Hemolytic Anemias
1/154
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
155 Terms
RBC defects in RBC membrane, metabolism, Hgb content (hemoglobinopathies):
intrinsic
RBC defects caused by malaria, drugs, immune hemolysis, trauma, microangiopathic (MAHA: TTP, HUS, DIC):
extrinsic
site of hemolysis that is related to RBC fragmentation (DIC, heart prosthetic pathways):
intravascular
site of hemolysis that is macrophage-mediated, in spleen, BM, or liver:
extravascular
main abnormality formed in intravascular hemolytic anemias:
schistocytes
main abnormality formed in extravascular hemolytic anemias:
spherocytes
total bilirubin is ____ in intravascular hemolytic anemias.
increased
total bilirubin is ____ in extravascular hemolytic anemias.
increased
indirect (unconjugated) bilirubin is ____ in intravascular hemolytic anemias.
increased
indirect (unconjugated) bilirubin is ____ in extravascular hemolytic anemias.
increased
direct (conjugated) bilirubin is ____ in intravascular hemolytic anemias.
normal
direct (conjugated) bilirubin is ____ in extravascular hemolytic anemias.
normal
LDH (LD1) is ____ in intravascular hemolytic anemias.
increased
LDH (LD1) is ____ in extravascular hemolytic anemias.
increased
haptoglobin is ____ in intravascular hemolytic anemias.
decreased
haptoglobin is ____ in extravascular hemolytic anemias.
decreased
free hemoglobin is ____ in intravascular hemolytic anemias.
increased
free hemoglobin is ____ in extravascular hemolytic anemias.
increased
hemopexin is ____ in intravascular hemolytic anemias.
decreased
hemopexin is ____ in extravascular hemolytic anemias.
decreased
urine urobilinogen is ____ in intravascular hemolytic anemias.
increased
urine urobilinogen is ____ in extravascular hemolytic anemias.
increased
urine free hemoglobin is ____ in intravascular hemolytic anemias.
positive
urine free hemoglobin is ____ in extravascular hemolytic anemias.
negative
urine methemoglobin is ____ in intravascular hemolytic anemias.
positive
urine methemoglobin is ____ in extravascular hemolytic anemias.
negative
urine prussian blue staining of urine sediment is ____ in intravascular hemolytic anemias.
positive
urine prussian blue staining of urine sediment is ____ in extravascular hemolytic anemias.
negative
hemoglobin, HCT, and RBC count is ____ in intravascular hemolytic anemias.
decreased
hemoglobin, HCT, and RBC count is ____ in extravascular hemolytic anemias.
decreased
most intrinsic RBC defects are inherited; however, ____ is an exception as it is intrinsic but acquired.
PNH
a 5 year old girl was seen by her physician several days before the current visit and was diagnosed with pneumonia. she was prescribed a standard course of antibiotics. her mother has brought her to the physician again because the girl’s urine began to darken after the first visit and now is alarmingly dark. the girl has no history of anemia, and there is no family history of any hematologic disorder. the CBC shows a mild anemia, polychromasia, and a few schistocytes. this anemia could be categorized as:
a. acquired, fragmentation
b. acquired, macrophage mediated
c. hereditary, fragmentation
d. hereditary, macrophage mediated
acquired, fragmentation
a patient has a personal and family history of a mild hemolytic anemia. the patient has consistently elevated levels of total and indirect serum bilirubin and urinary urobilinogen. the serum haptoglobin level is consistently decreased, whereas the reticulocyte count is elevated. the latter can be seen as polychromasia on the patient’s peripheral blood film. spherocytes are also noted. which one of the findings reported for this patient is inconsistent with a classical diagnosis of fragmentation hemolysis?
a. elevated total and indirect serum bilirubin
b. elevated urinary urobilinogen
c. decreased haptoglobin
d. spherocytes on the peripheral blood film
spherocytes on the peripheral blood film
an intrinsic defect of mutations in proteins which maintain vertical attachments:
hereditary spherocytosis
mostly mutations in ankyrin and spectrin:
hereditary spherocytosis
RBCs lose surface area (low s/v ratio), lose deformability, destroyed by the spleen leading to ____ hemolysis, or some RBCs may endure further membrane modifications forming microspherocytes.
