Restrictive Lung Disease
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
18 Terms
how do we define pulmonary restriction
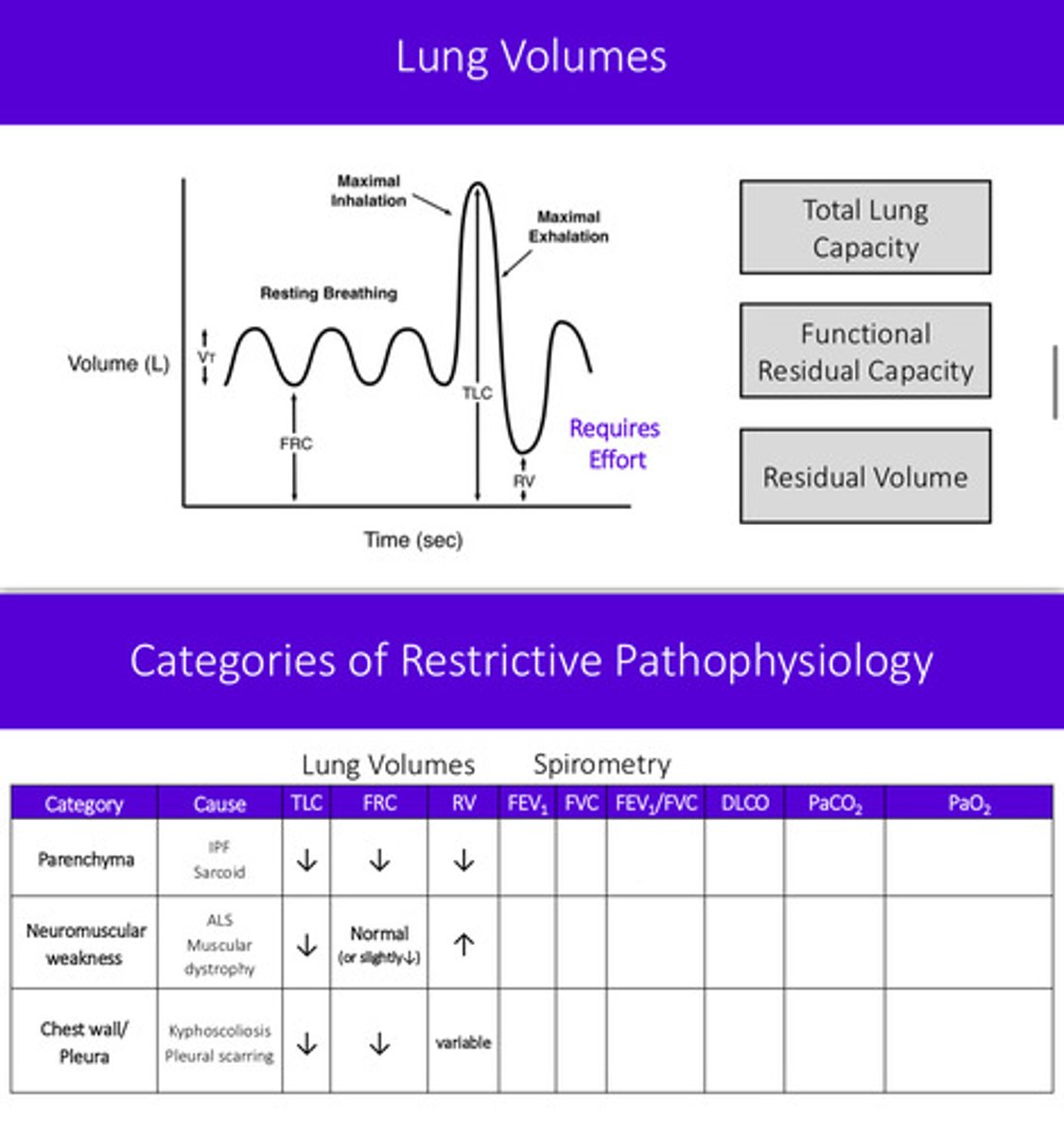
a decrease in total lung capacity (TLC); TLC less than lower limit of normal (z-score less than -1.645)
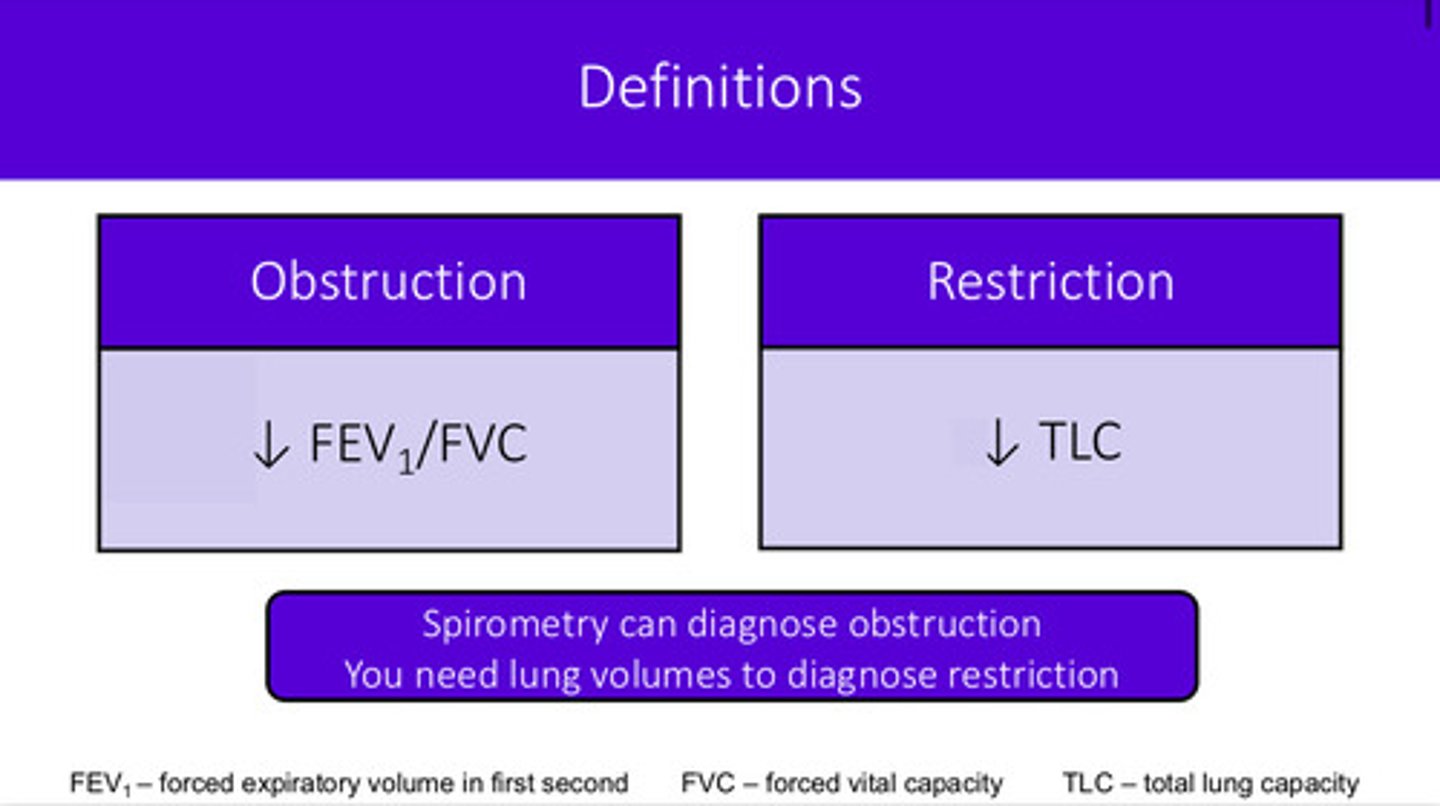
how can we diagnose restriction?
