Hip & Pelvis Pathology
1/62
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
63 Terms
superior
During the development of the extremities, the limb buds develop with the thumb and great toe _________________.
adducts, medially, extends
During gestation, the LE _______________, _______________ rotates and _______________.
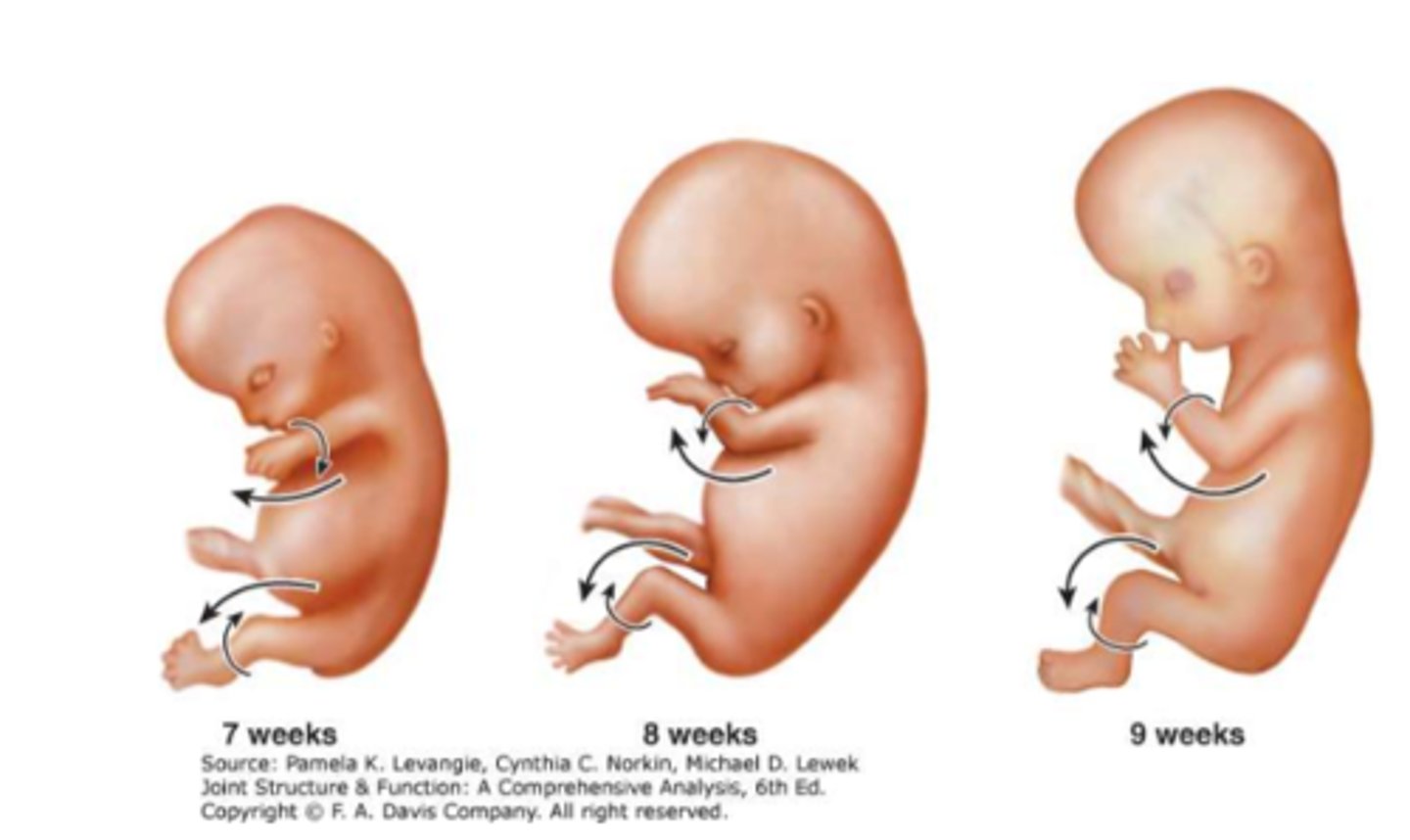
adducts
During gestation, the UE _______________.
development of extremities
CONSIDER:
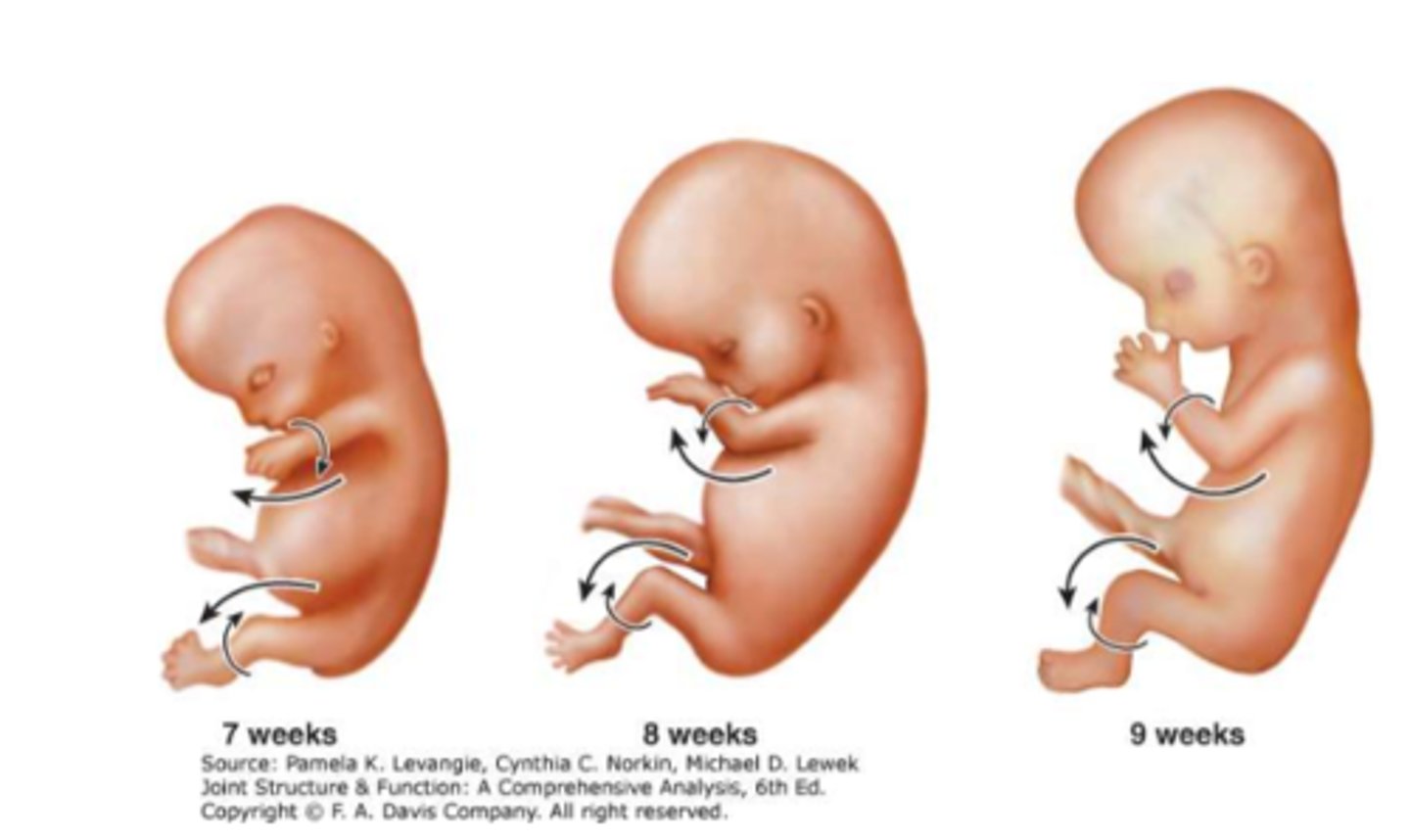
1. anatomical position and dermatomes
2. hip joint capsule spiral configuration
3. knee flexes posterior vs elbow anterior
4. toe extensors face anterior vs finger extensors posterior
medially, posteriorly, anteriorly, laterally
Originally anterior muscles turn to face ______________ and ______________, while originally posterior muscles turn to face ______________ and ______________.
movement of legs during embryological development
Why do the dermatomes on the legs appear slightly twisted?
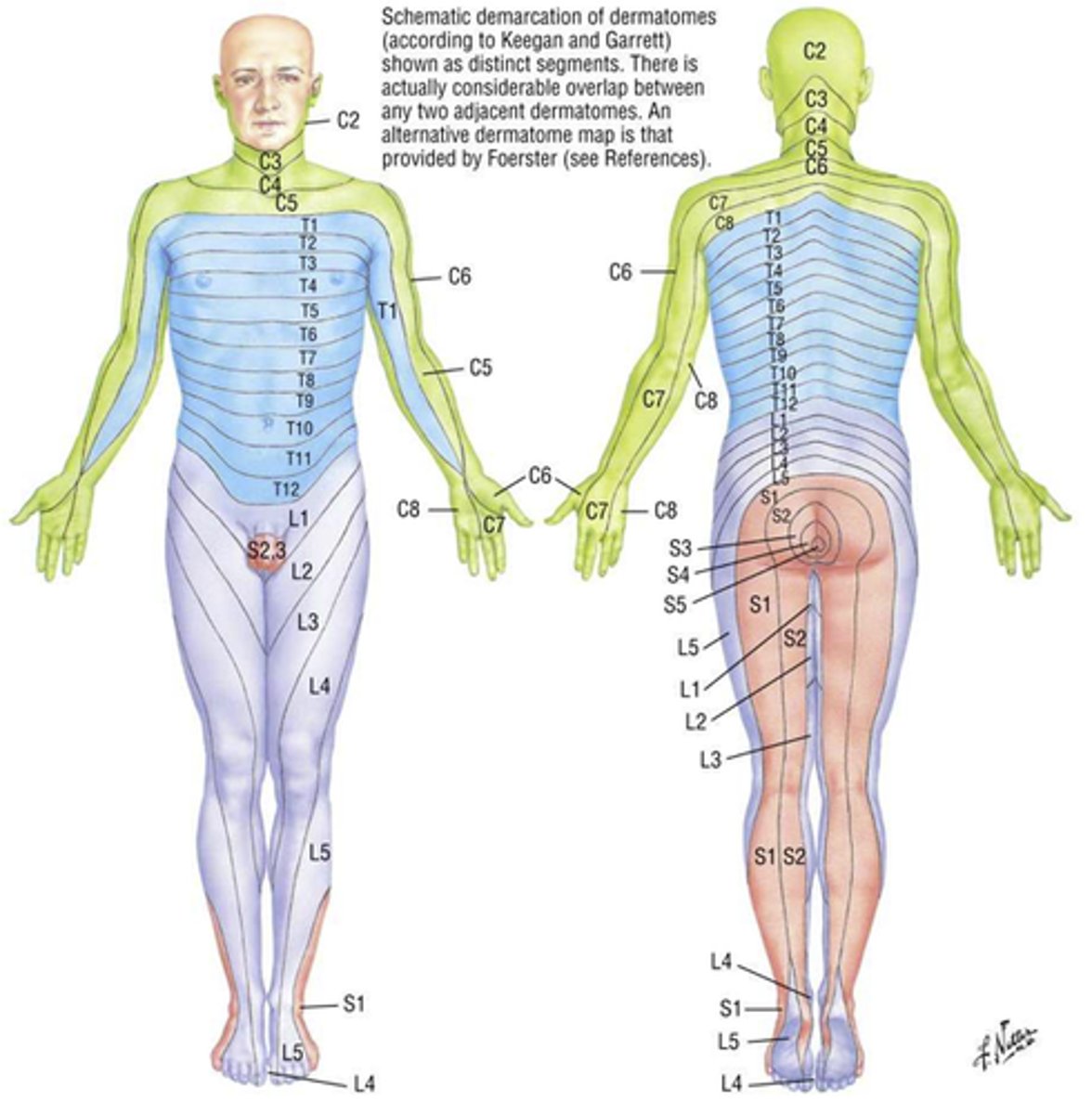
osteological dysfunctions
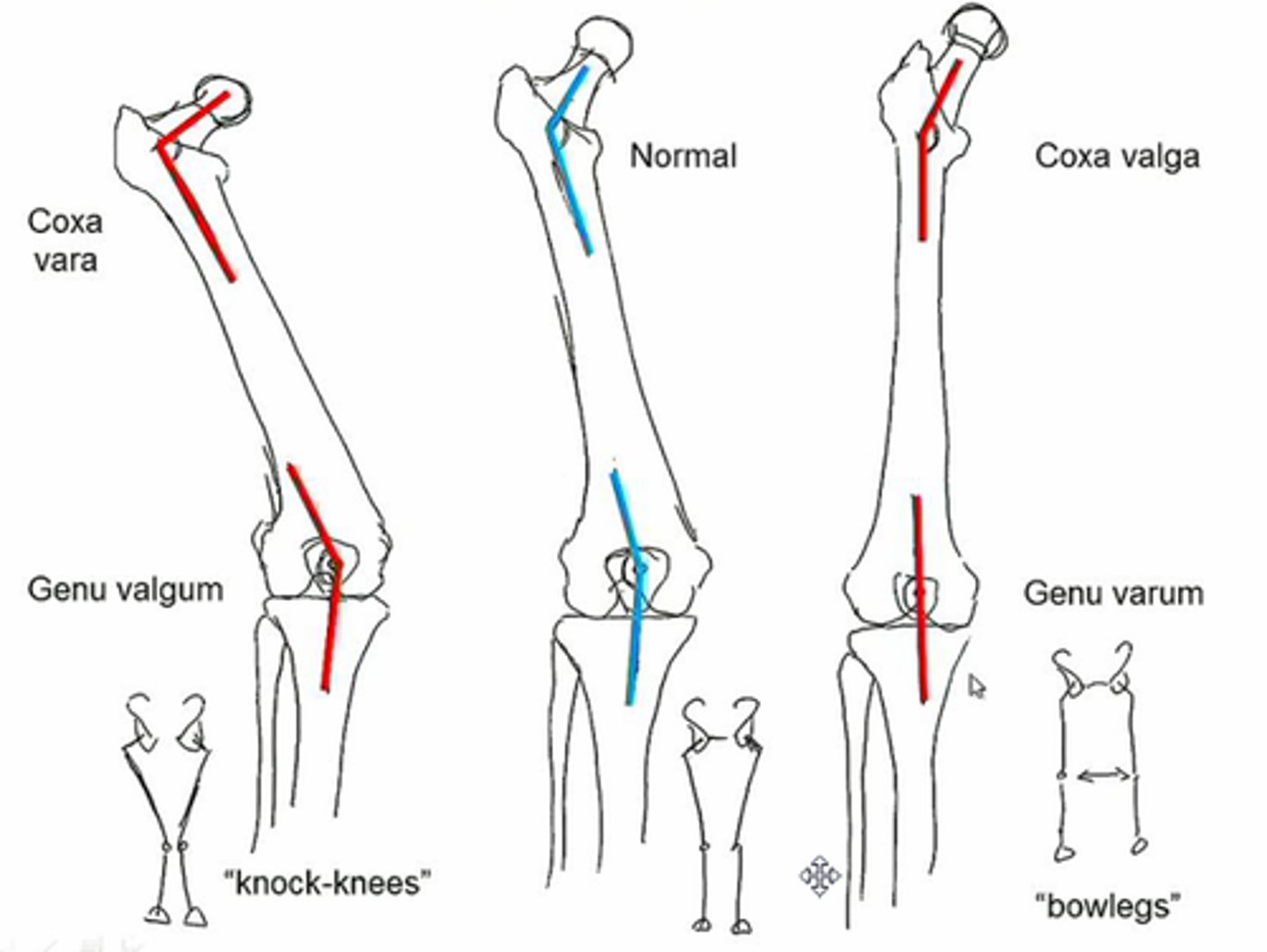
1. coxa valga
2. coxa vara
3. anteversion
4. retroversion
5. slipped capital femoral epiphysis
6. legg-calve-perthes disease
7. femoral acetabular impingement (FAI)
8. fractures/dislocations
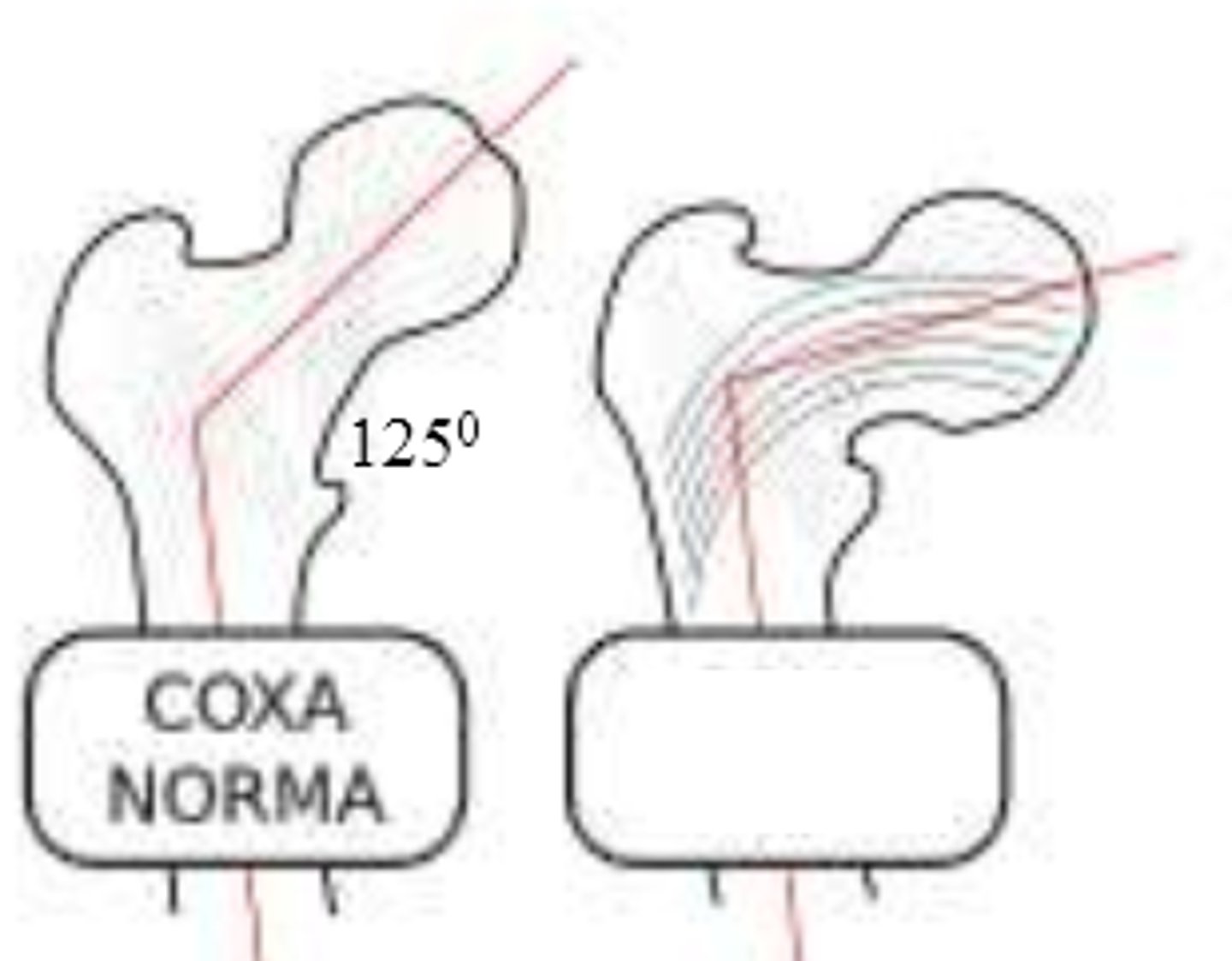
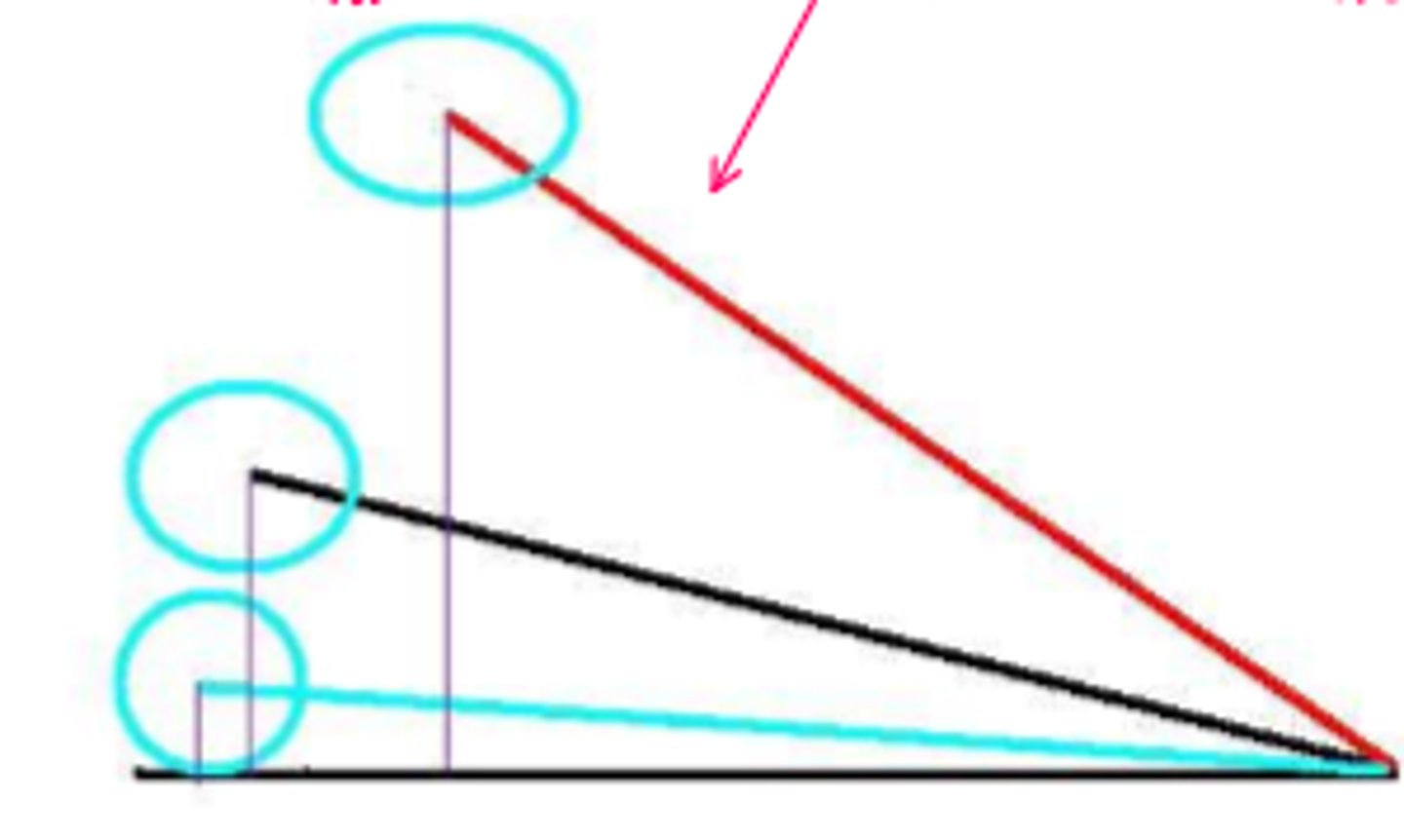
coxa valga
development of femur with angle of inclination GREATER than expected
*involves femoral head/neck and shaft
