min = Normal
What is kidney failure range, ideal range and normal range for GFR?
indicates how well kidneys are working, high level would
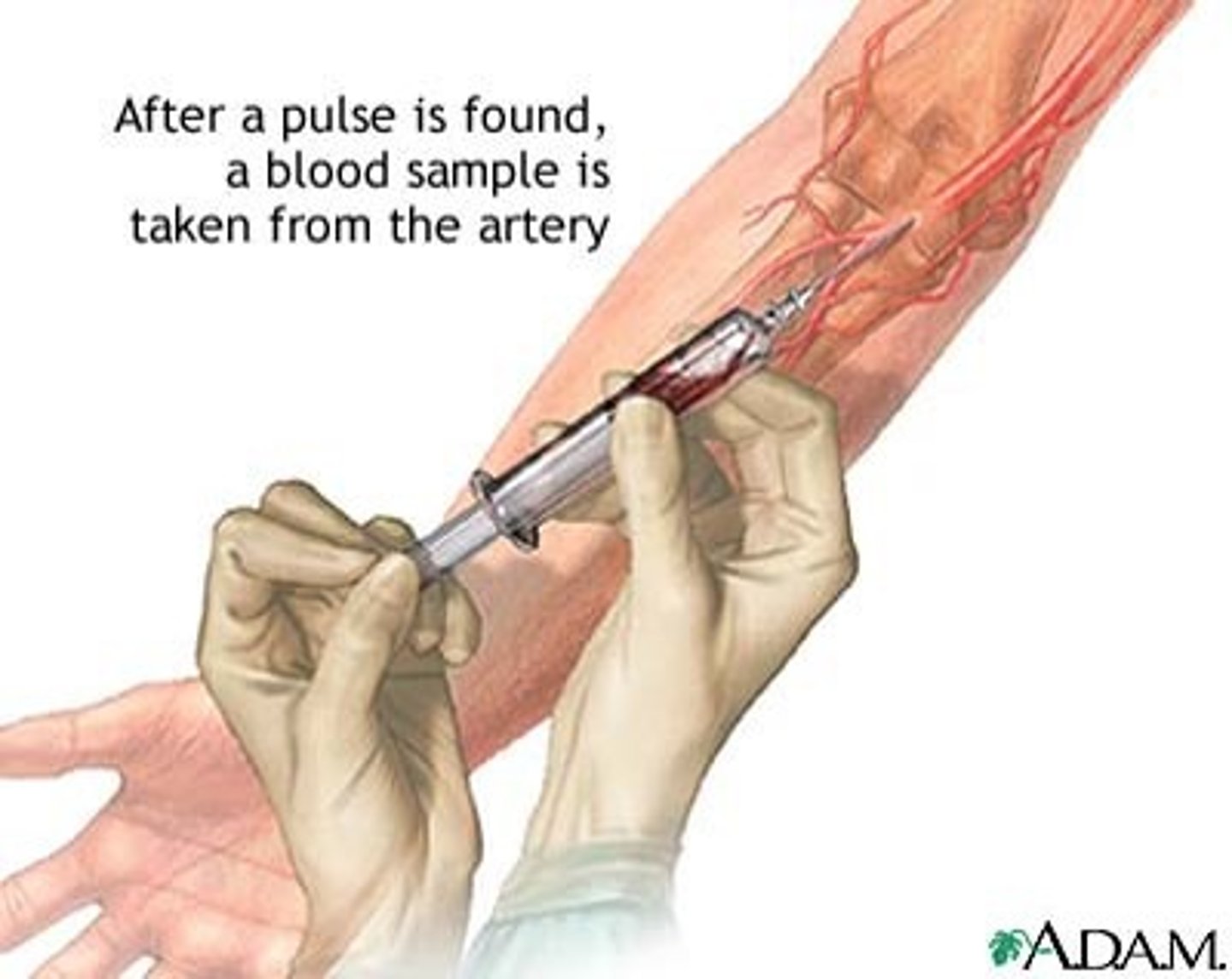
involves 24 hour urine collection and serum blood draw
What does the Creatinine clearance indicate and what is it?
Collecting pee over a 24-hour period is inconvenient. Instead, they usually use a blood test called the estimated glomerular filtration rate (eGFR) coupled with a urine test like urine albumin-creatinine ratio (uACR), which only involves peeing one time.