lung volumes!! (TLC and RV); spirometry can diagnose obstruction but we need the lung volumes
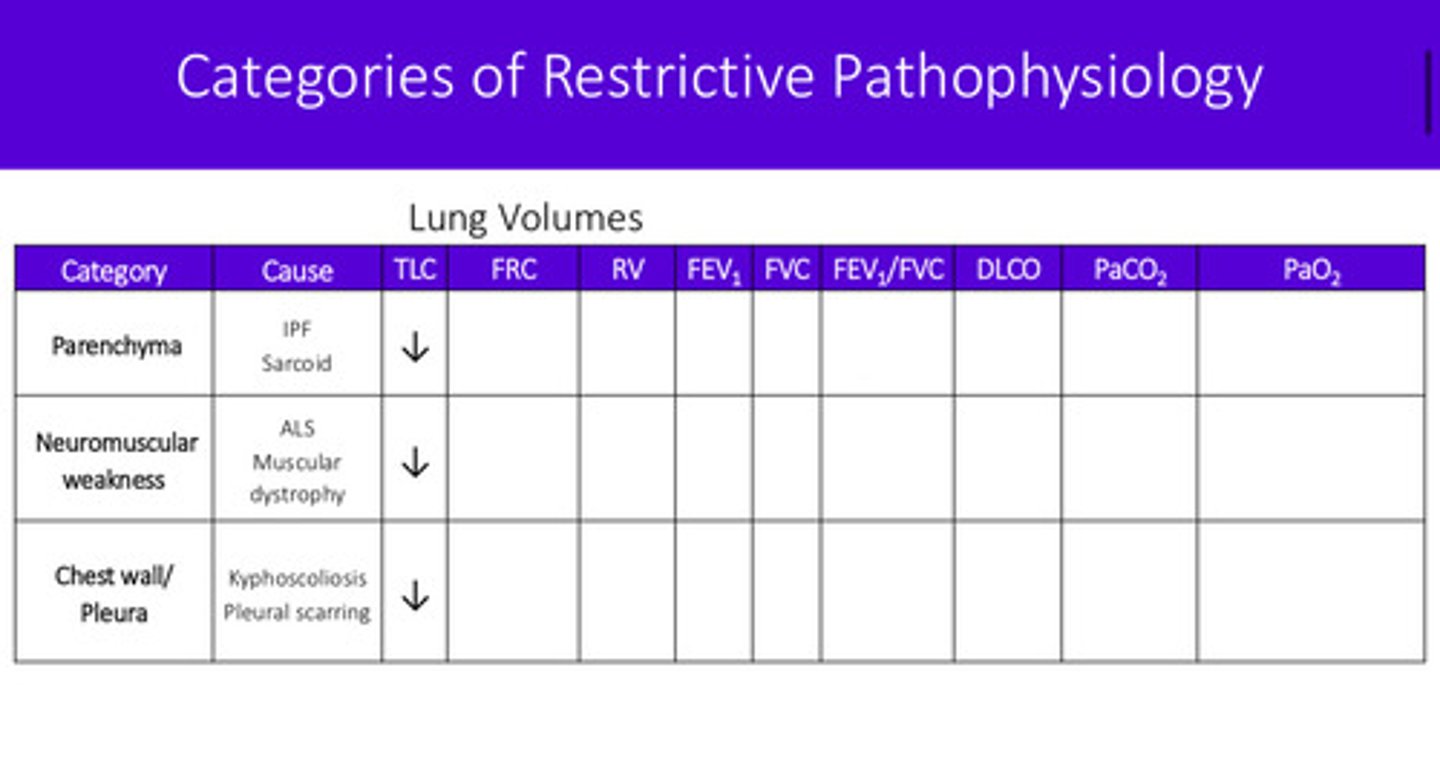
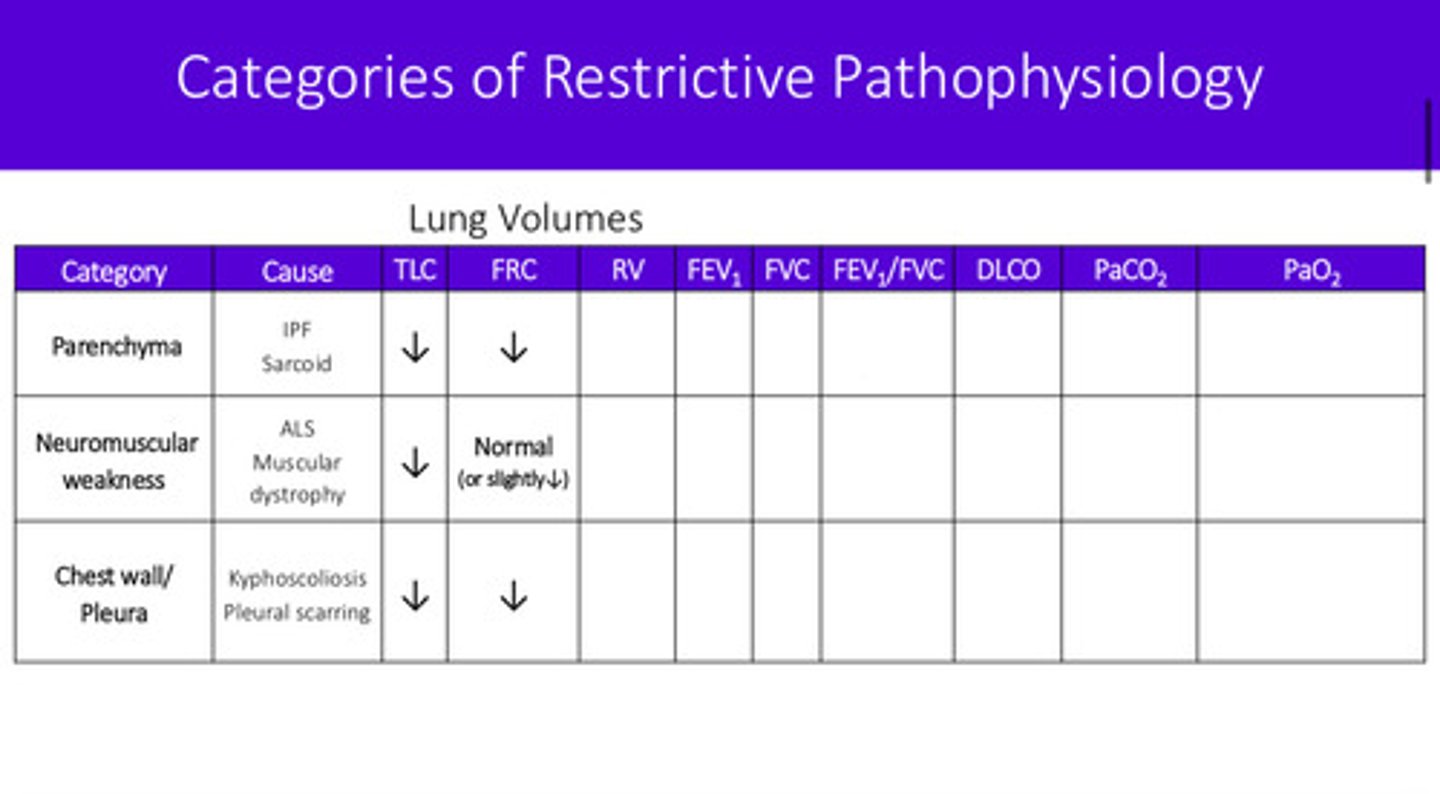
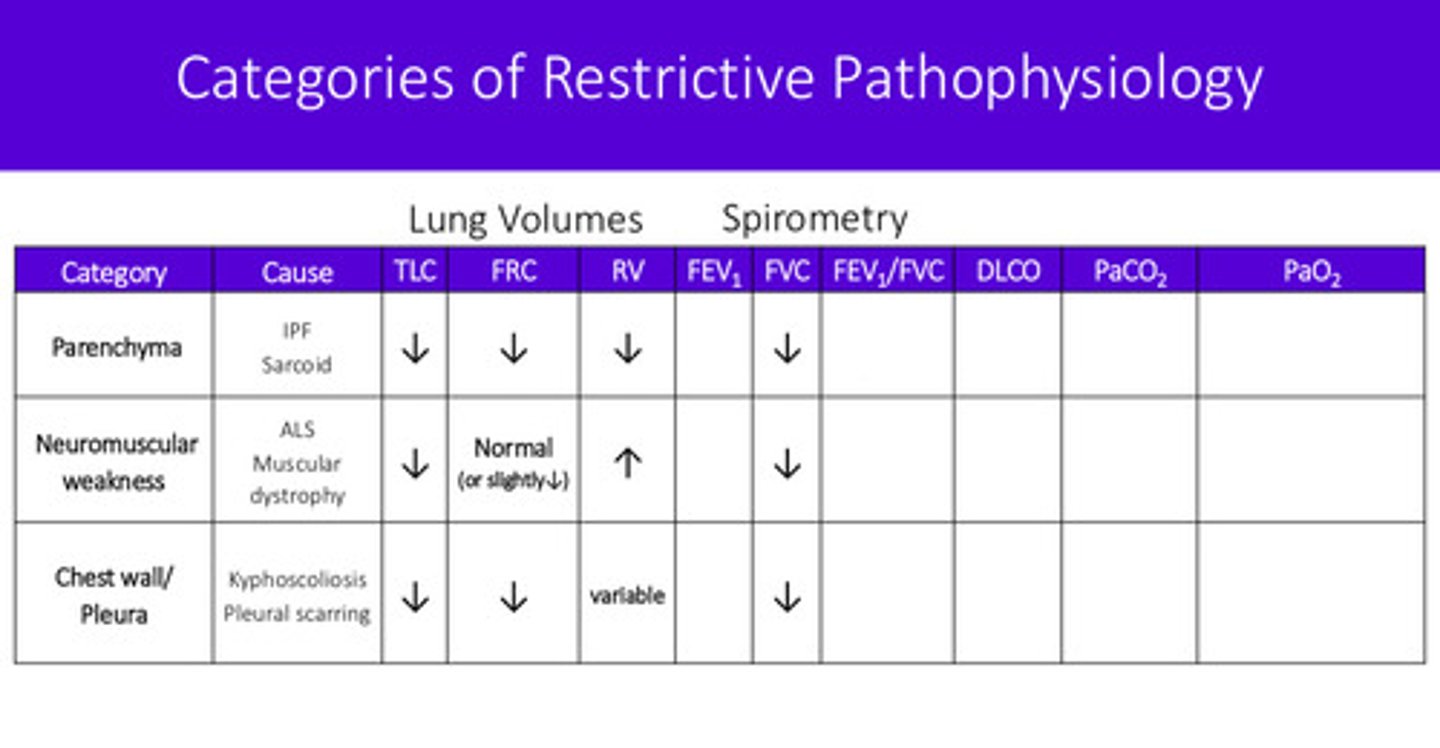
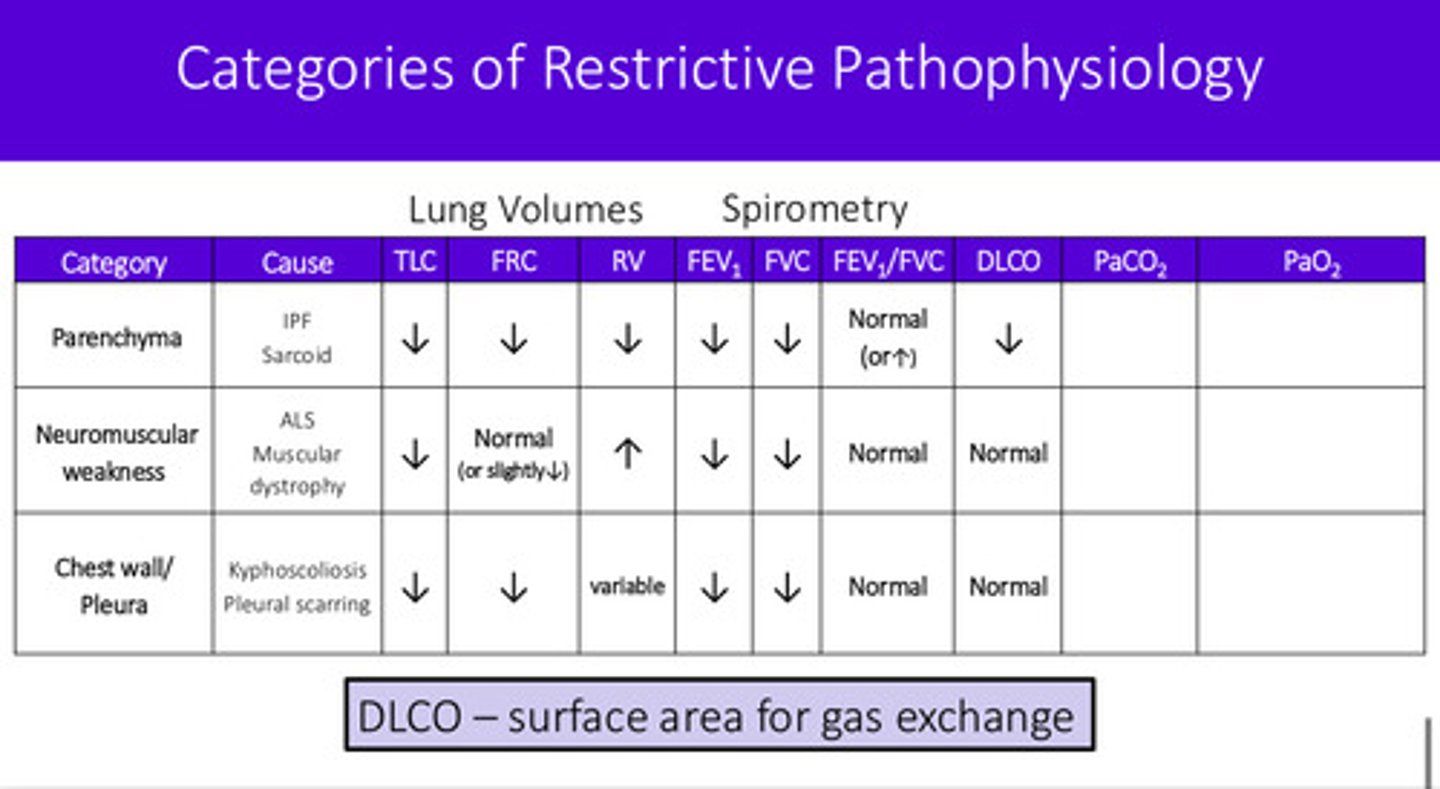
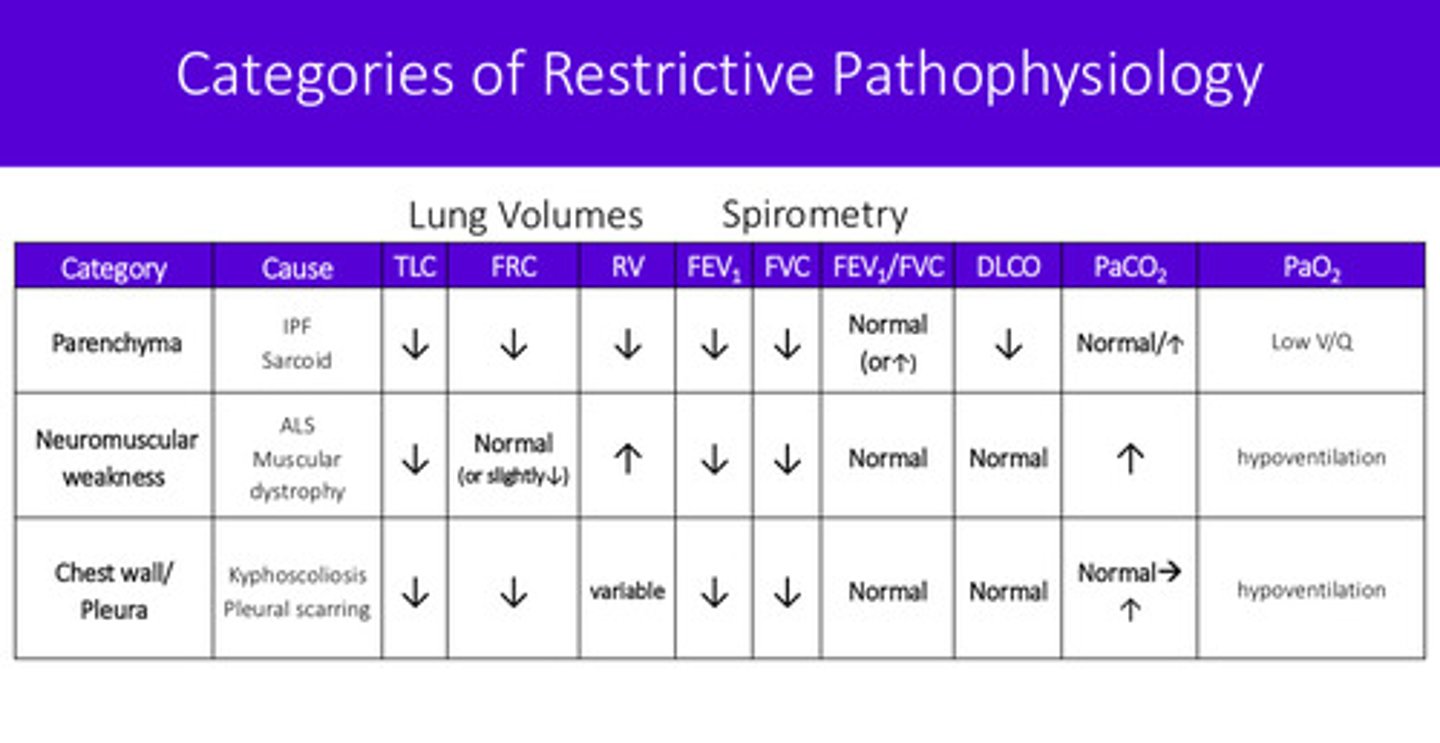
what are the 3 buckets of restrictive lung disease and what are some examples of causes for each
1) lung parenchyma —> IPF (idiopathic pulmonary fibrosis), black lung disease, asbestosis, sarcoid
