Hui DDX
1/25
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
26 Terms
Asthma
Types: Allergic (eczema, allergic rhinitis, or food/drug allergy; induced sputum eosinophils, steroid-responsive), Non-Allergic, Adult-onset, asthma with persistent airflow limitation, obesity
Exacerbations: infections—viral, bacterial, fungal; outdoors—respirable particulates, ozone, sulfur dioxide, cold air, humidity, smoking; indoors—smoke, dust mites, air conditioners, humidity, perfumes, scents, mold, animal dander; non-adherence (incorrect inhaler technique, major psychological or socioeconomic problems)
Risk Factors: >1 exacerbation in previous year, socioeconomic status, poor adherence, incorrect inhaler technique, low lung function, smoking, eosinophilia
Hx: history of asthma and any lifethreatening exacerbations, number of ER visits/ hospital admissions in the last 6 months (or ever), any ICU admissions, previous prednisone use, triggers for attacks, usual peak expiratory flow rate, change in peak flow rates, wheezing, cough, dyspnea, decreased function, exercise limitation, nocturnal symptoms, absenteeism from work/school, postnasal drip, recurrent sinusitis, GERD, past medical history, medication history, psychosocial issues, occupational and work environment, home environment (pets, heating source, filter changes, mold)
PHYSICAL—HR ↑, RR ↑, pulsus paradoxus, O2 requirement, moderate-severe dyspnea, barrel chest, cyanosis, stridor, chest hyperresonance, decreased breath sounds, wheezing, forced expiratory time
COPD
PRECIPITANTS - infections, lifestyle/environmental (10% [cigarette smoke, dust, pollutants, cold air]), non-adherence to medications, pulmonary embolism, pulmonary edema, pneumothorax, progression of COPD
Gold: 1 (>80%), 2 (>50%), 3 (>30%), 4 (<30%) MMRC 0, 1 (hill/hurrying), 2 (slower than age), 3 (100m/few mins), 4 (housebound)
![<p><strong>PRECIPITANTS</strong> - infections, lifestyle/environmental (10% [cigarette smoke, dust, pollutants, cold air]), non-adherence to medications, pulmonary embolism, pulmonary edema, pneumothorax, progression of COPD</p><p><strong>Gold</strong>: 1 (>80%), 2 (>50%), 3 (>30%), 4 (<30%) <strong>MMRC</strong> 0, 1 (hill/hurrying), 2 (slower than age), 3 (100m/few mins), 4 (housebound)</p>](https://knowt-user-attachments.s3.amazonaws.com/5fc5fd10-0952-4d12-84e9-088a5a8c46cc.png)
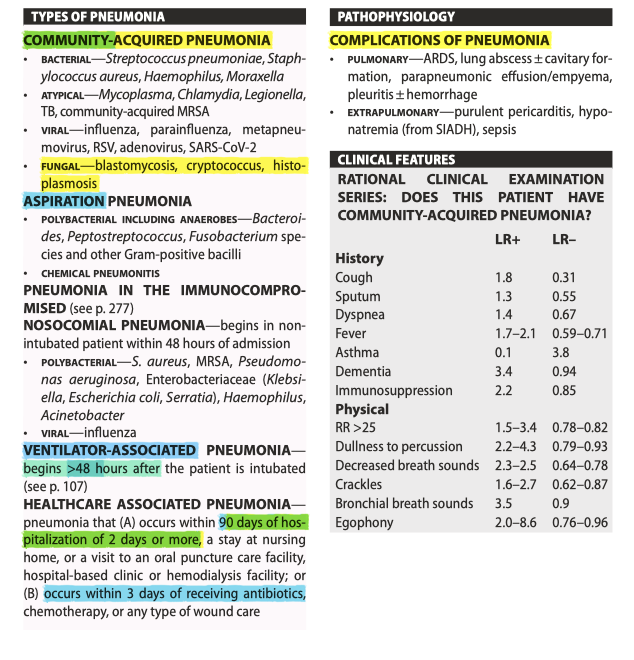
Pneumonia
Cx: Pulmonary—ARDS, lung abscess ± cavitary formation, parapneumonic effusion/empyema, pleuritis ± hemorrhage
Extrapulmonary—purulent pericarditis, hyponatremia (from SIADH), sepsis
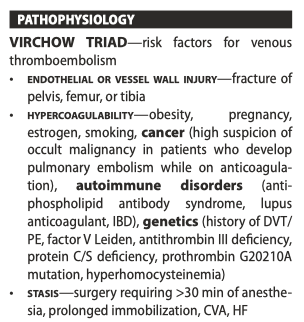
Pulmonary Embolism Risk Factors
HISTORY—dyspnea (sudden onset), pleuritic chest pain, cough, hemoptysis, pre/syncope, unilateral leg swelling/pain, past medical history (previous DVT/PE, active cancer, immobilization or surgery in last 4 weeks, miscarriages), medications (birth control pill, anticoagulation) PHYSICAL—vitals (tachycardia, tachypnea, hypotension, fever, hypoxemia), respiratory examination (pulmonary hypertension if chronic PE), cardiac examination (right heart strain), leg swelling
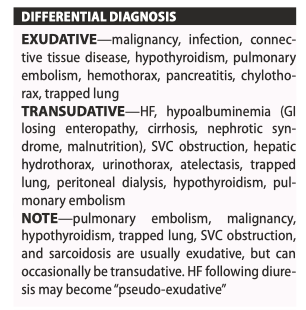
Pleural Effusion
HISTORY—dyspnea, cough, hemoptysis, chest pain, weight loss, fever, trauma, occupational exposures, past medical history (pneumonia, liver disease, kidney disease, thyroid disease, cancer, HF, thromboembolic disease, connective tissue disease, smoking), medications
Physical - vitals, cyanosis, clubbing, tracheal deviation away from side of effusion (if no collapse or trapped lung), peripheral lymphadenopathy, Horner syndrome, respiratory examination (decreased breath sounds and tactile fremitus, stony dullness to percussion), cardiac examination, leg swelling (HF or DVT); chest US is the most sensitive and specific test and should be done at point-of-care