Why don't healthcare provides use creatinine clearance tests as often anymore?
Ammonia, also known as NH3, is a waste product that bacteria in your intestines primarily make when digesting protein
NH3 is normally processed in the liver to urea and then excreted as urea by the kidneys
High ammonia can build up and cause damage because it easily crosses the BBB
Most common cause of high levels is liver problems
What does the serum ammonia level indicate?
Bilirubin is a waste product produced by the breakdown of red blood cells. Bilirubin is the end-product of heme metabolism; the liver is the site for bilirubin metabolism
high levels indicate liver damage
(At times, conditions such as a blockage of the liver ducts or certain types of anemia also can lead to elevated bilirubin)
What does the bilirubin level indicate?
ALT metabolizes proteins
AST breaks down amino acids
high levels indicate liver dysfunction
What do the ALT/AST (Liver function tests) levels indicate?
Proteins break down to ammonia which is turned into urea in the liver by liver enzymes then the urea travels via bloodstream to the kidneys where they are excreted in urine
High levels of BUN indicate kidney problems, while high ammonia indicates liver problems
(urea is less toxic than ammonia)
Describe the urea pathway? What would high BUN levels indicate?
3.4-5.4
Lower-than-usual levels o may mean liver damage or disease (also malnutrition)
(protein shake gas 3,4,5 ingredients)
Albumin range. What would low levels indicate>
1.8-2.6
(Magnesium a Mini car has room for 2-3 people)
Mg2+ range
8.2-10.2
(CAlifornia has big earthquakes, richter scale 8-10ish)
Ca2+ range
3.5-5.2
(bananas come in bunches of 3-5ish)
K+ range
135-145
(sODium, odd numbers 1,3,5)
Na+ range
pH 7.35-7.45
HCO3- 22-26
PaCO2 34-45
PaO2 75-100
ABG lab ranges
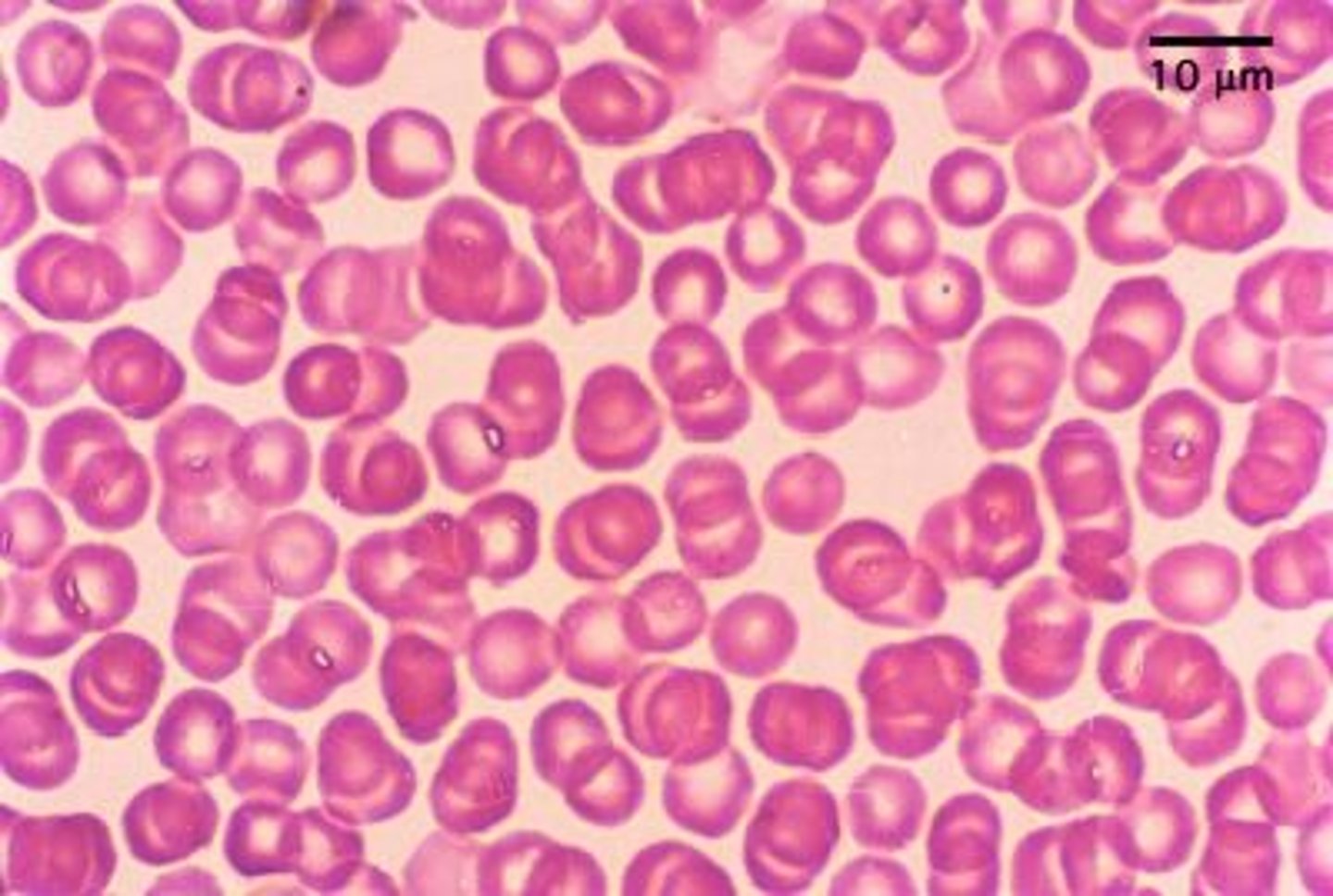
RBC 3.6-5.4
(3,4,5,6 just not in order)
Hct 36-48%
Hv 12-17.4
(RR is about 12-18)
RBC range
Hct range
Hb range
4,500-11,000
(Want to Buy a Car for about $4k-10k)
WBC range
assess clotting ability and monitor anticoagulant therapy
PT/INR- extrinsic pathway (warfarin)
