med surg II exam 3: cardiovascular, immune, gastrointestinal, STI/HIV, hepatic
1/127
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
128 Terms
right side of heart pumps blood to
pulmonary system
left side of heart pumps blood to
rest of body
flow of blood
vena cava -> R atrium -> tricuspid valve -> R ventricle -> pulmonary arteries -> lungs -> pulmonary veins -> L atrium -> mitral valve -> L ventricle -> aorta -> body
S1 (lub)
- closure of mitral and tricuspid valves
- start of systole
S2 (dub)
- closure of aortic and pulmonic valves
- end of systole
how does an increased HR affect perfusion in heart
coronary arteries perfuse heart during diastole, so as HR inc, diastolic time dec and there is not enough time for myocardial perfusion
cardiac electrophysiology
SA node -> AV node -> bundle of his -> right and left bundle branches -> purkinje fibers
depolarization
activation of cell caused by influx of Na into cell while K exits cell
repolarization
return of cell to resting state caused by reentry of K into cell while Na exits
refractory periods
- effective: cells incapable of depolarizing
- relative: cells need stronger than normal stimulus to depolarize
cardiac output
total blood ejected by a ventricle in L/min
- 4-6 L/min (SVxHR)
stroke volume is determined by
preload, afterload, contractility
ejection fraction
amount of blood the heart pumps
- L ventricle: 55-65%
- if perfusion decreases the body does not have enough blood or O2 (SOB, pallor, fatigue)
mean arterial pressure
perfusion
- above 65% is good perfusion
coronary artery disease
- symptoms caused by myocardial ischemia
- symptoms related to location and degree of vessel obstruction
- most common symptom: angina pectoris
- other symptoms: epigastric distress, pain that radiates to jaw/left arm, SOB
- women often have atypical symptoms like no pain resulting in more deaths than men
angina pectoris
- episodes/paroxysomal pain/pressure in anterior chest caused by insufficient coronary blood flow
- physical exertion/emotional stress increases O2 demand -> vessels unable to meet demands
- ask about location, quality, quantity, radiation, severity, symptoms, timing
- stable: pain stops when exertion stops
- unstable: nothing makes the pain stop
gerontologic considerations with CAD
- diminished pain with aging affect presentation -> silent CAD
- teach to recognize chest pain-like symptoms (weakness)
- pharmacologic stress testing
- cardiac catheterization
- use meds cautiously (toxicity)
interventions for CAD
- treat angina
- patient is to stop all activity, sit or rest in bed
- assess during interventions: VS, respiratory distress, pain, ECG
- administer meds as ordered usually NGT, reassess pain, give NGT up to 3 doses Q 5 min (check HR and BP before each time, wear gloves)
- administer O2 2L/min by nasal cannula
myocardial infarction
- emergent situation
- acute onset of myocardial ischemia that results in myocardial death if interventions do not occur promptly
- assess: pain, symptoms/activities preceding and precipitating attacks, ECG studies
- risk factors: obesity, smoking, HDL, alcohol, men, age, HTN
- elevation in ST segment in 2 continuous leads, cardiac enzymes, troponin, creatine kinase, myoglobin
medical management of MI
- nitrates, beta adrenergic blockers, calcium channel blockers, antiplatelets
- PCI: cardiac catheterization, percutaneous coronary intervention, coronary artery stent
- surgical intervention: coronary artery bypass graft (CABG)
- MONA : morphine, oxygen, nitrates, aspirin
interventions for MI
- relieve pain and sxs of ischemia
- improve respiratory function
- promote adequate tissue perfusion
- reduce anxiety
- monitor and manage complications
- educate patient and family