decrease shear force across femoral neck, increase functional length of abductor m
What are the 2 positive aspects of coxa valga?
decrease moment arm of hip abductor (muscle must work harder), less congruency (favors dislocation)
What are the 2 negative aspects of coxa valga?
coxa valga functional deficits
limb = LONGER
shear forces = LESS
moment arm of glut med = SHORTER
joint reaction forces = HIGHER
joint congruency = DECREASED
joint stability = LOWER
articular cartilage pressure = HIGHER

coxa valga compensatory changes
gluteus medius must work harder
*if not strong enough, then functional weakness with be displayed with a gluteus medius or trendelenburg gait
**overtime, joint reaction forces can predispose individual to DJD
coxa vara
development of femur with angle of inclination LESSER than expected
*involves femoral head/neck and shaft
coxa vara functional deficits
limb = SHORTER
shear forces = HIGHER
moment arm of glut med = LONGER
joint reaction forces = LESS
joint congruency = INCREASED
joint stability = GREATER
articular cartilage pressure = LOWER
*more overlap of femoral head and acetabulum

coxa vara compensatory changes
predisposed to fracture across femoral neck & increased incidence of slipped capital femoral epiphysis
varum, supinate
In an individual with a coxa valga hip, they may experience genu ____________ and therefore _____________ the foot.
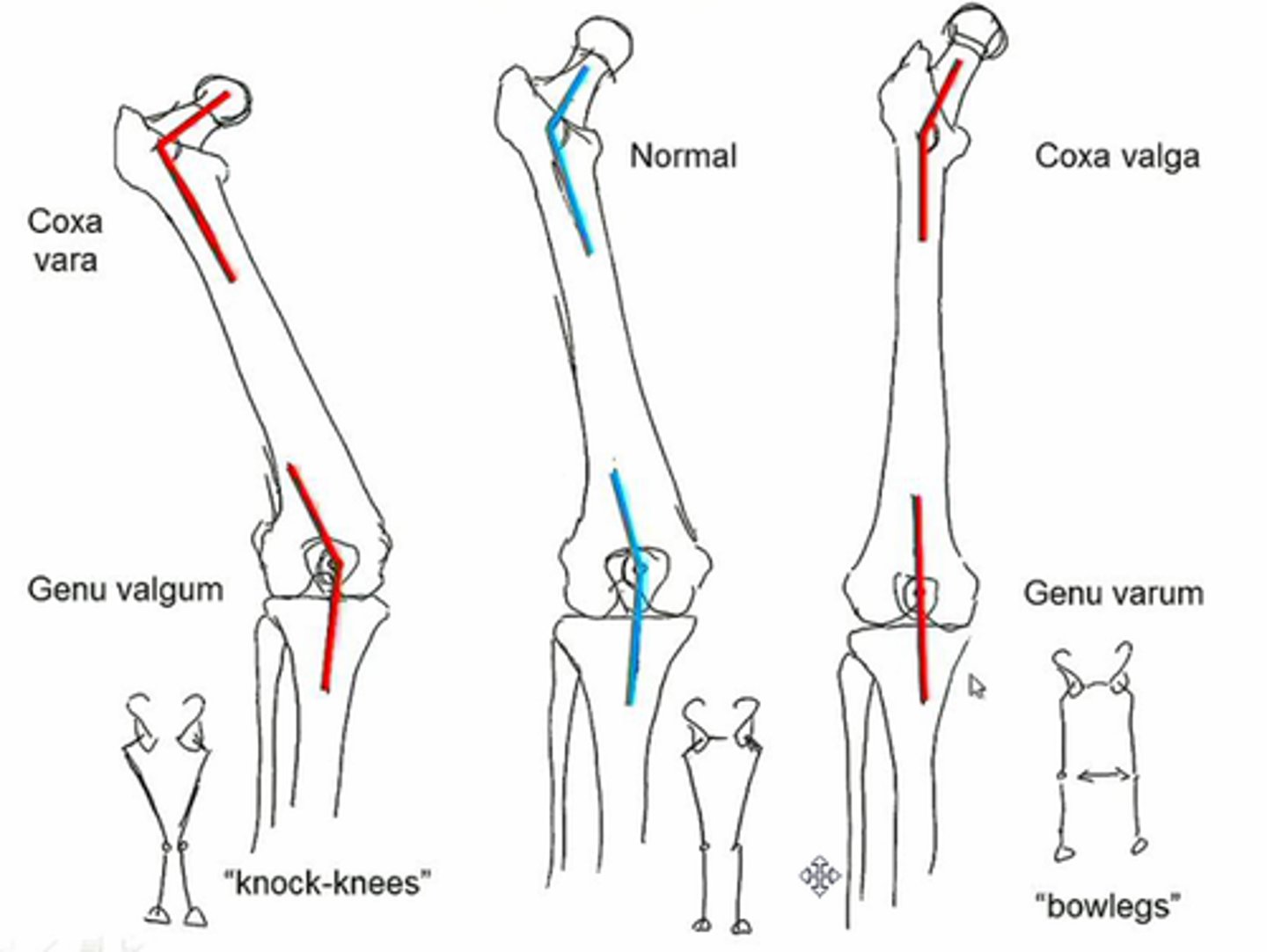
valgum, pronate
In an individual with a coxa vara hip, they may experience genu ____________ and therefore _____________ the foot.
