Clinical skills practical 3
1/17
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
18 Terms
Order of what to do? (11 steps)
Wash hands, clean everything, Introduce yourself.
Instruct what you will be doing, the intended outcome, and gain consent.
Ask about contraindication (Large open wounds or burns, gross edema, cancer history, fever, etc.)
Position and drape patient properly
Ask about allergies to lotion and emollient (If emollient will be used).
Identify target muscle origin and insertion.
Assess skin via horizontal drag, lift roll fold, and compression. Make sure to verbalize why.
Warm up tissue via stroke and/or effleurage (Need lotion), or active warm up. Make sure to verbalize why.
Begin main treatment. Can be either petrissage, percussion/vibration (Not on practical potentially), deep friction, myofascial release, trigger point, IASTM, Pin and stretch, or functional cupping. Make sure to explain why you’re do the treatment to the patient. Make sure to verbalize why.
Now asses patient to see if they gain the desired outcome (ROM, pain, tightness, etc.)
Give the patient a home program (Roller, lacrosse ball, general stretching) make sure to verbalize why.
For acuity, what are the three stages, their time frame, and what that means for treatment.
Acuity
Inflammation (Acute): 4 - 6 days, Lighter level techniques with light pressure around 1-2/10.
Proliferation (Subacute): 4 - 24 days. Medium level techniques with moderate pressure around 3-4/10.
Remodeling (Chronic): 21 days - 2 years. Any technique, heavier pressure around 4-5/10.
What are the contraindications one must ask before preforming anything?
Large open wounds or burns
Gross edema
Cancer in the skin or any tissues in the area to be treated (Cancer history)
Lacerations, or infections in the areas to be treated
Fever
Acute or chronic skin conditions- psoriasis, eczema,, dermatitis
Marked varicosities in the area to be treated
Within 3-6 months after radiation therapy in area to be treated
Areas of hyperesthesia
Before applying lotion or emollient what should you do?
Position patient properly
Drape patient properly (Tuck towel unto clothes)
Ask about allergies (Show back of bottle)
How do you assess skin, superficial fascia, and muscle before preforming any warm up and why?
Must assess all three: skin, superficial fascia, and muscle
For skin: Horizontal drag for thickness, elastic rebound, and moisture.
For superficial fascia: Lift, roll, fold for stretch and recoil.
Muscle: Compression to assess muscle tension.
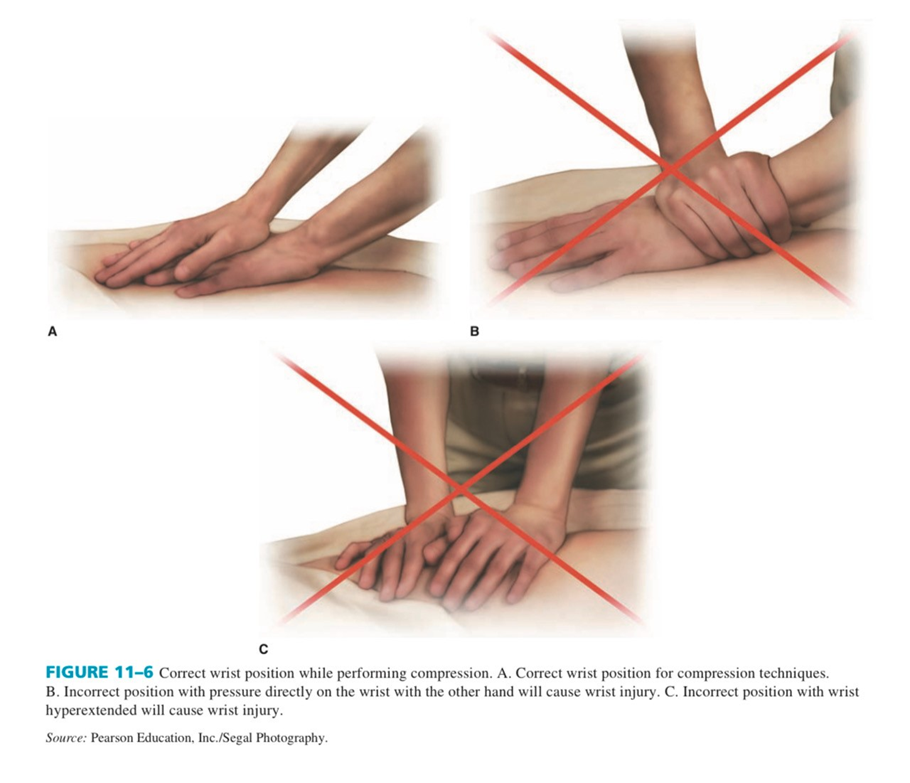
When preforming any sort of STM, what must you be aware of?