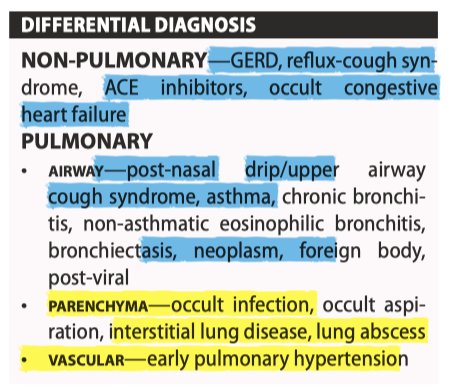
Chronic Cough
>3 weeks, Cx: exhaustion, insomnia, anxiety, headaches, dizziness, hoarseness, musculoskeletal pain, urinary incontinence, abdominal hernias
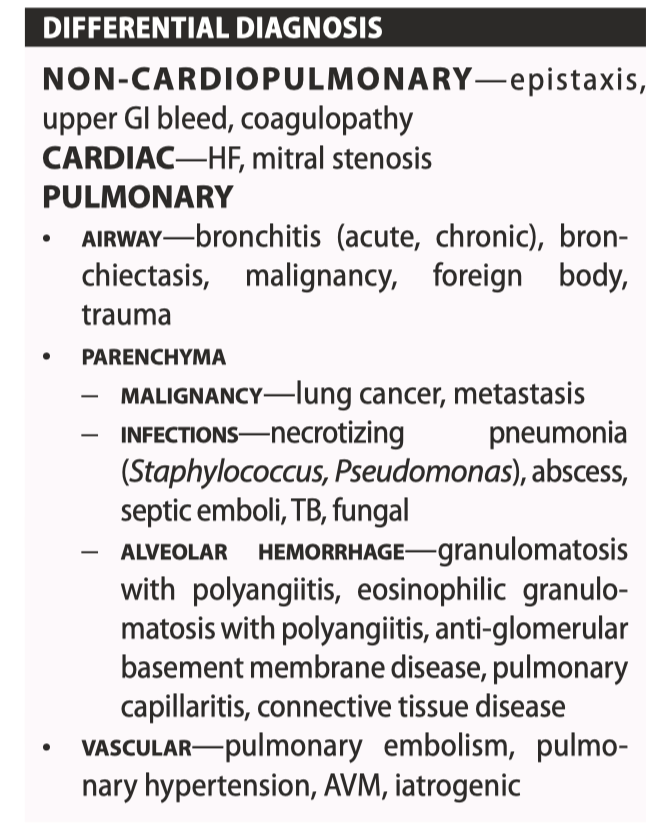
Hemoptysis
Massive: 100–600 mL blood in 24h. Patients may die of asphyxiation
HISTORY—characterize hemoptysis (amount, frequency, previous history), cough (productive), dyspnea, chest pain, epistaxis, hematemesis, weight loss, fever, night sweats, exposure, travel, joint inflammation, rash, visual changes, past medical history (smoking, lung cancer, TB, thromboembolic disease, cardiac disease), medications (warfarin, ASA, NSAIDs, natural supplements)
PHYSICAL—vitals, weight loss, clubbing, cyanosis, lymphadenopathy, Horner syndrome, respiratory and cardiac examination, leg swelling (HF or DVT), joint examination, skin examination
Management: ABC, Intubation, bronchoscopy, IR bronchial artery embolization (<5% risk of spinal cord ischemia); TXA inhaled x 5d, INR elevated → vitamin K 10 mg SC/IV × 1 dose or FFP; abx, rads (tumor) diuresis (HF), immunosuppression (vasculitis)
Syndromes: AntiGBM: hemoptysis + hematuria; Ix: lung/kidney Bx Tx: Steroids, CYC, Plasmapheresis
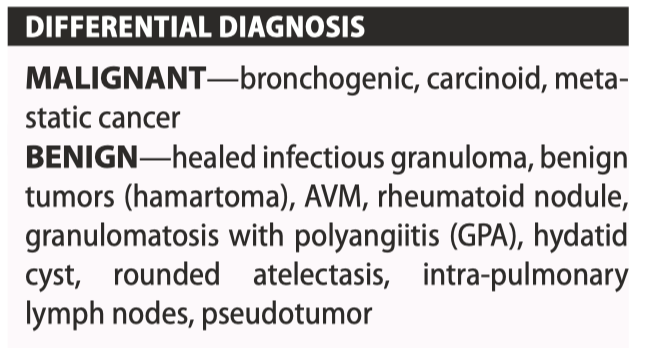
Solitary Pulmonary Nodule
Nodule ≤3 cm well-defined lesion, completely surrounded by lung parenchyma; Mass >3cm
HISTORY—most patients are asymptomatic unless lesion is central; dyspnea, cough, hemoptysis, wheezing, chest pain, weight loss, fever, night sweats, rheumatologic screen, past travel history, occupational exposures, medical history (smoking, lung cancer or other malignancies, TB, infections, rheumatoid arthritis), medications
PHYSICAL—vitals, weight loss, clubbing, cyanosis, Horner syndrome, SVC syndrome, lymphadenopathy, respiratory examination, abdominal examination (hepatomegaly), bony tenderness
High Risk: ABCD (age >50), border irregular/nodular/corona radiata, calcium (eccentric and NONcalcified), diameter (>3cm); timing <30d or >2yrs is low risk
FLEISCHNER guidelines CT between 3,6, or 12mo (<6mm vs. >6mm usually)
PANCOAST TUMOR - squamous cell CA (superior sulcus), features of Horner (ptosis, miosis, anhidrosis, EOM), shoulder pain C8-T2
THORACIC OUTLET OBSTRUCTION - neurovascular (C8/ T1 > C5/C6/C7, 95%): secondary to: anatomic (cervical ribs, congenital bands, subclavicular artery aneurysm), repetitive hyperabduction/trauma (hyperextension injury, painters, musicians), neoplasm (supraclavicular lymphadenopathy)
Pulmonary Hypertension
Group 1: Pulm Arterial HTN (idiopathic, familial, drug (fenphen), CTD, HIV, portal HTN, congenital heart, schistomatosis; CCB responders, pulmonary veno-occlusive disease, pulmonary–capillary hemangiomatosis, PPHN
Group 2: LEFT HEART DISEASE—heart disease with preserved LVEF, heart disease with reduced LVEF, valvular heart disease, cardiovascular conditions leading to postcapillary PH
Group 3: Lung disease/Hypoxemia - obstructive lung disease, restrictive lung disease, mixed restrictive/obstructive disease, including obstructive sleep apnea and obesity hypoventilation syndrome, developmental lung disease
Group 4: PULMONARY ARTERY OBSTRUCTIONS— CTEPH other pulmonary artery obstructions (i.e. tumor, parasites, foreign material)
Group 5: MULTIFACTORIAL—hematological (pulmonary Langerhans cell histiocytosis, lymphangiomatosis), systemic and metabolic disorders (sarcoidosis), complex congenital heart disease, others (compression of pulmonary vessels by tumor, fibrosing mediastinitis)
MPAP (mean pulm artery press): >25 mmHg at rest or mean PAP >30 mmHg with exercise