extravascular
refers to the triad in hereditary spherocytosis:
anemia, splenomegaly, jaundice
hallmark of ____ is spherocytosis (not specific), with increased polychromasia indicative of reticulocytosis (up to 10%):
hereditary spherocytosis
RBC indices of hereditary spherocytosis have high ____ (> 36 mg/dL).
MCHC
RBC indices of hereditary spherocytosis have high ____ (> 4%).
CHCM
indirect bilirubin is ____ in hereditary spherocytosis.
increased
LDH is ____ in hereditary spherocytosis.
increased
haptoglobin is ____ in hereditary spherocytosis.
decreased
childhood hemolytic anemia, family history of similar abnormalities, uniform spherocytes on PBS is highly suggestive of:
hereditary spherocytosis
family history, splenomegaly, high MCHC, reticulocytosis, and spherocytes on the PBS is indicative of:
hereditary spherocytosis
in hereditary spherocytosis, osmotic fragility test would be ____
increased
in hereditary spherocytosis, eosin-5’-maleimide (EMA) binding test is ____.
decreased
defects in horizontal interactions:
hereditary elliptocytosis
95% of cases of hereditary elliptocytosis is a mutation in ____ genes (alpha and beta).
spectrin
RBCs become elliptical over time in hereditary elliptocytosis. true or false?
true
severe form of hereditary elliptocytosis in which RBCs are fragmented on heating due to low stability (41-45°C):
HPP
extreme poikilocytosis, MCV is very low (50-65 fL), fragmentation, microspherocytosis, and elliptocytosis (similar to burns):
HPP
RBC membrane is highly permeable and deficiency in stomatin protein or mutation in RhAG protein:
overhydrated hereditary stomatocytosis
dehydrated hereditary stomatocytosis may also be known as:
hereditary xerocytosis
defect in membrane cation permeability causing RBCs to become dehydrated:
dehydrated hereditary stomatocytosis
a patient has anemia that has been worsening over the last several months. the hemoglobin level has been declining slowly, with a drop of 1.5 g/dL of hemoglobin over about 6 weeks. polychromasia and anisocytosis are seen on the peripheral blood film, consistent with the elevated reticulocyte count and RDW. serum levels of total bilirubin and indirect fractions are normal. the urinary urobilinogen level also is normal. when these findings are evaluated, the conclusion drawn that the anemia does not have a hemolytic component. based on the data given here, why was hemolysis ruled out as the cause of anemia?
a. the decline of hemoglobin is too gradual to be associated with hemolysis
b. the elevation of the reticulocyte suggests a malignant cause
c. evidence of increased protoporphyrin catabolism is lacking
d. elevated RDW points to an anemia of decreased production
evidence of increased protoporphyrin catabolism is lacking
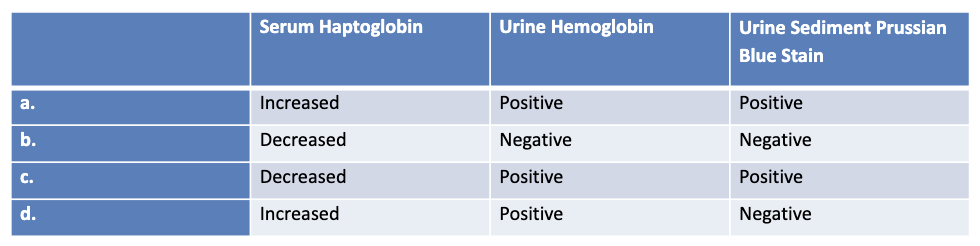
which of the following sets of test results is typically expected with chronic fragmentation hemolysis? (*refer to image)
c
rare chronic, intravascular hemolytic anemia, acquired membrane defect:
PNH
RBCs lack CD55 and CD59 in:
PNH
in PNH, the absence of CD55 and CD59 renders RBCs susceptible to lysis by ____.