- provide continuing care
valvular disease types
- mitral regurgitation
- mitral stenosis
- aortic regurgitation
- aortic stenosis
management for valvular diseases
1. nursing
- patient education
- monitor VS trends, for complications: HF, dysrhythmias, dizziness, syncope
- medication schedule, monitor for weight gain, plan activity with rest periods, sleep with HOB elevated
2. medical
- valvuloplasty: commissurotomy, balloon valvuloplasty, annuloplasty, leaflet repair, chodoplasty
- valve replacement: mechanical, tissue, bioprosthesis, hemografts, autografts
types of infectious disease related to valvular disease
- rheumatic endocarditis: most often in school aged after group A beta hemolytic streptococcal pharyngitis, need to promptly recognize and treat strep throat to prevent rheumatic fever
- infective endocarditis: people with prosthetic heart valves or structural cardiac defects, IV drug abusers and those with debilitating diseases, indwelling catheters, or prolonged IV therapy
- pericarditis: inflammation of pericardium, many causes, may cause pericardial effusion and cardiac tamponade
- myocarditis: inflammation of myocardium, viral pathogens most common but in endocarditis they're bacterial, may cause cardiomyopathy and HF
clinical presentation of valvular diseases
- fever
- heart murmur with pericarditis
- osler nodes (rheumatic)
- cardiomegaly
- heart failure
- splenomegaly
- fatigue
- syncope
- chest pain (myocarditis)
heart failure
- risk factors: HTN, CAD, cardiomyopathy, valvular disease, congenital defects, diabetes, smoking, family hx, lung disease, hyperthyroidism
- diagnostics: imaging (CXR, vascular engorement, cardiomegaly, pleural effusion), echocardiogram is best tool, ECG, stress testing, cardiac catheterization
- management: meds, IV infusion of inotropic and nutritional therapy
- assess: mental status, lung sounds, heart sounds, fluid status/overload, daily weight, I&Os, meds
brain natriuretic peptide (BNP) test
- gold standard for managing HF
- < 100 normal
- 100-299 suggest HF present
- 300-599 mild HF
- 600-899 moderate HF
- >900 severe HF
left sided HF
- pulmonary congestion, crackles, cough, wheezes
- S3 or ventricular gallop
- dyspnea on exertion (DOE)
- low O2 sat
- tachycardia
- cyanosis
- confusion
- dry nonproductive cough initially
- oliguria
- restlessness
right sided HF
- viscera and peripheral congestion
- JVD
- dependent edema
- hepatomegaly
- ascites
- weight gain (3 lbs/24 hr; 5 lbs/1 wk)
heart failure diagnoses
- activity intolerance RT decreased CO
- excess fluid volume RT heart failure syndrome
- anxiety type symptoms RT complex regimen
- powerlessness RT chronic illness, hospitalizations
- ineffective family therapeutic regimen management
- activity intolerance: bed rest for acute exacerbation, regular physical activity daily (30-45 min), exercise training, pacing of activities, wait 3 hrs post eating, avoid extreme heat/cold/humidity, modify to conserve energy, elevate HOB, support of arms
- patient education: meds, low sodium diet, fluid restriction, exercise, activity program, stress management, prevent infection, monitor for excess fluid and hypotension
medications for heart failure
- ACE inhibitors: vasodilation, diuresis, decrease afterload, monitor for hypotension, hyperkalemia, renal function, cough
- angiotensin II receptor blockers:
- hydralazine and isosorbide dinitrate
- beta blockers: in addition to ACE inhibitors, takes weeks to see effects, caution in patients with asthma
- diuretics: decrease fluid volume, monitor electrolytes
- digitalis: digoxin, improves contractility, monitor for toxicity especially of hypokalemic, monitor HR
IV meds (acute decompensated HF)