2) neuromuscular weakness (cannot take a big enough breath due to weakness) —> ALS (amyotrophic lateral sclerosis), GBS (guillain-barre syndrome), polio, muscular dystrophy
3) chest wall/pleura (chest wall is stiff or pleura has something in it) —> kyphoscoliosis, pleural scarring, pleural effusions
what is the biggest bucket of restrictive lung disease (has the most causes)
lung parenchyma
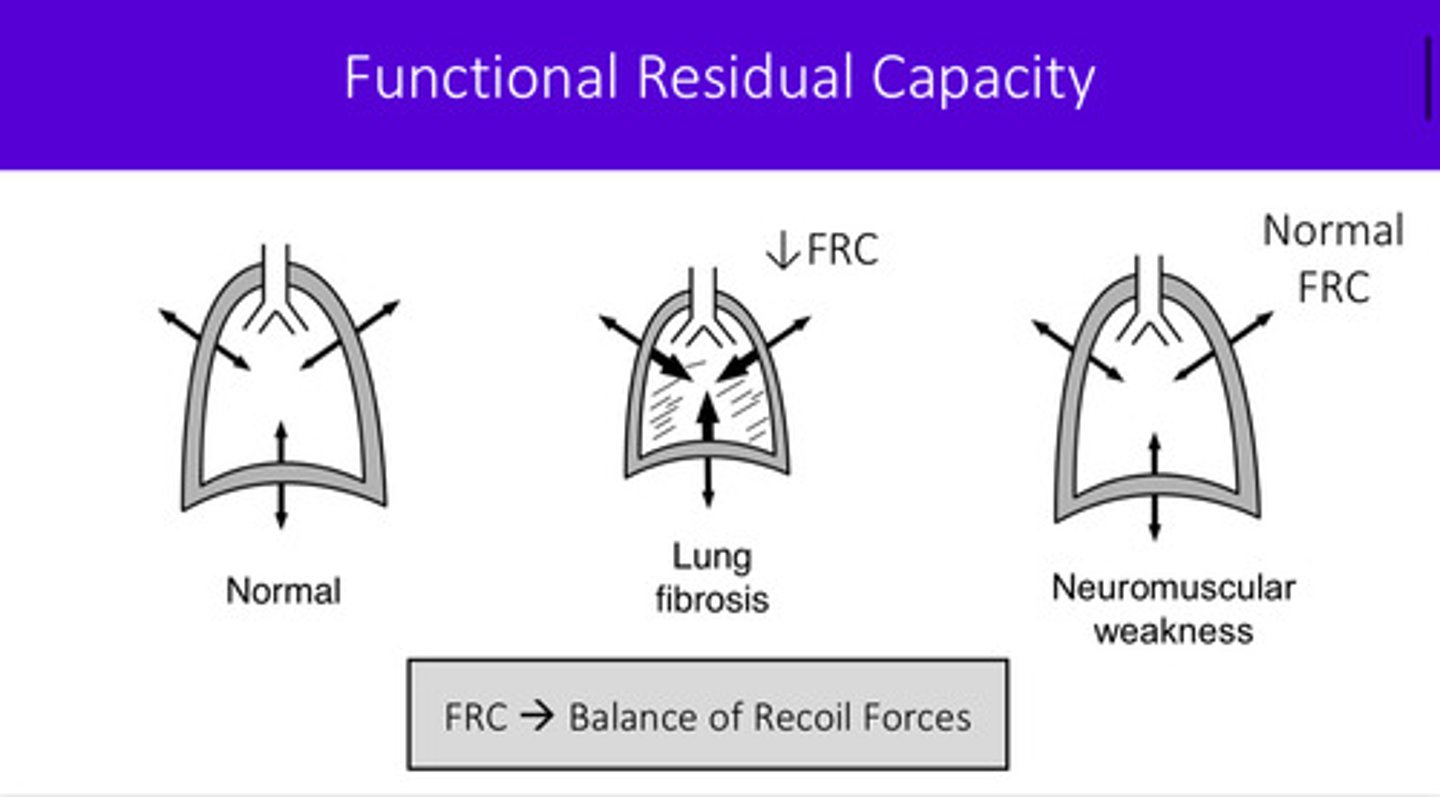
"parenchymal disease" means the tissue in the lungs is becoming more fibrotic and stiff, and not as soft and elastic as normal lung tissue. why does this cause a lower FRC?
the chest wall wishes to have a higher FRC as it wishes to occupy a larger volume while the lungs want to have a lower FRC as it wants to occupy a smaller volume —> these 2 are balanced through the pleura that connects the two. so when the lungs fibrose and become stiff, it stays in this smaller volume capacity and is unable to expand alongside the chest wall —> FRC and compliance is lower!!
why does neuromuscular weakness lead to high RV (some diseases cause the diaphragm not to work well)
1) RV: volume left over in the lungs after full exhalation
2) increased RV means that the patient cannot achieve their maximal exhalation —> there is most likely weakness in the muscles of exhalation: internal intercostals, obliques, transverse thoracis, and rectus abdominus
an issue of the diaphragm would or would not change the RV?
it would not bc it is a muscle of inhalation; RV is affected by exhalation
why does FRC in neuromuscular weakness stay fairly normal?
you do not use muscles to achieve FRC as it is the resting volume of lungs when no pressure is exerted
can you understand why the flow volume loop looks the way it does with restrictive disease?
