NR546 Psychopharmacology: Week 4 questions with complete verified solutions + rationales
1/104
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
105 Terms
Anxiety
- Anxiety is a response to situations that are perceived as stressful or dangerous.
- Anxiety increases alertness, heart rate, and respirations, preparing the body to respond to perceived threatening environmental stimuli.
- While some states of anxiety are normal, even adaptive, when symptoms of anxiety persist and become intense or excessive, a diagnosis of an anxiety disorder may be warranted, and treatment is required.
Prevalence of Anxiety Disorders
- Anxiety disorders are one of the most common mental health concerns in the United States.
- According to Rosenthal and Burchum, about 25% of people develop pathological anxiety during their lifetime.
- Anxiety affects more women than men.
- Anxiety disorders can be debilitating and negatively impact the quality of life.
Untreated anxiety leads to-
- increased utilization of healthcare, morbidity, and mortality.
Types of Anxiety Disorders
According to the Diagnostic and Statistical Manual of Mental Disorders, anxiety disorders include
- separation anxiety disorder
- selective mutism
- specific phobias (animal, natural environment, blood-injection-injury, situational, other)
- social anxiety disorder
- panic disorder
- agoraphobia
- generalized anxiety disorder
- substance/medication-induced anxiety disorder
- anxiety disorder due to another medical condition.
Closely Related Disorders
- obsessive-compulsive disorder
- acute stress disorder
- posttraumatic stress disorder.
Frequent comorbidities with anxiety include-
- depression and substance use disorder.
Anxiety is characterized by-
- feelings of tension, worried thoughts, and physical changes such as increased blood pressure, nausea, or headaches.
Other anxiety symptoms-
- excessive or persistent fear
- sleep disturbance
- poor concentration
- irritability
- chest discomfort
- increased HR
- SOB
- restlessness
Neurobiological basis: Genetics
- Meier et al. reported that genetic factors are correlated with various types of anxiety disorders, symptoms, and comorbidities.
- Results from family and twin studies indicate that GAD has a genetic heritability of approximately 30%.
- Children of parents with GAD are twice as likely to experience anxiety as those who do not have a positive family history.
- Childhood developmental disturbances, trauma, environmental adversity, and stressful life events were identified as environmental components with the potential to impact genetic expression.
Neurological basis: Neuroanatomy
Physical components of fear are associated with several structures in the nervous system-
- Amygdala
- Hypothalamus
- Sympathetic nervous system
- Adrenal gland
- HPA axis
Ongoing activation in the presence of chronic fear or anxiety can increase morbidity.
Neurological basis: Neural networks
The brain contains a system of neural circuits referred to as cortico-stirato-thalamo-cortical (CSTC) feedback loops or "worry loops". Different types of anxiety or worry are linked to malfunctions in the circuit.
Neurological basis: Neural signaling
- Several neurotransmitters are regulated within the CTSC feedback loops.
- Neurotransmitters include serotonin, GABA, dopamine, norepinephrine, and glutamate which also help regulate the amygdala.
The sympathetic nervous system is involved in the fear response. Which symptom(s) may occur in response to sympathetic stimulation from fear? Select all that apply.
a. hyperventilation
b. vomiting
c. urge to urinate
d. hypertension
e. diarrhea
f. hyperglycemia
g. increased salivation
h. chest pain
a. hyperventilation
d. hypertension
f. hyperglycemia
h. chest pain
Rationale: Fear can trigger an adaptive respiratory response which can exacerbate asthma or other chronic breathing disorders. This explains client's reports of not being able to breathe during a panic attack. Sympathetic nervous stimulation causes increased heart rate, dry mouth, constipation, urinary retention, and increased blood sugar. When autonomic nervous system symptoms become chronic, there is an association with hypertension, cardiac ischemia, myocardial infarction, and sudden death.
Treatment Approach
- Anxiety disorders may be treated using cognitive behavioral therapy, exercise, sleep hygiene, mindfulness, meditation, or medications may be prescribed.
