Chapter 34: Hematologic Problems Harding: Lewis’s Medical-Surgical Nursing, 12th Edition
1/46
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
47 Terms
An adult male is experiencing increased fatigue and occasional palpitations at rest. Which laboratory data would the nurse identify as consistent with these symptoms?
a. RBC count of 4,500,000/L
b. Hematocrit (Hct) value of 38%
c. Normal red blood cell (RBC) indices
d. Hemoglobin (Hgb) of 8.6 g/dL (86 g/L)
ANS: D
A low Hgb level can result in symptoms such as fatigue and palpitations, common in patients with anemia. The other values are all within the range of normal.
Which menu choice indicates that the patient understands the nurse's recommendations about dietary choices to manage iron-deficiency anemia?
a. Turkey on whole wheat bread
b. Cantaloupe and cottage cheese
c. Strawberry and banana fruit plate
d. Cornmeal muffin and orange juice
ANS: A
Poultry and whole grain breads are high in iron. The other choices are appropriate for other nutritional deficiencies but are not the best choice for a patient with iron-deficiency anemia.
A patient develops a megaloblastic anemia as an adverse effect of drug therapy. Which nutrient supplement would the nurse plan to explain to the patient?
a. Iron
b. Folic acid
c. Magnesium
d. Ascorbic acid (vitamin C)
ANS: B
Some drugs (such as phenytoin) interfere with absorption or use of folic acid, leading to megaloblastic anemia. Supplementation with oral folic acid supplements is the usual treatment. The other nutrients would not correct folic acid deficiency, although they would be used to treat other types of anemia.
Which patient statement to the nurse indicates that the patient understands self-care for pernicious anemia?
a. I need to start eating more red meat and liver.
b. I will stop having a glass of wine with dinner.
c. I could choose nasal spray rather than injections of vitamin B12.
d. I will need to take a proton pump inhibitor such as omeprazole.
ANS: C
Because pernicious anemia prevents the absorption of vitamin B12, this patient requires injections or intranasal administration of cobalamin. Alcohol use does not cause cobalamin deficiency. Proton pump inhibitors decrease the absorption of vitamin B12. Eating more foods rich in vitamin B12 is not helpful because the lack of intrinsic factor prevents absorption of the vitamin.
Which intervention would the nurse plan for a hospitalized patient who has severe hemolytic anemia?
a. Provide a diet high in vitamin K.
b. Teach the patient how to avoid injury.
c. Encourage alternating rest and activity.
d. Place the patient on protective isolation.
ANS: C
Nursing care for patients with anemia should alternate periods of rest and activity to avoidundue fatigue. There is no indication that the patient has a bleeding disorder, so a diet high in vitamin K or teaching about how to avoid injury is not needed. Protective isolation might be
used for a patient with aplastic anemia, but it is not indicated for hemolytic anemia.
Which patient statement to the nurse indicates a need for additional instruction about taking oral ferrous sulfate?
a. I could take a stool softener if I feel constipated.
b. I can take the iron with orange juice before eating.
c. I should notify my health care provider if my stools turn black.
d. I will increase my fluid and fiber intake while I am taking iron.
ANS: C
It is normal for the stools to appear black when a patient is taking iron, and the patient should not call the health care provider about this. The other patient statements are correct.
Which potential complication would the nurse identify as a high risk for a patient admitted to the hospital with idiopathic aplastic anemia?
a. Seizures
b. Infection
c. Neurogenic shock
d. Pulmonary edema
ANS: B
Because the patient with aplastic anemia has pancytopenia, the patient is at risk for infection and bleeding. There is no increased risk for seizures, neurogenic shock, or pulmonary edema
Which nursing intervention is important when providing care for a patient in sickle cell crisis?
a. Limiting the patient's intake of oral and IV fluids
b. Evaluating the effectiveness of opioid analgesics
c. Encouraging the patient to ambulate as much as tolerated
d. Teaching the patient about high-protein, high-calorie foods
ANS: B
Pain is the most common clinical manifestation of a crisis and usually requires large doses of continuous opioids for control. Fluid intake should be increased to reduce blood viscosity and
improve perfusion. Rest is usually ordered to decrease metabolic requirements. Patients are instructed about the need for dietary folic acid, but high-protein, high-calorie diets are not emphasized.