anteversion
GREATER angle of torsion than expected for age
*involves femoral head/neck and shaft
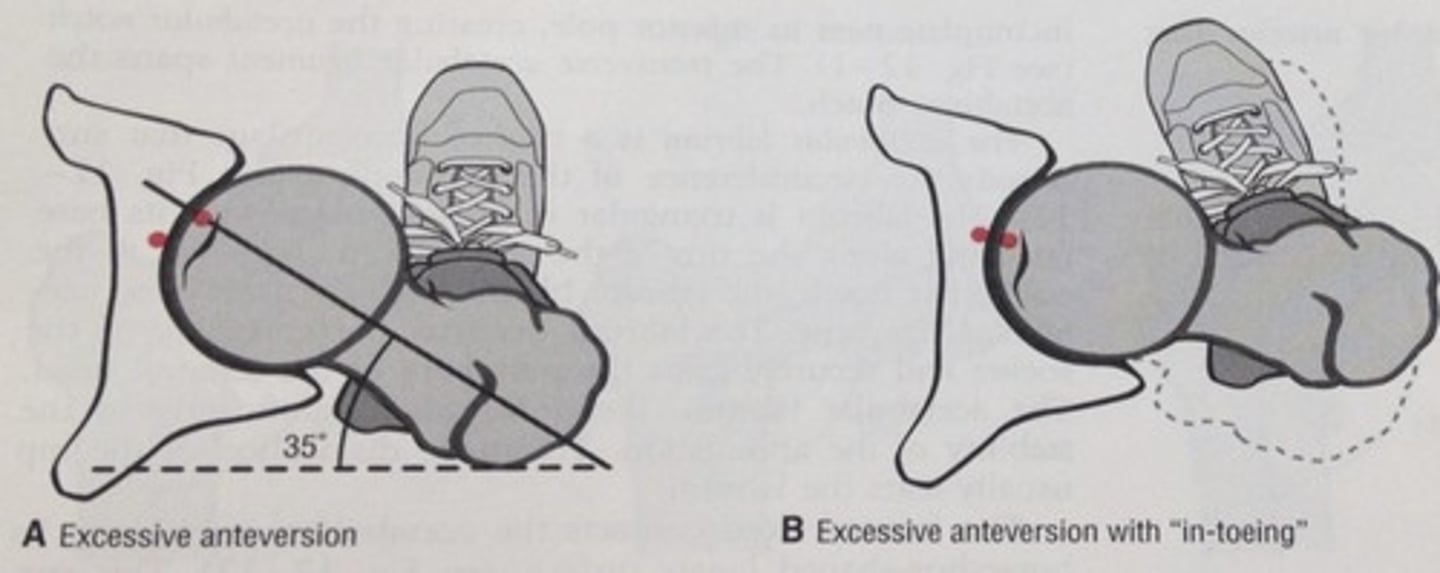
anteversion functional deficits
moment arm of glut med = DECREASED
joint reaction forces = INCREASED
joint congruency = DECREASED
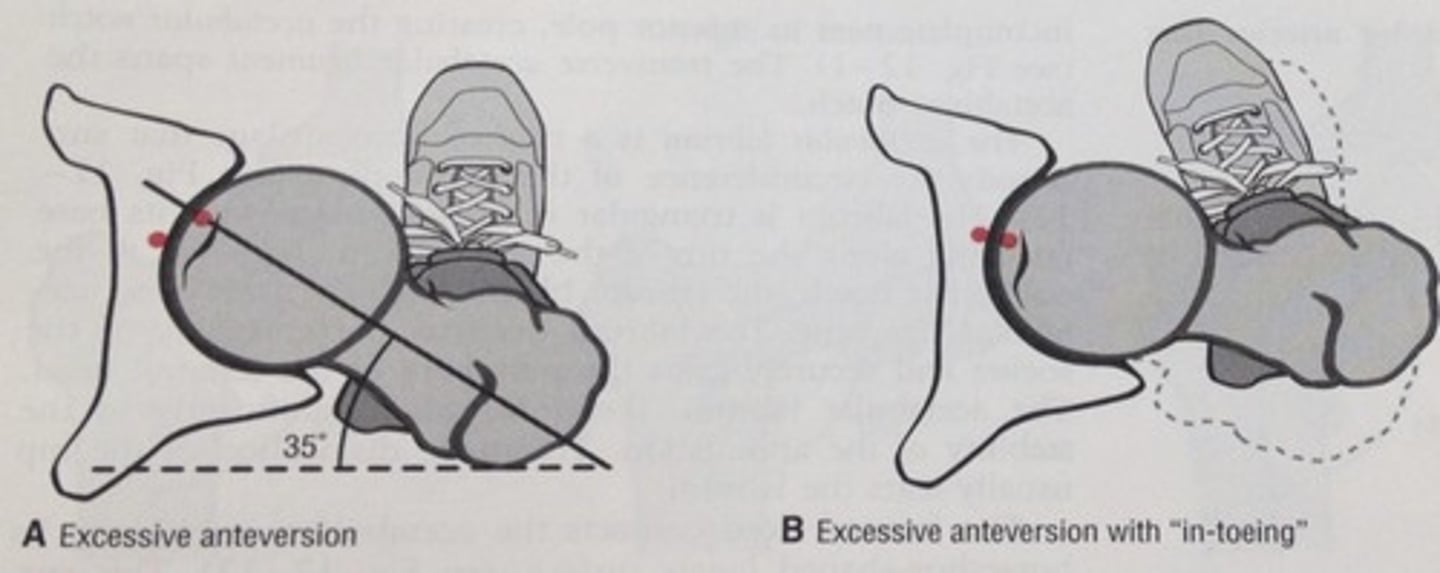
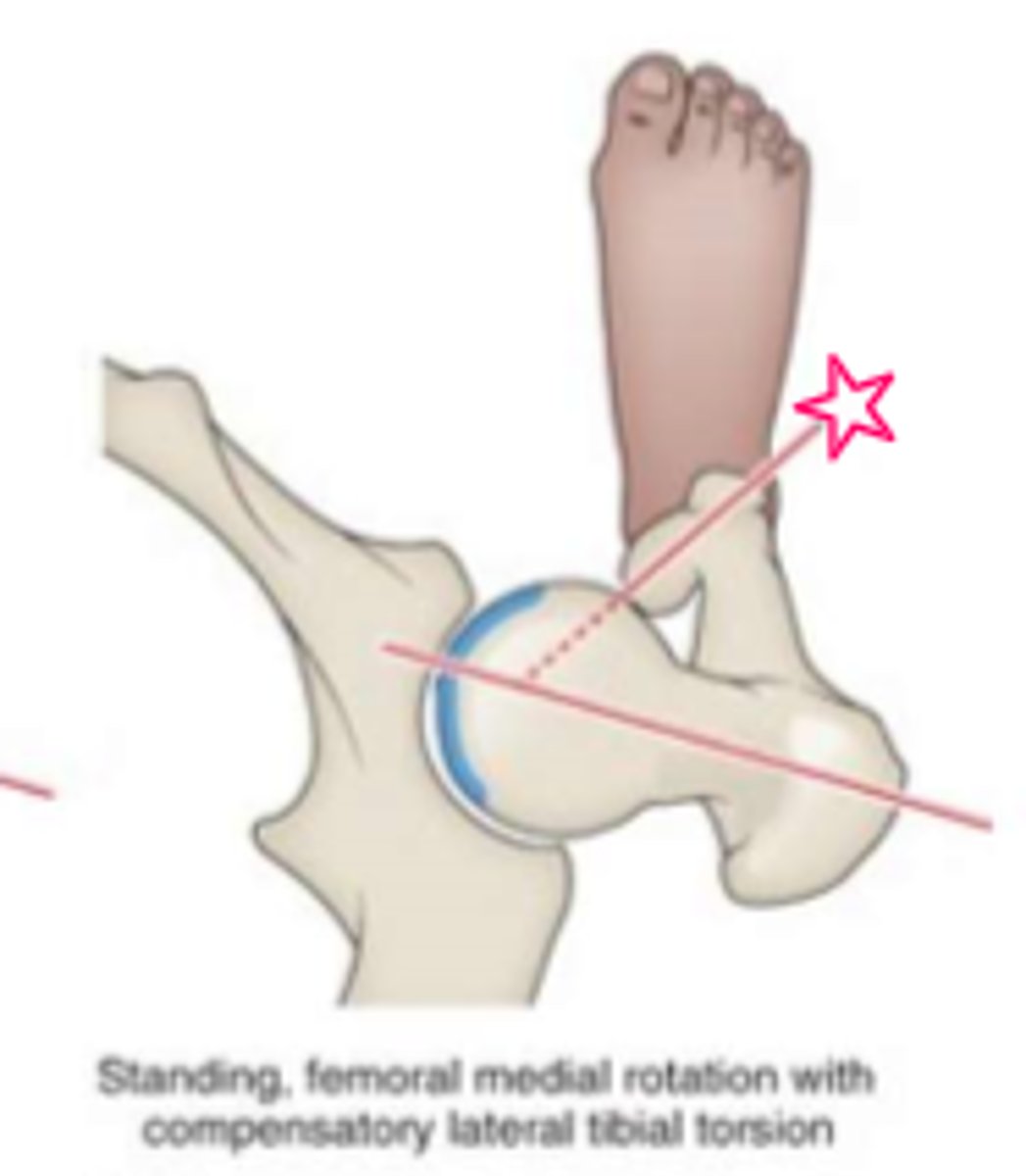
anteversion compensatory changes
toe-in to normalize joint congruency
*may result in compensatory lateral torsion of tibia and supination of the foot/ankle
**increased joint reaction forces may predispose individual to arthritis
lateral, supination
Toe-in compensatory change may result in ___________ torsion of tibia and _______________ of the foot/ankle.
shorter
An anteverted hip has a ______________ moment arm.
HINT: less mechanically advantageous
medial torsion
Anteversion of the hip resulting in a toe in gait to improve hip joint congruency, and then lateral tibial torsion to eliminate toe it - femoral condyles remain in ________________ ________________.
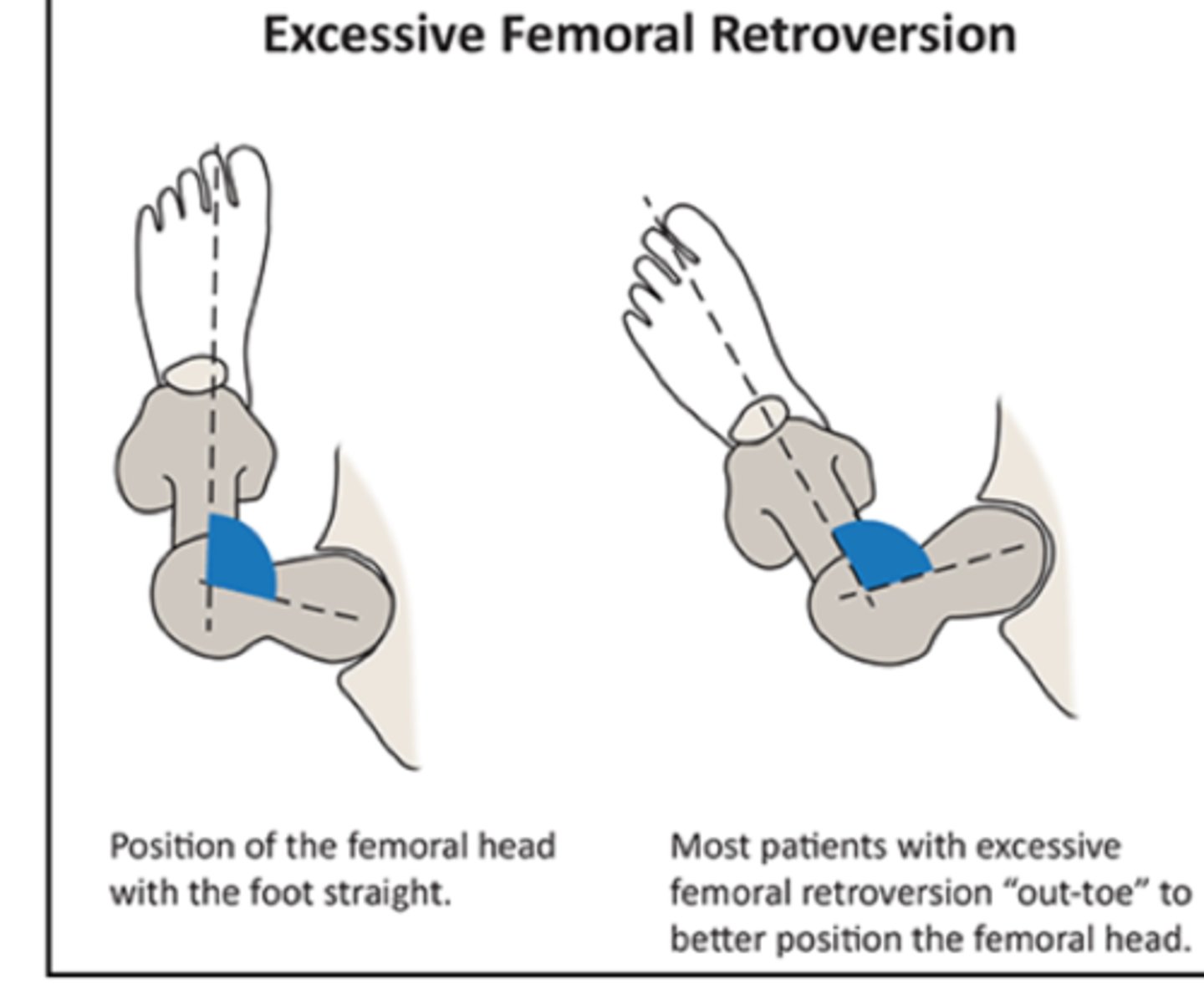
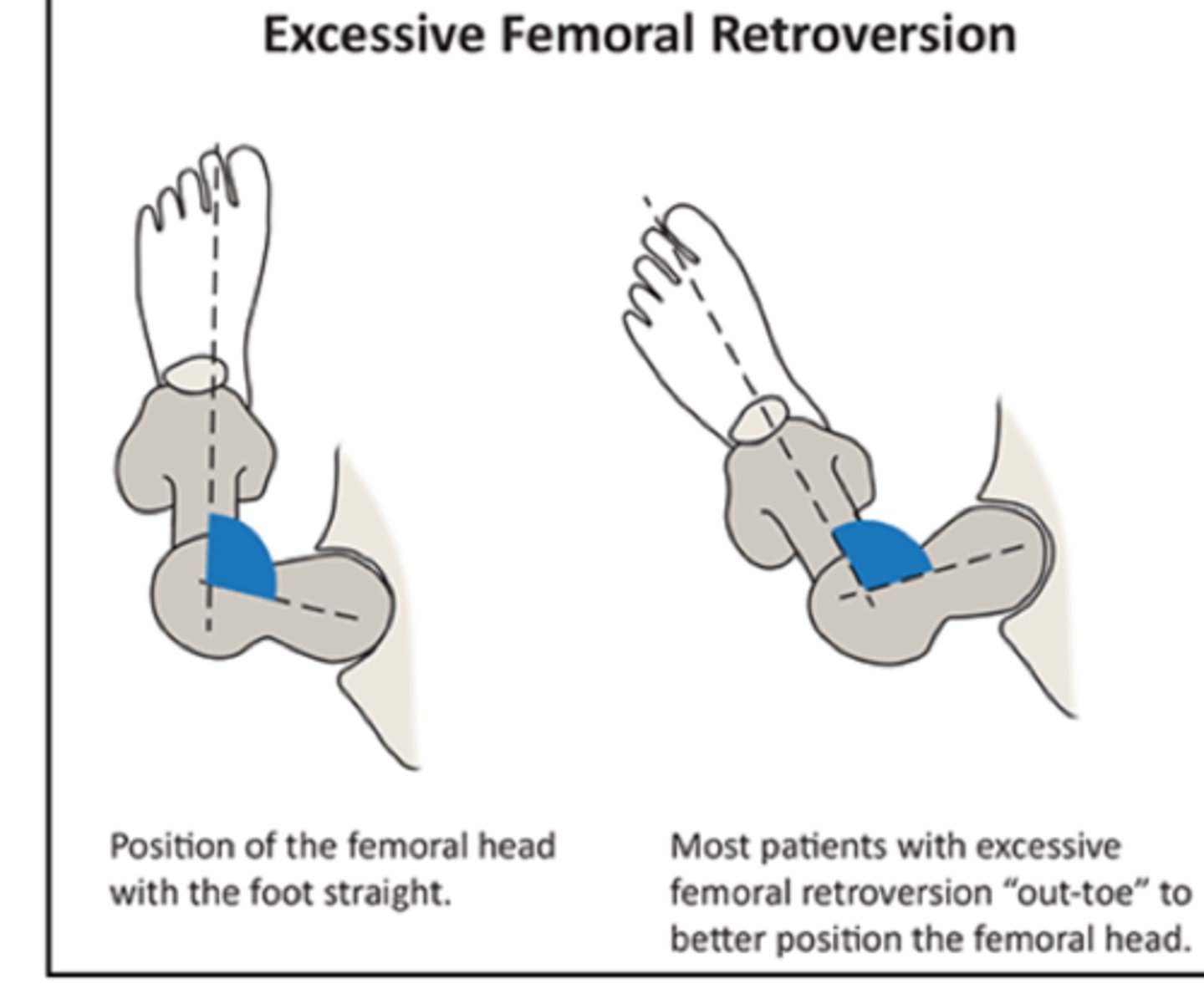
retroversion
LESSER angle of torsion than expected for age
*involves femoral head/neck and shaft
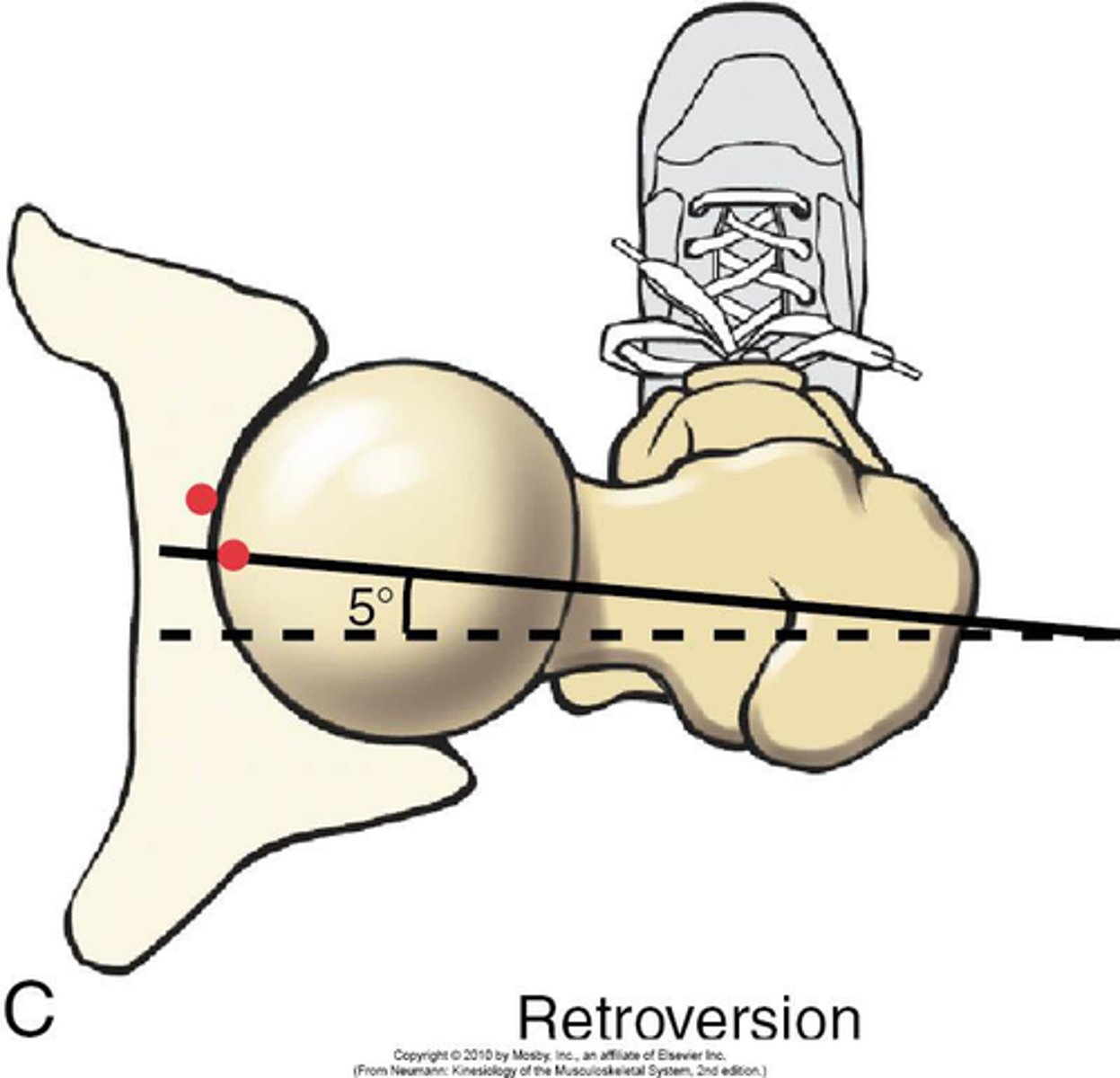
retroversion functional deficits
moment arm of glut med INCREASES
joint reaction forces DECREASE
joint congruency INCREASES
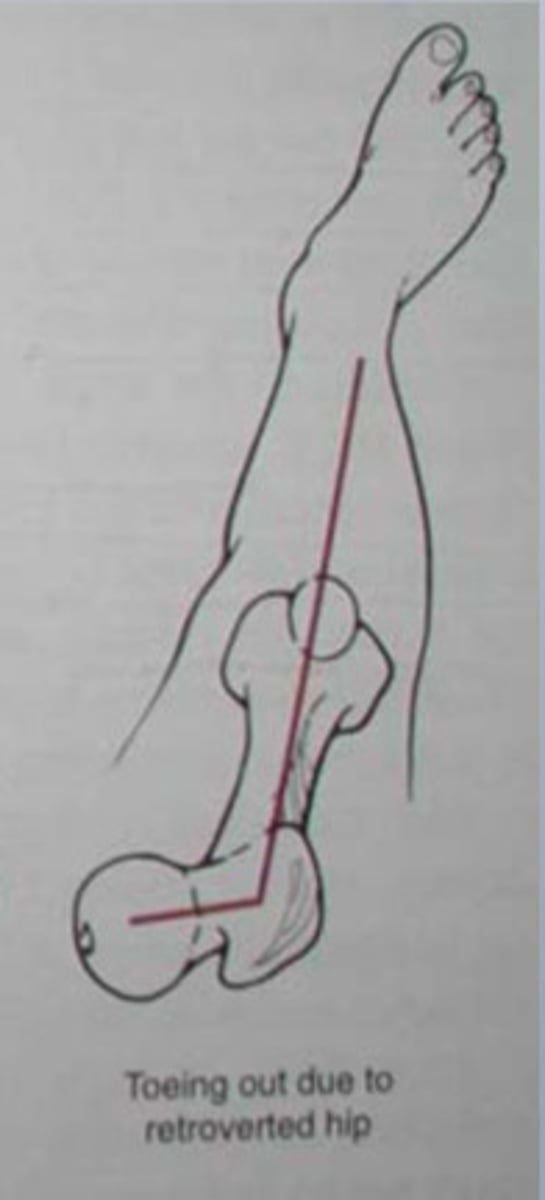
retroversion compensatory changes
toe out gait to normalize joint congruency
*may result in compensatory medial torsion of the tibia and pronation of the foot/ankle
medial, pronation
Toe out compensatory changes may result in __________ torsion of the tibia and _______________ of the foot/ankle.