- No single medication or therapy will be effective for all persons.
- Each type of anxiety has specific treatment recommendations.
- Thorough assessment and identification of the most specific troublesome symptoms are crucial for accurate treatment. The symptoms guide prioritizing treatment targets and approaches.
True or False: Most often, a combination of psychotherapy and drug therapy is more effective than either treatment alone in the management of anxiety.
True
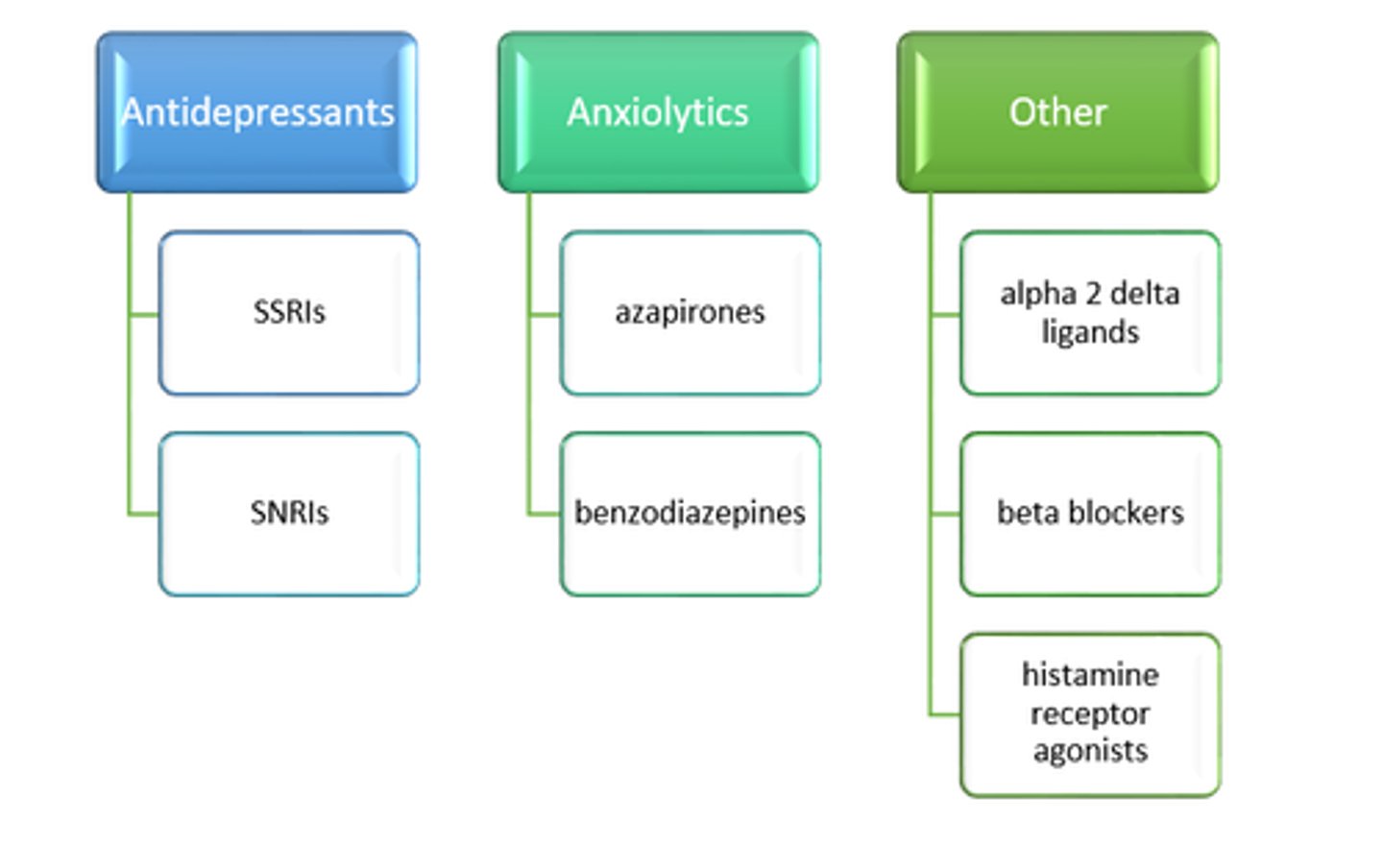
Medication Management of Anxiety
- Antidepressants are commonly used to treat anxiety, but they take several weeks for an optimal response.
