KNES 372 - Midterm Review
1/150
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
151 Terms
What are the 4 anatomical planes?
median → plane that runs through the midline of the body, splitting into left + right portions
sagittal → plane splitting the body into left + right portions
frontal → plane dividing the body into anterior and posterior portions
transverse → plane dividing the body into superior + inferior portions
What is valgus? What is varus?
valgus → lateral angling of the distal part of a bone or joint (knock knees)
varus → medial angling of the distal part of a bone or joint (bow legs)
What is hyper lordosis? What is kyphosis?
hyper lordosis → excessive curvature of the lower back
kyphosis → dorsally excessive curvature of the thoracic, lumbar or cervical spine
What is the difference between rotation + circumduction?
rotation → bone or limb turning around its own axis
circumduction → movement of a body part in a circular pattern by combining flexion, extension, adduction + abduction
Inversion and eversion vs. supination and pronation?
inversion → tilting the sole of the foot inward (toward midline)
eversion → tilting the sole of the foot outward (away from midline)
supination → combination of inversion, adduction, plantarflexion
pronation → combination of eversion, abduction, dorsiflexion
What is SEM team? What is another name for it? What is the purpose of it?
sport and exercise medicine team aka integrated support team (IST)
multi-disciplinary team of sport science, sport medicine + sport performance professionals
goal is to ensure athletes are healthy, fit + mentally ready for optimal performance
What are some examples of the members of an SEM team?
physician
therapist (physio, chiro, athletic)
strength + conditioning coach
exercise physiologist
sport psychologist
biomechanist
nutritionist
What are the roles of each of the members of an SEM team?
physician → diagnose, prescribe, X-rays, MRI’s, big picture (1st assessment)
therapist (physio, chiro) → taping, rehab exercises, manual therapy
strength + conditioning coach → skills + fitness, injury prevention
exercise physiologist → testing, limit determination
sport psychologist → mental readiness (after injury, before competitions)
biomechanist → ergonomics, equipment
nutritionist → food to optimize health + performance, education
SEM specialists must follow the __________ and standard of care.
scope of practice
What is scope of practice?
the procedures + actions that a qualified practitioner is allowed to do
What is standard of care?
medical treatment guideline
It specifies appropriate treatment based on scientific evidence + collaboration between medical and/or psychological professionals involved in the treatment of a given condition
What are the different levels of identifying risks in sport?
within/across sport
club/team level
individual level
What is the process of identifying risks in sport?
1) assessment → process of measurement/estimation of risks to teams + athletes
2) evaluation → involves determining the significance + acceptability of the risks
3) control → process of identifying + implementing methods to control the risks + consequences
What are the components of an effective risk management system for a team?
injury surveillance → recording/reporting injuries
season analysis → risks, travelling, timing
preseason screening → baseline testing, injury history, strengths/weaknesses
monitoring “at risk” team members → risk factors for future injuries
return to sport → facilitating safe return to sport
education → of all members
equipment + facilities → safe, up to date
emergency action plan (EAP)
When should an EAP (emergency action plan) be activated immediately?
if the person:
is not breathing
does not have a pulse
is bleeding profusely
has impaired consciousness
has injured the back, neck or head
has a visible major trauma
cannot move arms or legs (has lost feeling in them)
What is a SOAP note?
method of documentation → standardized way to store medical information
S: subjective
O: objective
A: assessment
P: plan
What direction of travel has the most jet lag? The least?
most: west → east
least: east → west
What is neuromuscular training? What are the components of NMT?
focuses on performing exercises that train the nerves + muscles to react + communicate, a specialized form of physical training that focuses on improving the coordination + function of the nervous + muscular systems, designed to enhance movement control, stability of movements, movement technique + skills, strength, power and speed
components: balance + proprioception, plyometrics, strength + stability, agility + coordination, acceleration + deceleration, reactive perturbation
What are the aims of NMT?
to improve neuromuscular control + stability
to improve movement skills + technique
to enhance performance
to reduce the risk of injury
What is the leading cause of injury in youth in Canada?
sport-related injury
What sports have the highest burden for sport-related injuries?
hockey, basketball, soccer
What type of sport accounts for 44% of all hospital treated sport injuries in the EU?
team ball sports
What is the leading risk for injury in sport?
previous injury
What is Van Mechelen’s 4 step sequence of injury prevention?