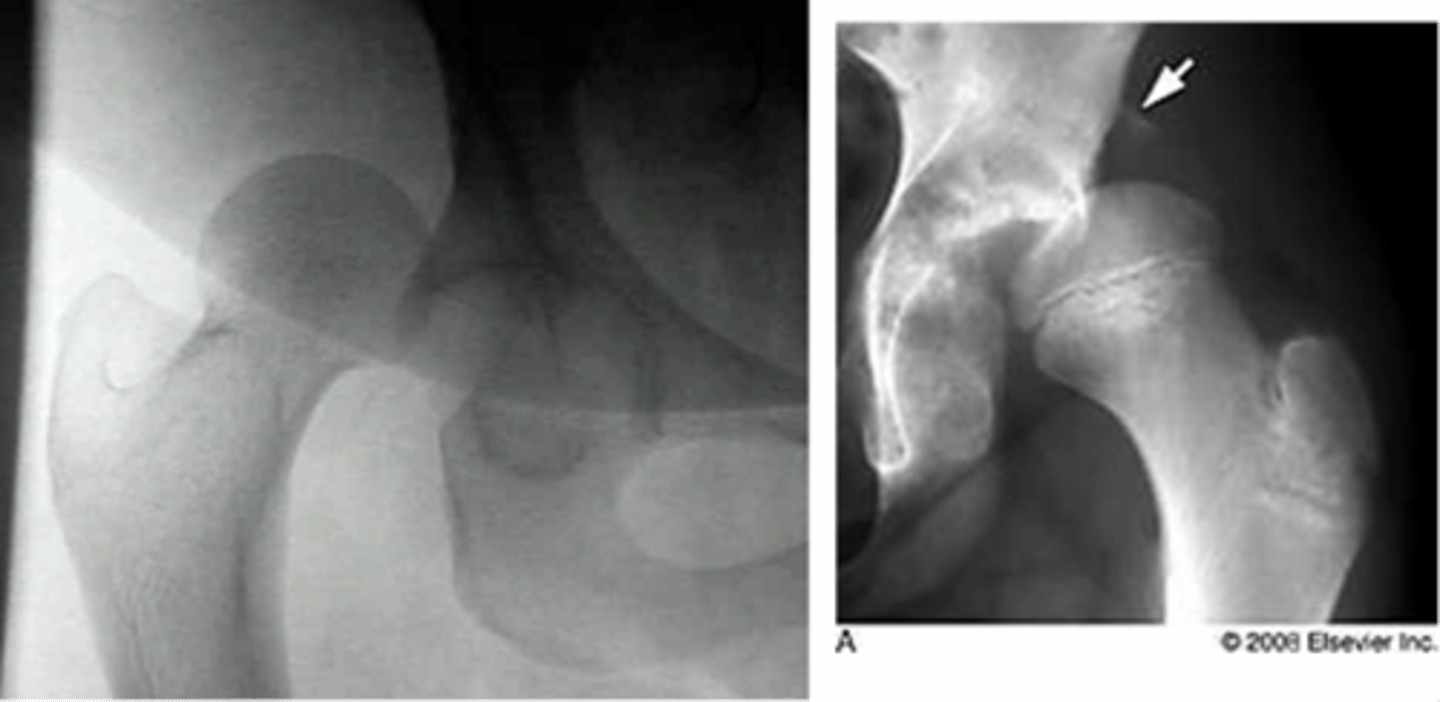
slipped capital femoral epiphysis
gradual or acute failure of the epiphyseal plate of the head of the femur due to shear forces parallel to the growth plate, causing the head to slide posterior/inferior
*may be related to trauma, inflammation, obesity, or hormonal factors
**more likely in males, onset approx 13 yrs of age (10-17)
FUNCTIONAL DEFICITS--> pain, gait changes (antalgic pattern)
COMPENSATORY MOVEMENTS--> may result in growth deficits, complications include avascular necrosis

posterior/inferior
In which direction(s) does the femoral head slide in a patient with slipped capital femoral epiphysis?
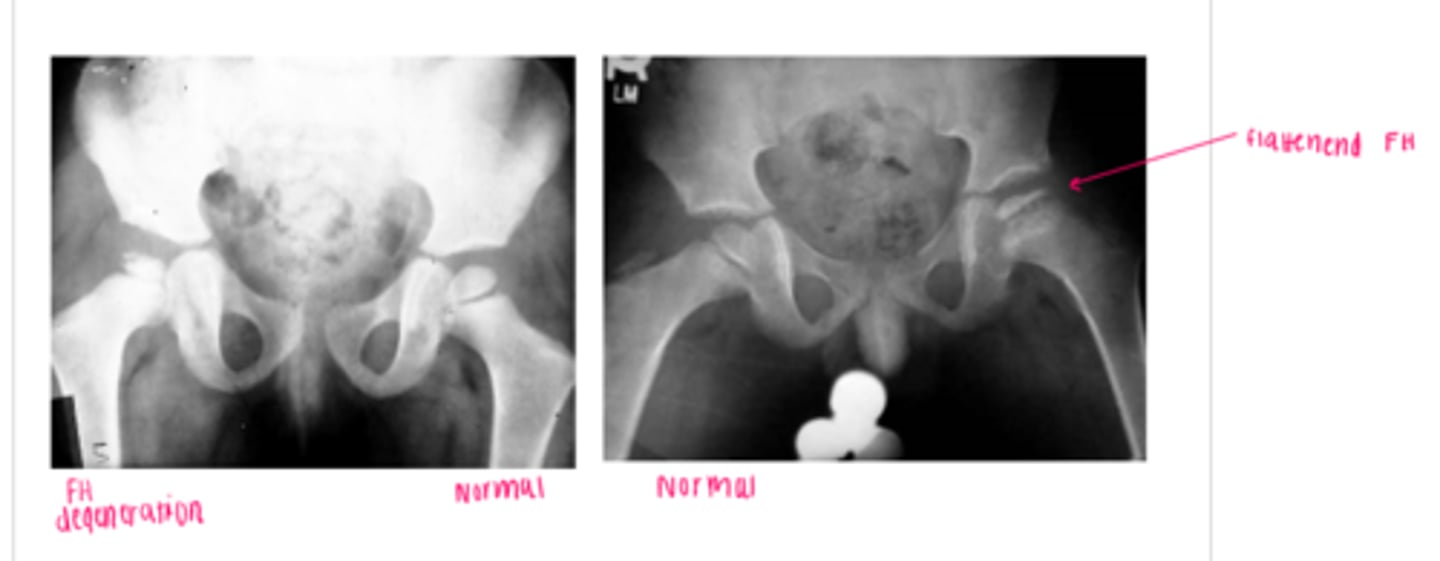
Legg-Calve-Perthes Disease
a type of osteochondrosis or disease of the growth centers in children which begins as a degeneration followed by regeneration and recalcification
*unknown etiology
**more likely in males, onset is generally 5-7 yrs of age (3-13)
FUNCTIONAL DEFICITS--> pain, limited ROM, gait changes
COMPENSATORY MOVEMENTS--> limit motion/use of the joint, limit overall activity level
COURSE--> bone necrosis, revascularization, reossification over a period of 24-36 months
femoral acetabular impingement (FAI)
impingement between the femoral head/neck and acetabular rim
*occurs secondary to previous hip trauma/pathology with boney overgrowth (osteophytes)
TYPES:
1. cam
2. pincer
*most individuals have a combo of both
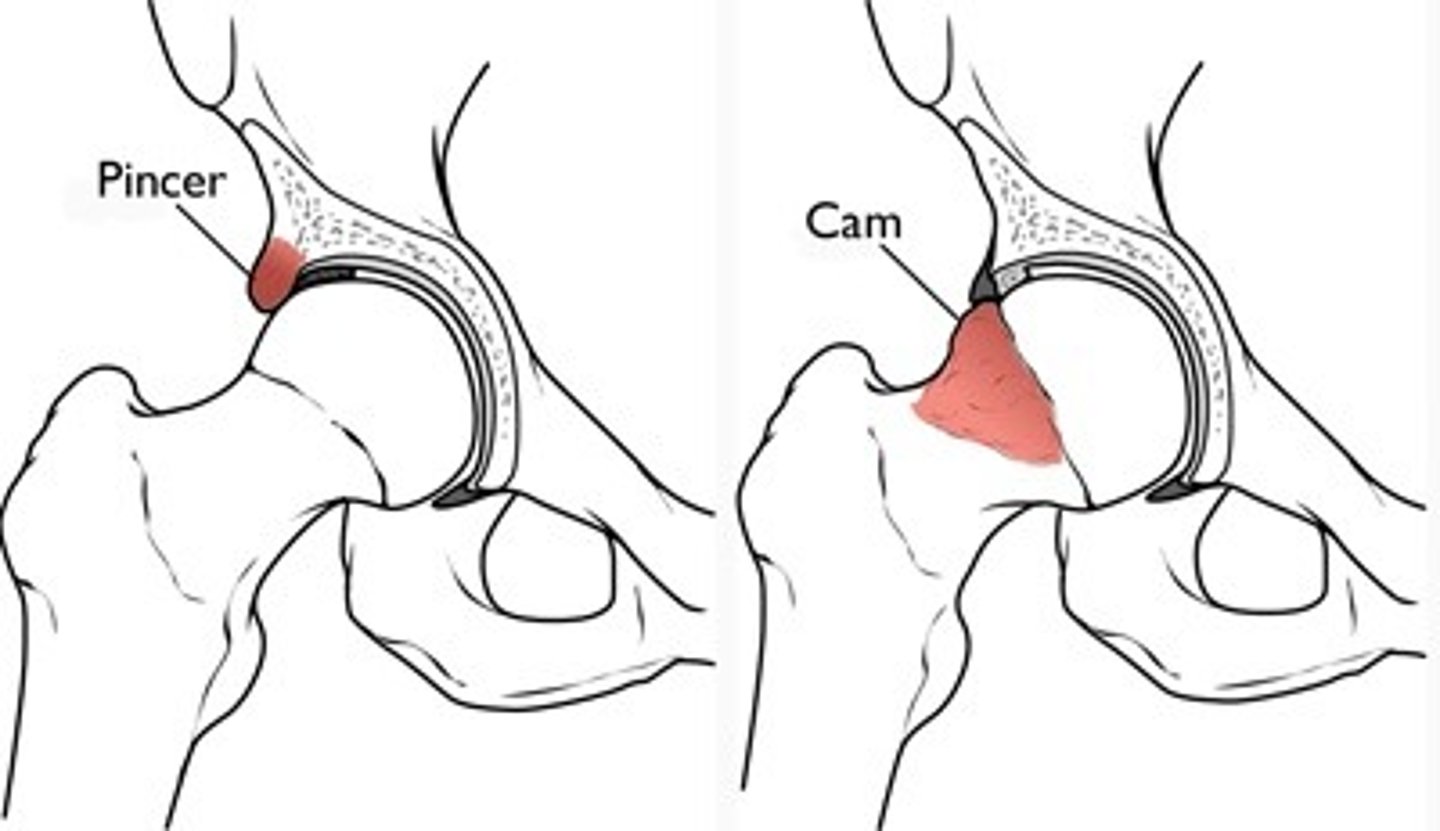
Cam type FAI
overgrowth of the femoral head/neck

Pincer type FAI
overgrowth of the acetabular rim

hip fractures
associated with decreased bone density and falls in the elderly (av. age 70)
females > males
STRUCTURES:
1. femoral neck/subcapital
2. intertrochanteric
FUNCTIONAL DEFICITS--> pain, difficultly or inability to ambulate, rotational deformity
COMPENSATORY MOVEMENTS--> LE will shorten and ER
*if able to ambulate, will present with decreased step length of the opposite side
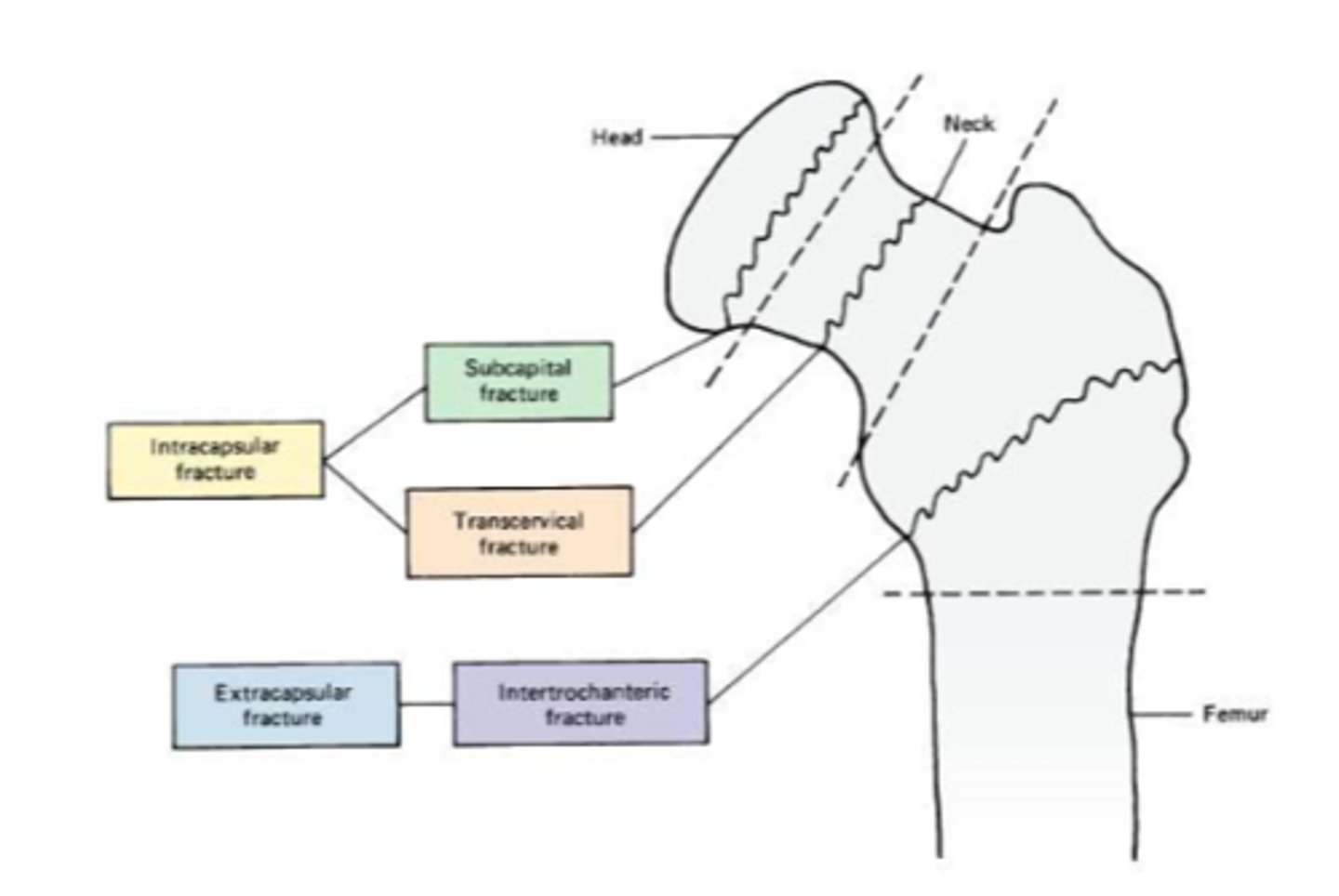
femoral neck (subcapital), intertrochanteric
What are the 2 most common hip fractures?
