Colorectal Cancer
1/38
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
39 Terms
Name the signs and symptoms of rectal cancer.
Rectal bleeding (blood in stool)
Change in bowel habits lasting 3 weeks or more
Tenesmus - needing to go but can’t
Mucous
Weight loss
Palpable ass in abdomen or rectum
Anaemia
Name signs and symptoms that may be seen in late stage disease.
Ascites - accumulation of fluid in the abdomen causing swelling.
Hepatomegaly - enlargement of liver.
Fistula - connection between organs or vessels that isn’t normal.
What do most people with bowel cancer present with ?
Persistent change in bowel habit usually accompanied by rectal bleeding.
Persistent change in bowel habit without blood in stools but with abdominal ain.
Blood in the stools without other haemorrhoid symptoms such as soreness, discomfort or pain.
Abdominal pain, discomfort or bloating always provoked by eating, resulting in weight loss.
Why is screening important for colorectal cancers ?
Some people present with nothing especially at an early stage.
Better picked up by screening.
The NHS provides a symptom checker.
What investigations should be carried out if a Pt presents symptoms suggesting possible rectal cancer?
CT - helpful n staging
MRI - general information about organs around.
Colonoscopy - great visualisation. Can take biopsies and remove polyps.
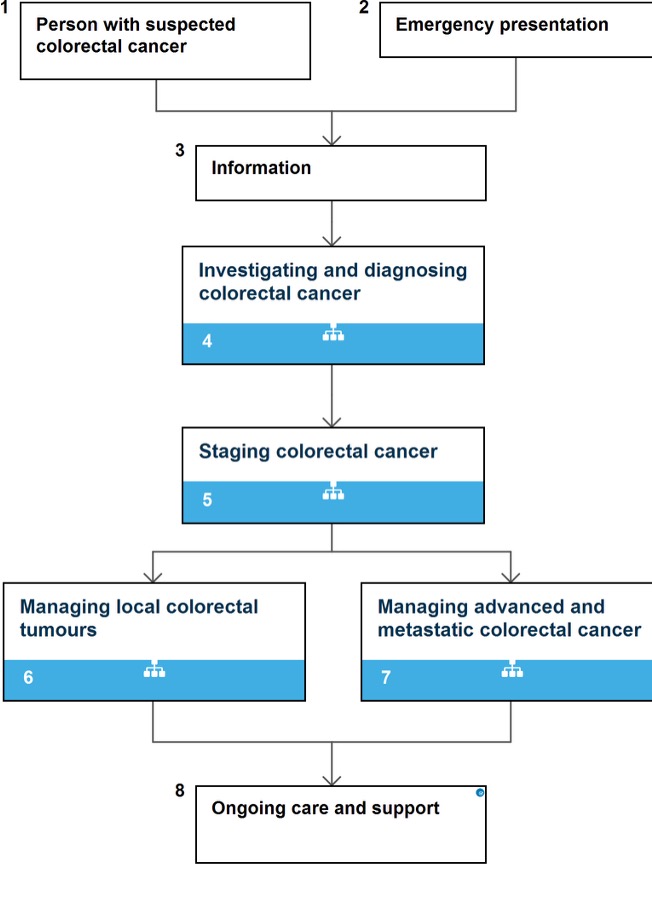
What is the general pathway followed for a person who present with symptoms of colorectal cancer ?
At primary care what examinations are usually done if rectal cancer suspected ?
Digital examination of rectum
Clinical examination : palpation of abdomen.
When should people be referrred?
An appointment with 2 weeks if:
40+ & unexplained wight loss+abdominal pain
50+ & rectal bleeding
60+ & anemia or change in bowels or blood on faeces
How is a diagnosis confirmed ?
Rectal ultrasound
Pt without major comorbidity : colonoscopy.
With comorbidity : flexible sigmoidoscopy then barium enema
If lesion suspicious of cancer detected perform a biopsy to obtain histological proof of diagnosis.
What can be offered as an alternative to colonoscopy or flexible sigmoidoscopy?
CT colonoscopy - uses CT scanner to produce detailed pictures of the colon and rectum.
A biopsy may still be required
Less invasive
Barium enema
A test used to help see the outline of the colon.
Not done much since colonoscopy became available.
Bowel preparation - laxatives
How to stage disease in patients who have been diagnosed with colorectal cancer?
Offer contrast enhanced CT of the chest, abdomen and pelvis
No further imaging needed for patients with colon cancer.