- milrinone: decrease preload and afterload, cause hypotension, increases risk of dysrhythmias
- dobutamine: used for patients with left ventricular dysfunction, increase cardiac contractility and renal perfusion
gerontologic considerations with heart failure
stiffening of vessels results in increased peripheral resistance, impaired blood flow and increased left ventricular workload
hypertension is known as the
silent killer
primary hypertension
- essential and unidentified cause
- atherosclerotic cardiovascular disease, dyslipidemia, sedentary lifestyle, obesity, diabetes, family hx, smoking, african american, poor diet, alcohol
secondary hypertension
- defined cause
- CKD, renal artery stenosis, hyperaldosteronism, pregnancy, peripheral artery disease
hypertension
- assess: hx, PE (retinal), labs, UA, blood chemistry, ECG, echocardiogram, risk factors, organ damage
- management: keep BP under 140/90, weight reduction, physical activity, meds, reduce alcohol
- interventions: educate meds, lifestyle changes, monitor BP, follow-ups, education and support are key
hypertensive crisis emergency
- reduce BP 20-35% in first hr
- reduce to 160/100 over 6 hrs
- gradual reduction to normal over days
- exceptions are ischemic stroke and aortic dissection
- IV vasodilators: sodium nitroprusside, nicardipine, fenoldopam, mesylate, enalaprilat, nitroglycerin
- need very frequent monitoring of BP and cardiovascular status
hypertensive crisis urgency
- oral agents can be administered with goal of normalizing BP within 24-48 hrs
- fast acting oral agents: beta blocker (labetalol), ACE inhibitor (catopril), alpha 2 agonist (clonidine)
- close monitoring of BP and cardiovascular status
- assess for potential evidence of target organ damage
arterial disorders types
- arteriosclerosis
- atherosclerosis
- peripheral artery occlusive disease
- upper extremity arterial occlusive disease
- aneurysms (thoracic, abdominal)
- arterial embolism and thrombosis
- raynaud phenomenon and other acrosyndromes
arteriosclerosis
hardening of artery, muscle fibers and endothelial lining of walls become thickened
atherosclerosis
accumulation of lipids, calcium, blood components, carbohydrates, fibrous tissue in intimal layer, atheromas/plaques
risk factors for atherosclerosis and PVD
- modifiable: nicotine, diet, HTN, diabetes, obesity, stress, sedentary lifestyle, c-reactive protein, hyperhomocysteinemia
- nonmodifiable: age, gender, familial predisposition, genetics
arterial disorders
- 5P's: pain, pallor, peripheral temp, peripheral circulation, pulses
- assess: hx, meds, risk factors, sxs of arterial insufficiency, claudication, rest pain, color changes, weak or absent pulses, skin changes/breakdown
- diagnosis: doppler ultrasound, ankle brachial index, duplex ultrasonography, treadmill
- management: antiplatelet, stent placement, bypass graft, lifestyle changes, statins
- interventions: exercise/activities (walking), positioning (elevate legs for PVD not PAD), temperature, stop smoking, stress reduction
aneurysms
- localized sac/dilation formed at weak point in artery wall
- classified by shape or form (most common is sacular and fusiform)
- management: BP meds (goal is to be hypotensive), endovascular repair, open surgical repair
- keep supine, VS monitoring (bleeding dec BP and inc HR), site assessment (rigidity, distention), renal output, movement of extremities
venous disorder types
- venous thromboembolism
- chronic venous insufficiency/post thrombotic syndrome
- leg ulcers
- varicose veins
venous thromboembolism
- endolthelial damage: venous stasis, altered coagulation
- sxs: deep veins, superficial veins
- complications: chronic venous occlusion, pulmonary emboli, valvular destruction, chronic venous insufficiency, increased venous pressure, varicosities, venous ulcers