shorten, ER
With a hip fracture, the LE will ____________ and ____.
decreased, opposite
If a patient is able to ambulate, they will present with _________________ step length of the ________________ side.
HINT: can't bear the weight of the body
pelvic fractures
generally result from a high force injury (ex. MVA) accompanies by multiple internal trauma
STRUCTURE--> pelvic ring with generally more than one site
FUNCTIONAL DEFICITS--> pain with ambulation or inability to ambulate
COMPENSATORY MOVEMENTS--> slow antalgic, may need assistive device, may require fixation of the fracture sites
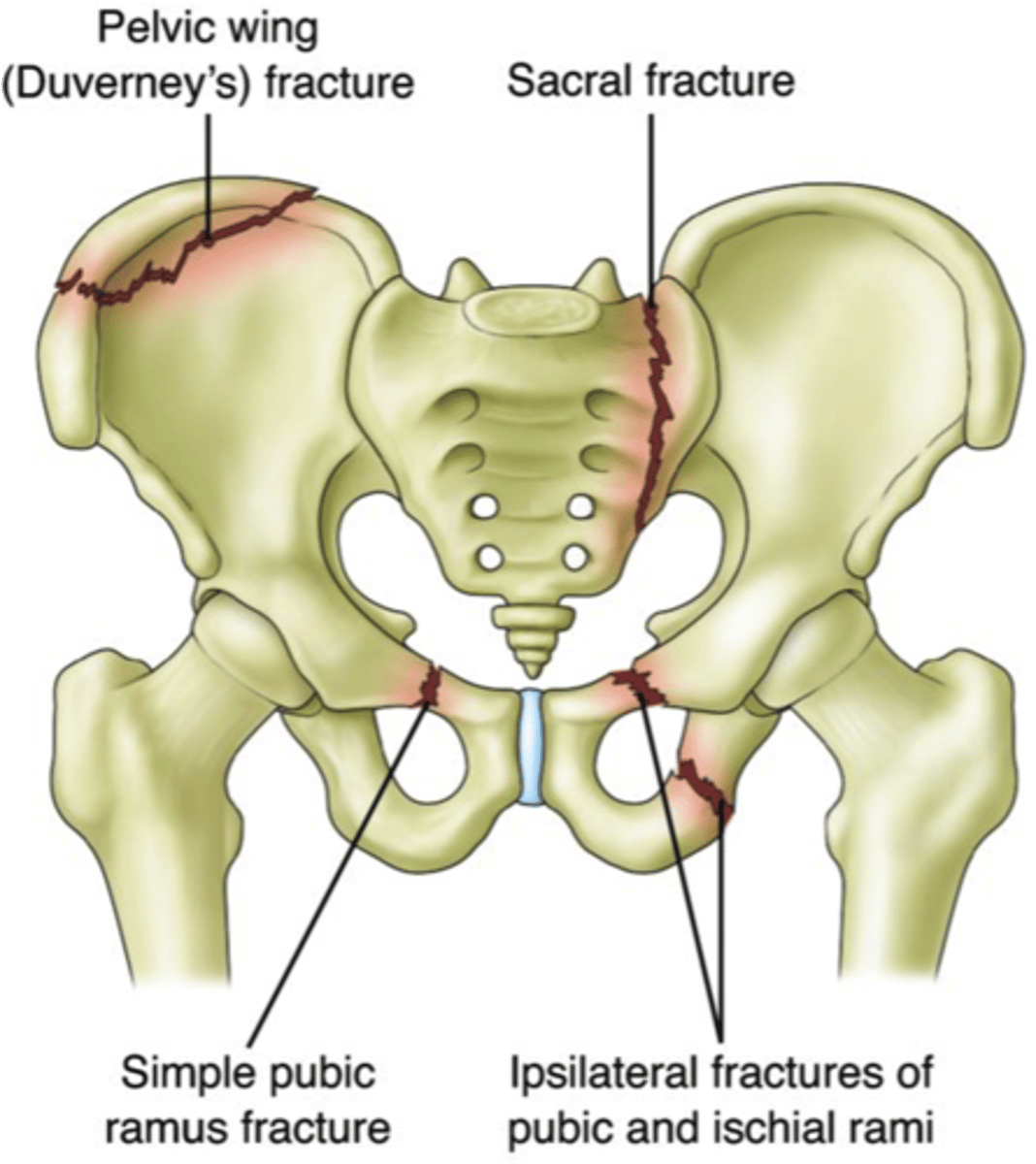
open book fracture of pelvis
disruption of pubic symphysis
*type of pelvic fracture

coxo-femoral dislocation
causes by high force (generally MVA)
*usually occurs posterior when the leg is flexed, adducted and medially rotated (crossed legs in passenger seat of car)
STRUCTURES--> tearing, overstretching of the joint capsule, labrum, and ligaments
FUNCTIONAL DEFICITS--> pain, limited motion, through may be hypermobile and prone to redislocation due to weakened/damaged joint structures
COMPENSATORY MOVEMENTS--> antalgic gait, muscle guarding around the joint
articular involvement
VERY COMMON IN CLINICAL SETTINGS
1. rheumatoid arthritis
2. osteoarthritis (aka DJD)
- total hip replacement
3. avascular necrosis
rheumatoid arthritis
systemic autoimmune inflammatory disorder which causes destruction of periarticular tissue
STRUCTURES--> joint capsule, ligaments, articular cartilage, tendon and muscle
FUNCTIONAL DEFICITS--> loss of ROM, strength, pain, swelling
COMPENSATORY MOVEMENTS--> joint protection via unweighting (assistive device, need to watch areas of pressure)

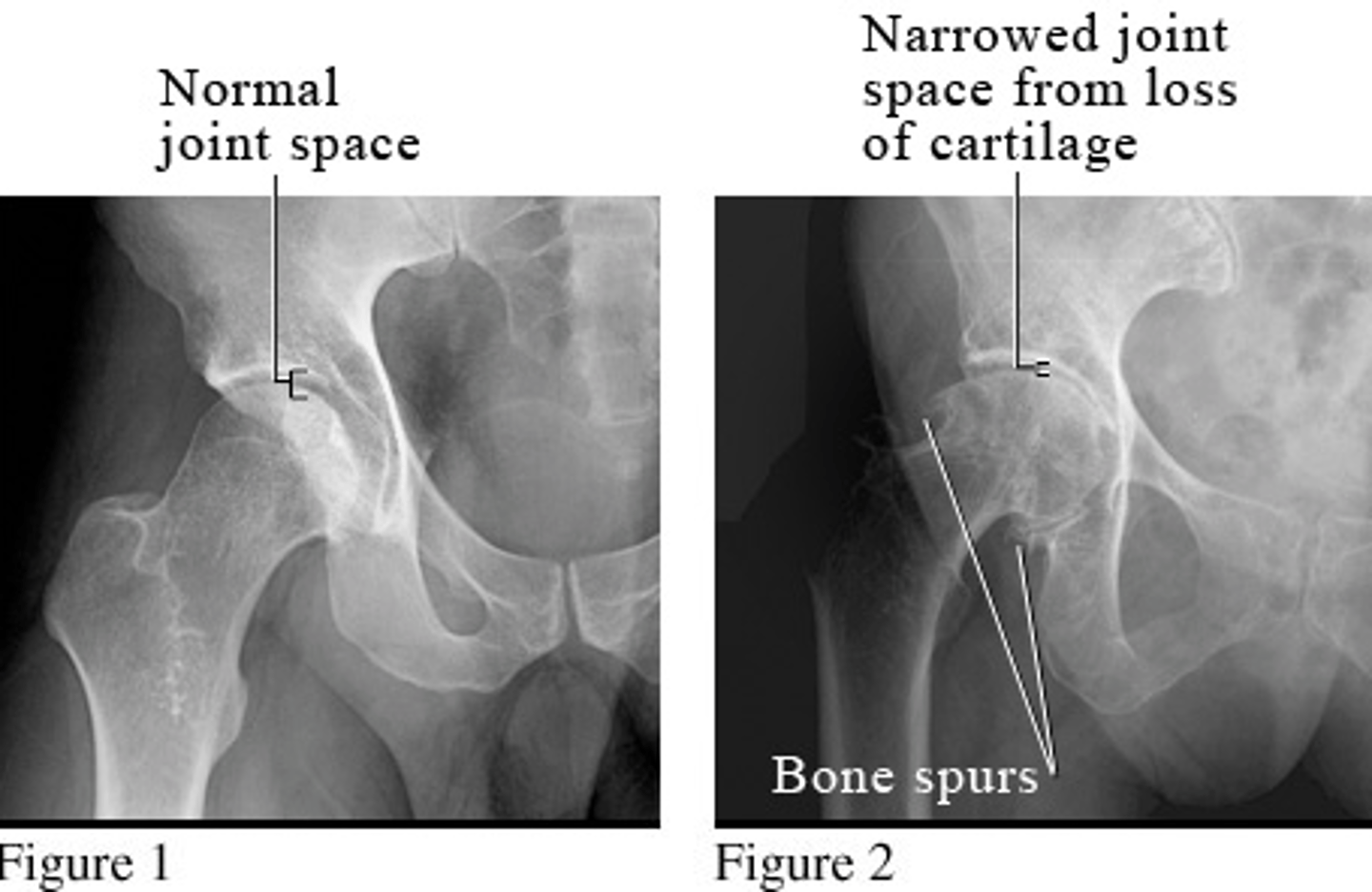
osteoarthritis
wear and tear arthritis
*occurs equally in males and females
**associated with trauma (50%) or idiopathic (50%)
***increased with height to weight ratio
STRUCTURES--> joints, primarily weight-bearing