Which statement by a patient indicates good understanding of the nurse's teaching about preventing sickle cell crisis?
a. Home oxygen therapy is frequently used to decrease sickling.
b. There are no effective medications that can help prevent sickling.
c. Routine continuous dosage opioids are prescribed to prevent a crisis.
d. Risk for a crisis is decreased by having an annual influenza vaccination.
ANS: D
Because infection is the most common cause of a sickle cell crisis, influenza, Haemophilus influenzae, pneumococcal pneumonia, and hepatitis immunizations should be recommended. Although continuous dose opioids and oxygen may be administered during a crisis, patients
do not receive these therapies to prevent crisis. Hydroxyurea (Hydrea), crizanlizumab -tmca (Adakveo), and voxelotor (Oxbryta) are medications used to decrease the number of sickle cell crises.
Which instruction will the nurse plan to include in discharge teaching for a patient who was admitted with a sickle cell crisis?
a. Limit exposure to crowds.
b. Restrict fluids to 2 liters per day.
c. Take a daily multivitamin with iron.
d. Do not drink any caffeinated beverages.
ANS: A
Exposure to crowds increases the patient's risk for infection, the most common cause of sickle cell crisis. There is no restriction on caffeine use. Iron supplementation is generally not recommended. A high-fluid intake is recommended
The nurse observes scleral jaundice in a patient being admitted with hemolytic anemia. Which laboratory result would the nurse check?
a. Schilling test
b. Bilirubin level
c. Stool occult blood
d. Gastric acid analysis
ANS: B
Jaundice is caused by the elevation of bilirubin level associated with red blood cell hemolysis. Other tests would not be helpful in monitoring hemolytic anemia.
A patient who has been receiving IV heparin infusion and oral warfarin (Coumadin) for a deep vein thrombosis (DVT) is diagnosed with heparin-induced thrombocytopenia (HIT) when the platelet level drops to 110,000/L. Which action will the nurse anticipate including
in the plan of care?
a. Preparing for platelet transfusion
b. Discontinuing the heparin infusion
c. Administering prescribed warfarin (Coumadin)
d. Giving low-molecular-weight heparin (LMWH)
ANS: B
All heparin is discontinued when HIT is diagnosed. The patient should be instructed to never receive heparin or LMWH. Warfarin is usually not given until the platelet count has returned to 150,000/L. The platelet count does not drop low enough in HIT for a platelet transfusion,
and platelet transfusions increase the risk for thrombosis
Which action would the nurse implement when caring for a patient who has an acute exacerbation of polycythemia vera?
a. Place the patient on bed rest.
b. Administer iron supplements.
c. Avoid use of aspirin products.
d. Monitor fluid intake and output.
ANS: D
Monitoring hydration status is important during an acute exacerbation of polycythemia vera because the patient is at risk for fluid overload or underhydration. Hydration therapy can
reduce the blood's viscosity. Aspirin therapy is used to decrease risk for thrombosis. The patient should be encouraged to ambulate to prevent deep vein thrombosis. Iron is contraindicated in patients with polycythemia vera.
Which intervention will the nurse include in the plan of care for a patient with immune thrombocytopenic purpura?
a. Assign the patient to a private room.
b. Avoid intramuscular (IM) injections.
c. Use rinses rather than a soft toothbrush for oral care.
d. Restrict activity to passive and active range of motion.
ANS: B
IM or subcutaneous injections should be avoided because of the risk for bleeding. A soft toothbrush can be used for oral care. There is no need to restrict activity or place the patient in a private room
The nurse is caring for a patient who has type A hemophilia and is being admitted to the hospital with severe pain and swelling in the right knee. Which action would the nurse take?
a. Apply heat to the knee.
b. Immobilize the knee joint.
c. Assist the patient with light weight bearing.
d. Perform passive range of motion to the knee.
ANS: B
The initial action should be total rest of the knee to minimize bleeding. Ice packs are used to decrease bleeding. Range of motion (ROM) and weight-bearing exercise are contraindicated initially, but after the bleeding stops, ROM and physical therapy are started.