Offer MRI to assess risk of local recurrence to al patients with rectal cancer.
Offer endorectal ultrasound to patients with rectal cancer if MRI shows disease amenable to local excision.
How is Duke’s system using for staging ?
A - confined to bowl wall
B - breached Owen wall
C- 1-4 local nodes
C2 - more than 4 regional nodes.
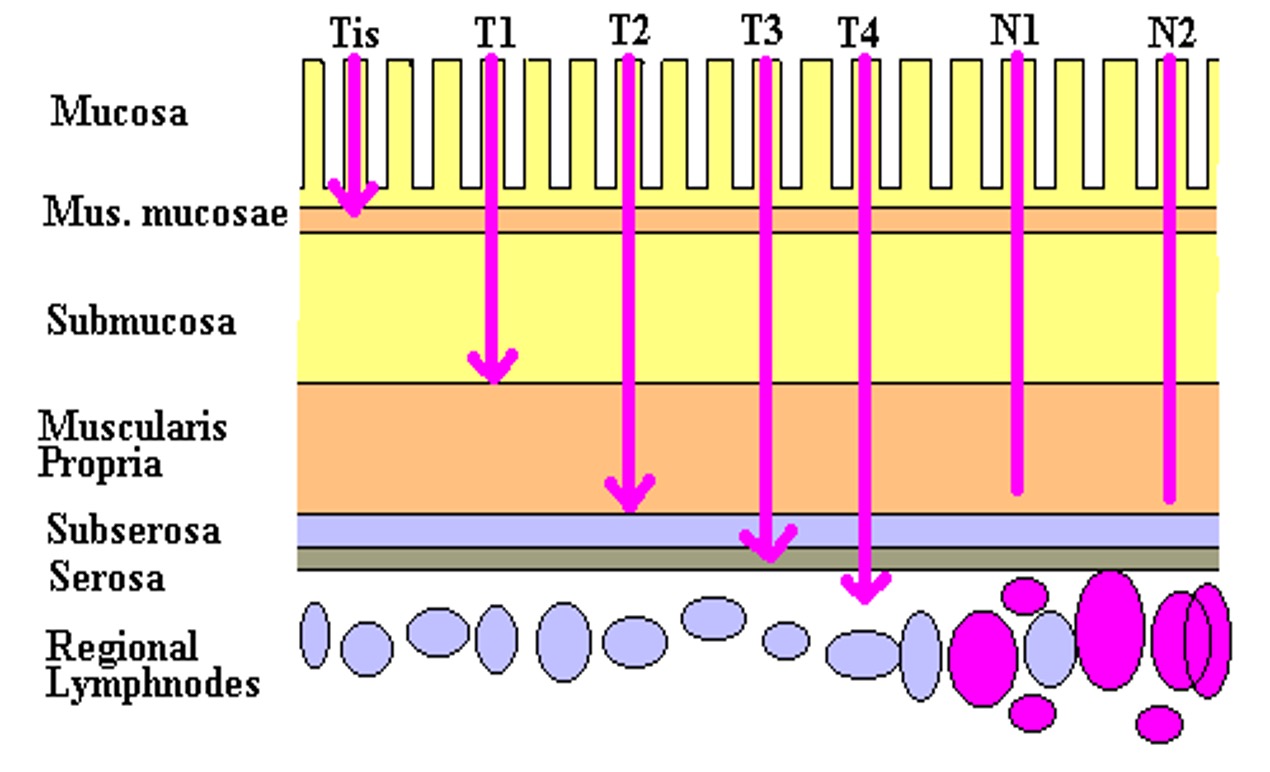
TNM system
Tis - carcinoma in situ
T1 - submucosa
T2 - muscular is propria
T3 - sub serosa
T4 - other organs visceral peritoneum
N0 - no nodes
N1 - 3 or less
N2 - more than 3
N3 - nodes on vascular trunk
Treatment for people with early rectal cancer (cT1-T2, cN0, M0)
Managed surgically and never really seen in RTD.
Surgeries include:
Total mesorectal excision (TME) - possible stoma needed.
endoscopic submucosal dissection (ESD) - no stoma needed.
Laparoscopic surgery for rectal cancer
What does total mesorectal excision include (TME)?
removal of the rectum with surrounding fat, nodes and vessels.
Aim for circumferential resection margin (an extra margin around the visible tumour)
How does removing the fatty tissue from around the rectum during TME reduce the risk of recurrence?
the fatty tissue contains lymph nodes and blood vessels.