HISTORY—unexplained dyspnea on exertion, cough, chest pain, hemoptysis, dizziness, syncope, hoarseness, past medical history (cardiac and respiratory diseases, thromboembolic diseases, HIV, cirrhosis, autoimmune and rheumatologic disorders), medications (amphetamine, diet pill such as dexfenfluramine)
PHYSICAL—vitals (tachypnea, tachycardia, atrial fibrillation, hypoxemia), peripheral cyanosis, small pulse volume, elevated JVP (prominent a wave or absent if atrial fibrillation, large v wave), right ventricular heave, loud or palpable P2, right-sided S4, tricuspid regurgitation murmur, Graham-Steell murmur (high-pitched, decrescendo diastolic rumble over LUSB), crackles, congestive liver, ascites, ankle edema
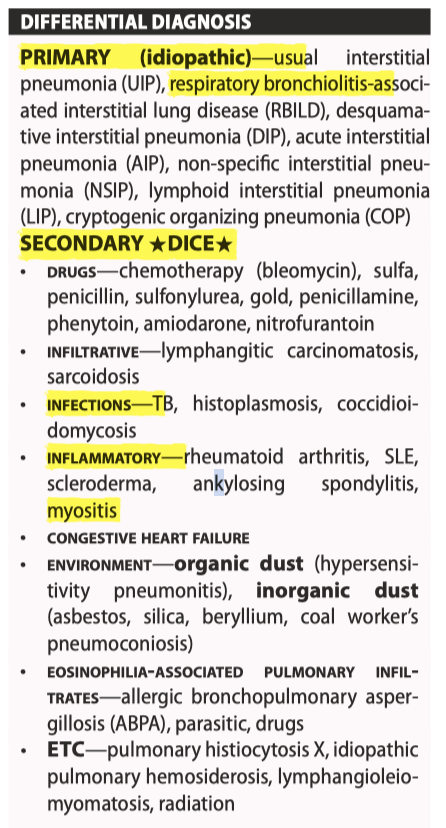
Interstitial Lung Disease
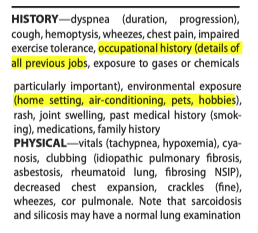
HISTORY—dyspnea (duration, progression), cough, hemoptysis, wheezes, chest pain, impaired exercise tolerance, occupational history (details of all previous jobs, exposure to gases or chemicals particularly important), environmental exposure (home setting, air-conditioning, pets, hobbies), rash, joint swelling, past medical history (smoking), medications, family history
PHYSICAL—vitals (tachypnea, hypoxemia), cyanosis, clubbing (idiopathic pulmonary fibrosis, asbestosis, rheumatoid lung, fibrosing NSIP), decreased chest expansion, crackles (fine), wheezes, cor pulmonale. Note that sarcoidosis and silicosis may have a normal lung examination
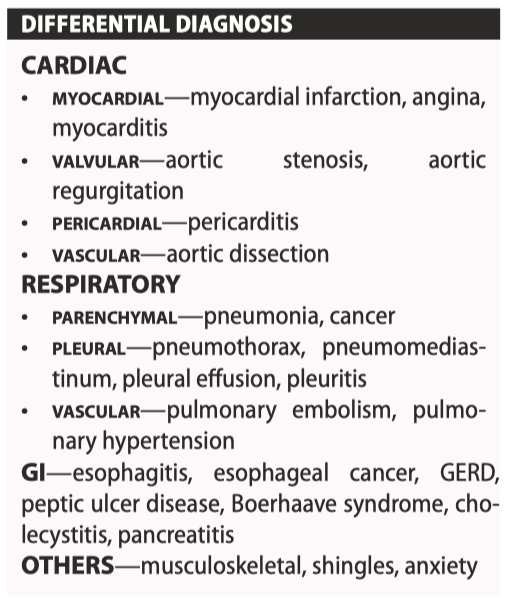
Obstructive Sleep Apnea
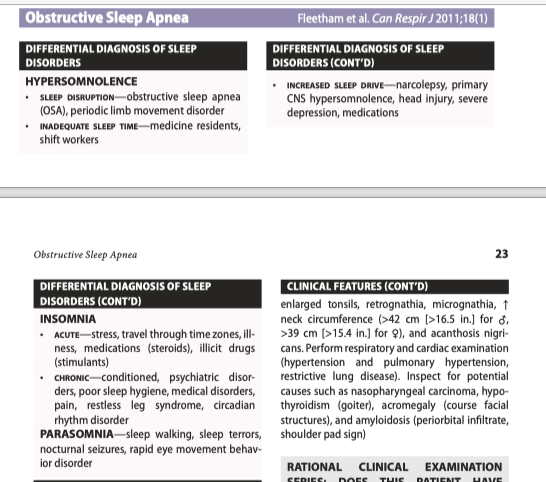
ASSOCIATIONS—obesity, hypothyroidism, acromegaly, amyloidosis, neuromuscular disease, vocal cord paralysis, nasopharyngeal carcinoma, Down syndrome (macroglossia) COMPLICATIONS—hypertension, pulmonary hypertension, CAD, CVA, increased motor vehicle accidents
HISTORY—daytime sleepiness, habitual snoring, witnessed apneic episodes, poor sleep hygiene, morning headaches, fall asleep while driving, dyspnea, cough, exercise capacity, short-term memory loss, excessive caffeine intake, alcohol intake, past medical history (weight gain, thyroid disease, neurological disease), and medications. The Epworth Sleepiness Scale and STOP-Bang Questionnaire may be used as screening tools
PHYSICAL—vitals (hypertension, hypoxia). Obtain weight and height (BMI often >30 kg/m2 ). Asterixis and plethora secondary to hypercapnia. Check for low-hanging soft palate, large uvula, enlarged tonsils, retrognathia, micrognathia, ↑ neck circumference (>42 cm [>16.5 in.] for Male, >39 cm [>15.4 in.] for Female), and acanthosis nigricans. Perform respiratory and cardiac examination (hypertension and pulmonary hypertension, restrictive lung disease). Inspect for potential causes such as nasopharyngeal carcinoma, hypothyroidism (goiter), acromegaly (course facial structures), and amyloidosis (periorbital infiltrate, shoulder pad sign)
![<p>ASSOCIATIONS—obesity, hypothyroidism, acromegaly, amyloidosis, neuromuscular disease, vocal cord paralysis, nasopharyngeal carcinoma, Down syndrome (macroglossia) COMPLICATIONS—hypertension, pulmonary hypertension, CAD, CVA, increased motor vehicle accidents</p><p></p><p>HISTORY—daytime sleepiness, habitual snoring, witnessed apneic episodes, poor sleep hygiene, morning headaches, fall asleep while driving, dyspnea, cough, exercise capacity, short-term memory loss, excessive caffeine intake, alcohol intake, past medical history (weight gain, thyroid disease, neurological disease), and medications. The Epworth Sleepiness Scale and STOP-Bang Questionnaire may be used as screening tools </p><p></p><p>PHYSICAL—vitals (hypertension, hypoxia). Obtain weight and height (BMI often >30 kg/m2 ). Asterixis and plethora secondary to hypercapnia. Check for low-hanging soft palate, large uvula, enlarged tonsils, retrognathia, micrognathia, ↑ neck circumference (>42 cm [>16.5 in.] for Male, >39 cm [>15.4 in.] for Female), and acanthosis nigricans. Perform respiratory and cardiac examination (hypertension and pulmonary hypertension, restrictive lung disease). Inspect for potential causes such as nasopharyngeal carcinoma, hypothyroidism (goiter), acromegaly (course facial structures), and amyloidosis (periorbital infiltrate, shoulder pad sign)</p>](https://knowt-user-attachments.s3.amazonaws.com/fc49f2a8-d83a-40de-a87f-b7189b6f7cdb.png)