1) establish the extent/severity of the injury problem
2) find the mechanisms + risk factors
3) introduce a preventative measure
4) evaluate the effectiveness of the intervention
What is the injury mechanism composed of?
events leading to injury situation
injury situation
whole body biomechanics
joint biomechanics
What are intrinsic + extrinsic risk factors?
intrinsic → physical characteristics, psychological + psychosocial characteristics, etc. (internal)
extrinsic → exposure, environment, equipment (external)
What are modifiable risk factors?
balance, flexibility, strength, aerobic fitness, training load
What are non-modifiable risk factors?
age, sex, previous injury
What are the different levels of injury prevention?
primary prevention → reduce occurrence in those who don’t yet have an injury
secondary prevention → early diagnosis
tertiary prevention → minimize consequences (stop worsening of injury + minimize future issues)
What are some strategies used in sport injury prevention?
training programs to improve fitness/movement quality
new or modified sport equipment
new or modified rules
education
______________ and _______________ are key factors in injury occurrence.
Biomechanics, mechanical loads/forces
ACL rupture occurs ___________ after initial foot contact.
30-40 ms
What mechanism causes the most ACL injuries?
non-contact
bodyweight on one leg
small knee flexion angle
knee valgus + internal rotation
high impact force
What are the 3 types of modes of onset for sport injuries? What is an example of each?
1) acute, sudden onset injury (ankle sprain)
2) repetitive, gradual onset injury (overuse, pain increases over time)
3) repetitive, sudden onset injury (stress fracture overuse injury, pain is sudden but tissue damage has been happening for a while)
What are the classifications of contact as a mechanism for acute injuries?
1) direct contact injury (contact with injured area) with another athlete or object
2) indirect contact injury (no direct contact to injured area, contact doesn’t occur at exact time of injury)
3) noncontact injury (no other athlete or object involved)
What do soft-tissue injuries involve? Skeletal injuries? Acute (traumatic) injuries?
1) cartilage, ligaments, tendons, muscle
2) bone fractures
3) bleeding (hematoma)
What is the difference between articular cartilage and fibrocartilage?
articular → flexible, provides smooth surface for joint movement (end of bones)
fibrocartilage → tough, able to absorb loads (discs of the spine, meniscus)
What is a tendon, enthesis, and a ligament?
tendon → connects muscle to bone
enthesis → the junction between a tendon and a bone
ligament → connects bone to bone
What structures can a tear involve? A sprain? A strain? A fracture? A rupture?
tear → ligaments, muscle, tendon, cartilage
sprain → ligaments, joints
strain → tendons + muscles
fracture → bone
rupture → muscle, tendons, ligaments, internal organs
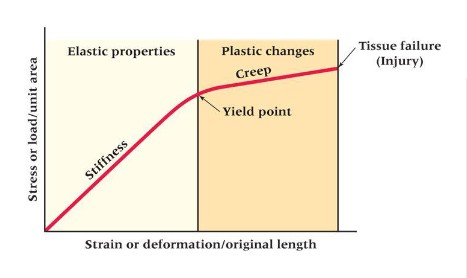
Describe the stress-strain curve. What is stiffness? What is the yield point? What is creep?
stiffness → ability of a tissue to resist a load
yield point → indicates the limit of elastic behaviour + the beginning of plastic behaviour
creep → deformation in the shape/properties of a tissue that occurs under the influence of persistent mechanical stress
What is hemostasis?
process to stop bleeding when injury occurs → results in formation of a clot
What are the steps of hemostasis?
vascular spasm
formation of a platelet plug
blood clotting (coagulation cascade)
formation of the final clot
platelets release growth factors
What is the purpose of inflammation?
defensive response of tissues to a physical or chemical injury, or bacterial infection
growth factors recruit inflammatory cells to destroy debris + bacteria
neutrophils → first 48 hours
macrophages → peak around 48-72 hours
lymphocytes → appear after 72 hours
indicated by redness, warmth, swelling, pain, and dysfunction
What is proliferation?
rebuild stage
What is angiogenesis?
component of proliferation: formation of new blood vessels, restoration of blood flow
What is fibroblast migration?
component of proliferation: fibroblasts produce collagen fibers + elastin, results in granulation tissue which replaces the clot
What is epithelialization?
component of proliferation: epithelial cells cover the exposed surface
What is wound retraction?
component of proliferation: contraction of the wound (healing + closing of the wound)
What is the purpose of remodelling?
to increase tissue strength
may last months/years
granulation tissue matures into scar
form + function of the scar tissue depend on loading during this stage
same level of tissue strength before the injury is never achieved!