- Benzodiazepines are effective immediately; they may be used concurrently as the antidepressants take effect when immediate relief is needed. Benzodiazepines must be tapered and discontinued once the antidepressants are at a therapeutic level.
- Other drugs such as alpha 2 delta ligands, beta-blockers, and histamine receptor agonists are used off-label to support anxiety treatment.
Antidepressants for Anxiety
- Antidepressants reduce symptoms of worry and apprehension; however, they have a limited effect on autonomic or somatic symptoms such as tremors, rapid heart rate, and sweating.
- Most antidepressants offer a similar degree of anxiety reduction, but selective serotonin reuptake inhibitors (SSRIs) or serotonin-norepinephrine reuptake inhibitors (SNRIs) are preferred over tricyclic antidepressants (TCAs) for the treatment of anxiety due to increased safety and tolerability.
- Antidepressant selection is generally based on a history of prior response, side effect profile, medication interactions, cost, or formulary availability.
- When SSRIs and SNRIs are used to treat anxiety, they should be started at half the recommended dose for depression. SNRIs should be used with caution as norepinephrine can initially exacerbate anxiety symptoms.
- The expected onset of the antianxiety effect is 2 to 4 weeks.
- Antidepressants should not be stopped abruptly because it can result in rebound anxiety.
Medication Management (Picture)
Selective serotonin reuptake inhibitors (SSRI) are the first-line drugs to treat which anxiety disorder(s)? Select all that apply.
a. social anxiety disorder
b. obsessive-compulsive disorder
c. generalized anxiety disorder
d. post-traumatic stress syndrome
e. panic disorder
All of the above
SSRIs are the first-line drugs to treat all anxiety disorders.
Medication Management for Anxiety
- SSRI
- SNRI
- Buspirone
- Alpha 2 Delta Ligands
- Beta Blockers
- Histamine Receptor Antagonists
Selective Serotonin Reuptake Inhibitors (SSRIs)
- Selective serotonin reuptake inhibitors (SSRIs) are used for the treatment of all anxiety disorders.
- They act by preventing the reuptake of 5-HT by synapses in the brain.
Selective Serotonin Reuptake Inhibitors (SSRIs): Drugs
- citalopram (Celexa)
- escitalopram (Lexapro)
- fluoxetine (Prozac)
- fluvoxamine (Luvox, Luvox CR)
- paroxetine (Paxil, Paxil CR)
- sertraline (Zoloft)
Selective Serotonin Reuptake Inhibitors (SSRIs): Adverse Effects
- anorexia
- diarrhea
- headache
- weight gain
- sexual side effects
- serotonin syndrome
Selective Serotonin Reuptake Inhibitors (SSRIs): Monitoring
- akathisia
- increased anxiety
- suicidal ideation
Selective Serotonin Reuptake Inhibitors (SSRIs): Clinical Pearls
- Each agent in the class has a unique pharmacological profile.
- Dosage should be started at half the recommended dose for depression; increase dosage after 2-4 weeks as needed to control anxiety.
- SSRIs should not be stopped abruptly because it can result in rebound anxiety.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs)
- Serotonin-norepinephrine reuptake inhibitors (SNRIs) are used to treat all anxiety disorders except obsessive-compulsive disorder.
- SNRIs work by preventing the reuptake of 5-HT and norepinephrine (NE) by synapses in the brain.