Proper body mechanics
Do not want to hyper extend fingers so reinforce finger (Side by side, stacking finger)
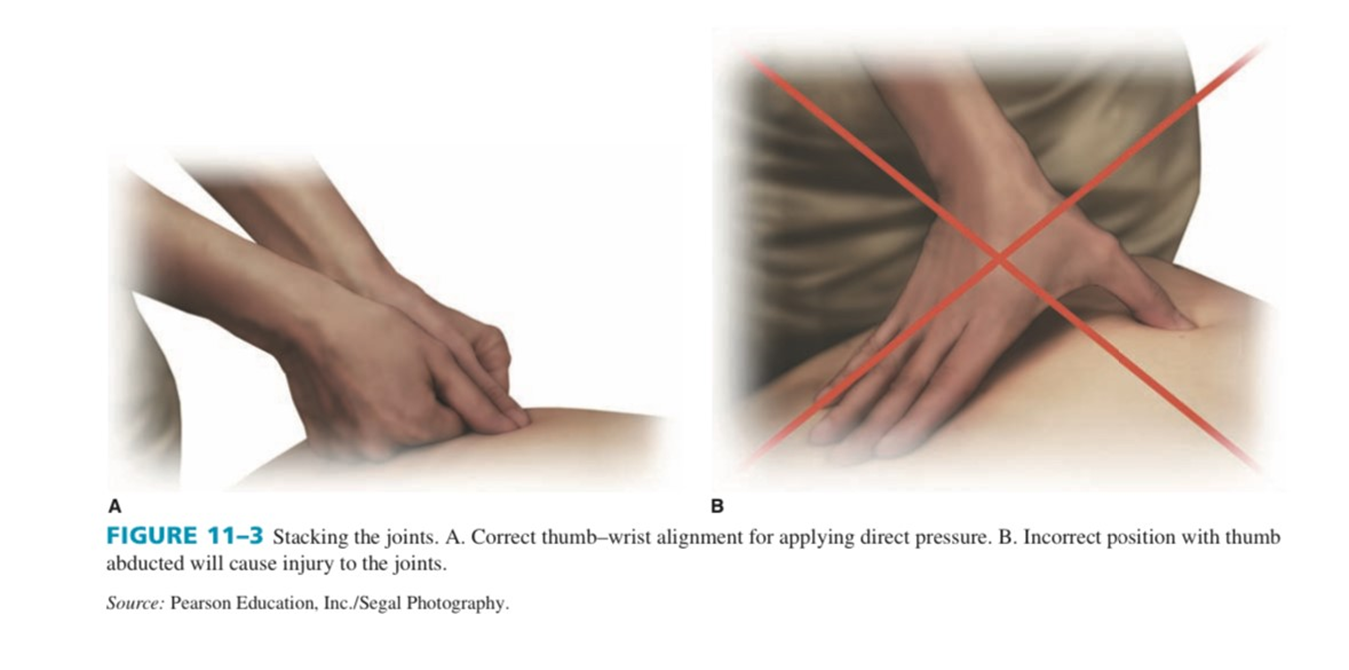
Do not want to hyper extend wrist so reinforce (Stack them and angle)
Why do we do warm up, what can you do for a warm up? How long
For warm up we can preform stroking, effleurage, or have the patient do an active exercise. Done to relax, decrease pain, increase circulation, and decrease muscle tone. Maintain constant contact for stroking and effleurage. Done for about
Stroking: Massage in no particular direction. Typically done with light pressure as an introduction into effleurage.