FUNCTIONAL DEFICITS--> decreased ROM, pain
COMPENSATORY MOVEMENTS--> antalgic gait pattern, may present with Trendelenberg gait due to muscle weakness, or may see gluteus medius gait
*associated with a high percentage of total hip replacement
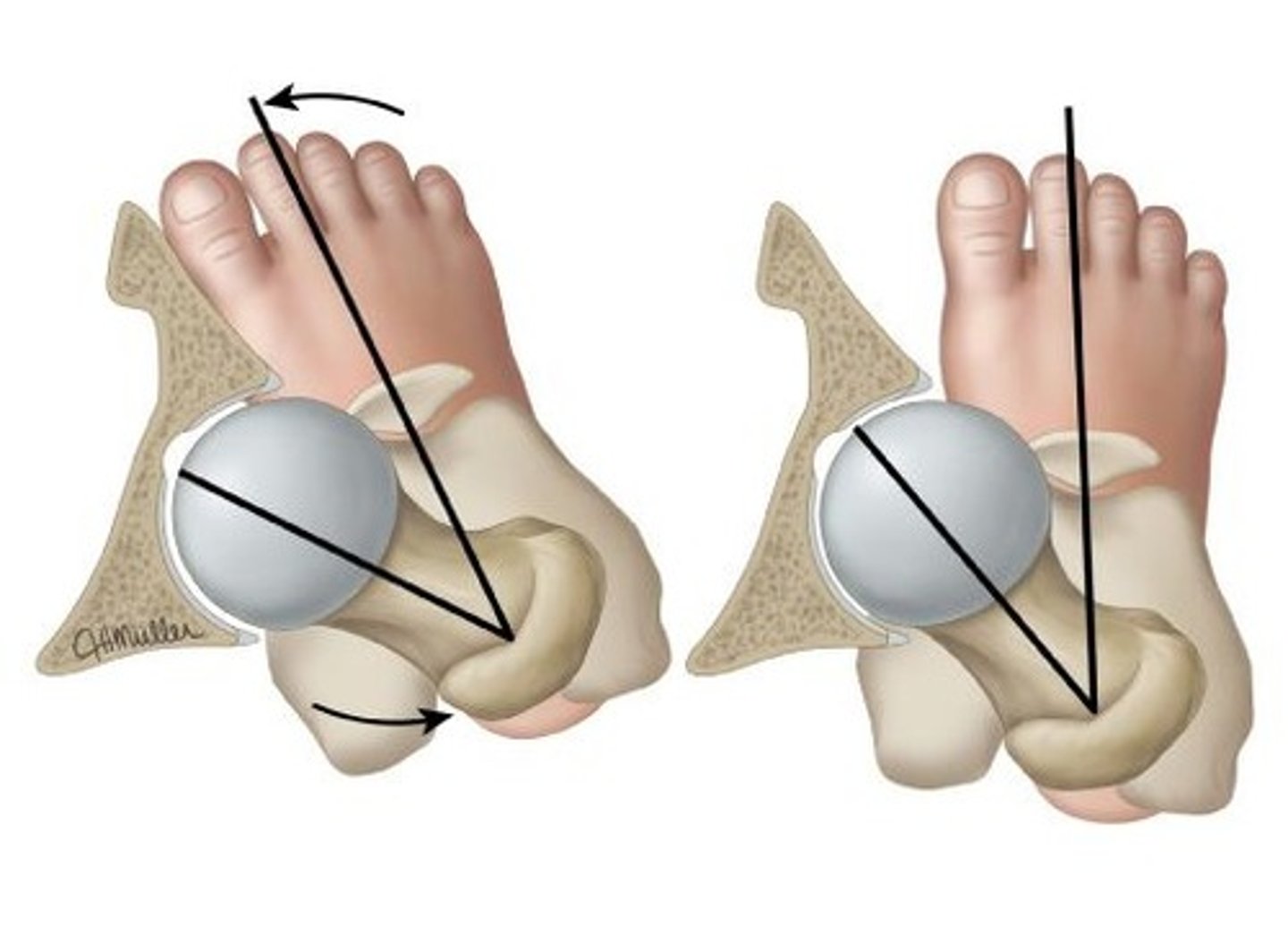
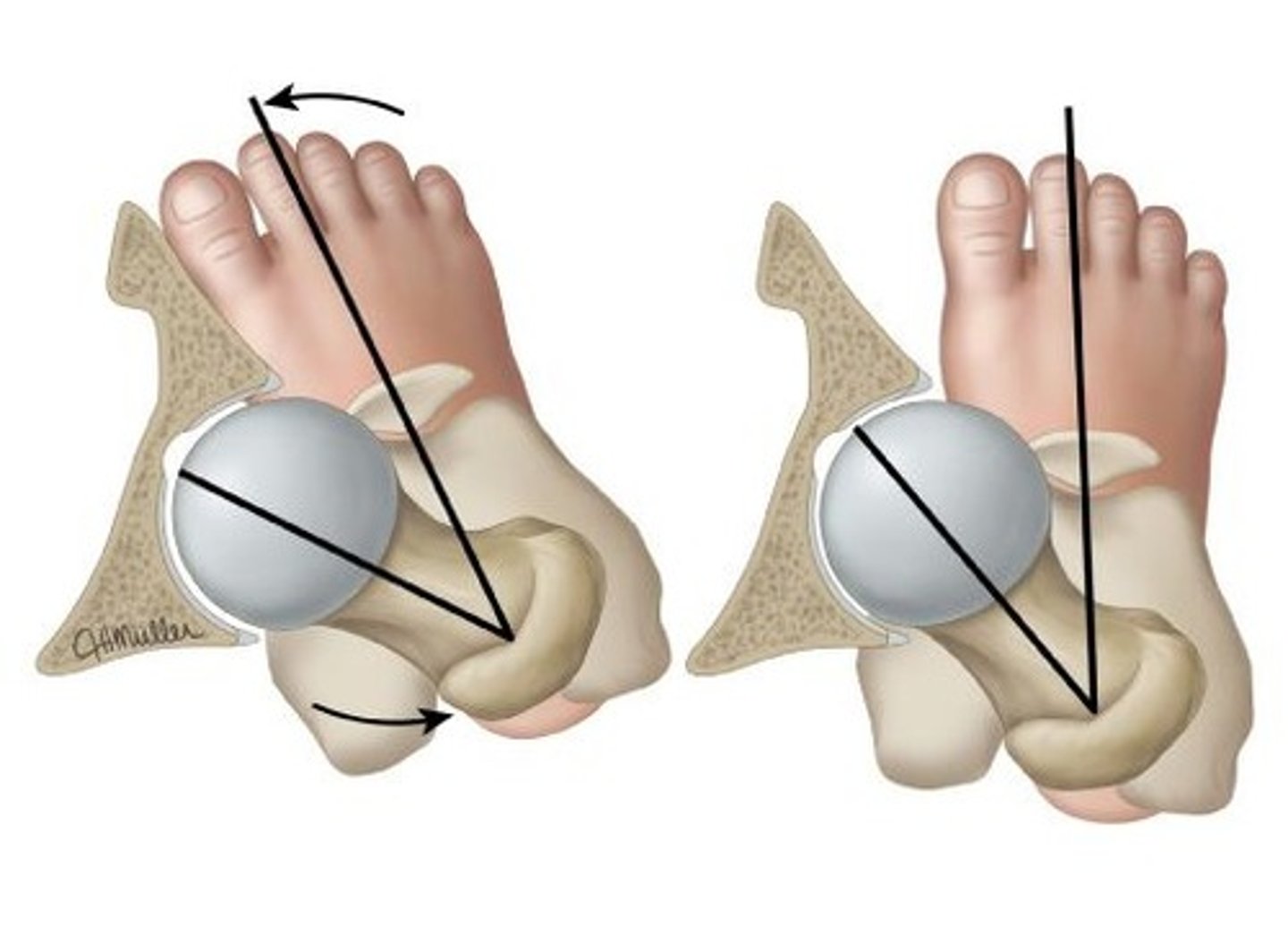
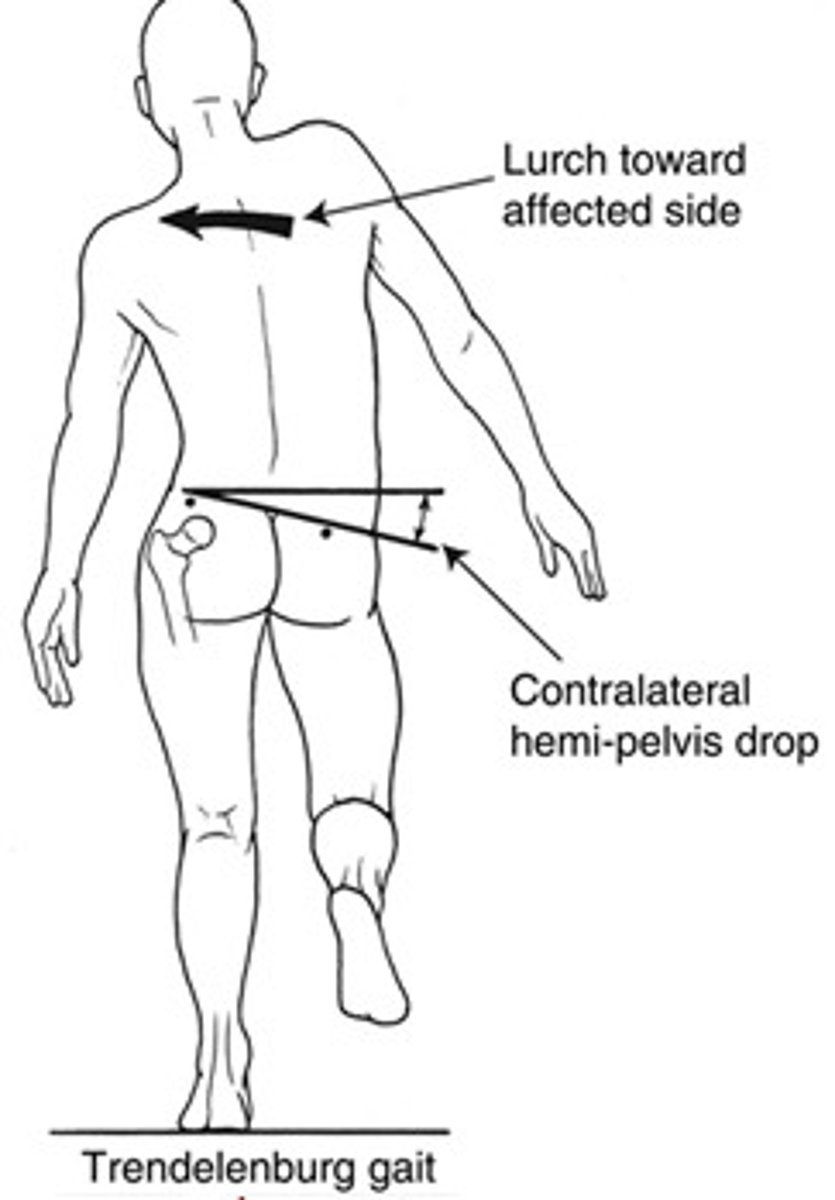
Trendelenburg gait
gait pattern that denotes gluteus medius weakness
*hip drop toward the non-affected side
ex. drop L hip w/ R glut med weakness
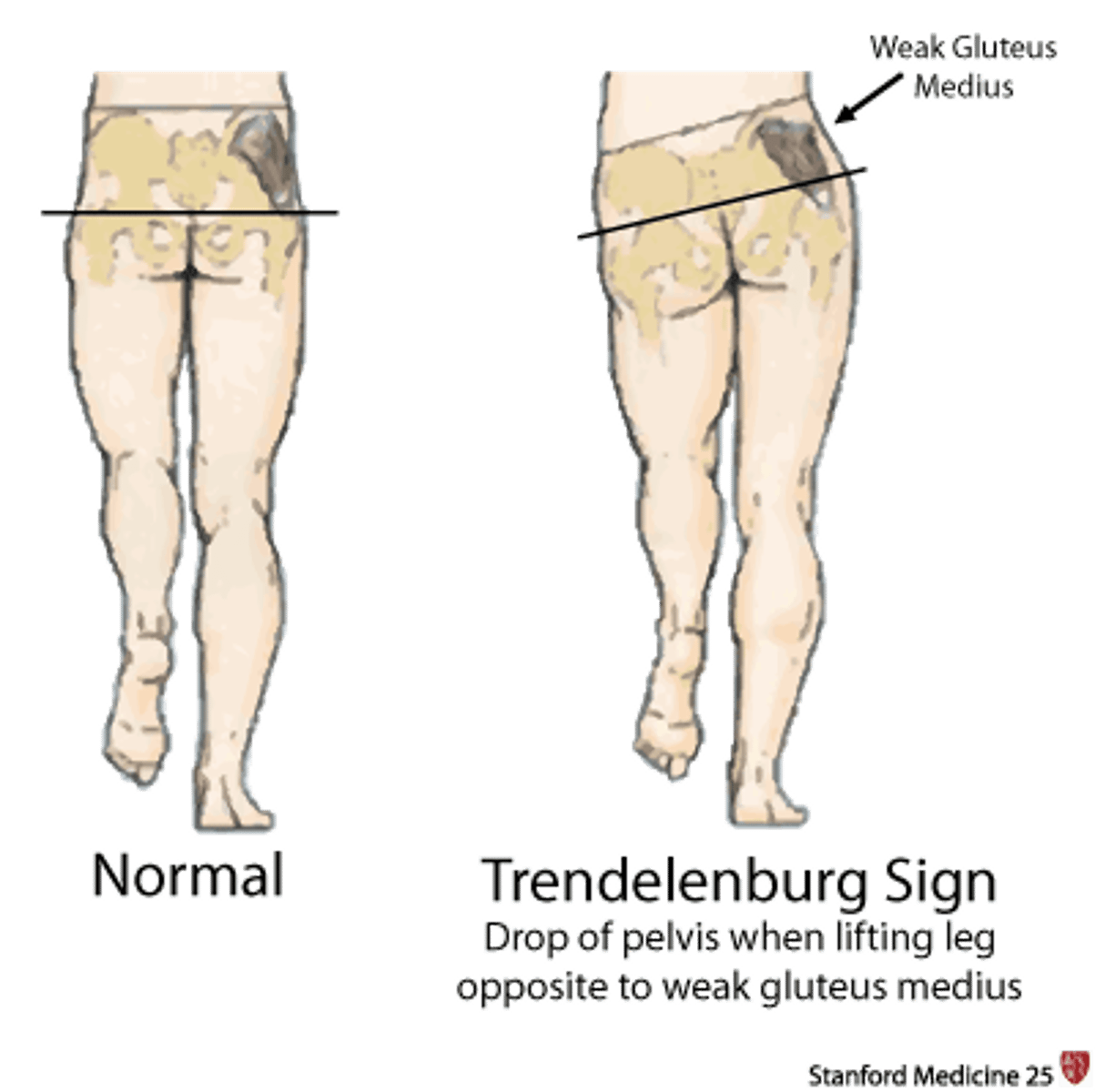
gluteus medius gait
gait pattern that denotes gluteus medius weakness
*individual shifts the trunk over the affected side during stance phase
avascular necrosis
involves death of the bone tissue due to compromised blood supply
*can be post surgery, due to trauma, corticosteroid use, alcohol abuse, in deep sea divers, or may occur with no known pathology
STRUCTURE--> femoral head
FUNCTIONAL DEFICITS--> pain, limited ROM, joint collapse/destruction
COMPENSATORY MOVEMENTS--> shift body weight to limit force through the affected region (gluteus medius gait), limit activity

soft tissue involvement overuse syndromes
1. iliotibial band syndrome
2. iliopectineal bursitis
3. gluteal tendinopathy
4. ischiogluteal bursitis
soft tissue overuse syndromes
caused by repetitive trauma to a region via internal or external forces which creates inflammation within the soft tissue
STRUCTURE--> bursae, tendon, or tendon sheath
FUNCTIONAL DEFICITS--> pain, with activities which further stress the region via external compression, active contraction of overlying muscles or passive stretching of overlying muscles
COMPENSATORY MOVEMENTS--> avoidance of activities which reproduce stress
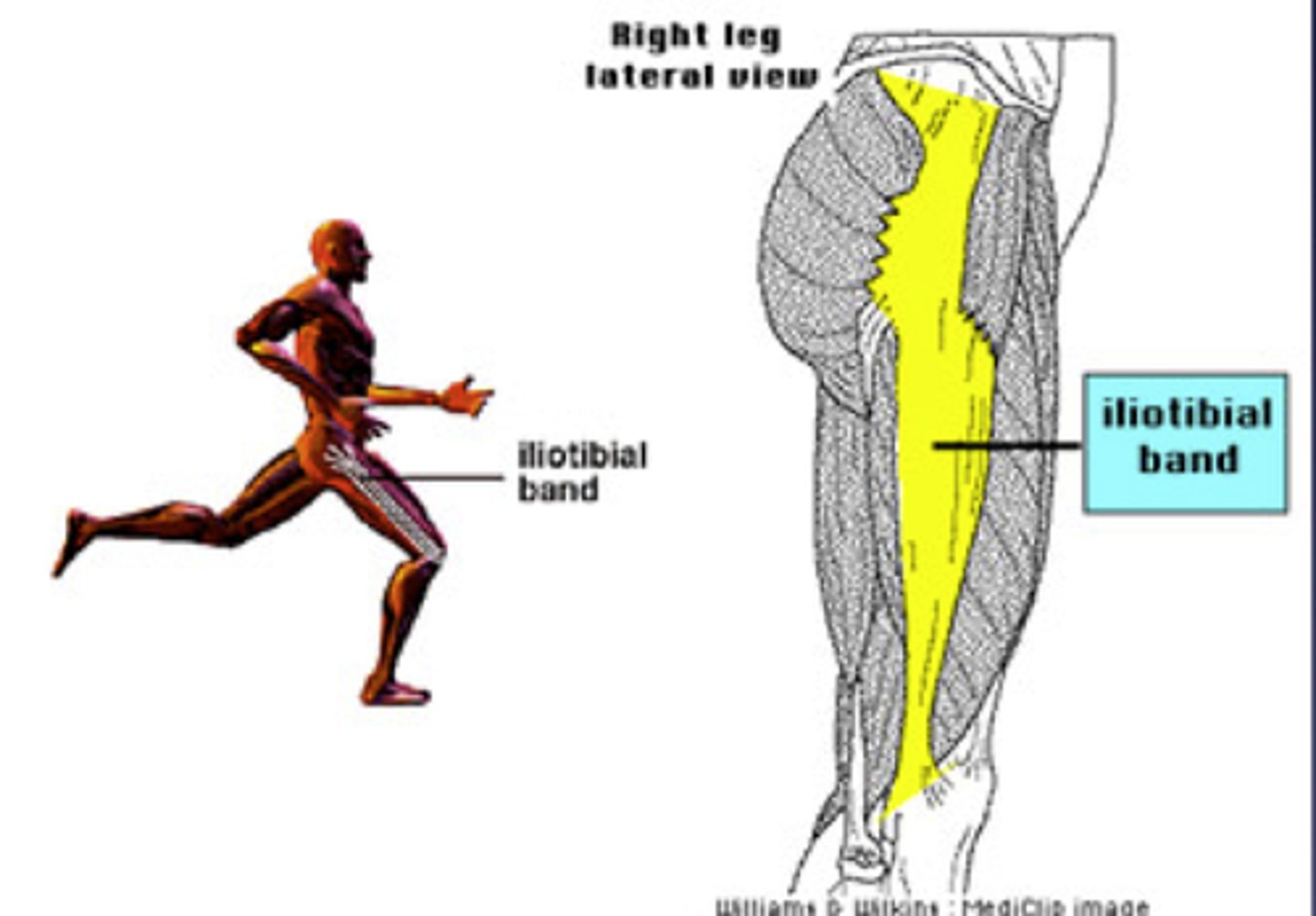
iliotibial band syndrome
- tendinitis
- frequently seen in downhill runners
- associated with patellofemoral pain
