Exam 3
1/157
Earn XP
Description and Tags
Unit 3 Flashcards
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
158 Terms
COMMUNICATION DISORDERS
What is involved in effective communication?
Effective communication involves:
Clear expression of thoughts
Active listening
Both speaker and listener understanding the message of the conversation
Signaling to appropriate Nonverbal Cues (body language)
Give feedback to ensure comprehension
Communication
Any verbal/nonverbal behavior that influences the behaviors, ideas or attitudes of another individuals.
It is the process of sharing information between people, groups or places. It requires a Sender, Receiver, and a Message.
Speech vs Language
Speech is the PHYSICAL ACT of producing sounds, including an individual’s articulation, fluency, voice, and resonance. Speech is considered “expressive” production of sounds
Language, regards the socially-shared rules about word meaning
Communication Disorders
A disorder characterized by deficits in speech, language, and/or communication
Impairments can occur in ability to receive, send, process and comprehend verbal/nonverbal messages
The 4 common types of communication disorders
Language Disorder
Speech-Sound Disorder
Child-Onset Fluency Disorder
Social Communication Disorder
Language Disorder - Definition
Problems acquiring, comprehending and using language (written OR spoken)
These language difficulties cannot be explained by other conditions, such as hearing loss or autism, and cannot be “enhanced” by exposure to language (even during early development).
Receptive vs Expressive Language Disorders
RECEPTIVE Language disorders involve difficulty in understanding written/spoken language
EXPRESSIVE language disorders involve problems with communicating thoughts and feelings through language
Language Disorder - Diagnostic Criteria
Language skills are much lower, perceptually and quantifiably, than expected for the person’s age. Results in limitations in effective communication, social participation, academic achievement or occupational performance.
Persistent difficulties in acquiring/using language to communicate.
Onset of symptoms is in early developmental period (birth-5yo)
Difficulties are NOT ATTRIBUTABLE to other sensory impairments OR medical conditions.
Language Disorders - Physical Characteristics
Reduced Vocabulary (word knowledge + use)
Limited sentence structure (deficits in use of syntax/morphology)
Impairments in discourse (inability to use vocab + connect sentences to explain a topic).
Language Disorder - Prevalence + Risk Factors
Prevalence - 7% of school-aged children (50% outgrow these issues).
Risk Factors -
Genetics - family history of language/communication issues can INCREASE likelihood of developing disorder
Chronic Ear Infections - Repeated ear infections during early childhood can impact hearing, which may affect language development
Temporal Lobe Processing/functional connectivity deficits - problems in the temporal lobe (Wernicke’s = language comprehension) may contribute to language difficulties
Between receptive and expressive language problems, which is more resistant to treatment?
Receptive Language problem are the most resistant to treatment.
Understanding language (receptive) is a COMPLEX process that involves not only hearing words but interpreting their meanings, whereas producing spoken language (expressive) can be readily practiced.
Speech Sound Disorder - Definition
Problems producing speech sounds.
Most common sound mix-ups are of w/r sounds.
Speech Sound Disorder - Characteristics
Impairment typically arises in articulation/sound production errors rather than word knowledge (which is a language disorder)
Trouble controlling rate of speech
Compared to peers in the same developmental age, speech of child tends to miss articulatory targets (most prominent in complex sounds)
Speech Sound Disorder - Prevalence + Risk Factors
Prevalence - 2-25% for children aged 5-7 yo
Risk Factors -
causes are unknown
Correlated risk factors include:
Family history
lack of learning supports
oral sucking habits
ear/nose/throat problem
Childhood-Onset Fluency Disorder - Definition
Problems with time-patterning of speech. Usually shown via repeated + prolonged pronunciation of certain syllables that interfere with communication
Most commonly associated with stuttering
Stuttering
A type of speech disorder that causes interruptions in the flow of speech.
It can be mild-to-severe
Intra-speaker variation across speaking situations and over time.
Childhood-Onset Fluency Disorder - Diagnostic Criteria
Disturbance in normal fluency and time of patterning of speech that are inappropriate for child’s age/language skills + persist over time and marked in:
Sound/syllable repetitions
sound prolongations of consonants
broken words (e.g. pauses within a word)
etc…
Disturbance causes anxiety about speaking + limitations in effective speech
Onset of symptoms occurs in early developmental period
Disturbance NOT ATTRIBUTABLE to speech-motor or sensory deficit
Childhood-Onset Fluency Disorder - Prevalence + Risk Factors
Prevalence -
80% of children who stutter < 5yo stop after 1 year of schooling
1% of people have COFD and prevalence peaks at 5 yo
Risk Factors -
Genetics
Environmental Factors (less of a cause)
Social Pragmatic Communication Disorder - Definition
Problems with the social use of language and communication.