Effleurage: Massage in a particular direction (in line with muscle fibers and distal to proximal). Can be done after stroke or stroke can be skipped if the patients pain is not too bad. Typically done with more pressure (1-5/10 pressure). Can potentially be done as the actual treatment for 2 - 5 minutes (?)
Active warm up: Any sort of exercise that works the target muscle. For instance having the patient do a set of leg extensions for quads.
(NOTE: Pressure applied depends on the pain of the patient or their stage of healing. Typically pain and stage coincide with each other. For instance effleurage can be light or moderate depending on pain and stage of healing). Used reinforced hand for deeper pressure)
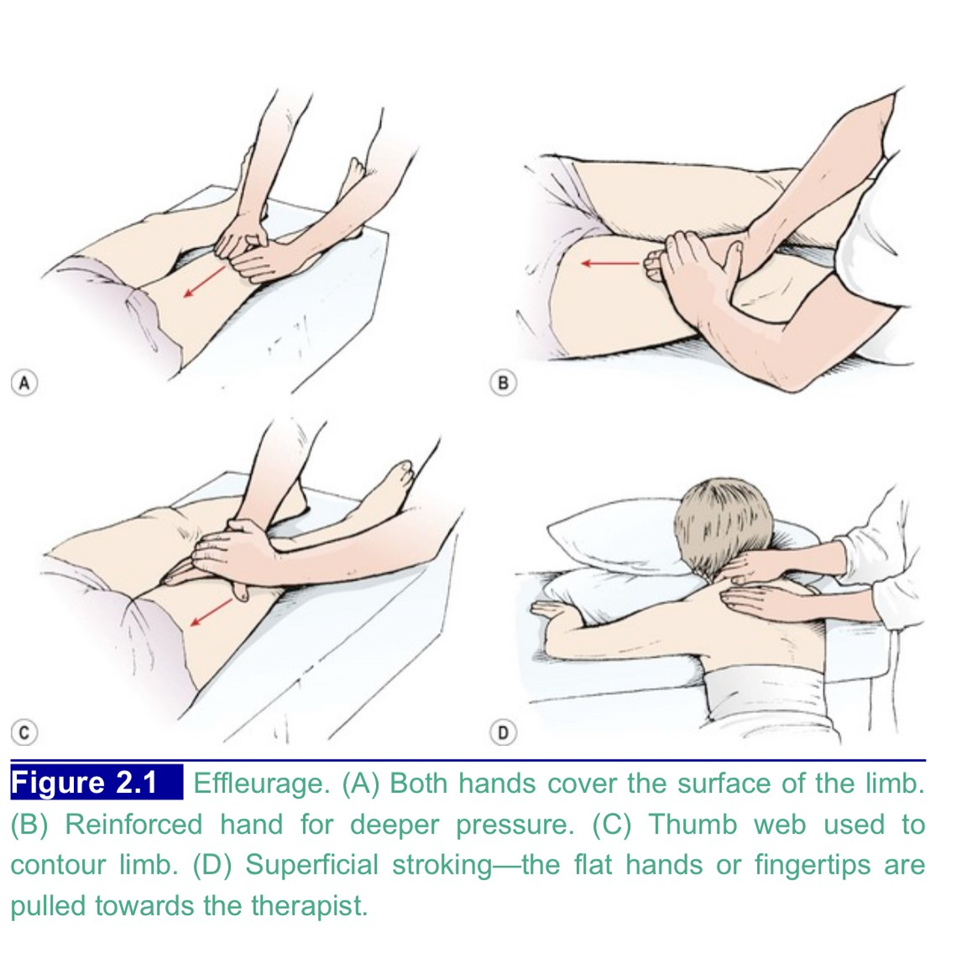
Techniques for efflurage?

Shingle effleurage: Sliding one hand after another repetitively.