- venous obstruction: increased distal pressure, fluid status, edema (1 leg), venous gangrene
- assess 5Ps, elevate legs, ambulate, pain control
- meds: unfractioned heparin, lovenox, warfarin, eliquis
- prevention: apply graduated compression stockings, pneumatic compression devices, early ambulation, subQ heparin or LMWH, lifestyle changes (weight loss, smoking, exercise)
leg ulcer
- assess: hx, pain, pulses, edema, infection, nutrition
- management: anti-infective therapy depends on agent (oral antibiotic common), compression therapy, dressings, debridement of wound
- interventions: skin integrity, improve mobility, nutrition, home and community based care, cleansing wound, positioning, avoid trauma, avoid heat sources
- nutrition: protein, vitamin C and A, iron, zinc
- many with PVD are older adults and anemic
systole
mechanical contraction, depolarization
diastole
mechanical relaxation, repolarization
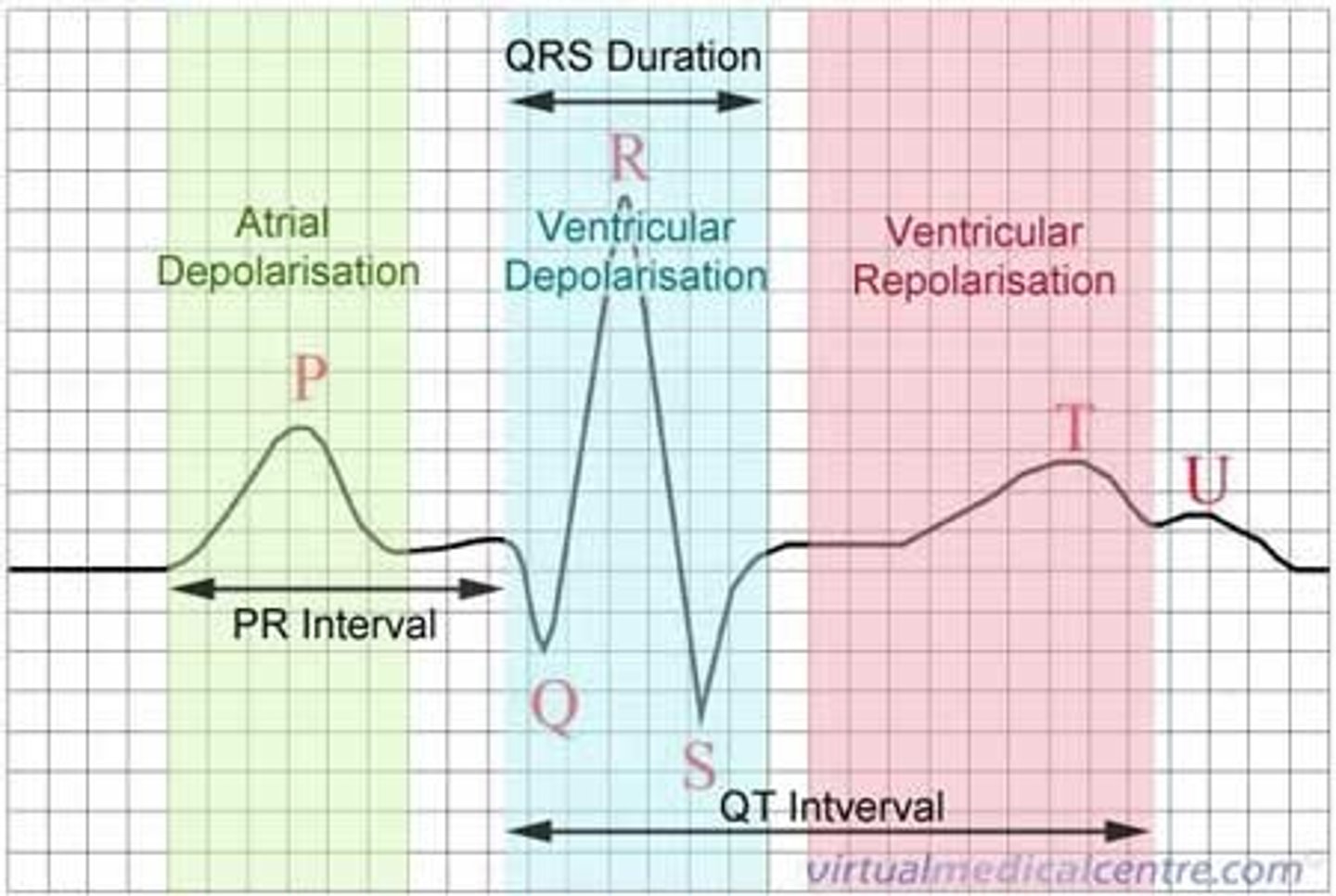
components of an ECG
- p wave: atrial depolarization
- QRS: ventricular depolarization (0.6-0.12 s)
- PR interval: 0.12-0.20 s (3-5 squares)
- T wave: ventricular repolarization
- ST segment: flat, isoelectric portion
cardiac electrolytes
- sodium: action potential
- potassium: hyper (decreased conduction, life threatening), hypo (myocardial hyperexcitability)
- calcium: hyper (blocks conduction pathways), hypo (decreased contraction)
- magnesium: hyper (delayed impulse conduction), hypo (irregular ventricular contraction)
calculating HR
1. count R waves and multiply by 10
2. find R wave on heavy black line and label the next 6 lines: 300, 150, 100, 75, 60, 50
normal sinus rhythm
- HR 60-100 bpm
- P wave for every QRS complex
- all QRS complexes similar in shape and size (<0.12 s)
- PR interval normal (0.12-0.20)
dysrhythmias
- disorder of impulse formation/conduction in heart
- can alter HR, rhythm
- can alter blood flow, hemodynamic changes
steps to identifying rhythms
1. it is regular
2. determine rate
3. is there a P wave before every QRS complex
4. determine PR interval
5. identify QRS shape consistency
6. identify rhythm
sinus bradycardia
- regular rhythm
- < 60 bpm
- P wave is present
- normal PR interval
- causes: athletic heart, hyperkalemia, hypothyroidism, increased ICP, increased vagal stimulation, inferior wall MI, meds
- possibly asymptomatic, hypotension, light headed, CP, SOB, LOC
- no symptoms = no treatment, monitor
- symptoms = administer O2, treat cause, atropine, transcutaneous pacing
sinus tachycardia
- regular rhythm, rate > 100 bpm less than 150, p wave present, PR interval normal
- causes: stress, caffeine, shock, HF, anxiety, pain, hyperthyroidism, meds
- CP, palpitations, hypotension, anxiety, cool/clammy skin
- asymptomatic = treat cause
- vagal maneuvers, adenosine, beta blockers
- unstable: synchronized cardioversion, follow ups
premature atrial complex (PAC)
- irregular rhythm, rate varies (extra beat), PRI normal, P wave is early and different with others normal
- causes: over 50, alcohol, nicotine, fatigue, infection, hypokalemia, heart disease, can lead to arrhythmias
- usually no symptoms, palpitations, skipped beats
- usually no treatment necessary, treat cause
atrial fibrillation
- irregular rhythm, atrial rate 300-600, ventricular rate may be normal or over 100 (uncontrolled)
- no discernible P wave, fibrillatory waves, PRI unmeasurable
- caused by pre-existing conditions
- may be asymptomatic, SOB, hypotension, fatigue, palpitation, light-headed
- treatment: rate and rhythm control
atrial flutter
- atrial rhythm regular, rate 250-400 ; ventricular rhythm regular or irregular, rate varies
- p waves saw tooth shape, flutter waves, PRI unmeasurable