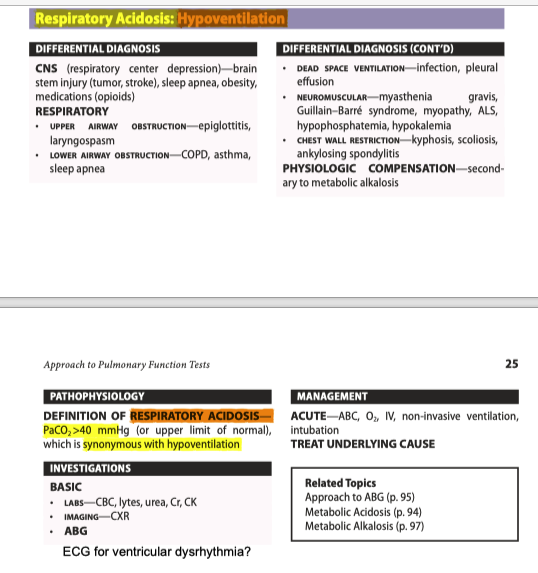
Respiratory Acidosis: Hypoventilation
PaCO2 >40 mmHg (or upper limit of normal), which is synonymous with hypoventilation
Labs + CXR + ABG
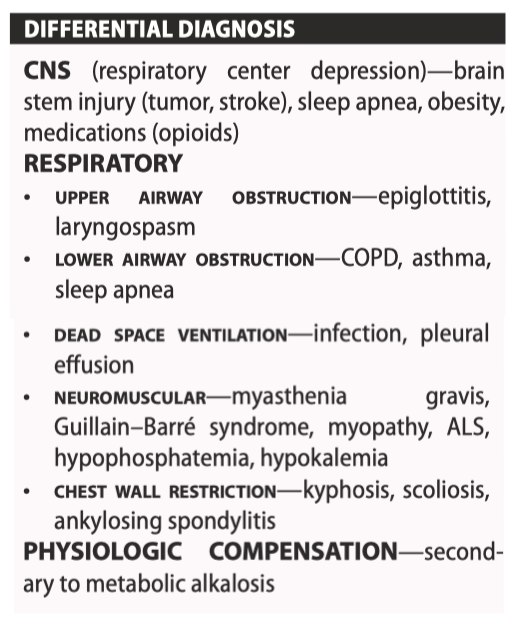
Respiratory Alkalosis: Hyperventilation
PaCO 2<40 mmHg (or lower limit of normal), which is synonymous with hyperventilation
Labs + CXR + ABG
Aortic Dissection
Stanford—A = any ascending aorta involvement, B = all others
Complications:
coronary—acute myocardial infarction (usually RCA)
brachiocephalic, left subclavian, distal aorta—absent or asymmetric peripheral pulse, limb ischemia
renal—anuria, renal failure
carotid—syncope/hemiplegia/death
anterior spinal—paraplegia/quadriplegia, anterior cord syndrome
Stanford—A = any ascending aorta involvement, B = all others
Causes:
• common—hypertension, age, male
• vasculitis—Takayasu arteritis, giant cell arteritis, rheumatoid arthritis, Behçet syndrome, syphilitic aortitis
• collagen disorders—Marfan syndrome, Ehlers–Danlos syndrome, Loeys-Dietz, cystic medial necrosis
• valvular—bicuspid aortic valve, aortic coarctation, Turner syndrome, aortic valve replacement
• others—cocaine, trauma, pregnancy, iatrogenic (e.g. cardiac catheterization)
CXR FINDINGS—wide mediastinum (>6 cm)
ABC—O 2 to keep sat >95%, IV, antihypertensive therapy (keep HR <60 bpm and SBP <120 mmHg.
Labetalol 2 mg/min IV loading drip, then 2–8 mg/min (target heart rate 55–60 bpm) or 20–80 mg IV q10 min, maximum 300 mg, then 200–400 mg PO BID.
Type A (emergent surgical repair, endovascular stenting, longterm blood pressure control). Type B (medical blood pressure control)
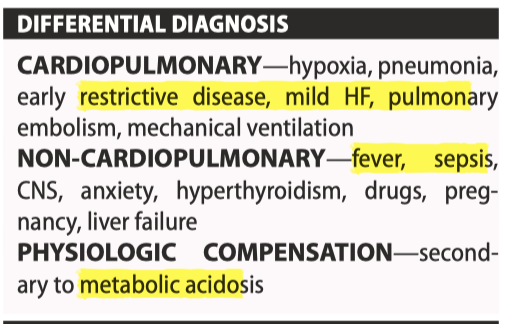
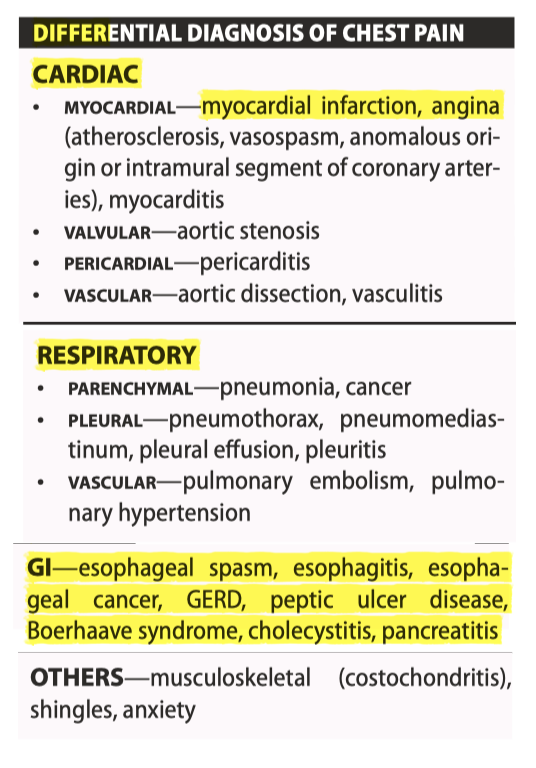
Chest Pain
Types: 1 (ACS - plaque rupture), 2 (demand schema), 3 (death), 4 (PCI), 5 (CABG)
RISK FACTORS
• major—diabetes, hypertension, dyslipidemia, smoking, family history of premature CAD, advanced age, male gender
• associated—obesity, metabolic syndrome, sedentary lifestyle, high-fat diet
• emerging—lipoprotein abnormalities, inflammation (↑ CRP), chronic infections, chronic kidney disease
POST–MI COMPLICATIONS—arrhythmia (VT/ VF, bradycardia), sudden death, papillary muscle rupture/dysfunction, myocardial rupture (ventricular free wall, interventricular septum), ventricular aneurysm, left ventricular thrombus, valvular disease (especially acute mitral regurgitation), heart failure/cardiogenic shock, peri-infarction pericarditis, post-cardiac injury pericarditis (Dressler syndrome)
NYHA: 1, 2 (>2 block 1 stair), 3 (minimal), 4 (rest)
CCS angina 1, 2 (slight limitation, angina w/meals/cold/stress), 3 (marked; <1-2 blocks <1 stairs), 4 (none w/o angina)
DDX Elevated Trop:
• cardiac—myocardial infarction, myocarditis, congestive heart failure, ventricular hypertrophy, pericarditis, vasospasm, tachycardia with supply–demand mismatch, drug/cocaine ingestion, stress (takotsubo) cardiomyopathy, vasculitis
• pulmonary—pulmonary embolism, pulmonary hypertension, COPD exacerbation
• hepatic—liver failure
• renal—chronic kidney disease
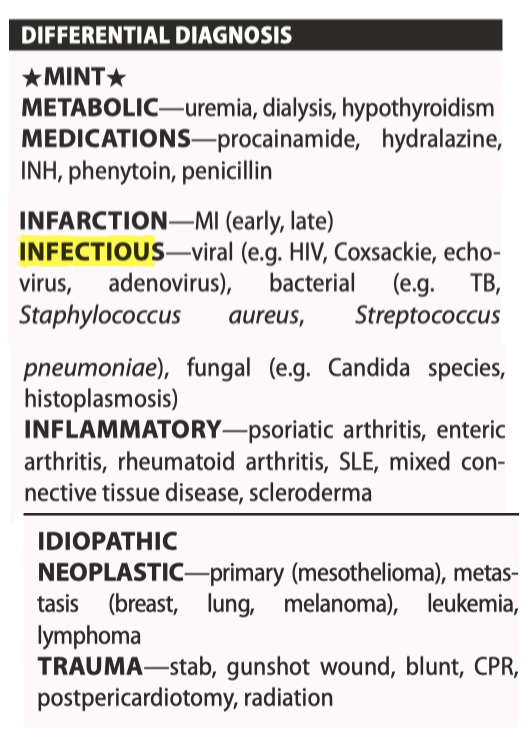
Pericarditis
ACUTE PERICARDITIS (likely 2’ URTI)—NSAIDs (indomethacin/ibuprofen) for most cases of idiopathic or viral pericarditis, but avoid after acute MI. If post-MI, ASA + colchicine. CTD (Prednisone).