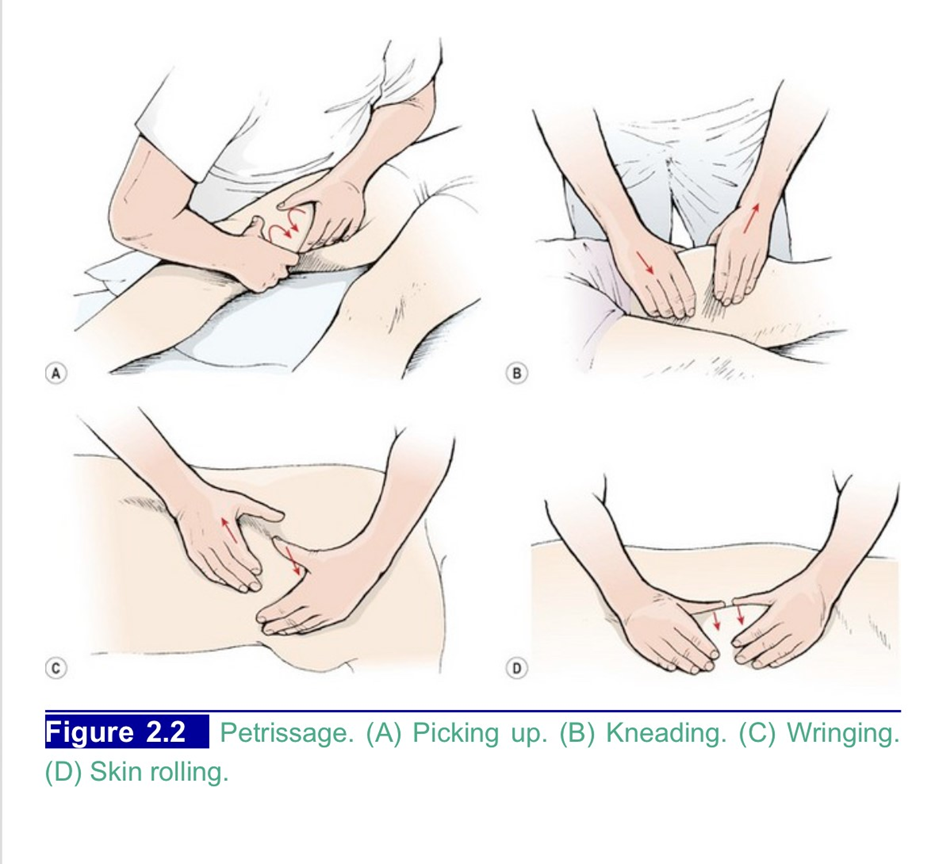
What is petrissage and when to use it? What are the types?
Petrissage is a repetitive lift, wringing or squeeze of soft tissue in a kneading motion or a press or roll of the tissues under or between the hands. Done for 5 - 10 minutes.
Reduces pain
Reduce muscle tension
Improve connective tissue extensibility
Reduce anxiety
Proprioceptive input
Muscle relaxation
There are 4 types:
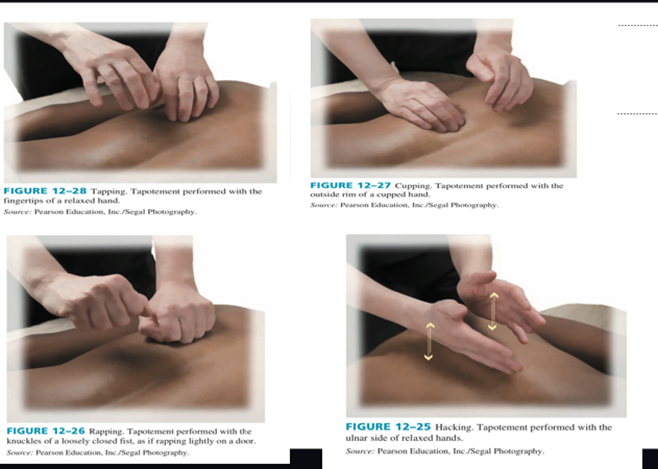
What is percussion and what is vibration? When to use each and techniques? (POTENTIALLY NOT ON PRATICAL)
Percussion is repetitive percussive movement. Done for 1 - 3 minutes.
Airway clearance
Stimulating effect at end of session
Prior to exercise to facilitate performance.