A young adult who is receiving desmopressin acetate (DDAVP) to treat von Willebrand disease is admitted to the hospital for minor surgery. Which laboratory value would the nurse
monitor?
a. Platelet count
b. Bleeding time
c. Thrombin time
d. Prothrombin time
ANS: B
The bleeding time is affected by von Willebrand disease. Platelet count, prothrombin time, and thrombin time are normal in von Willebrand disease. Beneficial effects of DDAVP (e.g.,
decreased bleeding time) are seen within 30 minutes when given IV and can last for more than 12 hours. Because the drug's effect is short lived, the patient must be closely monitored. They may need repeated doses.
A routine complete blood count for an active older man indicates possible myelodysplastic syndrome. Which procedure would the nurse plan to explain to the patient?
a. Blood transfusion
b. Bone marrow biopsy
c. Filgrastim administration
d. Erythropoietin administration
ANS: B
Bone marrow biopsy is needed to make the diagnosis and determine the specific type of myelodysplastic syndrome. The other treatments may be necessary later if there is progression of the myelodysplastic syndrome, but the initial action for this asymptomatic patient will be a bone marrow biopsy
Which action would the admitting nurse include in the plan of care for a patient who hasneutropenia?
a. Avoid intramuscular injections.
b. Check temperature every 4 hours.
c. Place a ―No Visitors‖ sign on the door.
d. Omit fruits and vegetables from the diet.
ANS: B
The earliest sign of infection in a neutropenic patient is an elevation in temperature. While unpeeled fresh fruits and vegetables should be avoided, fruits and vegetables that are peeled or cooked are acceptable. Injections may be required for administration of medications such as
filgrastim (Neupogen). The number of visitors may be limited and visitors with communicable diseases should be avoided, but a ―no visitors‖ policy is not needed
Which laboratory test will the nurse use to determine whether a prescribed myeloid growth factor is effective for a patient with acute lymphocytic leukemia who is receiving chemotherapy?
a. Platelet count
b. Reticulocyte count
c. Total lymphocyte count
d. Absolute neutrophil count
ANS: D
Myeloid growth factors increase the neutrophil count in neutropenic patients. The absolute neutrophil count is used to evaluate the effects of myeloid growth factors.
A patient who has a history of a transfusion-related acute lung injury (TRALI) is to receive a transfusion of packed red blood cells (PRBCs). Which action by the nurse will decrease the
risk for TRALI for this patient?
a. Infuse PRBCs slowly over 4 hours.
b. Transfuse leukocyte-reduced PRBCs.
c. Administer the prescribed diuretic before the transfusion.
d. Give the PRN dose of antihistamine before the transfusion.
ANS: B
TRALI is caused by a reaction between the donor and the patient leukocytes that causes pulmonary inflammation and capillary leaking. The other actions may help prevent respiratory problems caused by circulatory overload or by allergic reactions, but they will not prevent TRAL.
A patient who has acute myelogenous leukemia (AML) is considering treatment with a hematopoietic stem cell transplant (HSCT). Which approach would the nurse take?
a. Discuss the need for insurance to cover post-HSCT care.
b. Inquire whether there are questions or concerns about HSCT.
c. Emphasize the positive outcomes of a bone marrow transplant.
d. Explain that a cure is not possible with any treatment except HSCT.
ANS: B
Offering the patient an opportunity to ask questions or discuss concerns about HSCT willencourage the patient to voice concerns about this treatment and will allow the nurse to assess whether the patient needs more information about the procedure. Treatment of AML using
chemotherapy is another option for the patient. It is not appropriate for the nurse to ask the patient to consider insurance needs in making this decision.
Which action would the nurse include in the plan of care for a patient admitted with multiple myeloma?
a. Monitor fluid intake and output.
b. Administer calcium supplements.
c. Assess lymph nodes for enlargement.
d. Limit weight bearing and ambulation.