- causes: HF, hyperthyroidism, ETOH, MI, COPD
- assess: CP, SOB, hypotension
- treatment: vagal maneuvers if stable, adenosine, anticoagulation, rate control, cardioversion
supraventricular tachycardia (SVT)
- regular rhythm can be sudden burst, atrial rate 150-200, ventricular rate 120-200, p wave and PRI unmeasurable
- palpitations, CP, weakness, SOC, fatigue, nervousness, hypotension, syncope
- may resolve on its own, vagal maneuvers
- if unstable immediate cardioversion
- antiarrhythmics: adenosine, amiodarone, cardiac ablation
premature ventricular complex (PVC)
- irregular rhythm, rate varies (extra beat), P wave depends of QRS timing others normal, PRI normal
- cause: caffeine, tobacco, ETOH, digoxin toxicity, electrolyte imbalance, MI, hypoxia
- usually no symptoms, palpitations, sxs of decreased CO if frequent
- treat cause, meds for symptoms
- unifocal: arise from single focus, PVCs identical
- multifocal: arise from multiple foci, diff QRS morphologies
ventricular tachycardia
- regular rhythm, ventricular rate 100-200, p wave and PRI unmeasurable
- cause: similar to PVC, MI, ischemia, HF, electrolyte imbalance, cocaine, digoxin toxicity
- palpitations, dizziness, lightheaded, SOB, CP, near fainting, syncope, weak pulse (cardioversion) or no pulse (CPR, defibrillate)
- oral antiarrhythmic drugs: beta blockers (metoprolol, esmolol, propranolol), IV meds (amidarone, procainamide, lidocaine)
ventricular fibrillation
- irregular rhythm, ventricular rate over 300, no p wave, PRI unmeasurable
- cause: MI, ischemia, untreated v tach, acid base and electrolyte imbalance, hypoxia
- no pulse or respirations
- early defibrillation, CPR, O2, and Epi
asystole
- no rate, no p wave, no PRI
- cause: MI, electrolyte imbalance, massive PE, electric shock
- unresponsive, no pulse, apnea
- CPR, H's and T's, Epi
- defibrillation not possible
H's and T's
- hypovolemia, hypoxia, hydrogen ion (acidosis), hypo/hyperkalemia, hypoglycemia, hypothermia
- toxins, tamponade, tension pneumothorax, thrombosis, trauma
first degree AV block
- rhythm usually regular, rate varies
- p wave normal, PRI over 0.2 s
- cause: MI, digoxin, beta blockers, hypothermia
- may be normal/temporary, asymptomatic
- least dangerous AV block, monitor, treat cause
second degree AV block type 1 (wenckebach)
- atrial rhythm regular, ventricular rhythm irregular
- rate: ventricular < atrial
- p wave normal, PRI becomes longer until p wave not followed by QRS
- cause: CAD, MI, ischemia, cardiac meds, inc vagal stimulation
- can be asymptomatic, assess for tolerance of rhythm
- usually temporary, resolves when underlying condition is corrected, monitor progression
- symptomatic: atropine, pacemaker
second degree AV block type 2
- atrial rhythm regular, ventricular rhythm irregular
- rate: ventricular < atrial
- p wave regular and constant, PRI varies
- cause: MI, CAD
- assess syncope, palpitations, CP, light headedness, hypotension, slow irregular pulse
- asymptomatic: monitor
- symptoms: meds, transcutaneous pacing
third degree AV block
- regular rhythm, rate ventricular < atrial
- p wave regular can be hidden in QRS/t wave, PRI varies
- cause: congenital, CAD, MI, digoxin toxicity
- potentially life threatening, significant symptoms, decrease CO
- treatment: pacemaker, epi, dopamine, minimize exertion
myocardial infarction - ST elevation
- assess: CP unrelieved with rest (unstable), diaphoresis, nausea, anxiety, SOB, palpitations, elevated troponin
- treat: MONA, cardiac catheterization, rest, cardiologist
paced rhythms
- temporary or permanent
- able to set rate
- failure to capture
notice spikes on ECG strip:
- before p wave: atrial paced
- before QRS: ventricular paced
- before both: AV paced or dual