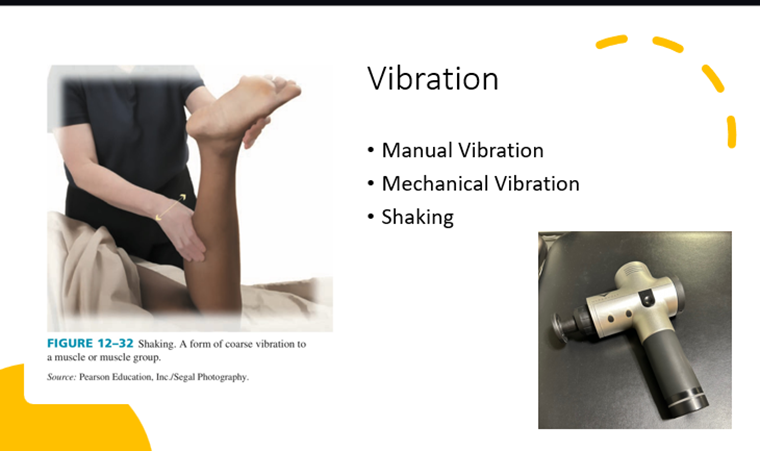
Vibration is fine shaking movement is delivered to the tissues by the hand of fingertips or by a device like a Thera gun. Done for 30 - 2 minutes.
Loosen secretions in lungs
Stimulating techniques over muscle tissue
Decrease pain
Muscle relaxation
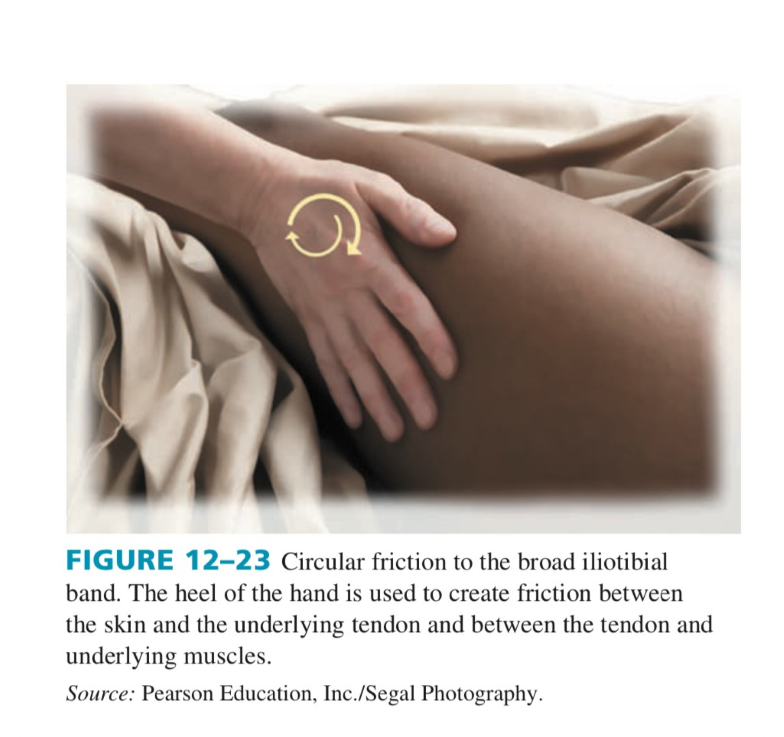
What is deep transverse friction? When do you use and not use it and techniques?
Deep transverse friction is repetitive Specific non-gliding technique that produces movement between fibers of dense connective tissue. Must be done perpendicular to muscle fibers. Done for 3 - 7 minutes moving at 1 - 2 cycles a second. (Tools can be use if hands are tired). Some lotion can be used but not all the time.