complement
RBCs display mosaicism where some RBCs are normal and some are abnormal:
PNH
what level of PNH shows normal level of CD55 and CD59 with little or no lysis?
type I
what level of PNH shows partial CD55 and CD59 deficiency with relative resistance to lysis?
type II
what level of PNH shows complete deficiency in CD55 and CD59 and is highly sensitive to lysis?
type III
most common RBC types in PNH:
combination of I and III
detection of CD55 and CD59 by flow cytometry is the confirmatory test of ____.
PNH
critical to RBCs as it is the only means to produce NADPH to maintain a healthy supply of reduced glutathione:
G6PD
G6PD enzyme is encoded on the ____ chromosome.
X
most common RBC enzyme defect:
G6PD deficiency
african males with ____ (A- variant) are protected against plasmodium falciparum malaria.
G6PD deficiency
oxidizing drugs, infections, and fava beans are triggers of acute hemolytic anemia in:
G6PD deficiency
G6PD deficiency anemia is moderate to severe with usually ____ RBCs.
normocytic/normochromic
denatured Hgb that is only seen in supravital stains:
heinz bodies
in G6PD deficiency, serum haptoglobin is very ____.
decreased
in G6PD deficiency, indirect bilirubin is ____.
increased
in G6PD deficiency, LDH is ____.
increased
in G6PD deficiency, plasma hemoglobin (intravascular hemolysis) is ____.
increased
a patient experiences an episode of acute intravascular hemolysis after taking primaquine for the first time. the physician suspects that the patient may have G6PD deficiency and orders an RBC G6PD assay 3 days after the hemolytic episode began. how will this affect the test result?
a. absence of enzyme activity
b. false decrease in enzyme activity due to hemoglobinemia
c. false increase in enzyme activity due to reticulocytosis
d. no effect on enzyme activity
false increase in enzyme activity due to reticulocytosis
key enzyme of the glycolytic pathway:
pyruvate kinase
catalyzes the conversion of phosphenolpyruvate to pyruvate forming ATP:
pyruvate kinase
PK deficiency causes premature destruction of ____.
RBCs
clinical presentation includes anemia, jaundice, splenomegaly and gallstones (chronic hemolysis):
PK deficiency
in PK deficiency, ____ experience severe anemia.
neonates
in PK deficiency, ____ experience severe to compensated anemia.
adults
echinocytes (burr cells) are highly indicative of:
PK deficiency
conditions where RBC survival is shortened because of antibody-mediated mechanisms:
immune hemolytic anemia
some antibodies of immune hemolytic anemia are able to activate ____.
complement
in immune hemolytic anemia, RBCs with antibodies or complement are removed by ____ (extravascular).
macrophages
in immune hemolytic anemia, RBCs with antibodies or complement are removed by ____ (intravascular).
complemented mediated hemolysis
in immune hemolytic anemia, RBCs with antibodies or complement cannot be removed by a combination of extravascular and intravascular processes. true or false?
false
____ mediated hemolysis can result in both extravascular and intravascular hemolysis.
IgM
____ mediated hemolysis is predominantly extravascular RBCs removed by macrophages in the spleen/liver.
IgG
immune hemolytic anemia is DAT ____.
positive
premature RBC destruction and anemia caused by autoantibodies that bind to the RBC surface with or without complement activation:
autoimmune hemolytic anemia
what are the 4 types of autoimmune hemolytic anemias?
WAIHA, CAD, PCH, mixed AIHA
what is the most common type of autoimmune hemolytic anemia?
WAIHA
what immunoglobulin is associated with WAIHA?
IgG
what is the optimum reactivity temperature of autoantibody for WAIHA?
37°C
what is the complement activation for WAIHA?
variable
what is type of hemolysis is primarily associated with WAIHA?
extravascular