Healing structures need to be exposed to ________________ to remodel because bone + tissue respond to _____________ + remodel accordingly.
progressive loads, loading
What time frame is each stage of wound healing occurring at?
1) hemostasis → minutes/hours
2) inflammation → days
3) proliferation → weeks
4) remodeling → months/years
What are the goals of early treatment of acute soft tissue injuries?
limit bleeding (too much bleeding slows healing)
limit swelling
relieve pain
improve conditions for subsequent treatment + healing
What are the new acronyms for acute injury management + what does each letter stand for?
PEACE and LOVE
P - protection (unload/restrict movement for 1-3 days)
E - elevation (higher than the heart)
A - avoid anti-inflammatories + ice
C - compression (helps limit edema + hematoma)
E - education (educate patients on benefits of active approach to recovery)
L - load (appropriate movement + exercise for healing stage)
O - optimism (associated with better outcomes)
V - vascularization (cardiovascular activity helps manage injuries)
E - exercise (to help restore mobility, strength + proprioception early after injury)
What does the acronym POLICE stand for?
protect, optimal loading, ice, compression, elevation
What injuries are X-rays used for?
fractures, dislocations (anything with bones)
What injuries are CT (computed tomography) used for?
cross-sectional areas, bone injuries that are complex (wrist, spine)
What injuries is U (ultra-sound) used for?
ligaments, tendons, other soft tissues
What injuries are MRI’s (magnetic resonance imaging) used for?
brain, detailed soft tissue images
What are the 3 stages of treatment + rehabilitation?
1) acute stage
2) rehabilitation stage
3) training stage
What is the difference in treatment during the acute stage for acute injuries and overuse injuries?
acute: PEACE/PRICE/POLICE
overuse: partial unloading of the injured structure, loading pattern must be altered
What occurs during the rehabilitation stage?
monitor pain + swelling
ensure normal ROM
ensure normal strength
ensure normal neuromuscular function
ensure normal aerobic capacity
______________ is a pre-requisite for returning the athlete to normal technique because reduced ____________ limits the ability to do strength + other training.
Normal ROM, ROM
What is alternative training? Why is it important during the rehabilitation stage?
maintaining general strength + endurance
well performed alternative training will allow the athlete to return to sport sooner
What is the specific training part of the rehabilitation stage?
training that affects the injured structures
amount, intensity, frequency, duration + exercises depend on the injury
highly repetitive training
weekly consultation with a physiotherapist
Why is neuromuscular training important in the rehabilitation stage?
painful conditions may result in reflex inhibitions → changes in movement patterns → unfavorable loading pattern → increased risk of reinjury
acute ligament injuries may also result in reduced joint position sense + coordination → increased risk of reinjury
proprioceptive training + progressive strength training will improve this
How much of an athlete’s original strength must be regained before being allowed to compete again?
85-90%
What occurs in the training stage?
gradual transition from controlled rehabilitation exercises to sport specific training
functional + sport specific testing to determine whether an athlete can tolerate sport specific training loads
What are the 3 elements of the return to sport continuum?
return to participation
return to sport
return to performance
What is the StARRT framework? What are the 3 steps of this framework?
strategic assessment of risk and risk tolerance
1) evaluation of health status
2) evaluation of participant risk
3) decision modification
What is the biopsychosocial model?
theoretical return to sport model that addresses the best interests of the athlete by looking at social/contextual, physical and psychological factors
What is the most common groin injury?
adductor related groin pain/injury
What is the structure of ligaments?
dense bands of collagen tissue (collagen, elastin, proteoglycan, other proteins)
vary in size, shape, orientation + location
What are the functions of ligaments?
connect one bone to another (passive stabilization of joints)
creep (stretching or deforming over time in response to sustained or repetitive stress)
proprioceptive function
What is the response of ligaments to injury?
ligament scars from healing have poor viscoelastic properties (reinjury risk = very high)
decreased proprioception
If force causes more than a ______ change of length, permanent elongation starts (microdamage begins)
4%
What are the 3 types of ligaments?