Promote healthy scar formation or break up scar adhesions
Tendons/ligaments, muscle, fascia
Relieves pain
Tissue mobilization
DO NOT USE IN ACUTE
Normal techniques (For scars there are different ones)
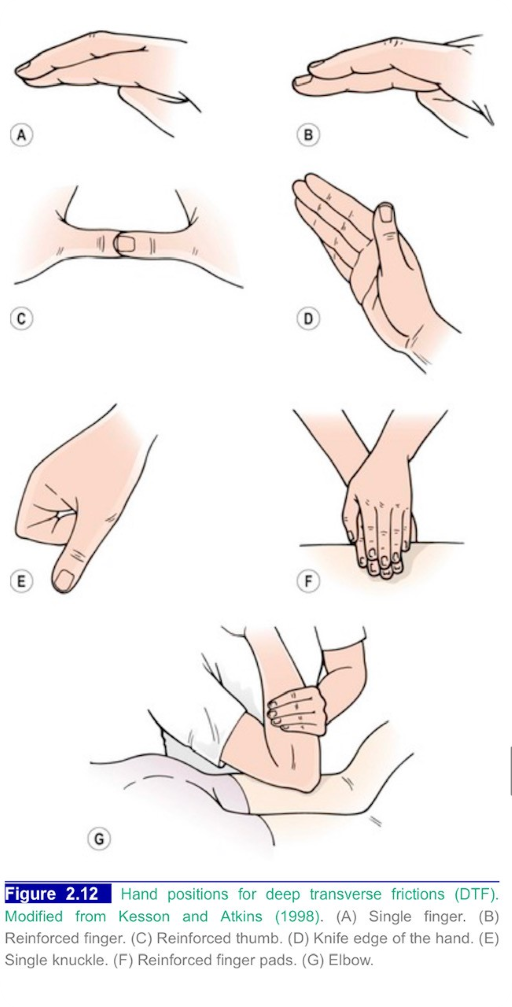
Circular friction can be done for larger areas, typically for lumbar paraspinals and ITB. No lotion for this unless patient is hairy.
Deep transverse friction for scars have different techniques. What are they, how long to preform them, and home program?
TO BE USED ON HEALED SCARS and make sure you asses the areas for restriction or pain before preforming. No to little lotion. 3 - 7 minutes. Patient can do it at home 2 times a day.
Rolling
S technique
Circular
Transverse
Refer to slide 55 for video demonstration
What is myofascial release? What is it used for and techniques?
Myofascial release is a STM that focuses on Fascia. Find area of increased tension (TAUT BAND that limits movement and triggers pain) and apply force over the area in slow deep swings. Done for 8 minutes and effleurage is done after to calm the system. Only use lotion as needed.
trigger points
muscle tightness
soft tissue dysfunction that may cause pain or limit motion.

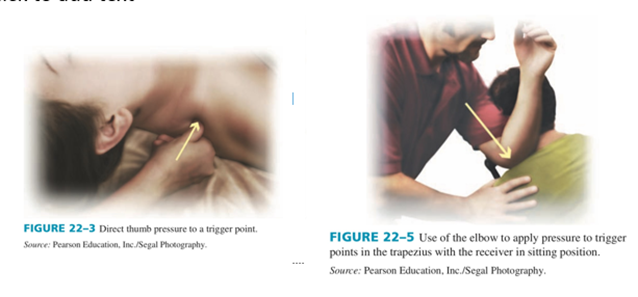
What are trigger points and what techniques can be done to alleviate it?
Trigger points are an irritable spot in skeletal muscle with a hypersensitive, palpable nodule in a taut band. Can cause pain, tenderness, motor dysfunction. Palpate via the presence of a taut band with patient feedback. Pressure is applied slowly and perpendicularly and increase gradually to desired depth. Remember to inform patient to breath. DONE FOR 30 sec - 1:30 minutes! Afterward passive stretch for 30 and than AROM.
What is IASTM? When to use it and techniques?
Myofascial release using instruments based on principles friction massage. Tools include shaped stainless steel that has beveled edges and contours that can conform the body. THIS SAVES YOUR HANDS. Done for 8 minutes.
Trigger points
muscle tightness
soft tissue dysfunction that may cause pain or limit motion.
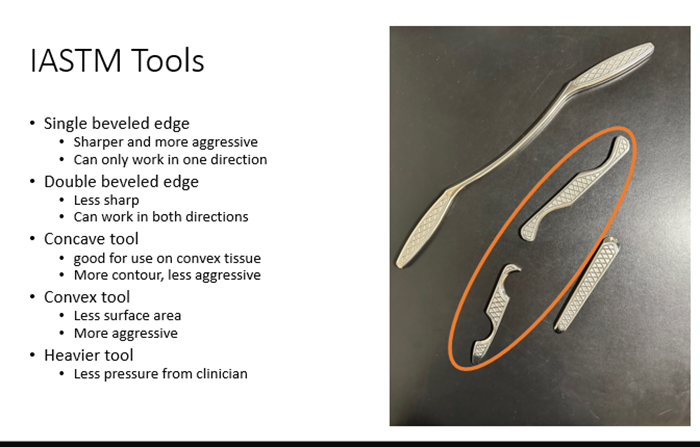
Make sure to move in the direction of the beveled edge (Think of shovel or ‘scooping’ the skin)
Hold at 45 degree angle
Use emollient
Stokes can be linear, curvilinear, or pressure
Maintain contact with the skin to avoid reflexive muscle tone (2 steps forward one step back
Slides 70 - 73 have pictures and video demos
What is pin and stretch? When is it used and techniques?