Recurrent pericarditis: likely 2’ rheumatologic disorders, Dressler syndrome, and post-pericardiotomy syndrome
TAMPONADE—ABC, O2 , IVs, bolus IV fluids, pericardiocentesis (subxyphoid blind approach, echocardiogram-guided parasternal or apical approach), pericardiectomy, pericardial window if recurrent/malignant effusion. Avoid nitroglycerin and morphine; clinical diagnosis based on dyspnea, tachycardia, hypotension, pulsus paradoxus, and elevated JVP. Tamponade causes restriction in left or right ventricular diastolic filling. Tamponade with inflammatory signs suggests malignant effusion (LR+ 2.9)
CONSTRICTIVE PERICARDITIS—consider diuresis if evidence of volume overload. Severe, medically-refractory cases may require surgical pericardiectomy; contraction of pericardium due to chronic inflammation, leading to left and/or right heart failure. May follow pericarditis or radiation. May be difficult to distinguish from restrictive cardiomyopathy clinically
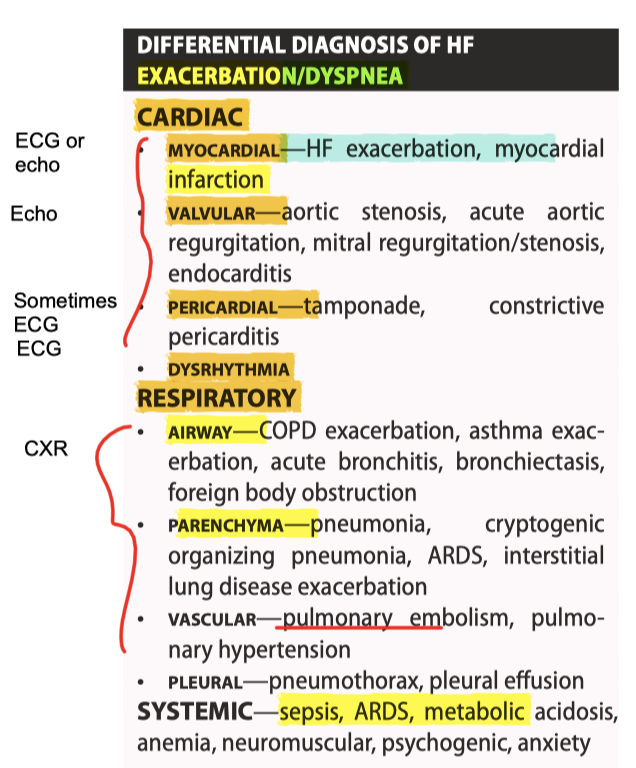
Heart Failure (vs. Dyspnea)
Classification (HFMEF 41-49%), HFREF (<=40%), HFPEF (>=50%)
Anatomical causes: dilated CM (idiopathic, ischemic, valvular, viral, genetic, late manifestation of hypertrophic heart disease, tachycardia induced, alcohol induced, peripartum); hypertrophic, idiopathic (autosomal dominant), storage (Fabry disease, Pompe disease, Hurler syndrome, Noonan syndrome), athlete’s heart (usually reversible), obesity, amyloid; Restrictive CM (familial, infiltrative (amyloidosis, hemochromatosis, sarcoidosis), drugs, radiation, endomyocardial fibrosis); arrhythmogenic RV dysplasia (replacement of right ventricular free wall with fatty tissue); other than(endocardial fibroelastosis, left ventricular non-compaction)
Etiologic Causes: Ischemic (dilated), Valvular (dilated), HTN (dilated, restrictive), diabetic (dilated), inflammatory (dilated; 2’ infection, autoimmune, idiopathic), metabolic (dilated, restrictive, hypertrophic) such as endocrine (thyrotoxicosis, hypothyroidism, acromegaly, pheochromocytoma), storage diseases (glycogen storage disease, Fabry disease, Gaucher dz, Nieman Pick), nutritional (beriberi, Kwashiorkor, pellagra), deposition (amyloidosis, hemochromatosis, sarcoidosis), muscular dystrophy (dilated), neuromuscular—Friedreich ataxia (hypertrophic), Noonan syndrome, lentiginosis, general systemic disease (mostly dilated such as CTD - RA, And Spond, SLE, Scleroderma, dermatomyositis; granulomatous (sarcoid, GPA, myocarditis), neoplasm; toxins (dilated; alcohol, amphetamine, arsenic, catecholamines, cocaine, anthracyclines, zidovudine, radiation (restrictive as well), peripartum
PRECIPITANTS OF HF ★FAILURE★: forget to take medications (non-adherence); Arrhythmia, anemia; Infection, ischemia, infarction; Lifestyle change (e.g. high salt and/or fluid intake); Upregulators (thyroid, pregnancy), Rheumatic heart disease, acute valvular disease; Embolism
CAUSES OF FLASH PULMONARY EDEMA - cardiac (ischemic heart disease, acute aortic regurgitation, acute mitral regurgitation, mitral stenosis/obstruction, arrhythmia), pulmonary (pulmonary embolism, pneumonia), renal (bilateral renal artery stenosis), systemic (hypertension crisis, fever, sepsis, anemia, thyrotoxicosis)
LHF—left-sided S3, rales, wheezes, tachypnea. Causes include previous MI, aortic stenosis, and left-sided endocarditis