systemic lupus (SLE)
- autoimmune disease: body attacks healthy tissue leading to inflammation and damage in multiple organs, includes flares
- risk factors: cigarette smoke, UV rays, meds, viral infections, emotional stress, physical body stress
- assess: pleural effusions, heart problems, lupus nephritis, arthritis, raynaud's phenomenon, butterfly rash
- diagnostic: antinuclear antibodies, CBC, metabolic panel, biopsy
SLE treatment/management
- treat based on symptoms goal is to manage symptoms, prevent/limit/stop flares, maintain lowest level of disease activity, if possible achieve complete remission, prevent/slow organ damage, improve quality of life
- Dx: fatigue, impaired skin integrity, body image disturbance, lack of knowledge for self management decisions
- educate: routine periodic screenings, health promotion activities, dietary consultation, compliance to meds
nutritional lab assessments
- hemoglobin: decreased -> anemia
- hematocrit: decreased -> anemia, increased -> dehydration
- albumin: decreased -> malnutrition (protein depletion), malabsorption
- prealbumin: decreased -> protein depletion, malnutrition
assessment, diagnoses, and interventions for GI disorders
1. assessment:
- health hx (surgeries), symptoms, dyspepsia, N/V/D, changes in bowel habits, family hx, social hx, bowel habits
- physical: dry/cracked lips, inflamed/bleeding gums, beefy, smooth tongue, auscultate bowel sounds, bruising, palpate, rectal and anal area
2. diagnoses:
- acute pain, deficient fluid volume, risk for aspiration, risk for infection, ineffective tissue perfusion, constipation, diarrhea
3. interventions:
- pain management, fluid resuscitation, monitor I&Os, monitor BG, assist with feedings, labs, diagnostics
- diagnostic tests: labs, stool for occult blood, breath tests, US, x-ray, barium swallow, CT, upper endoscopy, colonoscopy, MRI, motility studies, manometry, electrophysiology status
oral and esophageal disorders
- dental carries, ill-fitting dentures, gum disease, cancers of oral cavity, parotitis, tooth abscess, TMJ
- interventions: prevent infection, good oral care, assess for sores, avoid acidic and spicy foods, monitor swallowing, protect airway
achalasia esophagus disorder
- inability to swallow either/both solids or liquids
- sensation of food sticking in esophagus
- vomiting
- diagnostics: x-ray, EGD with dilation, barium swallow, CT
- treatment: eat slowly, drink fluids with food, calcium channel blocker or nitrates, EGD with dilation
hiatal hernia
- regurgitation, chest pain, N/V
- diagnostics: x-ray, barium swallow, EGD, esophageal manometry
- treatment: small frequent meals, avoid caffeine and peppermint, avoid reflux meals, sit up at least 1 hr after meds, H2 blockers
gastroesophageal reflux disease
- heartburn, burning in esophagus/throat, hypersalivation, esophagitis, chest pain, dental erosion, adenocarcinomas
- diagnostics: barium enema, EGD, barium swallow, pH monitoring
- treatment: avoid spicy/acidic/greasy foods, eat small frequent meals, avoid caffeine, sit upright 1 hr post eating, elevate HOB, H2 blockers, surgery, PPIs
barrett's esophagus
- asymptomatic
- diagnostics: EGD
- treatment: depends on extent of cell changes
- frequent follow ups, upper endoscopy
gastric and duodenal disorders
- causes: medications like aspirin and NSAIDs, alcohol, radiation therapy
- pain, indigestion, anorexia, hiccups, N/V, melena
- pain 2-3 hrs after eating a meal
gastritis
- inflammation of stomach lining
- treatment: gut rest, clear liquids, avoid alcohol, antacids, H2 blockers, low fat diet, no fried foods, decrease stress and anxiety
- ranitidine (zantac), famotidine (pepcid), omeprazole (prilosec) PPIs, antibiotics, H2 blockers, anatcids