Difficulties involve both expressive/receptive skills -
being able to adapt one’s communication to social context (receptive)
being able to understand the nuances and meanings expressed by others (expressive)
Social Pragmatic Communication Disorder - Diagnostic Criteria
Persistent Difficulties across four areas:
Deficits in using communication for social purposes (e.g. greeting/sharing information appropriately)
Difficulties following rules of language, such as conversation-taking
Difficulties in understand what someone is not explicitly saying (making inferences) and making out meaning during ambiguous speech (e.g., thinking “break a leg” actually means to break your leg during your audition)
What is Pragmatics in Language?
The use of language in context, and the context-dependence of various aspects of interpreting speech.
Social Pragmatic Communication Disorder - Prevalence + Risk Factors
Prevalence -
Onset = diagnoses occurs AFTER 4-5 YO. More subtle forms diagnosed in adolescence (10+)
Can have lasting negative impact on interpersonal relationships, behaviors and related skills
Risk Factors -
Family history of ASD/Communication Disorder/Specific Learning Disability
Prenatal medication exposure (questionable)
How are Communication Disorders different from the following disorders: ASD, ID, LD, and Selective Mutism
While communication deficits are present in ASD, ID, LG and SM, each has a distinct characteristic(s) that set them apart from Comm. Disorders.
ASD includes challenges in social interactions and repetitive behaviors.
ID affects communication proportionally to other effected cognitive/developmental pathways.
LD, such as dyslexia, impact academic skills which can include language processing, but this effect is broad.
SM involved anxiety-related inability to speak in certain social contexts, despite normal language abilities in comfortable environments.
Comm. Disorders overall relate to language deficits and challenges are primarily marked by language challenges (instead of broadly)
Name the communication disorder: Allison has difficulty understanding directions, struggles to express her thoughts, and uses short, disjointed sentences.
LANGUAGE DISORDER
trouble understanding directions + difficulty expressing thoughts (disorganized speech) are characteristics of Language disorders
Name the communication disorder: Josh struggles with writing, understanding humor or satire, topic shifting, and maintaining appropriate volume in class.
SOCIAL PRAGMATIC COMMUNICATION DISORDER
Difficulties understanding humor/satire, changing topics randomly and not managing volume aligns with SPCD
Name the communication disorder: Max is difficult to understand due to sound substitution and mispronunciations like “miwk” for milk.
SPEECH SOUND DISORDER
Challenges with sound substitution + mispronunciations (“milk” → /miwk/) point to SSD. This disorder involves problems with articulation or phonological processes
Name the communication disorder: Lydia avoids reading aloud due to stilted speech and has experienced teasing about stuttering.
CHILDHOOD-ONSET FLUENCY DISORDER (stuttering)
Stilted speech (disruption in speech flow) + avoidance of reading aloud (anxiety) point to COFD
Treatment for Communication Disorders
Response-Contingency Therapy - technique that involves providing different responses based on whether the person responds in a fluent way or not.
If the child responds FLUENTLY, they are given positive reinforcement (toys, more game time, etc.)
If the child responds NON-FLUENTLY, give corrected feedback
Attention Deficit Hyperactivity Disorder (ADHD)
Neurodevelopmental Disorder that causes difference in brain that effects:
Attention (inattention)
Behavior
Activity Levels (hyperactivity)
Cognitive Control (impulsivity)
Attention Deficiency Hyperactivity Disorder (ADHD) - Diagnostic Criteria
Persistent pattern of inattention that impedes on daily function. Criteria includes (6+ present for 6+ months):
Makes careless mistakes
Difficulty sustaining attention
Easily distracted
Often loses things
Often forgetful
Avoids/dislikes activities requiring sustained mental effort
Fails to follow through on instructions
does not listen even when being directly spoken to
Persistent Pattern of hyperactivity-impulsivity that impedes on daily function. Criteria includes (6+ behaviors for 6+ months):
Hyperactivity
Fidgets/squirms in seat
leaves seat where staying seated is expected
runs around/climbs excessively
has difficulty playing quietly
Talks excessively
Impulsivity
Blurts out answers before questions have been completed
Has difficulty awaiting turn
Interrupts Others
These impairments occur in two+ settings (e.g., school, extracurriculars, home, etc.)