RHF—right-sided S3, ↑ JVP, ascites, hepatomegaly, peripheral edema. Causes include left heart failure, pulmonary hypertension, right ventricular MI, mitral stenosis, and right-sided endocarditis
EF<35% → CRT ± ICD
Digoxin Intoxication
serum level should be collected at 12–24 h after the last dose (postdistribution phase). While the upper normal limit is 2.6 nmol/L [2.0 ng/mL], higher digoxin levels may be seen in asymptomatic patients. digoxin, resulting in serum levels 0.5–0.9 nmol/L [0.4–0.7 ng/mL] is associated with possible survival benefit compared to ≥1 nmol/L [≥0.78 ng/ mL] in HF patients
For instance, hypokalemia, hypernatremia, hypomagnesemia and acidosis predispose to toxicity even at low-serum digoxin levels because of their depressive effects on the Na/K ATPase pump. In contrast, hyperkalemia occurs in acute toxicity and is directly related to prognosis
SIGNS AND SYMPTOMS: neurological—delirium, hallucination, blurred vision with altered color perception, headaches, dizziness; cardiac—bradycardia, high-degree AV block, paroxysmal atrial tachycardia (often 2:1 AV conduction), unifocal or multifocal PVCs, bidirectional ventricular tachycardia, accelerated junctional tachycardia; GI—anorexia, N&V, diarrhea, abdominal pain; metabolic—hyperkalemia
![<p>serum level should be collected at 12–24 h after the last dose (postdistribution phase). While the upper normal limit is 2.6 nmol/L [2.0 ng/mL], higher digoxin levels may be seen in asymptomatic patients. digoxin, resulting in serum levels 0.5–0.9 nmol/L [0.4–0.7 ng/mL] is associated with possible survival benefit compared to ≥1 nmol/L [≥0.78 ng/ mL] in HF patients</p><p>For instance, hypokalemia, hypernatremia, hypomagnesemia and acidosis predispose to toxicity even at low-serum digoxin levels because of their depressive effects on the Na/K ATPase pump. In contrast, hyperkalemia occurs in acute toxicity and is directly related to prognosis</p><p>SIGNS AND SYMPTOMS: neurological—delirium, hallucination, blurred vision with altered color perception, headaches, dizziness; cardiac—bradycardia, high-degree AV block, paroxysmal atrial tachycardia (often 2:1 AV conduction), unifocal or multifocal PVCs, bidirectional ventricular tachycardia, accelerated junctional tachycardia; GI—anorexia, N&V, diarrhea, abdominal pain; metabolic—hyperkalemia</p>](https://knowt-user-attachments.s3.amazonaws.com/43af1038-f76a-4b85-b970-87a6d1d7981e.png)
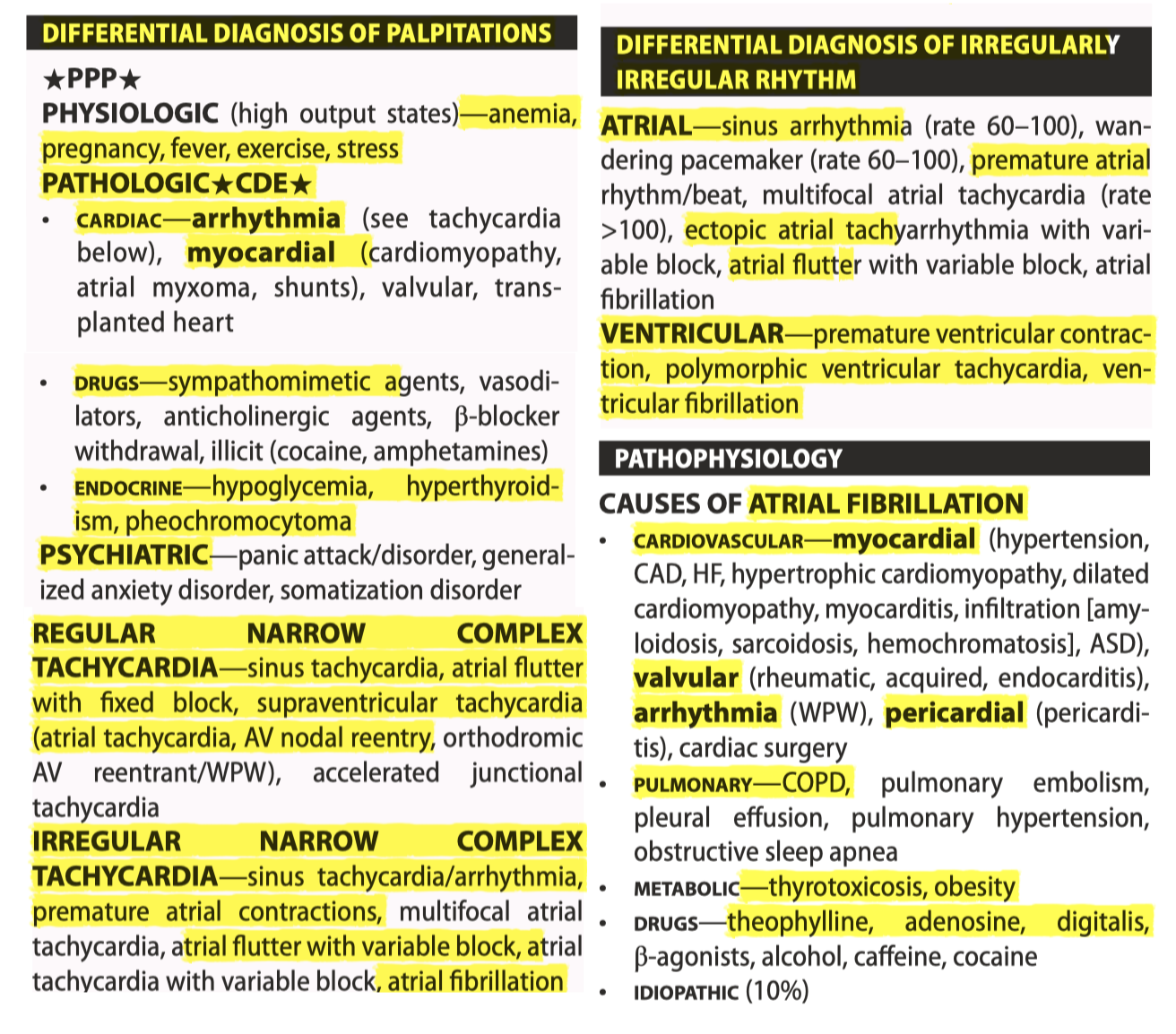
Atrial Fibrillation
Paroxysmal <7d, Persistent >7d, Longstanding >12mo; Permanent
Management
SYNCHRONIZED CARDIOVERSION for unstable: midazolam 1–2 mg IV q2–3 min, fentanyl 50–150 μg IV × 1, shock 50, 100, 200, 300, 360 J, prepare to intubate and give IV anti-arrhythmics PRN
AV NODAL BLOCKING AGENTS ★ABCD★ Amio 150 IV q10-15m, BB - metoprolol 5mg IV over 1min q5min x3; CCB: diltiazem 15–20 mg IV over 2 min, repeat in 15 min at 20–25 mg PRN; digitalis—digoxin 0.25–0.5 mg IV q6h to a total dose of 1 mg, maintenance dose 0.125–0.25 mg PO/IV daily
Amio toxicity: baseline TSH, LFTs, PFT and CXR. TSH and LFTs every 6 months, CXR yearly, and PFT as needed
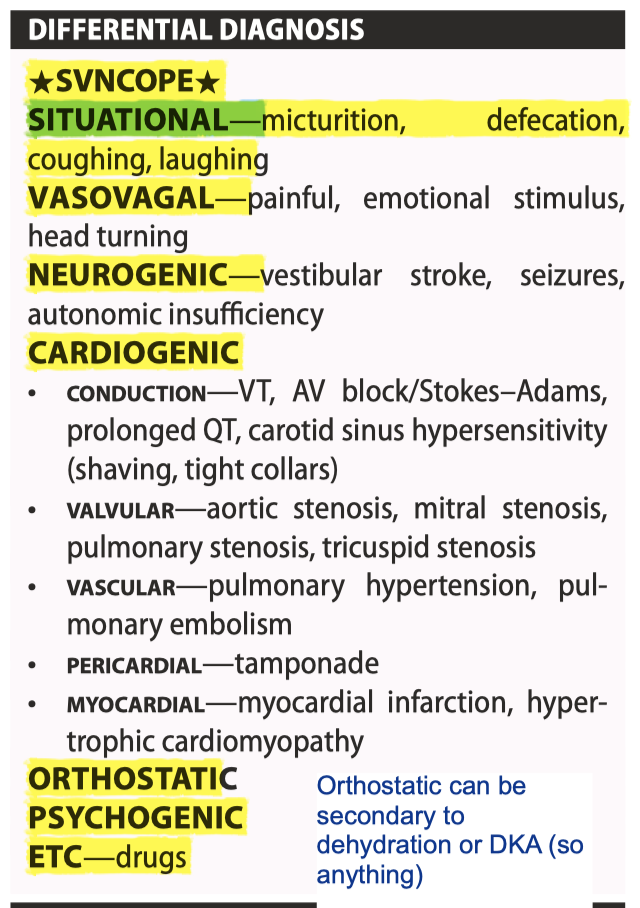
Syncope
HISTORY—N&V before collapse, syncope with exertion, seizure features (tongue biting, incontinence, post-collapse disorientation), last meal, history of cardiac disease (arrhythmias, heart failure, ischemic heart disease, aortic stenosis), previous syncope, seizures, or psychiatric problems, current medications, family history of unexplained syncope or sudden death