- foods to avoid: tea, coffee, cola, chocolate, tobacco, alcohol, mustard, paprika, cloves, pepper, hot spices
- pain in upper left abdomen, N/V, fullness
- diagnosis: H. pylori test via upper endoscopy, visualize
peptic ulcer disease (PUD)
- pain in epigastric region, occurs after eating, pain during night, vomiting with or without blood, constipation
- severe complications: elevate HR, hypotension, hypovolemic shock, peritonitis
- treatment: antibiotics metronidazole (flagyl), alcohol avoidance, PPIs (1-2 wks), adherence education, smoking cessation, diet modification, surgical repair
- famotidine (pepcid), calcium carbonate (maalox)
- diagnostics: EGD, biopsy, histologic exam, antibodies screening, stool antigen test, urea breath test, blood test for H. pylori, decreased Hgb and Hct, occult blood
- complications: GI bleed, intestinal obstruction
gastric cancer
- pain associated with eating, indigestion, weight loss, decreased appetite, vomiting, fatigue, nausea, bloating
- diagnostics: EGD with biopsy, barium x-ray, US, CT, MRI, CBC, cancer tumor markers
- treatment: chemotherapy, radiation therapy, surgery
- complication: dumping syndrome
- goals: reduce anxiety, optimal nutrition, pain relief
dumping syndrome
- early: 30 min after eating, vertigo, tachycardia, syncope, sweating, pallor, palpitations, distention, wanting to lie down
- late: 90 min after eating, dizziness, light headed, palpitations, diaphoresis, confusion
- rise in blood sugar
- treatment: eat high protein, high fat, low to moderate carbs
- meds: acarbose (precose), octreotide (sandostatin)
small bowel obstruction
- pain, N/V (fecal matter, bile), inability to eat, bloating, inability to pass, cramps
- diagnostics: x-ray, CT, MRI
- treatment: NGT, NPO, pain relief, antiemetics, surgery (hemicolectomy), fluid and electrolyte replacement
irritable bowel syndrome
- chronic functional disorder, recurrent abdominal pain
- triggers: chronic stress, sleep deprivation, surgery, infections, diverticulitis, food sensitivities
- alteration in bowel patters, diarrhea, constipation, abdominal pain, bloating, abdominal distention
- diagnostics: CBC, CRP, fecal calprotectin, tests for celiac, stool studies, colonoscopy
- treatment: lifestyle modifications, increase fiber, food diary, antispasmotics, peppermint oil, probiotics
celiac disease
- malabsorption of protein gluten, women most affected
- gluten found in wheat, barley, rye, dextrin
- predispose patients: DM type 1, down syndrome, turner syndrome
- diarrhea, oily stool, abdominal pain, distention, flatulence, weight loss, infertility, swelling
- treatment: avoidance therapy, no meds, educate on diet, consult with dietician
appendicitis
- acute inflammation of appendix
- most frequent cause of acute abdomen, often in young adults
- RLQ pain, peritonitis or abscess, gangrene 24-36 hrs
- emergency surgery
- McBurney's point
- N/V before abdominal pain (gastroenteritis), rebound tenderness, inc WBCs, perforation
- abdominal pain followed by N/V (appendicitis), cramping pain, epigastric/periumbilical area, abdomen or flank and McBurney's point, anorexia
- interventions: NPO, surgery, use of IS, IV fluids, high fowler's, opioids, antibiotics, no laxatives/enemas, no heat to abdomen
diverticular disease
- sac like herniation of lining of bowel
- diagnosis by colonoscopy
- encourage fluid intake of at least 2L/day
diverticulosis:
- multiple diverticula without inflammation, no problematic symptoms, bowel irregularity, nausea, bloating
- soft foods, fiber, cooked vegetables, avoid seeds
diverticulitis:
- infection and inflammation of diverticula, constipation, cramping, bloating, fever, leukocytosis
- low residue food, exercise, bulk laxatives, stool softeners, NGT, assess F&E imbalances, nutritional status