Clear clinical evidence of significant impairment in functioning
Symptoms present before 12 YO
Attention Deficit/Hyperactivity Disorder - Subtypes of ADHD (“specifiers”)
Combined (ADHD-C) - has at least 6 inattentive + hyperactive/impulsive symptoms
Predominantly inattentive type (ADHD-PI) - 6 inattentive symptoms, but NOT 6 hyperactive/impulsive symptoms
Predominantly Hyperactive-impulsive type (ADHD-HI) - 6 hyperactive/impulsive symptoms, but NOT 6 inattentive symptoms
Executive Functioning
Cognitive processes in the brain that activate, integrate, and manage other brain functions (THINK: air-traffic control)
EF underlies a child’s ability for self-regulation functions (e.g., self-awareness, planning, monitoring, self-evaluation)
The 4 types of Executive Functions (used together in everyday life!)
Language processes - verbal fluency + use of self-directed speech
Cognitive processes - working memory (holds facts + mental manipulation), mental computation, planning, anticipation
Motor Processes - allocation of effort, following instruction
Emotional process - self-regulation + tolerating frustration
Executive Function (impairment) and Attention Deficit/Hyperactive disorder
What’s impaired | Results of Impairment:
Organize, prioritize, activate
trouble getting started
difficulty organizing work
misunderstand directions
Focus, shift + sustain attention
lose focus when trying to listen; forget what has been read
easily distracted
Regulate alertness, effort + processing speed
excessive daytime drowsiness
difficulty completing a task on time
slow processing speed
Manage frustration + modulate emotion
very easily irritated
feeling hurt easily
WM + accessing recall
forget to do planned task
difficulty following sequential directions
Monitor/regulate action
Find it hard to sit still/quiet
rush things/blurts out loud
Attention Deficiency/Hyperactive Disorder (ADHD) - Causes
Genetics - Dopamine D4 + D5 receptor genes; these receptors are distributed in cortical + limbic brain regions = ADHD seems to be related to disruption in dopamine signaling pathways
Perinatal Complications (questionable; might also predict comorbid aggression)
Parental Control (NO)
Attention Deficit/Hyperactive Disorder - Prevalence + Risk Factors
Prevalence -
11.4% (7M) US children 3-17 YO diagnosed with ADHD
Those diagnosed MORE likely to have combined/HI subtypes
Risk Factors -
Genetics - Dopamine D4 + D5 receptor genes; these receptors are distributed in cortical + limbic brain regions = ADHD seems to be related to disruption in dopamine signaling pathways
Perinatal Complications (questionable; might also predict comorbid aggression)
Parental Control (NO)
Sugar (NO)
Attention Deficit/Hyperactivity Disorder - Developmental Pathway
Infancy
high activity level
unpredictable
inconsolable (difficult “temperament”)
Toddler (1-3 YO)
“normal” toddlers may appear “hyper”
ADHD toddlers have frenzied quality to their movements
Randomly going from one activity to another
temper tantrums
Pre-school (3-5 YO)
restless
careless
demanding
defiant
Middle childhood (treatment implemented)
In-Classroom; ADHD symptoms visible
comorbid ODD/CD
Adolescence
continuance of childhood symptoms (70%)
hyperactive/impulsive symptoms may decline
school dropout/parent conflict begins
Adulthood
Higher risk for crime
substance abuse (if ADHD comorbid with CD)
Attention Deficient/Hyperactive Disorder - How to Diagnose
Observation (i.e., classroom, home, clinic)
measures hyperactivity (more likely in younger kids in structured situations)
Behavior Rating Scales (e.g., Child Behavior Checklist; CBCL)
completed by parents/teachers
if disagreements occur, you want to assess if informants have different interpretations of behaviors
Neuropsychological Evaluation - typically used to assess:
Attention - e.g., continuous performance task (CPT), Auditory attention Task
Impulsivity - e.g., Timed Draw a Circle Task
Hyperactivity - e.g., Observation of Behavior During Tasks
Assess Comorbid Disorders - symptoms of ADHD must present on their own and NOT PART of other conditions (e.g., schizophrenia; psychotic disorder; mental disorders
Treatment for ADHD (2 types)
Behavioral Treatments
Parent Training
Classroom Accommodations
Individual Therapy
Medication
Stimulants
Non-stimulants
Parent Training - Structure
Teaches parents how to manage their child’s behavior using positive reinforcement, structure and clear expectations:
Set consistent house rules/routine
Don’t say you’re going to do something unless you follow through (kids remember lies!)