PTT intrinsic pathway (heparin)
What do PTT and PT/INR measure?
skin breakdown
changes in daily activity
social isolation
What can incontinence lead to?
discomfort/pain
urine backflow to ureters and kidneys causing increased risk of infection (pyelonephritis) and bladder injury
Feces can contribute to constipation/impaction
What can retention of urine or feces lead to?
stress-increased abdominal pressure
urge- involuntary contraction of the bladder (and you feel the urge)
reflex -involuntary contraction of the bladder (and you don't feel the urge)
overflow-bladder fills up and overflows due to blockage of the urehtra (like w/BPH) or they don't feel the urge (may be most dangerous because it can stretch too much or reflux urine up into ureters and kidneys)
functional-problems getting to the bathroom once you feel the urge, decreased mobility, bedrest, children etc.
Name five types of incontinence. Briefly describe each one. Which one is the most dangerous?
dysuria
frequency
urge incontinence
What are some some signs of UTI?
1. Fiber/bulk forming agents (psyllium, metamucil)
2. Osmotic laxatives in small doses (polyethlylene glycol, milk of magnesia)
3. Surfactant/stool softener (docusate sodium)
4. Bowel stimulants (bisocodyl, senna)
Order the laxatives we talked about from most to least gentle
loperamide
would not want to suppress diarrhea if the body is getting rid of toxins like cholera- we don't want toxins to accumulate
(fiber can also help with diarrhea)
What is the antidiarrheal we talked about? When would we not want to suppress diarrhea?
acute surgical abdomen, fecal impaction, bowel obstructions, severe abdomen pain, cramps, appendicitis, UC,
When are laxatives contraindicated
pregnant/breastfeeding- ask provider first (stool softeners are often okay)
Avoid magnesium and phosphate if patient has kidney problems (milk of magnesia and sodium polyethlyene glycol- the osmotic laxatives)
In what situation should caution be used when giving laxatives
full glass of water because they work better and you want to avoid FVD
What should you take laxatives with?