PHYSICAL—orthostatic hypotension, irregular or slow-rising pulse, apical-carotid delay, soft or paradoxically split S2, presence of S4, murmurs (particularly aortic stenosis), carotid sinus massage, injuries, decreased level of consciousness, any focal neurological signs
Etiology:
REFLEX SYNCOPE—consists of situational syncope, vasovagal syncope, and carotid sinus syndrome
NEUROCARDIOGENIC (VASOVAGAL) SYNCOPE weakness, light-headedness, diaphoresis, visual blurring, headache, nausea, and feeling warm or cold. Syncope lasts about 30 s to 5 min. Recovery is rapid with minimal postictal state; —tilt-table test (spc 90%), implantable loop recorders
Situational: coughing, swallowing, urination, and defecation, respectively
NEUROGENIC ORTHOSTATIC - lightheadedness, dizziness, syncope, weakness, fatigue, angina, orthostatic dyspnea. Typically happens in older individuals and exacerbated by prolonged standing, strenuous exercises, high temperature, and meals; causes—physical deconditioning, medications (alpha-blockers, antihypertensives, diuretics), Parkinson disease, Lewy body dementia, multisystem atrophy, pure autonomic failure; SBP drop of ≥20 mmHg or DBP drop of ≥10 mmHg during first 3 min of standing, or a head-up tilt on tilt table
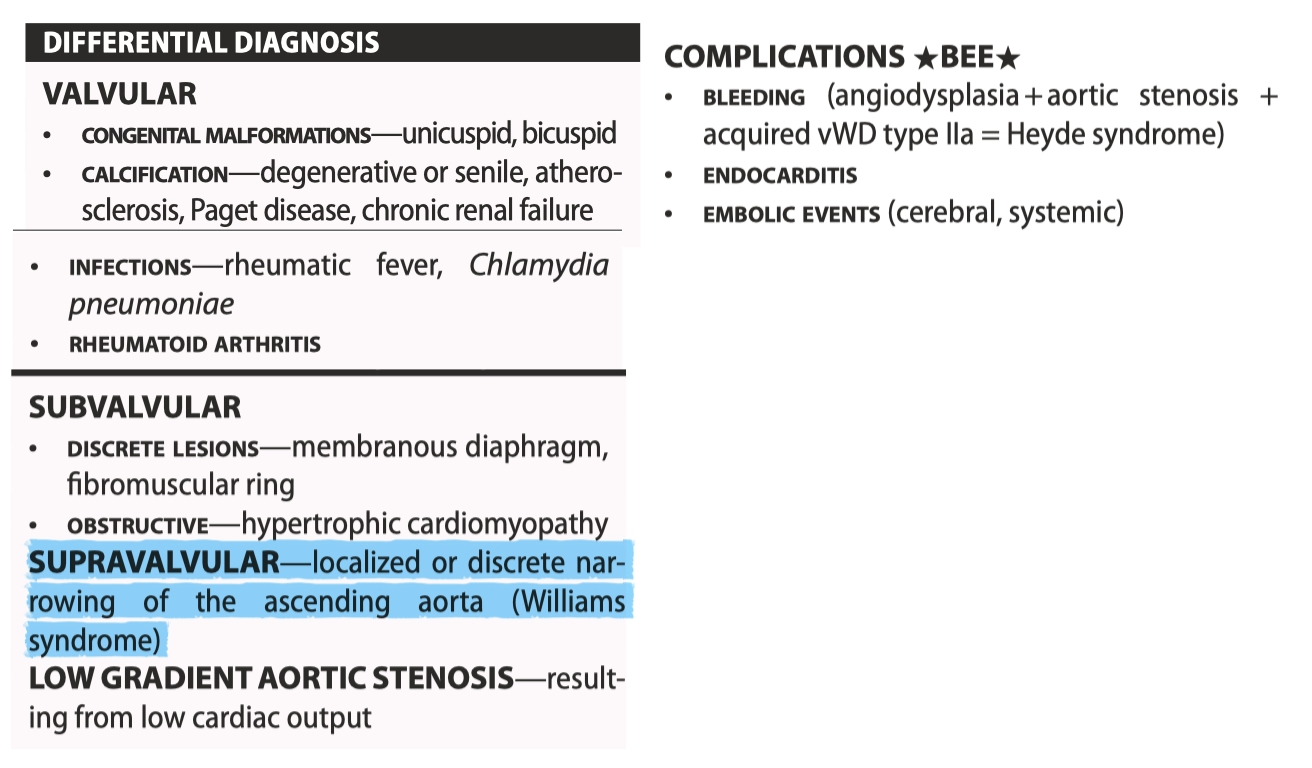
Aortic Stenosis
PHYSICAL—tachypnea, decreased pulse pressure, brachioradial delay, pulsus parvus et tardus (slow rise and low amplitude), apical-carotid delay, hyperdynamic apical beat, systolic thrill at the base of heart, narrowly split or paradoxical splitting of S2 or absent S2, harsh mid-systolic ejection murmur (radiation to carotids), Gallavardin phenomenon
GALLAVARDIN PHENOMENON—aortic stenosis murmur is usually harsh and loudest over the right upper sternal border, whereas a Gallavardin murmur is musical and may be heard over apex. It is due to radiation of the high-frequency components of the aortic stenosis murmur to the apex
AS severe = peak velocity ≥4 m/s, mean gradient >40 mmHg, area = ≤1 cm 2 (or indexed area ≤ 0.6 cm2 /m2 )
PROGNOSIS OF AORTIC STENOSIS ★ASH★ (Angina 50% in 5 yrs mortality, Syncope 50% mortality in 3 yr, Heart failure 50% in 2 yrs, post Sx = normal survival)
Class 1 Indications for Valve replacement: symptoms of HF, syncope, exertional dyspnea, angina, or presyncope (by history or on exercise testing); asymptomatic severe AS and LVEF <50%; or severe AS and undergoing cardiac surgery for other reasons
2A reasonable—if asymptomatic but very severe AS (i.e. peak velocity ≥5 m/s or mean gradient ≥60 mmHg); severe AS and exercise test with ↓ exercise tolerance or ↓ in SBP; symptomatic low-flow/low-gradient severe AS (i.e. valve area ≤1 cm2 ) with LVEF <50%, and severe/high gradients on dobutamine stress test; symptomatic low-flow/low-gradient severe AS (i.e. valve area ≤1 cm2 ) with normal LVEF ≥50% and valve obstruction as most likely cause of symptoms (based on clinical, hemodynamic, and anatomic data); or moderate AS and undergoing cardiac surgery for other reasons possible indications
2B: if severe AS and rapid disease progression and low surgical risk
TAVR should be considered for patients with an indication for AVR who have intermediate-to-high or prohibitive risk for surgical AVR.