Do homework at same time/place (stimulus control)
Use daily charts + point systems for both rewards/consequences
Use “when-then” directions (e.g., “when you do XXX, then you will get XXX”)
Parent Training - When to Reward Praise
Ignore DISRUPTIVE Behaviors
Attention to behavior is, in it of itself, reinforcement. Weaken response by ignoring (no reinforcement)
When behavior can’t be ignored, use PROPER “time-outs” (consequence)
Praise GOOD Behavior
Includes ALL improvements (no matter how small)
Use SUCCESSIVE APPROXIMATIONS (rewarding behavior that approximates desired behavior)
Praise incompatible behavior (“positive opposite”)
Use of behavior charts to make praise more salient

Behavior Chart (choosing a set of desired behaviors and rewarding stickers on days’ behavior is imitated)
Classroom Accommodations - How it Works
Seat child away from window/doors; sit within rows
Give instructions one at a time and repeat (when neccesary)
Allow students to have most challenging classes earlier in the day
Create worksheets/tests with fewer items (frequent quizzes rather than long tests)
Use of Daily Report Card/ Tracking System for Assignments
Individual Therapy - How it Works
Teach SOCIAL SKILLS
Help child solve social problems
Teach other skills that children find important (allows child to show initiative)
Increase child compliance with home behavior plans
Help form close friendship between child w/ ADHD with another child
NOTE: For therapy to work, parent + therapist + teacher will work on same goals so that child can practice skills in MULTIPLE SETTINGS
Medication for ADHD - Stimulants vs Non-Stimulants
Stimulants: common ADHD medications; increase dopamine levels in the brain, improving focus/reduce hyperactivity
Ritalin/Dexedrine/Adderall
Academy of Pediatric Guidelines diagnose stimulants as young as 4 YO
70-80% ADHD children get better
Child shows less impulsive/distractibility in classroom
better social skills
fewer auto-accidents
Non-Stimulants: used when stimulants are ineffective/cause side effects. Work slowly but help attention/impulse control
Medication - Ritalin (Stimulants)
Taking Ritalin typically results in fast/temporary improvements in performance
helps increase ability to:
pay attention
focus on activity
control behavior problems
organization
listening skills
Risk:
Nervousness
trouble sleeping
loss of appetite
Weight loss
Problems that May arise due to misuse of prescription stimulants (ADHD)
Misuse of medical stimulants can be a serious problem due to:
potential health risk (addiction, heart issues)
ethical concerns
legal implications (using controlled substances WITHOUT prescription)
Drug-dependence instead of proper development
Findings of NIMH (National Institute of Mental Health) Treatment Study on Treatments/Interventions for ADHD
Between Meds Only, Behavior Therapy Only, Meds + Therapy and Routine Care:
Meds Alone & Combined Treatment - more effective than Routine care/Behavior therapy alone
Combined Treatment - led to less dropout than Meds Alone + improvement of non-ADHD symptoms
Group differences lessened over time
How does comorbid diagnoses with ADHD impact proper diagnosis and treatment?
Comorbid conditions (anxiety, depression, LD, ODD) can make diagnosis treatment of ADHD:
HARDER to diagnose accurately, as symptoms may overlap/mask each other.
Complicates treatment, required more tailored approach to address both ADHD + co-occurring disorder
Necessity to use multiple intervention strategies (i.e., combination of medication, therapy and specific supports)
What other mental disorders has ADHD been linked to?
Anxiety Disorders
Learning Disorders (LD)
Oppositional Defiant Disorder (ODD)
Conduct Disorder (CD)
ASD
Speech and Language Impairment
Sleep and ADHD
25-55% of individuals with ADHD report having sleep disturbance
Relationship between Sleep/ADHD is COMPLEX:
Problems w/ sleep can arise due to symptoms of ADHD
Problems with sleep ALSO leads to development of ADHD/ADHD-like symptoms
Comorbidity of sleep disorder symptoms and ADHD
Children with disrupted sleep show less executive control, irritation, impulsivity, distractibility and emotional dysregulated.