intestinal obstruction
- blockage prevents normal flora or intestinal contents through intestinal tract
- mechanical: intussusception, volvulus, hernia, adhesions, tumors
- nonmechanical: surgical manipulation bowel
bowel obstruction
- adhesions, strangulated inguinal hernia, ileocecal intussusception, intussusception from polyps, mesenteric occlusion, neoplasm, volvulus of sigmoid colon
- high pitched bowel sound above, decreased/absent bowel sounds below, abdominal pain and distention "colicky", obstipation, N/V
- treatment: NGT, intestinal decompression, NPO, F&E replacement, electrolytes, fowler's position, measure abdominal girth, analgesics
crohns
- frequent steatorrhea, rare, rectal bleeding not typical, mucus/pus in stool, rare diarrhea (5-6 formed stools/day), weight loss, anemia, dehydration, fever, fistula, anal abscess, abdominal pain after meals
- complications: intestinal narrowing, perianal disease, malnutrition, GI bleeding, fluid loss, colorectal cancer risk
- treatment: high cal, high vitamin, high protein, low residue milk free diet, antimicrobial agents, corticosteroids, elemental diet, parental nutrition, rest, surgery partial colectomy
ulcerative colitis
- absent steatorrhea, 10-15% malignancy, frequent rectal bleeding, mucus/pus in stool, defecation resolves, abdominal pain, diarrhea (10-12 liquid stools/day), weight loss, anemia, dehydration, fever, rare fistula, anal abscess
- complications: hemorrhage, F&E imbalances, perforation, toxic megacolon, osteoporosis risk, colorectal cancer risk
- mild/moderate treatment: low roughage diet, no milk products, antimicrobial therapy, corticosteroids, anticholinergics, antidiarrheals
- severe treatment: IVF with electrolytes, blood transfusions, NPO, NGT to low suction, antimicrobials, corticosteroids, monitor BG, TPN, surgery
inflammatory bowel disease
- assess: health and social hx, dietary patterns, bowel elimination, abdominal assessment, dietary recall
- diarrhea, acute pain, deficient fluid, imbalanced nutrition, activity intolerance, anxiety, ineffective coping, risk for impaired skin integrity, ineffective regimen management
- treatment: encourage normal bowel patterns, pain relief, fluid balance, nutrition, rest, skin health, electrolytes
colorectal cancer
- most are adenocarcinomas
- age over 50, genetics, family hx, familial adenomatous, polyposis, poor diet
- change in bowel habits, blood in stool-occult, tarry, bleeding, urge to have BM, sxs of obstruction, abdominal/rectal pain
- chemotherapy, diet modifications, surgery, colostomy
- assess: health hx, fatigue, weakness, pain, nutrition status, diet, elimination patterns, stool characteristics
- diagnosis: imbalanced nutrition, risk for deficient fluid, anxiety, impaired skin integrity, disturbed body image
GI bleed
- can be lower or upper GI tract
- blood in stool, vomit, coffee ground emesis/stool indicative of dried blood, achy pain, hypotension, tachycardia
- upper or lower endoscopy to stop bleeding
- NS infusion for hypotension/dehydration, avoid NSAIDs and aspirin
- encourage at least 2L of fluid/day, high fiber, bulk laxatives, stool softeners, topical meds, promote urinary elimination, hygiene, sitz bath, self care, use a donut to sit
anorectal conditions
- proctitis, anorectal abscess, anal fistula, anal fissure, hemorrhoids, pilonidal sinus or cyst
hemorrhoids
- swelling of anal tissue
- causes: straining during BM, advanced pregnancy, chronic constipation, eating food low in fiber, advanced age, frequent heavy lifting
- physical exam and visualization
- increase fiber and fluids in diet, stool softeners, topical treatment, sitz baths, pain relievers, surgical banding