- ITB tightness may be a factor
- quads and hamstrings also have attachment to lateral intermuscular septum/continuous with ITB
HINT: glut max and tendinitis insert here
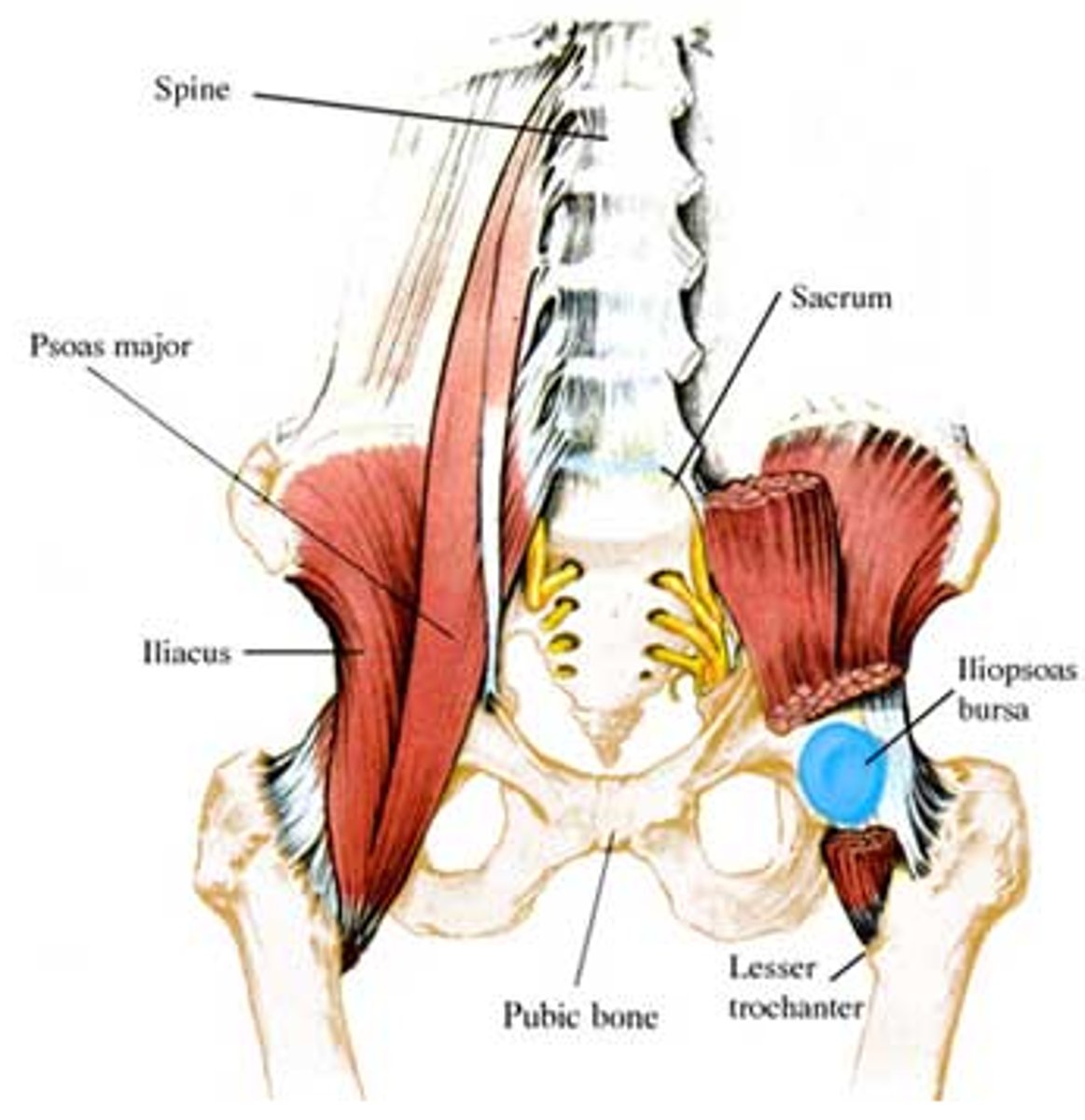
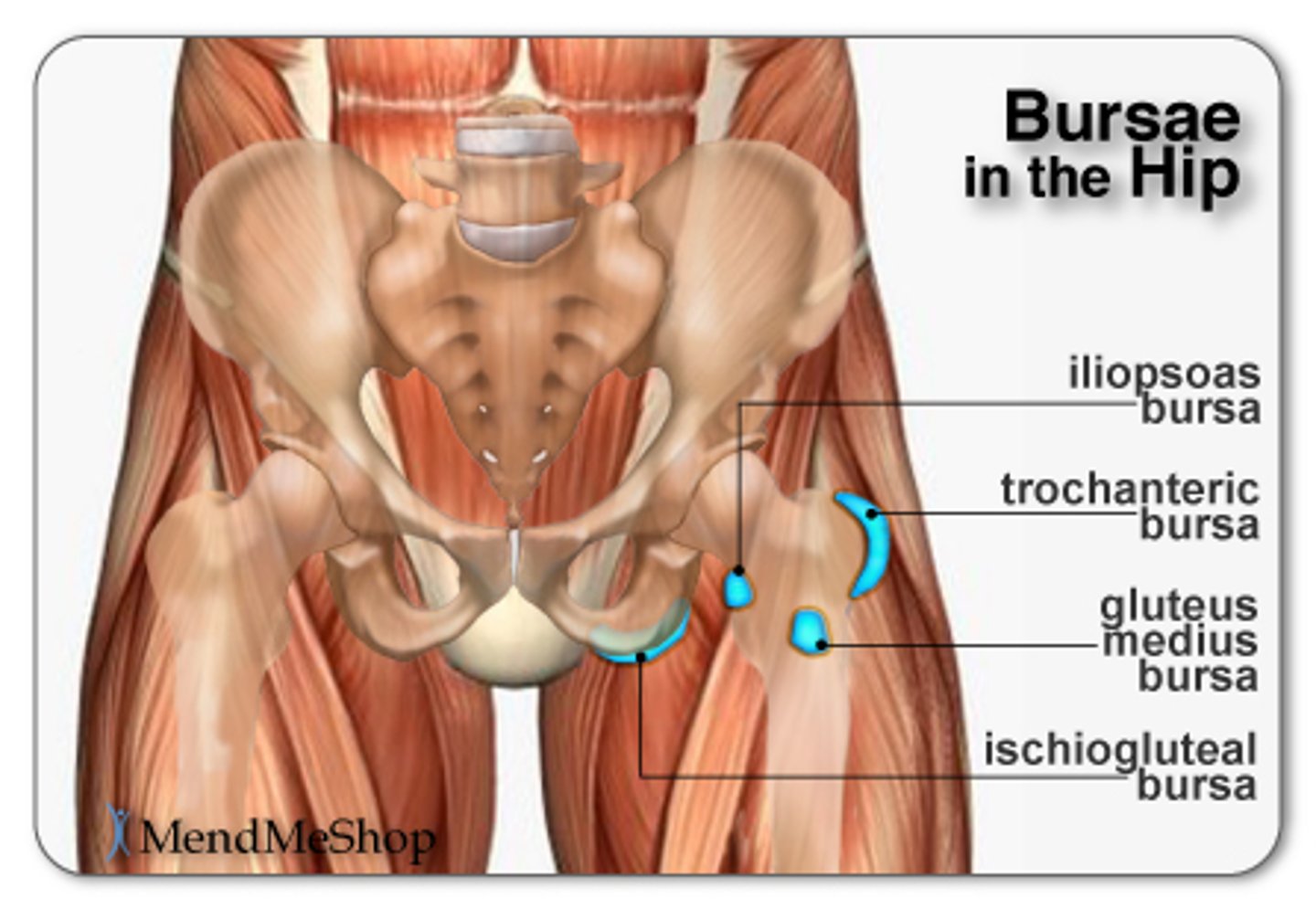
iliopectineal bursitis
bursae lies between the deep surface of the iliopsoas muscle and the anterior aspect of the hip joint
*irritatied with repetitive hip flexion/extension
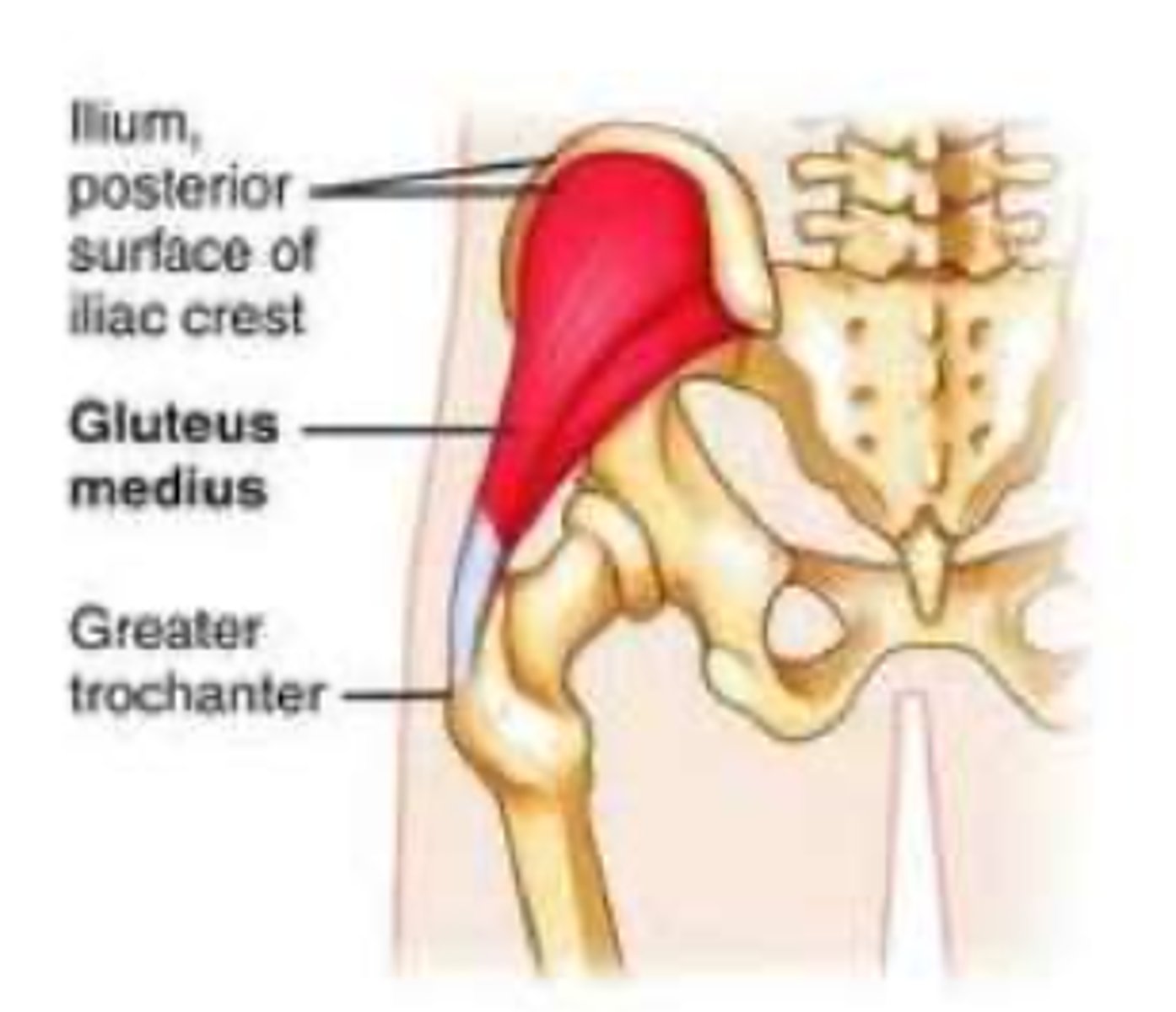
gluteal tendinopathy
non-inflammatory degenerative condition within the tendon due to collagen overload within the tendon
*though to be due to repetitive loading
**results in pain with contraction of the gluteal muscles or with passive stretching
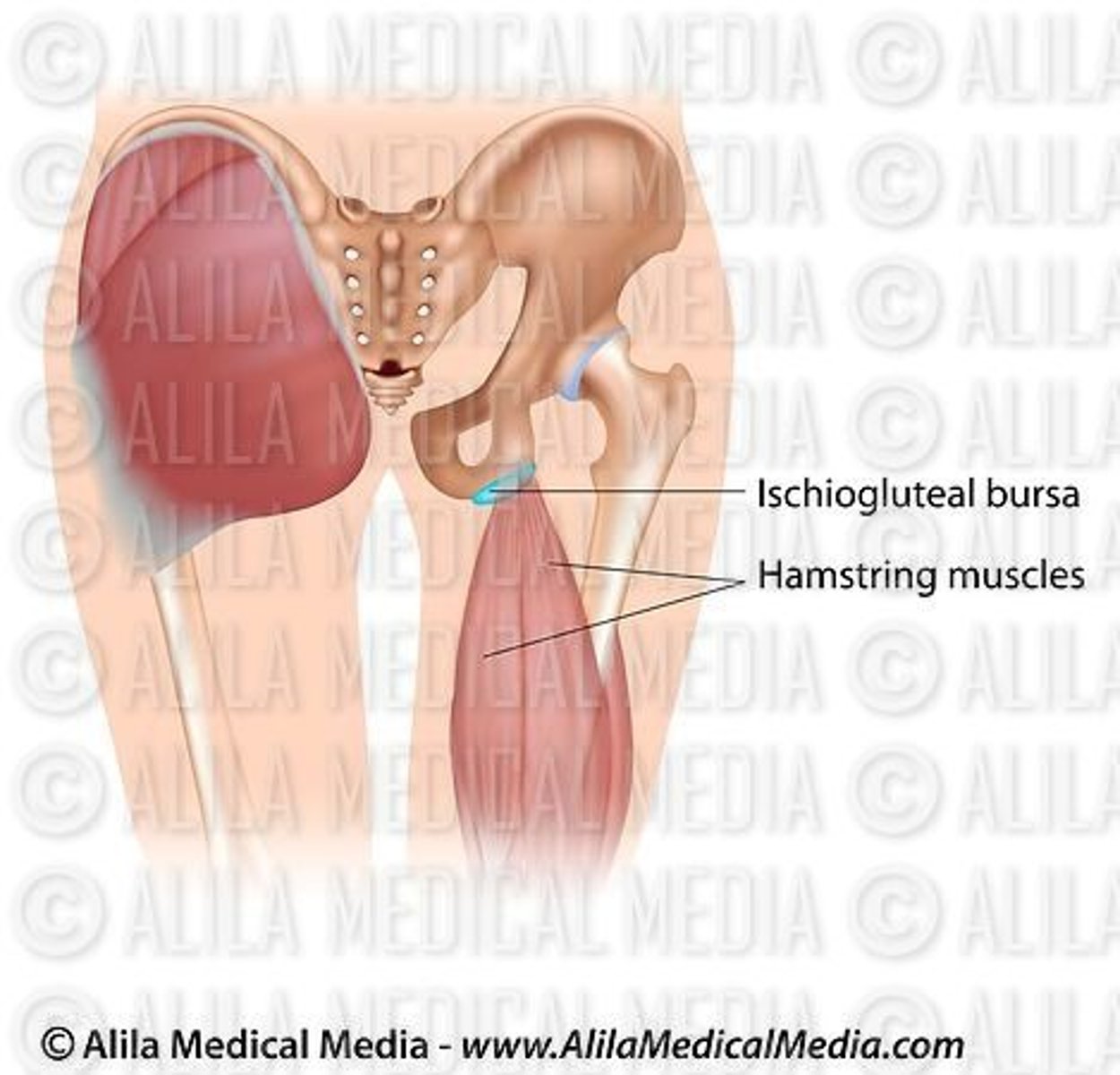
ischiogluteal bursitis
bursae located over the ischial tuberosity
*may occur with sciatic nerve, and/or posterior cutaneous nerve irritation due to the proximity to this nerve
**may also be a tendinopathy of the hamstrings at their origin
hip bursitis
irritation of the greater trochanteric bursa of the hip; often caused by rubbing of the musculature
muscular involvement (GAIT issues)
weakness--> due to nerve involvement (LESS COMMON), disuse, injury, pain, muscle disease
tightness/contracture (MORE COMMON)--> decreased flexibility/extensibility of the muscle due to disuse/immobilization, injury or disease
*passive insufficiency
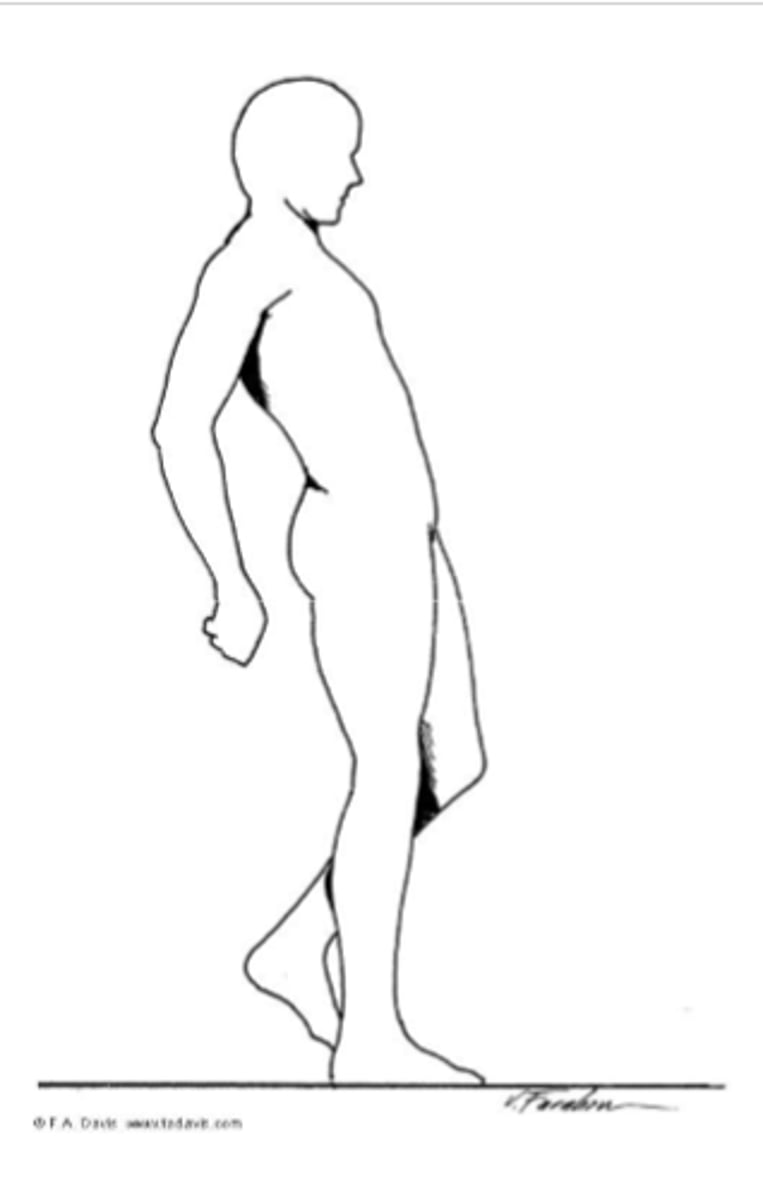
gluteus maximus
muscular involvement
weakness - results in Gluteus Maximus gait
*backward lean to compensate for weakness
gluteus medius
muscular involvement
weakness - results in Gluteus Medius Lurch (ipsilateral lean) if compensated or a Trendelenburg Gait (dropping of the contralateral pelvis) if uncompensated
*may be seen with gluteal medius tendinopathy
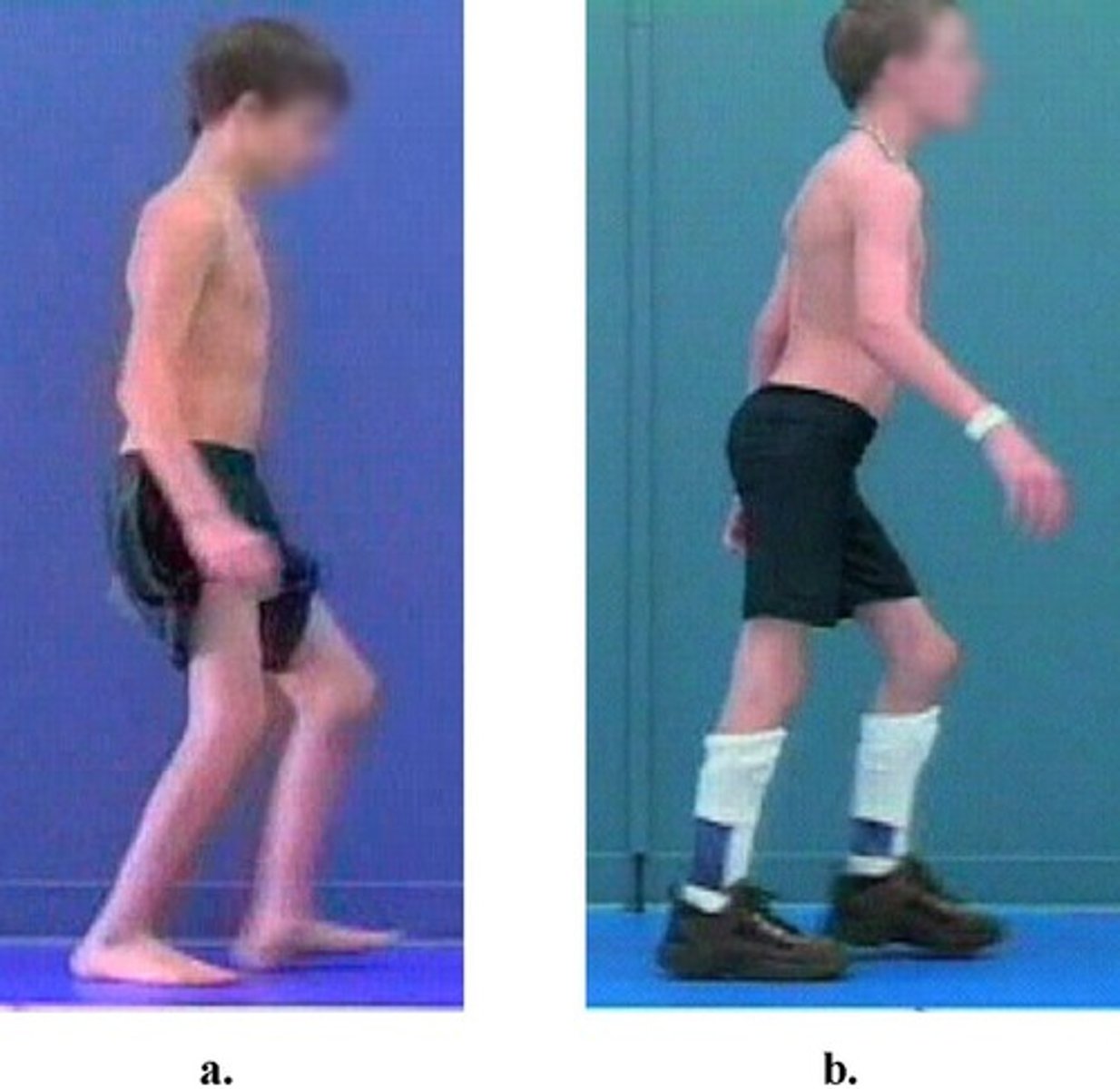
IMAGE = LURCH
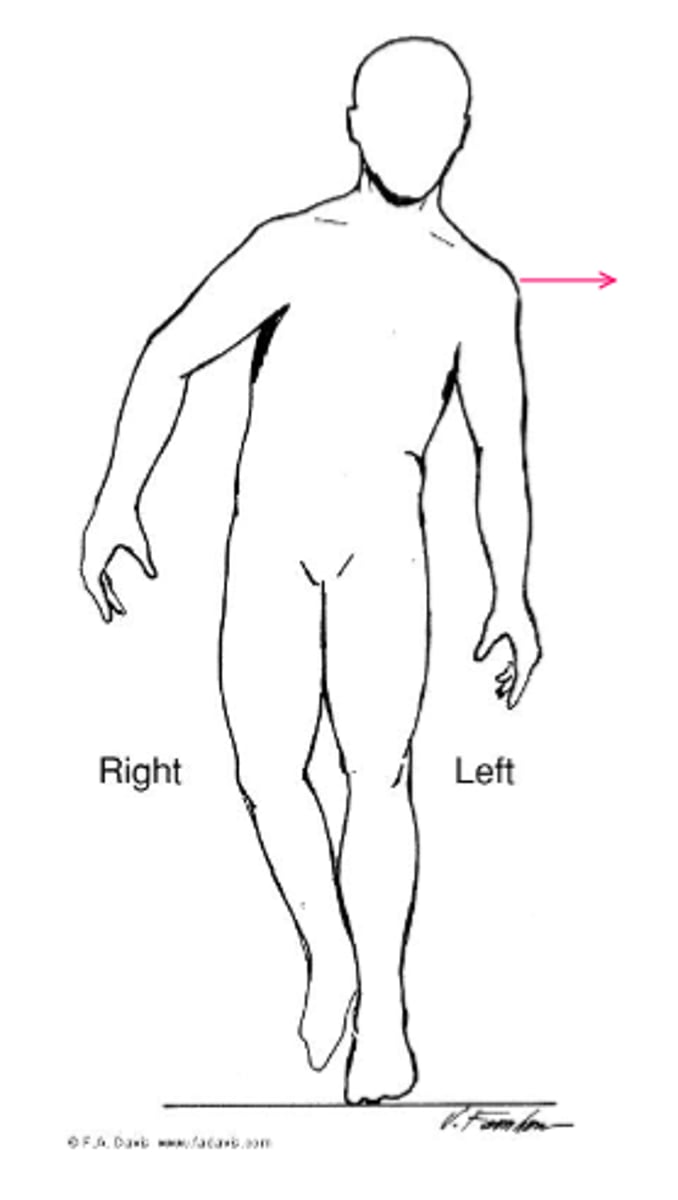
compensated, uncompensated