FVC: forced vital capacity which is the total amount of air a person can exhale with maximal effort after taking a deep breath in
if a patient is restricted, their FVC becomes restricted as they are unable to exhale their full amount —> as a result, the flow volume loop narrows
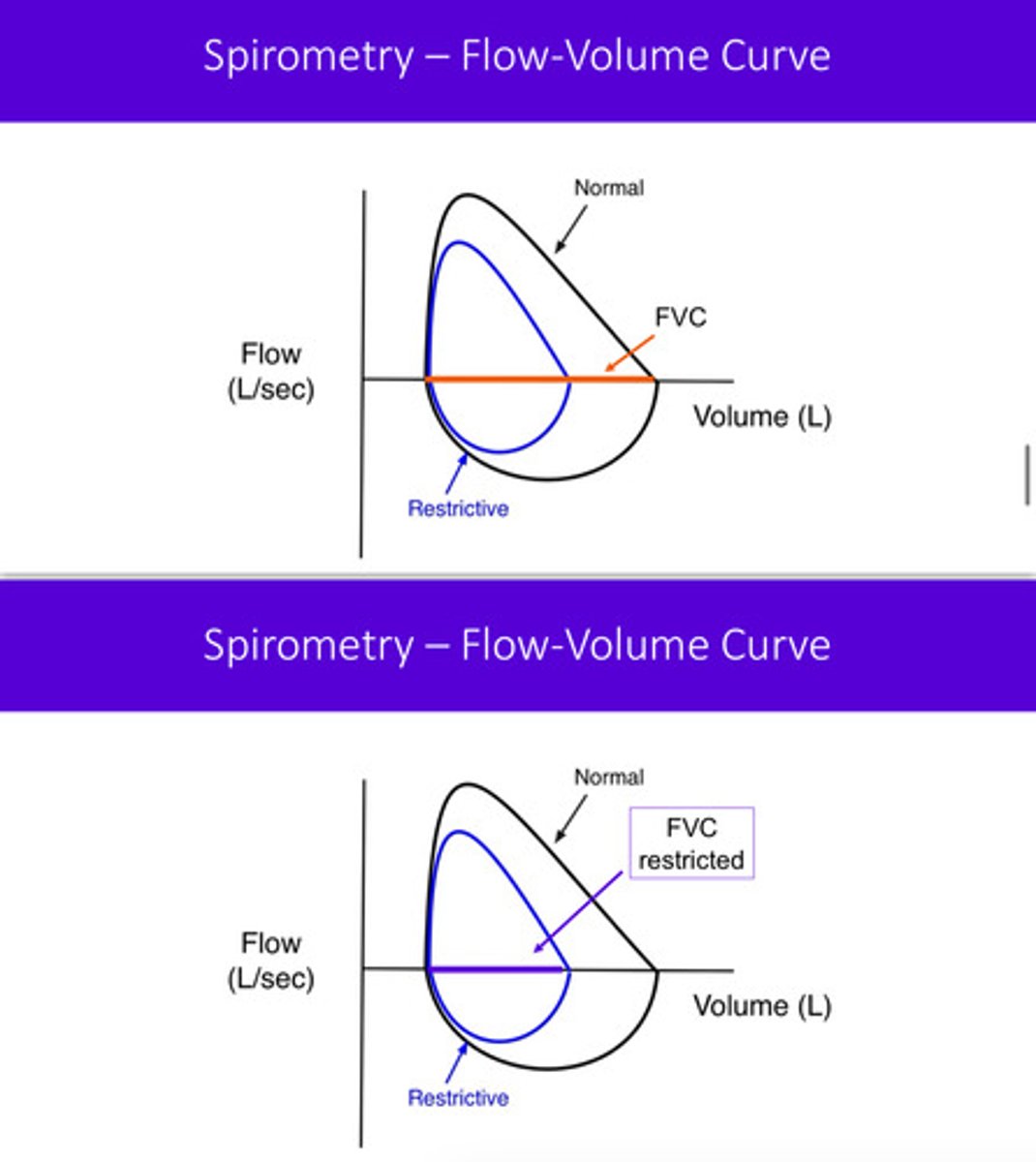
FVC is reduced in restrictive lung disease!
what does DLCO stand for? does it tell you how well the lung tissue can diffuse? what information does it really tell you?
DLCO: diffusing capacity for carbon monoxide
it does not necessarily tell you how well the lung tissue can diffuse, but how much surface area is available for gas exchange
how does the DLCO change in the 3 buckets of restrictive lung disease?
1) lung parenchyma —> damaged alveoli —> decreased DLCO
2) neuromuscular weakness —> fairly normal DLCO
3) chest wall/pleura issue —> fairly normal DLCO
last 2 buckets do not affect lung alveoli!!
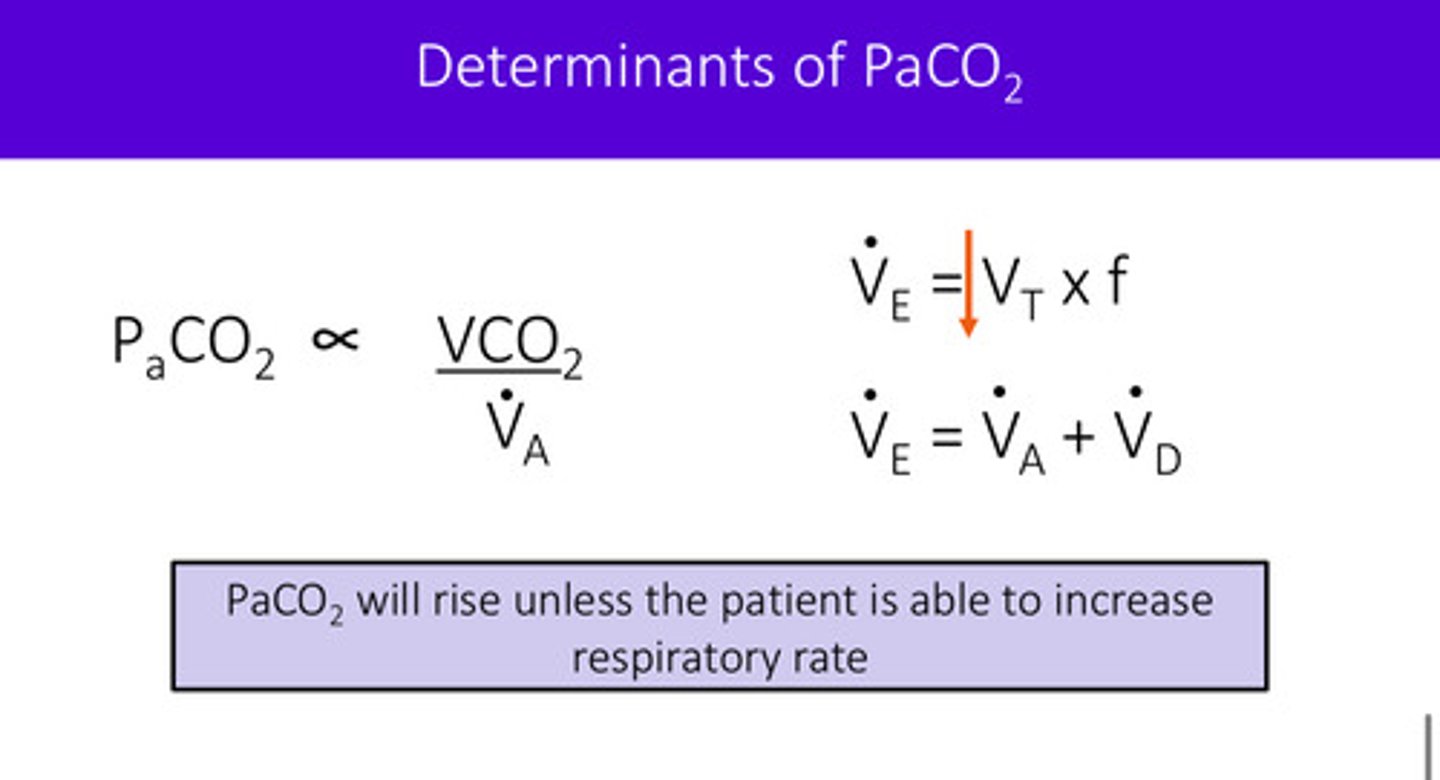
what is minute ventilation; how does it relate to tidal volume and respiratory rate?