ANS: A
A high fluid intake and urine output helps prevent the complications of kidney stones caused by hypercalcemia and renal failure caused by deposition of Bence-Jones protein in the renal tubules. Weight bearing and ambulation are encouraged to help bone retain calcium. Lymph
nodes are not enlarged with multiple myeloma. Calcium supplements will further increase the patient's calcium level and are not used.
Which intervention would the nurse plan for a patient with non-Hodgkin's lymphoma whose platelet count drops to 18,000/L during chemotherapy?
a. Test all stools for occult blood.
b. Encourage fluids to 3000 mL/day.
c. Provide oral hygiene every 2 hours.
d. Check the temperature every 4 hours.
ANS: A
Because the patient is at risk for spontaneous bleeding, the nurse should check stools for occult blood. A low platelet count does not require an increased fluid intake. Oral hygiene is
important, but it is not necessary to provide oral care every 2 hours. The low platelet count does not increase risk for infection, so frequent temperature monitoring is not indicated.
A patient receiving outpatient chemotherapy for myelogenous leukemia develops an absolute neutrophil count of 850/L. Which collaborative action would the nurse anticipate?
a. Discuss the need for hospital admission to treat the neutropenia.
b. Teach the patient to administer myeloid growth factor injections.
c. Plan to discontinue the chemotherapy until the neutropenia resolves.
d. Order a high-efficiency particulate air (HEPA) filter for the patient's home.
ANS: B
The patient may be taught to self-administer myeloid growth factor injections. Although chemotherapy may be stopped with severe neutropenia (neutrophil count <500/L), administration of myeloid growth factor usually allows the chemotherapy to continue. Patients
with neutropenia are at higher risk for infection when exposed to other patients in the hospital. HEPA filters are expensive and are used in the hospital, where the number of pathogens is much higher than in the patient's home environment.
Which assessment finding would the nurse caring for a patient with thrombocytopeniacommunicate immediately to the health care provider?
a. Bruises on the patient's back.
b. Difficulty awakening the patient.
c. Purpura on the patient's oral mucosa.
d. The patient's platelet count is 52,000/L.
ANS: B
Difficulty in awakening the patient may indicate a cerebral hemorrhage, which is life threatening and requires immediate action. The other information would be documented and reported but would not be unusual in a patient with thrombocytopenia.
The nurse is planning to administer a transfusion of packed red blood cells (PRBCs) to a patient. Which action can the nurse delegate to assistive personnel (AP)?
a. Verify the patient identification (ID) according to hospital policy.
b. Obtain the patient's temperature and blood pressure before the transfusion.
c. Double-check the product numbers on the PRBCs with the patient ID band.
d. Monitor the patient for shortness of breath or chest pain during the transfusion.
ANS: B
AP education includes measurement of vital signs. AP would report the vital signs to the registered nurse (RN). The other actions require more education and a larger scope of practice and would be done by licensed nursing staff members.
A postoperative patient receiving a transfusion of packed red blood cells develops chills, fever, headache, and anxiety 35 minutes after the transfusion is started. After stopping the transfusion, which action would the nurse expect to take?
a. Send a urine specimen to the laboratory.
b. Administer PRN acetaminophen (Tylenol).
c. Draw blood for a new type and crossmatch.
d. Give the prescribed PRN diphenhydramine.
ANS: B
The patient's clinical manifestations are consistent with a febrile, nonhemolytic transfusion reaction. The transfusion would be stopped, and antipyretics administered for the fever as ordered. A urine specimen is needed if an acute hemolytic reaction is suspected. Diphenhydramine is used for allergic reactions. This type of reaction does not indicate incorrect crossmatching.
A patient in the emergency department reports back pain and difficulty breathing 15 minutes after a transfusion of packed red blood cells is started. Which action would the nurse take first?
a. Administer oxygen therapy at a high flowrate.
b. Obtain a urine specimen to send to the laboratory.
c. Notify the health care provider about the symptoms.
d. Disconnect the transfusion and infuse normal saline.
ANS: D
The patient's symptoms indicate a possible acute hemolytic reaction caused by the
transfusion. The first action would be to disconnect the transfusion and infuse normal saline. The other actions also are needed but are not the highest priority.