technique used to focus the force of a stretch or STM to a specific region of the muscle. The therapist uses their hand or other body part to manually “pin” the area of the muscle and then moves the muscle away from the pinned point. (Shorten the muscle, pin at the targeted area and then lengthen the muscle.) Pressure depends on where, how deep the muscle, and muscle tone. Can be active or passive.
tightness
Gain ROM
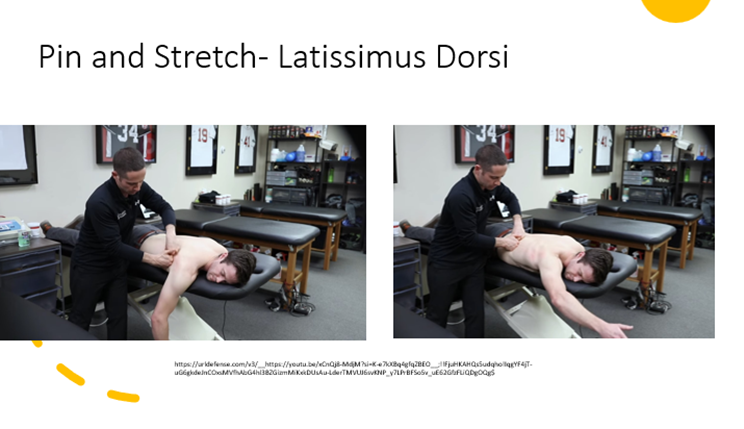
more picture and video demos from slide 79 - 83.
What is traditional cupping? When is it used and techniques?
Traditional cupping therapy is an ancient medicine technique that has proven to be effective at
pain
CV disease
inflammatory and metabolic issues
MSK conditions,
Can also be used to preform the same techniques for scar tissue. (S shape, Transverse, circular, vertical). Squeezing harder determines pressure.

There are 4 different techniques:
Static cup on static body (90 - 120 sec)

Static cup on dynamic body

Dynamic cup on static body

Dynamic cup on dynamic body
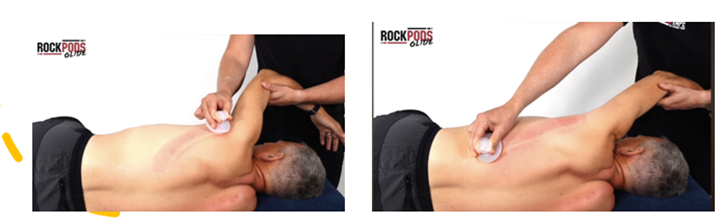
(Static cup with dynamic body if for more stretching)
Self myofascial release is good for? What do they need?
HEP that allows patients to preform myofascial release independently
Roller: larger muscles
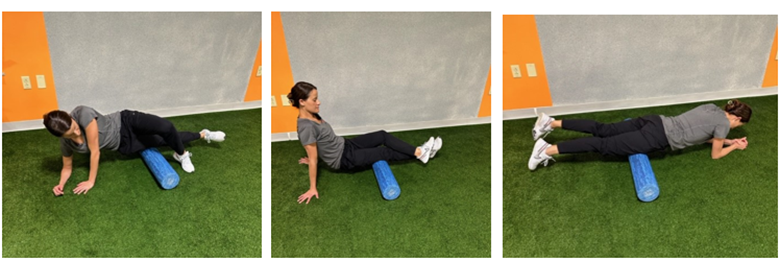
Lacrosse ball: Deeper targeted tissue

Roller stick (Not on PowerPoint)