These symptoms are easily confused with ADHD, resulting in misdiagnosis if the patient is monitored for a short time.
Eating Disorder - Definition
Mental disorder, defined by abnormal eating behaviors that adversely affect a person’s physical mental health
Eating Disorder - Prevalence
Global Eating Disorder - increased by 4% from 2000-2018
9% (28.8M) of the U.S. population suffer from eating disorder
Eating Disorder - Developmental Stages
Infancy/Childhood:
Pica
Ruminative Disorder
Avoidant Restrictive Food intake Disorder (ARFID)
Adolescence/Adulthood
Anorexia Nervosa
Bulimia Nervosa
Binge Eating Disorder
Types of Eating Disorders Prevalent in Infancy/Childhood
Pica
Ruminative Disorder
Avoidant/Restrictive Food Intake Disorder
Pica - Defintion
Persistent eating of nonfood, non-nutritive substances over a period of at least ONE MONTH
Common among younger children
Can be life-threatening if continued
Associated with ID and certain chronic medical conditions (e.g., sickle cell)
Pica - Causes
Etiology:
Low environmental stimulation
poor parental supervision
vitamin deficiencies
Other mental disorders (e.g., Autism, OCD)
Pica - Treatment
Treatments focus on BEHAVIORAL STRATEGIES
Remove/Block access to dangerous substances
Redirection to a preferred activity
reinforcing incompatible behavior (positive opposite)
Monitor child’s lead levels
Rumination Disorder - Definition
Automatic regurgitation (throwing up) of previously eaten food, re-chewing, and either swallowing it again/spitting it out
Rumination Disorder - Causes and Treatment
Etiology:
generally develops in early childhood
common among children with ID
Cause by self-stimulation/Stress (?)
Treatment
Behavioral strategies
habit reversal - working with individual in becoming aware of triggers and REPLACING them with alternative responses
Overcorrection - intervention strategy used to teach individuals appropriate behaviors by providing additional opportunities to practice correct responses
Avoidant/Restrictive Food Intake Disorder (ARFID) - definition
Disorder characterized by avoidance/restriction of food intake
Usually leads to significant weight loss/failure to maintain normal growth
Avoidant/Restrictive Food Intake Disorder (ARFID) - Etiology
Etiology is multifactorial:
Biological
Medical
Psychological
Environmental Factors
History of the following:
Vomiting
food allergies
Gastrointestinal difficulties
Avoidant/Restrictive Food Intake Disorder (ARFID) - characterisitcs
Weight loss
Significant nutritional deficiency
Dependence on enteral feeding (feeding tube) OR oral nutritional supplements
difficulties in psychosocial functioning
Avoidant/Restrictive Food Intake Disorder (ARFID) - Developmental Trajectories
Picky Eating - common among younger children (via parent self-report)
If the onset of Picky eating occurs during < 2yo, this can have serious developmental consequences
societal norms + media focus on thinness especially among different gender groups have exacerbated poor eating habits among children
Eating disorders normally found among adolescents and adulthood
Anorexia Nervosa
Bulimia Nervosa
Binge Eating Disorder
Anorexia Nervosa - Definition
Characterized by:
Refusal to maintain minimally normal body weight
Intense fear of gaining weight
Significant disturbance in perception/experiences of body size
Anorexia Nervosa - subtypes
DSM-V identifies TWO specific subtypes of Anorexia Nervosa:
Restricting Type - individual wants to lose weight through diet, fasting or excessive exercise
Binge eating/purging type - individual regularly engages in episodes of binge-eating, purging, or both
Bulimia Nervosa - Definition/Diagnostic Criteria
Characterized by:
Recurrent episodes of binge-eating and associated purging for at least 1 a week for 3 months
eating an amount of food that is LARGER than what most individuals would eat in a similar period of time
A sense of lack of control during eating
Recurrent inappropriate compensatory behavior in order to prevent weight gain (purging)
Purging
Recurrent and inappropriate compensatory behaviors (e.g., throwing up recently eaten food)
Binge
An episode of overeating that normally involves:
eating an objectively large amount of food
lack of control over what/how much is eaten
Compensatory Behaviors
Intended to prevent weight gain following a binge episode, and this can include behaviors like:
Self-induced vomiting
fasting
misuse of diuretics/diet pills
Binge Eating Disorder
Similar to Bulimia Nervosa Disorder, only it does not involve “compensatory behaviors”, such as throwing up or excessive exercising
Treatment for Anorexia Nervosa
Inpatient Treatment - severe AN patients receive 24-hour care in a hospital/treatment center
Family-based treatment - parents help their child restore healthy eating relationships via empowering/positive reinforcement
Adolescent Focused Therapy -individual therapy designed to help teens with AN learn to emotionally regulate
Less response to treatment
Treatment for Bulimia & Binge Eating Disorder
Nutrition planning/consultation
Cognitive Behavioral Therapy - helps individuals identify and challenge negative thought patterns and unhealthy behaviors around eating
Interpersonal Therapy
Appetite Awareness
Name That Disorder: LJ has a history of defiant, angry, and manipulative behavior, including disobeying rules, losing his temper, and blaming others. He often deliberately annoys people and gets into arguments with adults.