Mechanical: lasts longer but MORE VTE risk → needs warfarin
BIOprosthetic valve: for those CI to warfarin (childbearing women)/noncomplaint; >65 w/o VTE risk factors
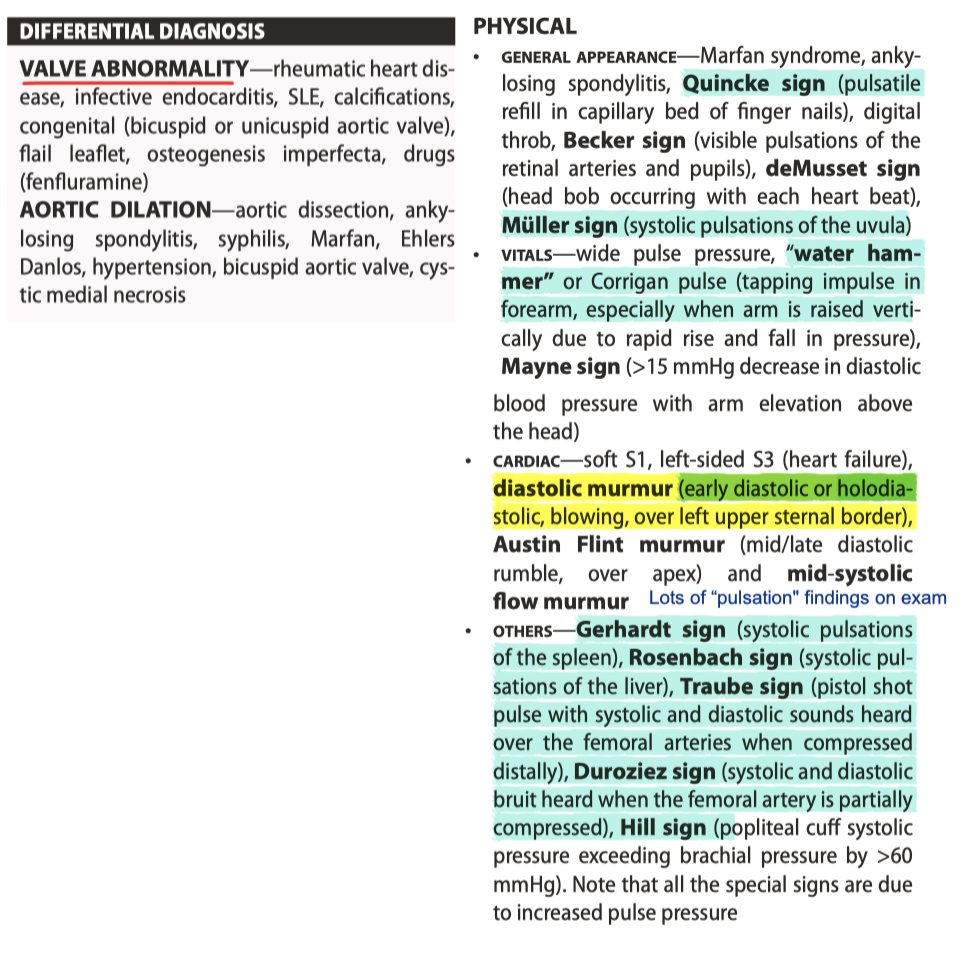
Aortic Regurgitation
LV dilatation and eccentric hypertrophy (palpitations, atypical chest pain), wide pulse pressure (due to increased stroke volume with elevation in SBP and regurgitation with rapid collapse of the arteries and a low diastolic blood pressure) → eventually → LV dysfunction
pulmonary regurgitation murmur—high pitch decrescendo diastolic murmur (Graham Steell murmur) loudest over left upper sternal border. Increases with inspiration. May be associated with signs of pulmonary hypertension
• aortic regurgitation murmur—early diastolic decrescendo murmur loudest over right and/or left upper sternal border. No change or decreases with inspiration. May be associated with Austin Flint murmur and the other signs of aortic regurgitation
Class 1: if symptomatic severe AR; asymptomatic chronic severe AR (regurgitant fraction ≥50%, regurgitant volume ≥60 mL/beat, Doppler jet width ≥65% of LVOT) and LVEF <50%; or severe AR and undergoing cardiac surgery for other reasons
2A: Reasonable —if asymptomatic severe AR with normal LVEF ≥50% but severe LV dilatation (LVESD >50 mm); or moderate AR and undergoing other cardiac surgery
2B: Possible—if asymptomatic severe AR and normal LVEF ≥50% but with progressive severe LV dilatation (LVEDD >65 mm) and low surgical risk
F/U:
Mild + ASX with normal LV function and little/no LV dilatation can be followed annually with clinical exam and TTE q2-3 years (sooner if symptoms emerge).
Asymptomatic severe AR with normal LV function and LV dilatation (>60 mm) should be seen every 6 months with echocardiogram every 6–12 months
ILD Differential
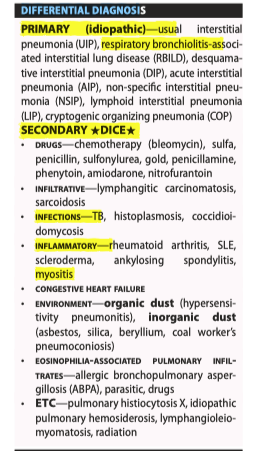
ILD Hx
Differential of OSA
Respiratory acidosis