Do not crush or chew Bisacodyl
Senna may turn urine red/brown which is harmless
What is one specific patient teaching for bisacodyl and one for senna?
to treat diarrhea and to reduce volume of discharge from ileostomies
Do not crush or chew
When would we give loperamide and what patient teaching to provide?
bethanechol to promote bladder emptying to treat urinary retention and overflow incontinence
(doesn't treat underlying issue)
What is the cholinergic med we talked about and what is it used for in relation to elimination?
oxybutynin to decrease bladder spasm to treat urge and reflex incontinence
(doesn't treat underlying issue)
What is the cholinergic med we talked about and what is it used for in relation to elimination?
structural problems
BPH
opioids
What are some things that can cause urinary retention
azotemia- elevated BUN and creatinine (indicates kidney dysfunction)
Uremia- seeing S&S of those increased waste
Define aztomeia and uremia
ammonia because it can easily cross the BBB and cause neuron dysfunction (hepatic encephalopathy)
What is more toxic: ammonia or urea? Why?
asterixis (neurologic irritability- hand tremor/bounce)
Changes in personality
agitation
restlessness
impaired judgement
slurred speech
confusion
disorientation
(similar to alcohol intoxication symptoms)
What are signs and symptoms of high ammonia levels?
early signs- nausea, apathy, weakness, fatigue that continues to worsen
possibly to mental status changes and organ dysfunction
(less toxic than ammonia)
What are signs and symptoms of high urea/creatinine levels?
liver disease/cirrhosis
The following symptoms are likely indicative of what disease?
esophageal varices
abdominal pain
anorexia
ascites
nausea,
clay-colored stool
peptic ulcers
GI Bleed
hemmorrhoids
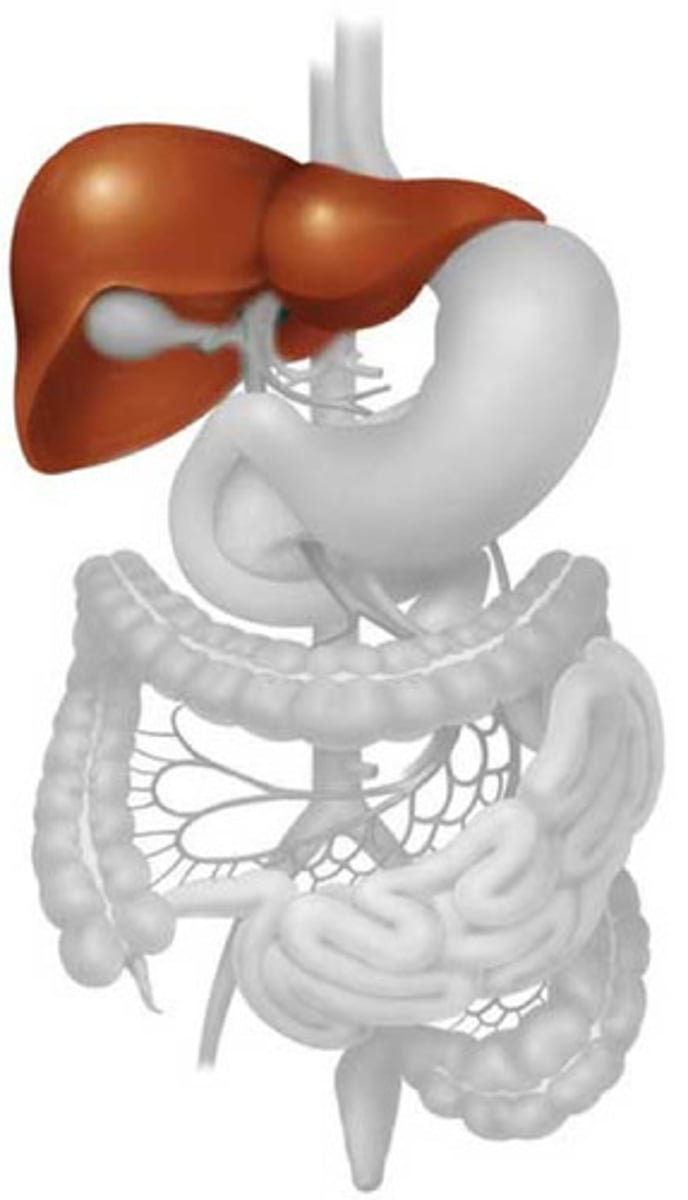
-Glycogen storage
-Secretion of bile (breaks down lipids)
-Stores fat-soluble vitamins (ADEK, and B12 (water soluble))
-Protein synthesis (metabolism of food)
-Production of clotting factors
-Medication breakdown
Name 6 functions of the liver
eliminate urine
balance electrolytes
balance acid-base
Name 3 functions of the kidney
K+
phosphate (lots of sodas have high levels)
protein
What are some things in the diet that should be restricted with chronic kidney disease?