- Compared with venlafaxine and desvenlafaxine, which have serotonin reuptake inhibition (SRI) activity and dose-related affinity for norepinephrine reuptake inhibition (NRI) primarily, duloxetine has more balanced SRI and NRI activities.
- Levomilnacipran has higher activity at NRI than SRI.
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Drugs
- desvenlafaxine (Pristiq)
- duloxetine (Cymbalta)
- venlafaxine (Effexor, Effexor XR)
- levomilnacipran (Fetzima)
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Adverse Effects
- elevated blood pressure
- sweating
- anxiety
- dizziness
- insomnia
- constipation
- serotonin syndrome
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Monitoring
- increased anxiety
- suicidal ideations
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Contraindications
- liver problems
- hypertension
Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs): Clinical Pearls
- Due to the presence of norepinephrine, SNRIs can exacerbate anxiety.
- Dosage should be started at half the recommended dose for depression to minimize side effects.
Buspirone
- Azapirones are Federal Drug Administration (FDA) approved for short-term anxiety treatment and are used alone or as an adjunct to antidepressants.
- They bind to serotonin and dopamine receptors in the brain and increase norepinephrine metabolism in the brain.
Buspirone: Adverse Effects
- dizziness
- headache
- sedation
- nervousness
- nausea
Buspirone: Contraindications
- severe renal impairment
- severe hepatic impairment
- concurrent use of monoamine oxidase inhibitors (MAOIs)
Buspirone: Clinical Pearls
- Buspirone is not habit-forming, does not have abuse potential, causes withdrawal reactions, or potentiates alcohol and sedative-hypnotic effects.
- It is prescribed for two or three times a day due to the short half-life; it is not prescribed as needed (PRN).
- It has a gradual onset of action of 2 weeks, but over time provides the same efficacy as a benzodiazepine.
- BuSpar may decrease sexual side effects when used in combination with an SSRI.
Alpha 2 Delta Ligands
- Alpha 2 delta ligands are used off-label for general anxiety disorder (GAD).
- They bind with glutamate calcium channel blockers (Glu-CB) to inhibit the release of several neurotransmitters.
- Pregabalin has anxiolytic properties with selective binding to the α-2-delta subunit of voltage-gated calcium channels.
Alpha 2 Delta Ligands: Drugs
- pregabalin (Lyrica)
- gabapentin (Neurontin)
Alpha 2 Delta Ligands: Adverse Effects
- sedation, dizziness, impaired attention, confusion
- dry mouth, constipation, blurred vision
- possible weight gain
Alpha 2 Delta Ligands: Precautions
- suicidal ideation
- substance abuse
- heart failure
- renal impairment
Alpha 2 Delta Ligands: Contraindications
- myopathy
- avoid prescribing concurrently with benzodiazepines (BZOs)
Alpha 2 Delta Ligands: Clinical Pearls
- works quickly to reduce anxiety symptoms.
- pregabalin reduces anxiety with a similar onset to alprazolam.
Beta Blockers
Beta blockers can be used to treat somatic anxiety effects such as tachycardia and physical tension symptoms. They block the effects of norepinephrine and epinephrine.
Beta Blockers: Drugs
- propranolol (Inderal)
- atenolol (Tenormin)
Beta Blockers: Adverse Effects
- dizziness, vertigo
- fatigue
- hypotension
- decreased libido and sexual dysfunction
Beta Blockers: Precautions
- Use with caution in clients with asthma or heart failure; beta-adrenergic blockade can reduce heart rate and cause bronchoconstriction.
- Can blunt signs of hypoglycemia in diabetics
- Can mask clinical signs of hyperthyroidism
Beta Blockers: Contraindications
- first-degree heart block
- bradycardia
Beta Blockers: Clinical Pearls
- Beta blockers are not FDA-approved for the treatment of anxiety but are commonly used.