This means all the lymph nodes near the tumour are removed.
What are 3 common surgeries used to treat rectal cancer?
Trans anal excision (TAE) - surgery performed through the anus, sphincters reserved and a small amount of tissue.
Transanal minimally invasive surgery (TAMIS) - laparoscopic procedure (sphincter sparing)
Transanal endoscopic microsurgery (TEMS) - uses an endoscope (sphincter sparing)
Which management options should be considered?
surgery - permanent/semi-permanent stoma
RT
Chemotherapy - single/multiple agents
Adjacently/ neoadjuvant
Concurrently
When and when not is preoperative treatment offered for pt with rectal cancer ?
Do not offer preoperative RT to people with early rectal cancer (cT1-T2, cN0, M0)
Offer preoperative RT or chemo to people with cT1-T2, cN1-N2, M0) or cT3-T4, any cN, M0)
shrinks the tumour prior to surgery
given if there is threat to surgical margin, lymph node, extramural invasion (blood vessel)
When should surgery be offered ?
cT1-T2, cN1-N2, M0
cT3-T4, any cN, M0
What can be offered to patients who need surgery but cannot tolerate it?
Low energy contact X-ray Brachytherapy (Papillion technique)
involves inserting X-ray tube through the anus and placing it in close contact with the tumour, to kill cancer cells and reduce size of tumour.
When is pre -op chemo/RT offered to patients with high-risk locally advanced disease?
Offer pre-op Chemo XRT with an interval to allow response and shrinkage.
Do not offer pre-op XRT alone to solely facilitate surgery
Do not offer chemo alone unless part of a clinical trial.
What is offered to stage II/ III high-risk pt post surgery ?
Adjuvant chemotherapy reduces the risk of local and systemic recurrence.
For people with stage III colon or rectal cancer pT1-4, pN1-2, M0 offer:
capecitabine + oxaliplatin (CAPOX) for 3 months or if not suitable
oxaliplatin + 5-fluorouracil and folinic acid (FOLFOX) for 3-6 months
Which radiotherapy options are available pre-op for low/moderate risk?
Pre-op long course XRT - then surgery
Pre-op long course chemoXRT - then surgery
Which post-op options are there for high risk ?
surgery then - long course chemoXRT
Surgery - long course XRT
When to use short course (pre-op) ?
upper rectal cancers
T3B cancers
Potential surgical margin threatened
What is the usual dose of pre-op XRT ?
25Gy, #5, 5 days
objective to kill micrometasteses
When to use long course (post-op) ?
surgical margin is threatened, borderline moderate/high risk (bulkier so margin compromised)
Low rectal cancers
cT3/T4
cN1/N2
Tumour within 1mm of CRM
(for downstaging of advanced disease, usually combined with chemo)
What is the usual XRT long course (post-op) dose ?
45Gy #25 5 weeks
usually with concurrent chemo Capecitabine 825mg/m2 for 35 days
What is the dose for curative XRT ?
50.4Gy #28 6 weeks with or without chemo
What is the palliative XRT dose ?
25Gy #5 5 days mon- fri
What chemo drugs are taken with curative XRT ?
Capecitabine- once daily for duration of XRT, only on XRT days.
Same with long course (post op)
Why is concurrent chemotherapy offered with XRT?
eeficiancy of XRT can be increased.
Chemo potentially functions to sensitise cancer cells to radiation effects.
Name side effects of Capecitabine
chest pain / angina-like symptoms (red flag- contact hospital)
nausea and being sick - usually mild
sore mouth and ulcers
taste changes
diarrhoea
abdominal pain and constipation
loss of appetite
tiredness
Name acute toxicities of short course
lethargy
skin redness
diarrhoea
back pain
Name acute toxicities for long courses
lethargy
redness
diarrhoea/constipation
urinary symptoms
call doctor of urinary retention, bowel obstruction, cardiac morbidity
How to treat unresectable (cannot be completely removed) cancer ?
Patients with stage 4 colorectal disease
Pre-op chemoradiotherapy - to allow tumour shrinkage
radiotherapy - pain relief for mets
chemo - palliating patients
surgery - defunctioning colostomy, stenting
When and how are patients followed up after completion of treatment ?
offer regular surveillance with minimum of 2 CTs (chest/abdo/pelvis) in the first 3 years.
Regular CEA (blood test) every 6 months for first 3 years