Pros: montioring and help from medical professionals, faster and more powerful
Cons: needles, larger fluid shifts, often have to go into clinic, limit potassium (may be recommended to limit protein too...)
What are pros and cons of hemodialysis compared to peritoneal dialysis?
Pros: often done at home, can be portable machine, smaller fluid shifts (gentler) less protein restriction, no potassium restriction
Cons: not a candidate if you've had abdominal surgeries, no heavy lifting because you may dislodge catheter
What are pros and cons of peritoneal dialysis compared to hemodialysis?
removes waste from the body
required in end stage renal disease to replace kidney function
removes urea/creatinine, removes fluid, balances electrolytes and acid base
May also be used in cirrhosis to remove ammonia in hepatic encephalopathy flares
What is dialysis used for? (are there times when it could assist with liver problems?)
connection that a surgeon makes between an artery and a vein (takes a few months to be ready)
Check for patency:
palpate for thrill
ascultate for bruit
(if you can't hear and feel them it may be clotted)
What is a dialysis fistula? How to assess a fistula?

inspect catheter insertion site/look for signs of infection/inflammation
drainage should be clear NOT CLOUDY
What to assess before peritoneal dialysis?
osmotic laxative (its a non digestible sugar)
decreases ammonia levels and may be used to treat constipation
PO or PR (traps ammonia in the GI tract and decreases its production)
What is lactulose? What routes is it given
diarrhea
(patients in liver failure may need to take this forever)
What is a side effect for lactulose?
Regular toileting
hydration
diet, including fiber
mobility
Med reconciliation (are they taking meds that cause constipation?)
meds to prevent constipation high risk patients
What are five general primary prevention strategies to keep constipation from occurring in the first place?
Constipation can lead to fecal impaction.
Assessments for fecal impaction: Abdominal discomfort/pain, distension, palpable mass of stool. Patients may have no recent BMs, very small BMs, or overflow diarrhea. May cause urinary retention if increasing pressure on urethra
What is the relationship of constipation to fecal impaction? How might a nurse be able to assess for / or identify if a patient is impacted?
stool softeners: D. Often soften by letting more water in and coating stool so that it is easier to pass
bulk forming: C. Add bulk by introducing fiber, drawing water towards the stool. Bulk can help stimulate peristalsis
bowel stimulants: A. Directly act on the intestine to trigger peristalsis. Often more effective, but can contribute to painful cramping
osmotic laxatives: B. Cause fluid shifts to draw water into the colon.
Match the laxative types to the following descriptions
stool softeners:
bulk forming:
bowel stimulants:
osmotic laxatives:
A. Directly act on the intestine to trigger peristalsis. Often more effective, but can contribute to painful cramping
B. Cause fluid shifts to draw water into the colon.
C. Add bulk by introducing fiber, drawing water towards the stool. Bulk can help stimulate peristalsis
D. Often soften by letting more water in and coating stool so that it is easier to pass
Overuse can lead to painful cramps and diarrhea and fluid/electrolyte/acid-base imbalance, laxative dependence
Many are NOT for long term use
What risks are associated with the overuse of laxatives? What can we teach patients about taking these medications safely?
Did you do it?
Do Google docs exam questions!!
Likely caused by kidneys (adrenals) not producing erythropoietin. Decreased perfusion to kidney can impact the function of the adrenal gland , contributing to possible hormone regulation issues.
Why are RBCs low in CKD?
N/V/D and abdominal cramps, muscle weakness
(EKG changes)
Decreased kidney function can result in hyperkalemia, as the kidneys may not be able to excrete extra potassium. What are signs and symptoms of hyperkalemia the nurse should educate patients to report?
Peritonitis - Abd pain, fever, gi changes, cloudy dialysate - NOTIFY PROVIDER
Skin infection - redness, inflammation, drainage - Notify provider
Low back pain
Disturbed body image
What are 4 potential complications that can arise from peritoneal dialysis?
Abd pain, fever, gi changes, cloudy dialysate - NOTIFY PROVIDER
What are signs of peritonitis?
Asterixis is a tremor of the hand when the wrist is extended, also described as a flapping tremor. This motor disorder is characterized by an inability to maintain a position, which is demonstrated by jerking movements of the outstretched hands when bent upward at the wrist. https://www.youtube.com/watch?v=sEnp2ss8VoA
What is asterixis? Describe the finding and how you assess.