minute ventilation is the total volume of air moved in and out of the lungs in one minute; this is found by multiplying the tidal volume (amount of air inhaled/exhaled per breath) and the respiratory rate (breaths per minute); VE = f x VT
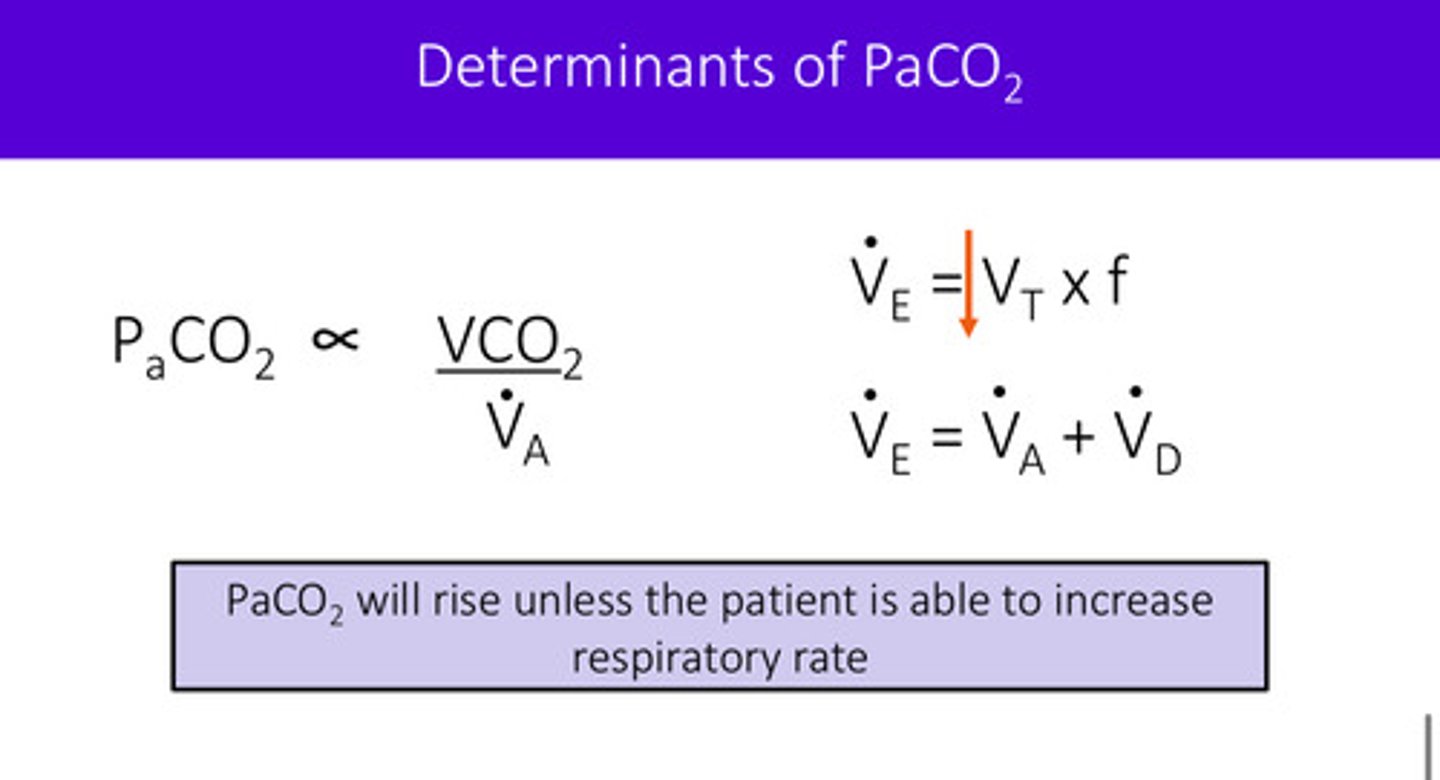
the portion of the minute ventilation that can exchange gas is the alveolar ventilation. if the ventilation is low, what will go up in the blood because it cannot be exchange out at the alveoli?
if ventilation is low (like in the case of neuromuscular weakness due to shallow breathing and inability to increase frequency), PaCO2 will increase because it cannot exchange out at the alveoli
recall that minute ventilation has 2 compartments: dead space ventilation + alveolar ventilation (VE = VD + VA)
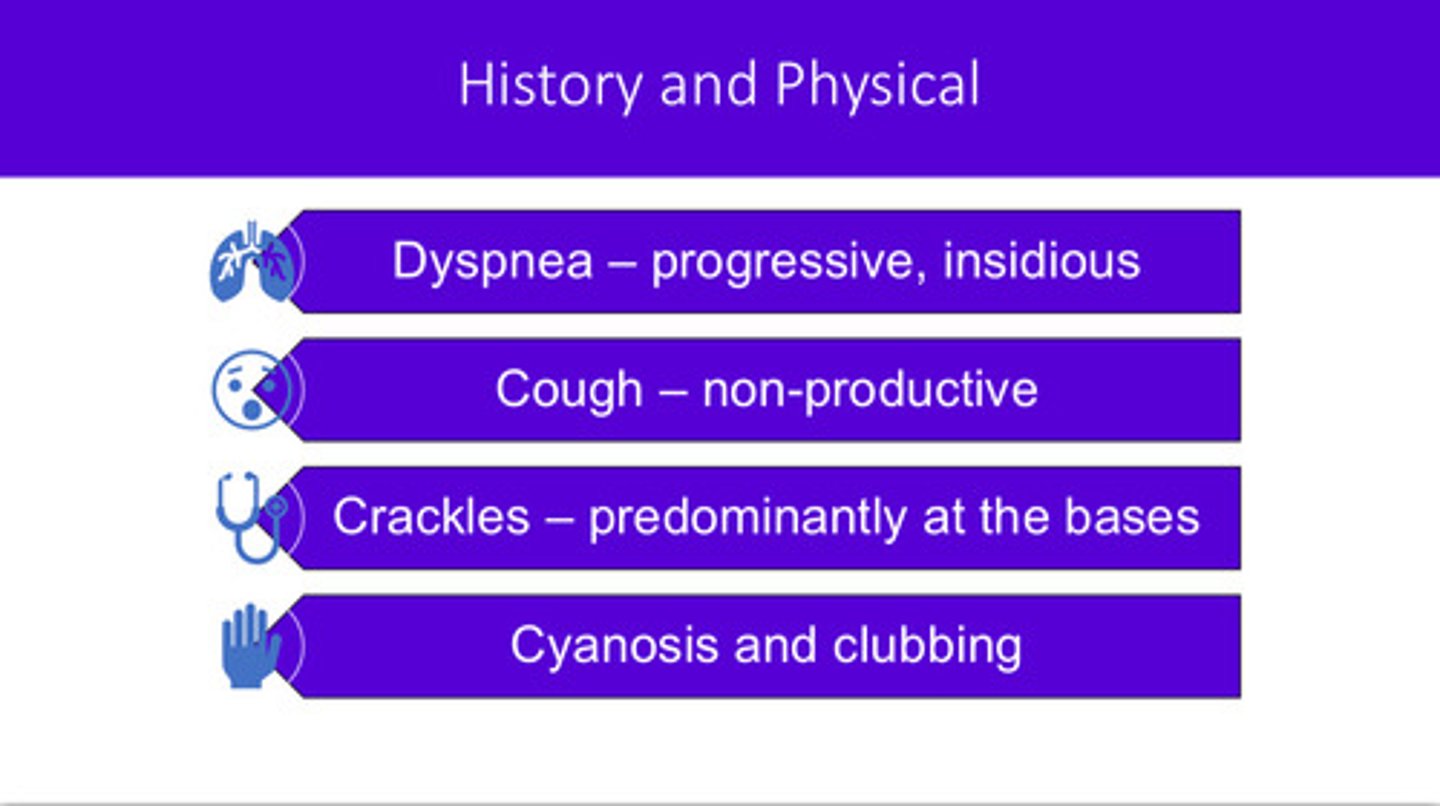
diffuse parenchymal lung disease (DPLD) most commonly presents with what symptoms? (4)