Oppositional Defiant Disorder (ODD)
LJ shows a consistent pattern of defiance, anger and irritability. He deliberately annoys others, loses his temper and blames other's for his actions.
Name That Disorder: Mackenzie has a history of stealing, lying, running away, and harming others, including setting a fire and showing no remorse for her actions.
Conduct Disorder (CD)
Mackenzie exhibits a pattern of serious rule violations (stealing, breaking/entering, running away, etc.). She is also physical aggressive, destroys property, and is very deceitful.
Characteristics of Disruptive, Impulse-Control and Conduct Disorders
These disorders are characterized by problems with self-control of emotions and behaviors
Problems manifest through behaviors that violate the rights of others and/or conflict with norms/figures
Types of Disruptive, Impulse-Control and Conduct Disorders
Intermittent Explosive Disorders - sudden, intense outburst of anger/aggression that is disproportionate to situation
Opposition Defiant Disorder (ODD) - persistent, pattern of angry, defiant and vindictive behavior toward authority figures
Conduct Disorder (CD) - pattern of violating societal rules and rights of others through aggression, deceitfulness or destructive behavior
Pyromania - compulsive urge to deliberately set fires for pleasure
Kleptomania - recurrent inability to resist urge to steal
Antisocial Personality Disorder - involves chronic pattern of disregarding the rights of others
Among the disruptive, Impulse-control and conduct disorders, which are more likely to appear in childhood?
Opposition Defiant Disorder (ODD) and Conduct Disorder (CD) are more likely to manifest and be diagnoses in childhood
Opposition Defiant Disorder (ODD) - Definition
Characterized by patterns of angry, defiant or vindictive behavior towards authority figures.
Children with ODD show patterns of being uncooperative, defiant and hostile towards peers, parents, teachers and other authority figures
Opposition Defiant Disorder - Diagnostic Criteria
A. 4+ of symptoms that fall under 3 categories (must persist for 6+ months):
Angry/Irritable Mood
Loses temper
sensitive/easy to annoy
angry or resentful
Argumentative/Defiant Behavior
Often argues with authority figures
Actively defies/refuses to comply with request from authority figures
Vindictiveness
spiteful or vindictive (for at least 2x in 6 months)