Which patient would the nurse assign as the roommate for a patient who has aplastic anemia?
a. A patient with chronic heart failure
b. A patient who has viral pneumonia
c. A patient who has right leg cellulitis
d. A patient with multiple abdominal drains
ANS: A
Patients with aplastic anemia are at risk for infection because of the low white blood cell production associated with this type of anemia, so the nurse would avoid assigning a roommate with any possible infectious process.
Which patient requires the most rapid assessment and care by the emergency department nurse?
a. The patient with hemochromatosis who reports abdominal pain
b. The patient with neutropenia who has a temperature of 101.8F
c. The patient with thrombocytopenia who has oozing gums after a tooth extraction
d. The patient with sickle cell anemia who has had nausea and diarrhea for 24 hours
ANS: B
A neutropenic patient with a fever is assumed to have an infection and is at risk for rapidly developing sepsis. Rapid assessment, cultures, and initiation of antibiotic therapy are needed. The other patients also require rapid assessment and care but not as urgently as the neutropenic patient.
A patient with immune thrombocytopenic purpura (ITP) has an order for a platelet
transfusion. Which information indicates that the nurse would consult with the health care provider before obtaining and administering platelets?
a. Platelet count is 42,000/L.
b. Blood pressure is 94/56 mm Hg.
c. Petechiae are present on the chest.
d. Blood is oozing from the venipuncture site.
ANS: A
Platelet transfusions are not usually indicated until the platelet count is below 10,000 to 20,000/L unless the patient is actively bleeding. Therefore, the nurse would clarify the order with the health care provider before giving the transfusion. The other data all indicate that
bleeding caused by ITP may be occurring and that the platelet transfusion is appropriate.
Which problem reported by a patient with hemophilia is most important for the nurse to communicate to the health care provider?
a. Leg bruises
b. Tarry stools
c. Skin abrasions
d. Bleeding gums
ANS: B
Melena is a sign of gastrointestinal bleeding and requires collaborative actions such as checking hemoglobin and hematocrit and administration of coagulation factors. The other problems indicate a need for patient teaching about how to avoid injury but are not indicators of possible serious blood loss.
A patient with septicemia develops blood in the stools and prolonged bleeding from
venipuncture sites. Which action is most important for the nurse to take?
a. Avoid other venipunctures.
b. Apply dressings to the sites.
C.Notify the health care provider.
d. Give prescribed proton-pump inhibitors.
ANS: C
The patient's new onset of bleeding and diagnosis of sepsis suggest that disseminated intravascular coagulation (DIC) may have developed, which will require collaborative actions such as diagnostic testing, blood product administration, and heparin administration. The other actions are also appropriate, but the most important action would be to notify the health care provider so that DIC treatment can be initiated rapidly.
A patient with possible disseminated intravascular coagulation arrives in the emergency department with a blood pressure of 82/40, temperature of 102F (38.9C), and severe back pain. Which prescribed action will the nurse implement first?
a. Administer morphine sulfate 4 mg IV.
b. Give acetaminophen (Tylenol) 650 mg.
c. Infuse normal saline 500 mL over 30 minutes.
d. Schedule complete blood count and coagulation studies.
ANS: C
The patient's blood pressure indicates hypovolemia caused by blood loss and would be addressed immediately to improve perfusion to vital organs. The other actions are also appropriate and would be rapidly implemented, but improving perfusion is the priority for this
patient.
Which action for a patient with neutropenia is appropriate for the registered nurse (RN) to delegate to a licensed practical/vocational nurse (LPN/VN)?
a. Administering injections of myeloid growth factor
b. Assessing the patient for signs and symptoms of infection
c. Teaching the patient the purpose of neutropenic precautions
c. Developing a discharge teaching plan for the patient and family
ANS: A
Administration of subcutaneous medications such as myeloid growth factor is included in LPN/VN education and scope of practice. Patient teaching, assessment, and developing the plan of care require RN level education and scope of practice.