2 cardinal symptoms:
1) dyspnea: progressive, insidious (starts at exertion and progresses to occur also at rest)
2) cough: non-productive (dry! no phlegm production)
2 other symptoms found through hx and physical:
3) crackles: predominantly at the bases (unlike asthma or COPD where you would hear wheezes)
4) cyanosis and clubbing
what are the PFT changes of diffuse parenchymal lung disease (DPLD)
low TLC, low FRC, low RV, low DLCO
DPLD is complicated to diagnose (it can look like lots of other things, including heart problems). and ultimately, once it is diagnosed, it can have many different causes. the therapy depends on the cause. the 150+ causes are sometimes categories as what?
1) chronic systemic diseases
2) inorganic environmental exposures
3) organic environmental exposures
4) idiopathic pulmonary fibrosis (IPF) in which the cause is unknown
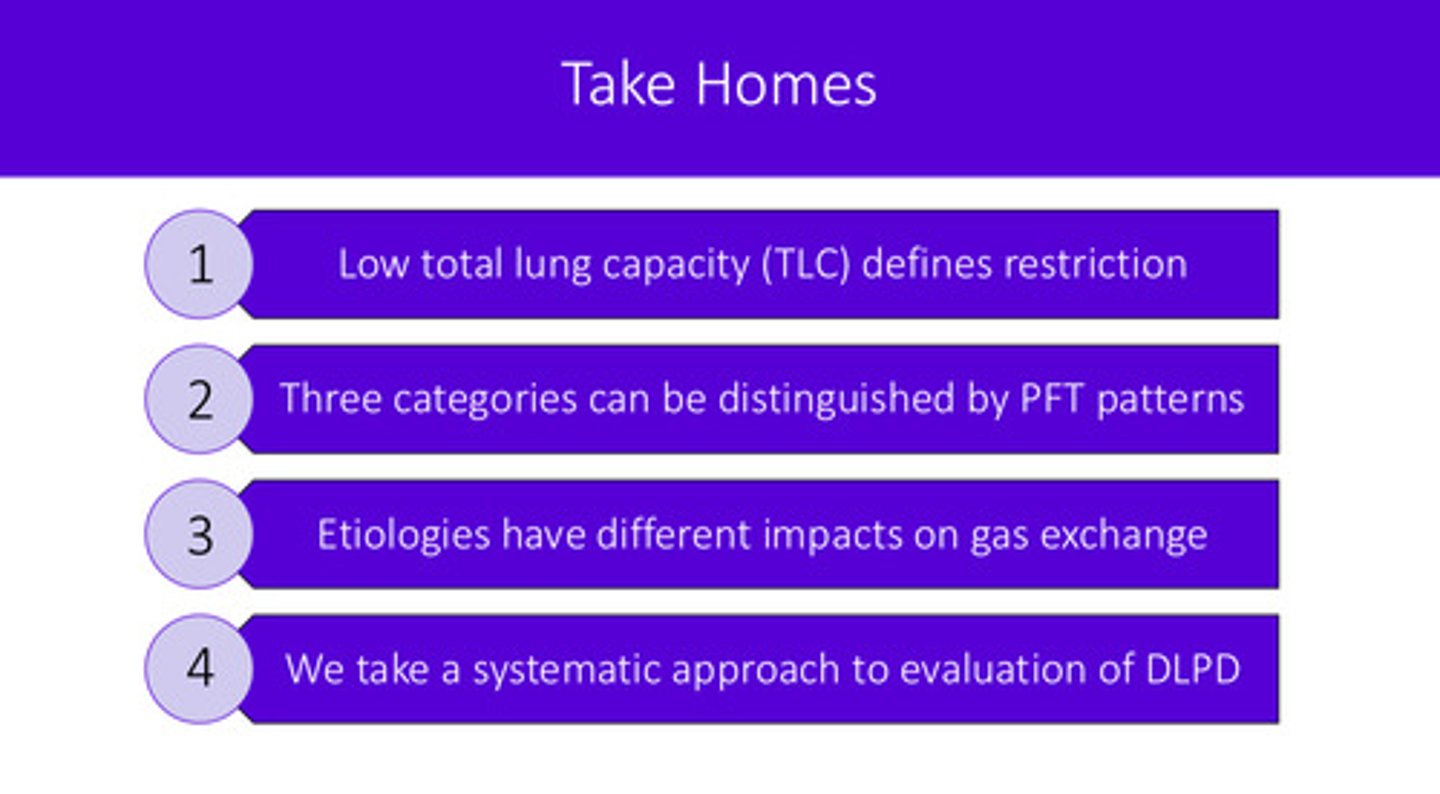
take home points