B. The disturbance in behavior is associated with distress in individual/others in child’s immediate social context.
C. Behavior DOES NOT OCCUR with other disorders (e.g., psychotic, substance-use, depression or bipolar disorder)
Opposition Defiant Disorder (ODD) - Prevalence and Risk Factors
Prevalence
3.3% of children (5-17 YO) in US have ODD
More common in males 4:1
Risk Factors
comorbid with internalizing disorders (anxiety/depression)
Negative emotions experienced in ODD can be expressed as internalized distress
Conduct Disorder (CD) - Definition
Children who display persistent pattern of aggressive and anti-social acts such as inflicting pain on others or interfering in the rights of others through physical/verbal aggression, stealing or vandalism
Conduct Disorder (CD) - Diagnostic Criteria
A. Repetitive pattern of behavior that violates the basic rights of others/societal norms. Manifest as 3+ symptoms from any of the 4 categories:
Aggression to People/Animals
often bullies or threatens others
Initiates physical fights
Use of weapon that can cause serious physical harm to others
physically cruel to people/animals
Destruction of Property
Deliberately plays with fire
Deliberately destroys other’s property
Deceitfulness or Theft
Broken into someone’s property
lies to obtain goods/favors OR avoid obligations
Serious Violations of Rules
Stays out at night despite parental prohibition (< 13 YO)
B. Disturbance of behavior causes clinically significant impairment in social/academic/occupational functioning
C. If > 18 YO, must not be comorbid with antisocial personality disorder
Conduct Disorder (CD) - Prevalence and Risk Factors
Prevalence
4% of children age 5-17 YO
More common in males
Risk Factors
Comorbid with substance use
Subtypes of Conduct Disorder (CD)
Childhood-Onset CD
Diagnosed for children age < 10 years old
Displays of aggression during early childhood
More common in males
Disturbed Peer relationships
If COCD develops, more likely for CD to persistent in adulthood
More likely to have “callous-unemotional traits”
Adolescent-onset CD
Less likely to be emotionally aggressive
No differences among gender
More normative peer relationships
Less likely to have CD in adulthood
Gender Differences in Onset/Diagnosis of Conduct Disorder
Developmental Trajectory via Gender reveal:
Preschool - gender differences are NONEXISTENT
School-aged - CD/(ODD) 2-3:1 to be diagnosed in boys
Adolescence - 2:1, gap closes between boys and girls due to increase rates of diagnosis
Reactive Aggression
Impulsive, defensive RESPONSES to a real/perceived threat
Occurs due to tendency to believe that neutral/ambiguous reactions from peers are actually hostile
Proactive Aggression
PLANNED, goal-directed behavior design to achieve an objective by provoking aggression
Usually premeditated/planned
occurs due to delinquency and alcohol abuse in adolescence (criminality in adulthood)
Causes of ODD + CD (Disruptive, Impulse-Control and Conduct Disorders)
2 theories of etiology of ODD + CD
Biosocial Theory
Vile Weed Theory
Biosocial Theory (Moffitt, 1993)
Suggest that ODD/CD (antisocial behaviors) arise from complex interaction of different biosocial factors. These interactions manifest as either:
ADOLESCENT-limited Antisocial Behavior (AL)
antisocial behaviors that are restricted to adolescent years
CD/ODD caused AND maintained by imitating delinquent peers + reinforcement from peers
LIFE-COURSE persistent antisocial behavior (LCP)
Antisocial behavior emerges in early childhood and PERSIST into adulthood
Throughout development, CD/ODD symptoms/behaviors persist (not as common!)
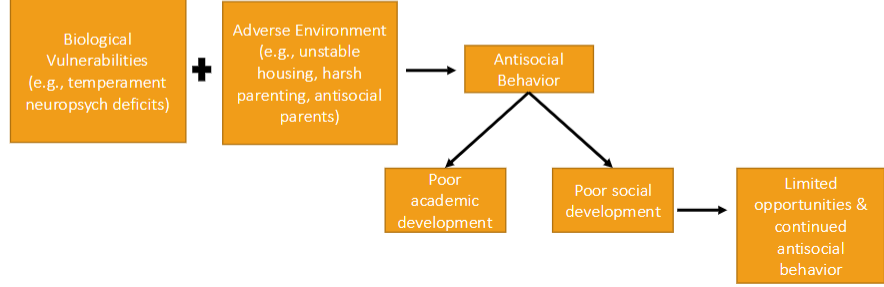
Time course of Life-Course persistent antisocial behavior
Vile Weed Theory (Patterson)
CD/ODD gets WORSE and MORE INTRACTABLE (cannot be reversed) over time.
This is similar to the growth of a weed
Causes of CD/ODD Explained by the Vile Weed Theory
Theory explains that CD/ODD are rooted in
Ineffective parenting
Poor parental monitoring/poor supervision
Poor discipline
Parents modeling coercive behavior to their children (e.g., “I won’t love you if you do X”)
4 Developmental Stages according to the Vile Weed Theory
Preschool (Stage 1) - Child learns negative behaviors by observing parents (negative modeling)
School Age (Stage 2) - Negative behaviors lead to social rejection, reinforcing antisocial patterns
Adolescence (Stage 3) - Child associates with deviant peers, exacerbated negative behaviors w/ lack of supervision
Adulthood (Stage 4) - Antisocial behaviors are engrained, leading to chronic deviant behaviors.
Psychopathy
Interpersonal Style characterized by persistent antisocial behavior, selfishness, lack of remorse, impulsivity and callous/emotional traits
Interpersonal Style
Person’s typical behaviors when interacting with others
Examples of “callous” or “unemotional” traits displayed in psychopathy
lacking guilt
no empathy
shallow emotions
charming/insincere