"Breath of the dead" - Caused by toxic substances (that are not being detoxified by the liver) travelling to other parts of the body, such as the lungs. Traces of the substances can be exhaled and are detectable. (Normally described as smelling like a mixture of rotten eggs and strong garlic, although sometimes described as sweet) Likely related to the sudden hepatic encephalopathy
What is fetor hepaticus
Proteins circulating in the blood break down into amino acids, which break down into ammonia. Ammonia is also produced by normal flora of the GI tract. A healthy liver will take ammonia and convert it into urea, a form that can be excreted by the kidneys in the urine. A diseased liver can't perform this function well, and ammonia accumulates in the blood stream. This toxin easily crosses over the blood-brain barrier and causes impairment of brain/neurological function.
How does hepatic encephalopathy develop?
Difficulty thinking
· Personality changes, poor concentration
· Confusion, forgetfulness, poor judgment
· A musty or sweet breath odor
· Problems with handwriting or loss of other small hand movements -
What are signs and symptoms of hepatic encephalopathy
Lactulose. Medication in a sugary syrup (and osmotic laxative) that pulls water into the bowel also trapping ammonia and excreting it in the form of stool - usually diarrhea. Lactulose is also a treatment for constipation.
What med do you anticipate will be given for hepatic encephalopathy and how does it work?
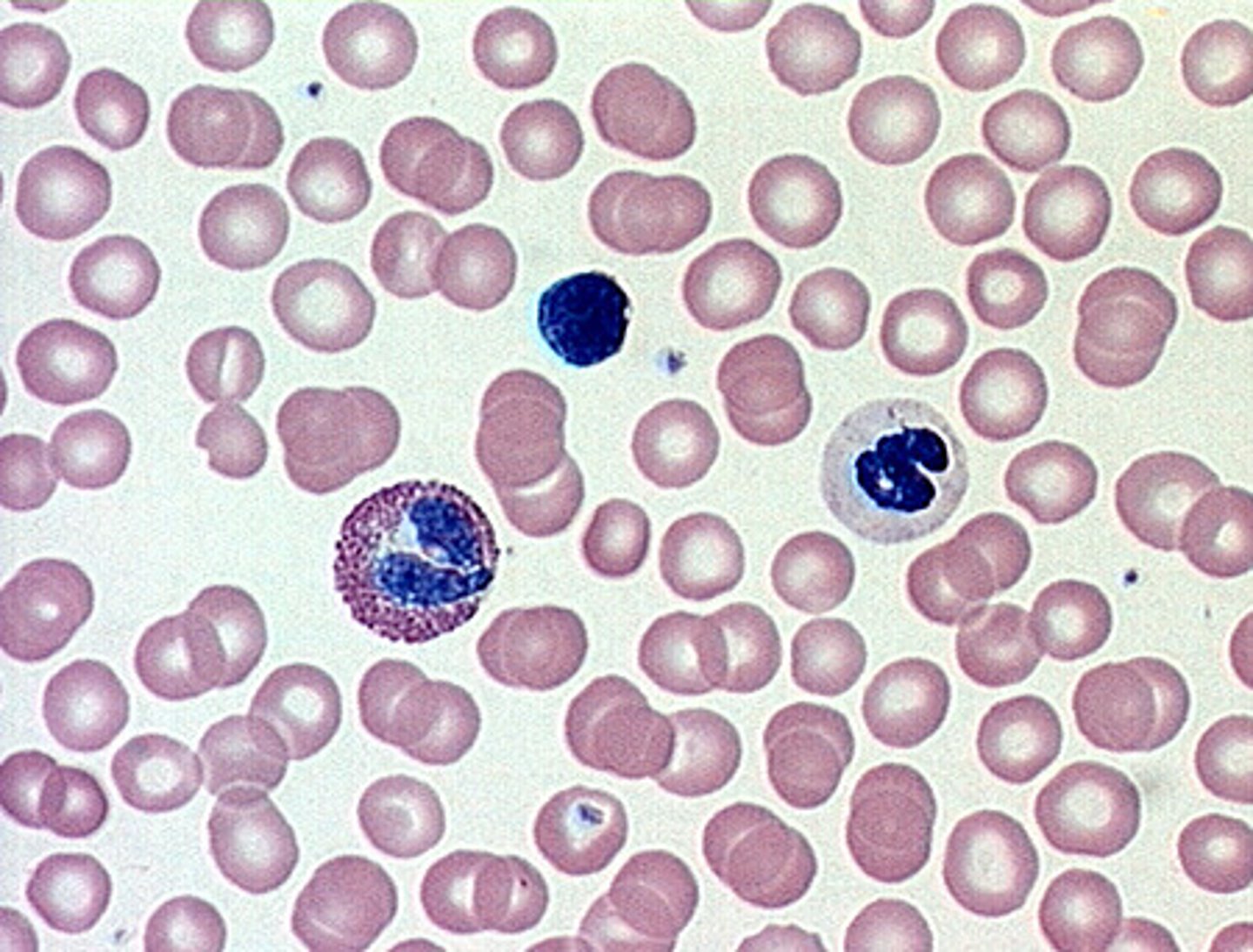
Enlargement of the spleen (splenomegaly). Portal hypertension can also cause changes to and swelling of the spleen and trapping of white blood cells and platelets. Decreased white blood cells and platelets in your blood can be the first sign of cirrhosis.