Several patients call the outpatient clinic and ask to make an appointment as soon as possible. Which patient would the nurse schedule to be seen first?
a. A 44-yr-old with sickle cell anemia who says his eyes always look yellow
b. A 23-yr-old with no previous health problems who has a nontender axillary lump
c. A 50-yr-old with early-stage chronic lymphocytic leukemia who reports chronic
fatigue
d. A 19-yr-old with hemophilia who wants to learn to self-administer factor VII
replacement
ANS: B
A young adult with a nontender axillary lump suggests possible lymphoma, which needs rapid diagnosis and treatment. The other patients have questions about treatment or symptoms that are consistent with their diagnosis but do not need to be seen urgently
After receiving change-of-shift report for several patients with neutropenia, which patient would the nurse assess first?
a. A 23-yr-old who reports severe fatigue
b. A 56-yr-old with frequent explosive diarrhea
c. A 33-yr-old with a fever of 100.8F (38.2C)
d. A 66-yr-old who has white pharyngeal lesions
ANS: C
Any fever in a neutropenic patient indicates infection and can quickly lead to sepsis and septic shock. Rapid assessment and (if prescribed) initiation of antibiotic therapy within 1 hour are needed. The other patients also need to be assessed but do not have symptoms of potentially
life-threatening problems.
Which action would the nurse include in the plan of care for a patient who has thalassemiamajor?
a. Administer chelation therapy as needed.
b. Teach the patient to use iron supplements.
c. Avoid the use of intramuscular injections.
d. Notify health care provider of hemoglobin 11 g/dL.
ANS: A
The frequent transfusions used to treat thalassemia major lead to iron toxicity in patients unless iron chelation therapy is consistently used. Iron supplementation is avoided in patients with thalassemia. There is no need to avoid intramuscular injections. The goal for patients with thalassemia major is to maintain a hemoglobin of 10 g/dL or greater.
Which information is most important for the nurse to monitor when evaluating the
effectiveness of deferoxamine (Desferal) for a patient with hemochromatosis?
a. Hematocrit
b. Liver function
c. Serum iron level
d. Mucous membrane color
ANS: C
Because iron chelating agents are used to lower serum iron levels, the most useful information will be the patient's iron level. The other parameters will also be monitored but are not the most important to monitor when determining the effectiveness of deferoxamine.
Which finding about a patient with polycythemia vera is most important for the nurse to report to the health care provider?
a. Hematocrit 55%
b. Presence of plethora
c. Calf swelling and pain
d. Platelet count 450,000/L
ANS: C
The calf swelling and pain suggest that the patient may have developed a deep vein
thrombosis, which will require diagnosis and treatment to avoid complications such as pulmonary embolus. The other findings will also be reported to the health care provider but are expected in a patient with this diagnosis.
Following successful treatment of Hodgkin's lymphoma for a 55-yr-old woman, which topic would the nurse include in patient teaching?
a. Potential impact of chemotherapy treatment on fertility
b. Application of soothing lotions to treat residual pruritus
c. Use of maintenance chemotherapy to maintain remission
d. Need for follow-up appointments to screen for malignancy
ANS: D
The chemotherapy used in treating Hodgkin's lymphoma results in a high incidence of secondary malignancies; follow-up screening is needed. Chemotherapy will not impact the
fertility of a 55-yr-old woman. Maintenance chemotherapy is not used for Hodgkin's lymphoma. Pruritus is a clinical manifestation of lymphoma but would not be a concern after treatment.
A patient who has non-Hodgkin's lymphoma is receiving combination treatment with rituximab (Rituxan) and chemotherapy. Which patient assessment finding requires the most rapid action by the nurse?
a. Anorexia
b. Vomiting
c. Oral ulcers
d. Lip swelling
ANS: D
Lip swelling in angioedema may indicate a hypersensitivity reaction to the rituximab. The nurse would stop the infusion and further assess for anaphylaxis. The other findings may occur with chemotherapy but are not immediately life threatening.
Which information about a patient admitted with multiple myeloma is most important for the nurse to report to the health care provider?
a. Patient reports back pain.
b. Serum calcium level is 15 mg/dL.
c. Patient reports no stool for 5 days.
d. Urine sample has Bence-Jones protein.
ANS: B
Hypercalcemia may lead to complications such as dysrhythmias or seizures and would be addressed quickly. The other patient findings will also be discussed with the health care provider but are not life threatening.