Gluteus medius weakness results in Gluteus Medius Lurch (ipsilateral lean) if it is ____________________ or a Trendelenburg Gait (dropping of the contralateral pelvis) if it is ________________________.
hamstrings
muscular involvement
weakness - difficulty with hip extension, less control of leg in swinging forward
tightness- results in inability to fully extend the knee when the hip is flexed, associated with posterior tilting of the pelvis, in extreme cases results in a crouched gait
eccentrically
With hamstring weakness, the hamstrings have a hard time ___________________ controlling the forward swing.
iliopsoas
muscular involvement
weakness - may see a decreased speed of walking, but can still ambulate with marked weakness (2+/5)
tightness- results in more marked effect on gait with anterior pelvic tilting (requires increased energy to maintain erect position)
*decreased step length of the contralateral side
contralateral
Iliopsoas weakness leads to a decreased step length of the ________________ side.
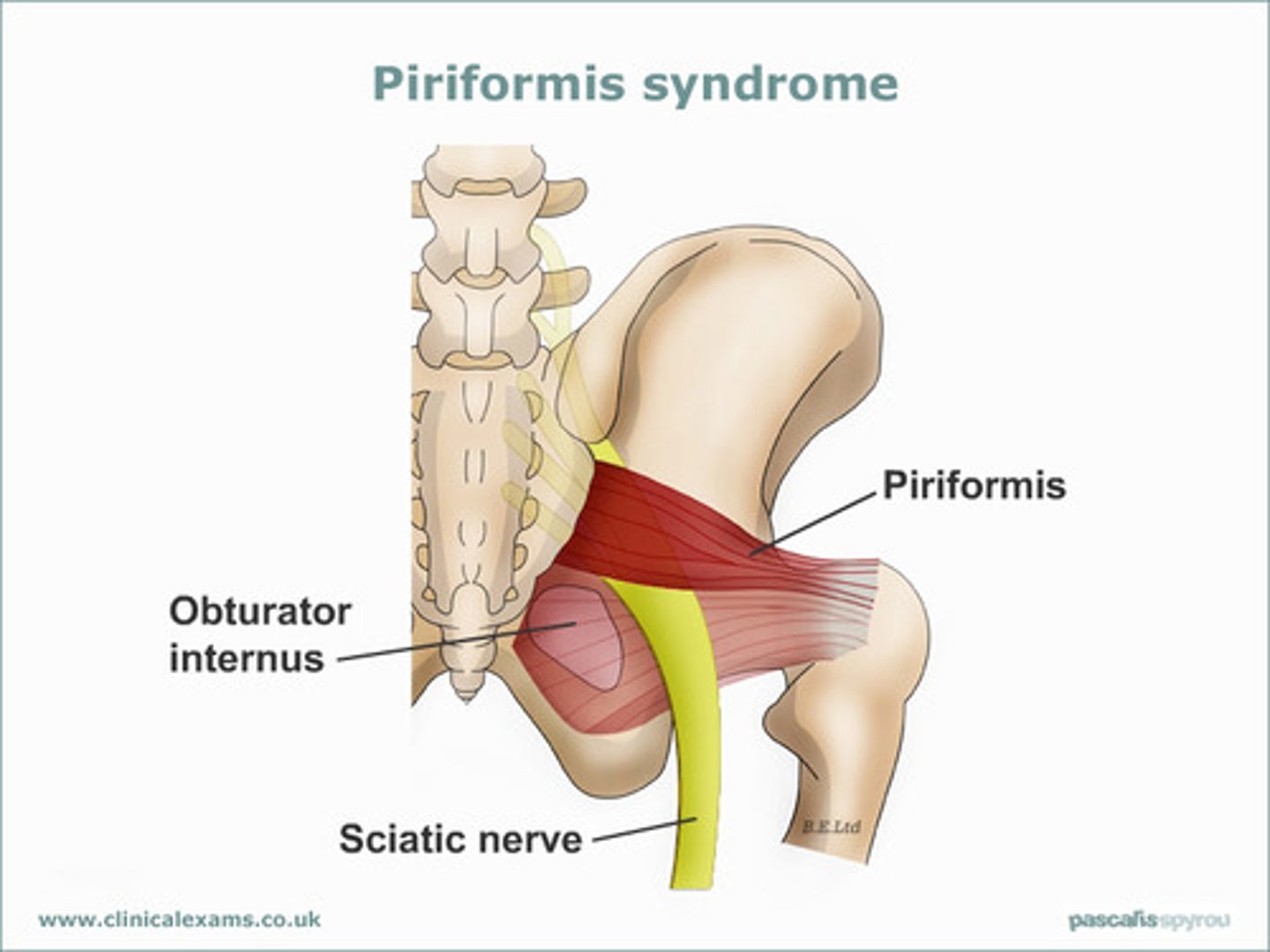
piriformis syndrome
muscular/nerve involvement
structure - piriformis muscle spasm or tightness, can result in compression of the sciatic nerve in the greater sciatic notch
etiology - related to lower back pain, SI joint dysfunction, postural changes or activity involving hip ER
functional limitations/compensatory movements - less painful with muscle on slack (ER), can result in contracture over time, pain with palpation, and resisted ER
meralgia parasthetica
nerve involvement
irritation of the lateral femoral cutaneous nerve
etiology - more common in those who utilize workbelts as it occurs as a result of compression as the nerve passes just inferior to the ASIS, and pierces the iliotibial fascia
*numbness & tingling on outer side of thigh
functional limitations/compensatory movements - NO motion limitations, NO weakness, NO weightbearing difficulty
*complaints limited to sensory changes