Why might WBC and platelet count be altered in a patient with cirrhosis?
white blood cells and platelets due to portal HTN and enlargement of the spleen that traps white blood cells and platelets
Decreased ____________ and ____________in your blood can be the first sign of cirrhosis.
decreased production of proteins leading to anemia, or low count possible from bleeding of ruptured varices
(Amino acids are transported to the liver during digestion and most of the body's protein is synthesised in the liver)
Why might RBC/HgB/Hct be low in a patient with cirrhosis?
the liver synthesizes proteins like albumin. A diseased liver cannot.
(decreased albumin can lead to ascites)
Why might albumin levels be low in a patient with cirrhosis?
high- b/c a healthy liver usually metabolizes it and when it can't it builds up and can lead to jaundice
How might bilirubin levels be altered in a patient with cirrhosis and why?
elevated liver enzyme with liver damage
What would AST and ALT levels look like in a patient with cirrhosis
Fluid from ascites is in the peritoneal cavity. When laying down that fluid will push on the diaphragm, pushing it upward into the lungs and interfering with movement and respiratory capacity. Position the patient by sitting them up!
What position should you put a patient with severe ascites in and why?
IV albumin
Fluid/sodium restrictiion
paracentesis
K+ sparing diuretic
(the liver isn't breaking down aldosterone so K+ is lost and sodium and water are retained)
What are some anticipated treatments for ascites?
Cirrhosis compresses the blood vessels running through the liver and reduces their blood flow causing portal HTN, smaller vessels are not able to accommodate higher pressures and develop varices as a result. Major complication is the risk of bleeding (major bleeding in the esophagus or slower bleeds that are detected in the stool)
How do esophageal and gastric varices develop in a patient with liver failure? What complications can arise because of them?
In type 2 diabetes the lack of insulin doesn't allow glucose uptake in cells so the body attempts to provide by breaking down lipids (lipolysis) into ketoacids which causes metabolic acidosis
How does DKA happen?
3 P's, Kussmaul respirations, fatigue (no glucose available for cellular metabolism), Fluid Volume Deficit/ dehydration signs (tachycardia, cool extremities, weak pulses, massive urine output), fruity-smelling breath (ketosis). If untreated, DKA will result in profound acidosis, coma, and death.
What are signs and symptoms of DKA
To avoid rapid change in dextrose
Reversing DKA safely is a process that usually takes 12-24 hours or more, depending on severity
The following is in an order for a patient with DKA:
Once blood glucose < 300 mg/dL, change IV fluids to: D5 0.45% NS with 40 mEq KCl / L = Hypertonic solution
Why is dextrose added? How long does reversing DKA usually take?
rapid drop in serum osmolality can cause cerebral edema
so DON'T allow the patient to drink unrestricted volumes of water even if they're thirsty (try toothettes)
Assess for neuro changes
In a patient with DKA: What complication could develop in a patient who has been extremely dehydrated, and suddenly has a very low serum osmolality? What will you as the nurse assess and monitor for?
DKA is causing osmotic diuresis
A patient in DKA's heart rate, blood sugar, and blood pressure in the ED all supported a finding of fluid volume deficit. Yet the ED nurse reported 500 mL of urine production. Why would this patient, who is likely profoundly dehydrated, keep urinating