When a patient with splenomegaly is scheduled for splenectomy, which action will the nurse include in the preoperative plan of care?
a. Recommend ibuprofen for left upper quadrant pain.
b. Schedule immunization with the pneumococcal vaccine.
c. Avoid the use of acetaminophen (Tylenol) for 2 weeks prior to surgery.
d. Discourage deep breathing and coughing to reduce risk for splenic rupture.
ANS: B
Asplenic patients are at high risk for infection with pneumococcal infections and immunization reduces this risk. There is no need to avoid acetaminophen use before surgery, but nonsteroidal antiinflammatory drugs (NSAIDs) may increase bleeding risk and would be avoided. The enlarged spleen may decrease respiratory depth, and the patient would be encouraged to take deep breaths.
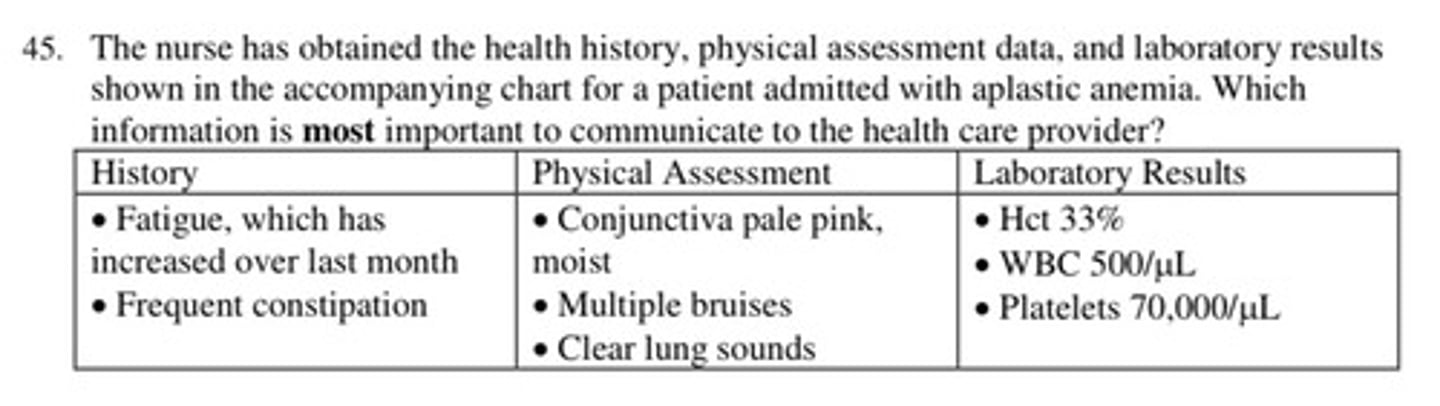
The nurse has obtained the health history, physical assessment data, and laboratory results shown in the accompanying chart for a patient admitted with aplastic anemia. Which information is most important to communicate to the health care provider?
a. Bruising
b. Neutropenia
c. Increasing fatigue
d. Thrombocytopenia
ANS: B
The low white blood cell count indicates that the patient is at high risk for infection and needs immediate actions to diagnose and treat the cause of the leukopenia. The other information may require further assessment or treatment but does not place the patient at immediate risk
for complications.
A patient is being discharged after an emergency splenectomy following a motor vehicle crash. Which instructions would the nurse include in the discharge teaching?
a. Check often for swollen lymph nodes.
b. Watch for excess bleeding or bruising.
c. Take iron supplements to prevent anemia.
d. Wash hands and avoid persons who are ill.
ANS: D
Splenectomy increases the risk for infection, especially with gram-positive bacteria. The risks for lymphedema, bleeding, and anemia are not increased after a person has a splenectomy.
COMPLETION
1. A patient is to receive an infusion of 250 mL of platelets over 2 hours through tubing that is labeled: 1 mL equals 10 drops. How many drops per minute will the nurse infuse?
___________
ANS:
21
To infuse 250 mL over 2 hours, the calculated drip rate is 20.8 drops/min or 21 drops/min.