1) intra-articular ligaments (inside joint capsule, e.g. cruciate ligaments of the knee)
2) extra-articular ligaments (outside of joint, e.g. calcaneofibular ligament)
3) capsular ligaments (surrounds a joint + has great healing potential, e.g. glenohumeral ligament)
How do ligaments adapt to training?
adapt slowly to increased loading, but weaken very rapidly when immobilized
adapt to loading by increasing cross-sectional area
normal everyday activity is sufficient to maintain mechanical properties
systematic ligament training can increase ligament strength by 10-20%
Joint stability depends on the interaction between the ___________, ____________ and ____________ subsystems.
passive, active, neural
What are the passive, active + neural subsystems in joint stability?
passive → consists of non-contractile connective tissues
active → controlled by the neural sub-system to provide dynamic joint stability
Mechanisms of ligament injuries?
acute → sudden overload, ligament is rapidly stretched out
overuse → repetitive loading, ligament is gradually stretched out
What is hemarthrosis? What injuries usually cause hemarthrosis?
bleeding into the joint, ACL tear, peripheral meniscus tear, osteochondral injuries, fractures
The ACL has two bundles. What are they and what are their respective functions? Does the ACL have pain fibers?
anteromedial bundle → resists tibial anterior translation
posterolateral bundle → resists tibial rotation
no pain fibers, but has proprioceptive fibers
What is the ACL injury mechanism?
heel strike (lots of force), then valgus knee movement (knee caves in)
What tests can be used to assess the ACL?
anterior drawer test
Lachman test
What are some ACL complications?
osteochondral injury → articular cartilage + underlying bone are damaged in a joint
ACL injury, meniscus tear
unhappy triad (ACL, MCL, medial meniscus)
osteoarthritis
What are some modifiable risk factors for ACL injuries?
weak hip abductors + external rotators
increased knee abduction moments during cutting + landing
What is a labrum injury?
injury to the fibrocartilage rim of a joint
What are the 2 types of bone tissue?
1) trabecular (spongy) bone → high porosity, cuboidal bones, flat bones, ends of long bones
2) cortical (compact) bone → low porosity, forms outer shell of long bones
How do bones adapt to training?
physical training increases bone mass (bone mineral density) and is site specific
bone mass increases are driven by dynamic rather than static loading (fast, impactful)
only a short duration of loading is necessary
What is the difference in function between osteoclasts and osteoblasts?
osteoclasts → remove bone
osteoblasts → produce bone
What are the bone injury types? (7)
traumatic fracture → closed or open
pathological fracture → break due to weakness from osteoporosis or cancer)
stress fracture → fatigue fracture
bone contusion → acute traumatic bone injury without fracture
osteitis → inflammation of bone
periostitis → inflammation of periosteum
osteochondral injury → articular cartilage + underlying bone
What is the difference between woven bone + lamellar bone?
woven (soft callus stage):
quickly formed, poorly organized
first bone formed during the healing process
lamellar (hard callus + remodeling stages:
slowly formed, highly organized
replaces woven bone during the later stages of healing
What are some possible complications from fractures?
infection (open fractures)
delayed union, malunion, non-union
acute compartment syndrome (pressure inside muscle compartment)
osteonecrosis
nerve injury
vascular injury
osteoarthritis
deep vein thrombosis + pulmonary embolism
What are the common mechanisms for bone stress injuries?
high impulse forces
repetitive bone loading
high training volumes
What bones do bone stress injuries usually occur in?
highly loaded bones
tibia, tarsals, lumbar spine, humerus, ulna
What is the difference between spondylolysis and spondylolisthesis?
fracture and slipping of vertebra, respectively
What is the continuum for spine injuries? What are the risk factors?
1) bone stress reaction (posterior element overuse syndrome)
2) fracture (spondylolysis)
3) slipping of vertebra (spondylolisthesis)
one can lead to the next (progressively worse) if not treated early or properly
excessive extension + rotation loads
improper technique
hyperlordosis
What is medial tibial stress syndrome (MTSS)?
repetitive loading leads to periosteal inflammation along the tibia (diffuse pain)
What is a tibial stress fracture caused by?
running + jumping, focal pain
What is the myotendinous junction?
connection between tendon and muscle that is susceptible to injury