- They are often used for test anxiety, performance anxiety, and social anxiety because these drugs are nonsedating.
- Beta blockers may be prescribed after a traumatic event to help prevent a permanent fear response.
Histamine Receptor Antagonists
Histamine receptor antagonists are used for the treatment of anxiety and skeletal muscle tension associated with psychoneurosis, for anxiety symptoms associated with alcohol withdrawal, and for anxiety related to cardiac impairment. They act by blocking histamine 1 receptors.
Histamine Receptor Antagonists: Drug
hydroxyzine (Atarax)
Histamine Receptor Antagonists: Adverse Effects
- sedation
- dry mouth
- tremor
Histamine Receptor Antagonists: Monitoring
- hepatic status
- potassium level
- QT interval
Histamine Receptor Antagonists: Contraindications
- severe hepatic impairment
- QT prolongation
Histamine Receptor Antagonists: Clinical Pearls
- It is unclear if efficacy is due to an anxiolytic effect or a sedative effect.
- Caution clients about potential sedation when prescribing.
- When used concurrently with another central nervous system (CNS) depressant, the depressant dose should be reduced to half.
- Elderly clients are more sensitive to the sedative and anticholinergic side effects of hydroxyzine.
Treatment: Generalized Anxiety Disorder
- SSRIs
- SNRIs
- buspirone
- Drug Therapy for at least 1 year
Treatment: Panic Disorder
- paroxetine
- sertraline
- fluoxetine
- Drug therapy 6-9 months
Treatment: Obsessive Compulsive Disorder
- fluoxetine
- fluvoxamine
- sertraline
- paroxetine
- clomipramine
- Drug therapy for at least 1 year
Treatment: Social Anxiety Disorder
- sertraline
- paroxetine
- Drug therapy takes 4 weeks to see effects
Treatment: Post-Traumatic Stress Disorder
- paroxetine
- sertraline
Josie is a 36-year-old who was diagnosed with generalized anxiety disorder. She was prescribed paroxetine (Paxil) 12 weeks ago. She has been taking the medication as prescribed, and although she has tolerated the medication well, she has not achieved relief of anxiety symptoms with increases in dosing at each follow-up visit. Place the following medications in order of what would be prescribed next for Josie.
Duloxetine (Cymbalta)
Pregabalin (Lyrica)
Alprazolam (Xanax)
Hydroxyzine (Atarax)
Buspirone (BuSpar)
Escitalopram (Lexapro)
The correct order of prescription is:
- escitalopram (Lexapro)
- duloxetine (Cymbalta)
- buspirone (BuSpar)
- pregabalin (Lyrica)
- hydroxyzine (Atarax)
- alprazolam (Xanax)
Rationale: Use a stepwise plan to change drug treatment if the initial medication was either ineffective or poorly tolerated.
- Switch from one SSRI to another.
- Switch from SSRI to SNRI.
- Augment with buspirone.
- Augment with pregabalin.
If standard drugs are not effective, nonstandard drugs approved for other anxiety disorders may be used.
- Hydroxyzine.
- Benzodiazepines (if clinically justified) are for short-term use only.
Benzodiazepines (BZOs)
- Benzodiazepines (BZOs) are used to treat acute anxiety symptoms.
- BZOs provide short-term relief of acute anxiety but do not treat the underlying cause.
- Benzodiazepines are controlled substances and not intended for long-term use due to the risk of tolerance, dependence, and an uncomfortable withdrawal process.
- Abrupt cessation of BZOs can lead to severe withdrawal symptoms including seizures and death.
Benzodiazepines: MOA
- BZOs enhance gamma-aminobutyric acid's (GABA's) inhibitory effects in the brain by acting on GABA receptors outside of the receiving neuron to open a channel that allows negatively charged chloride ions to pass into the neuron. The negative ions "supercharge" the neuron making it less responsive to neurotransmitters that would normally excite it.
- BZOs also react at specific benzodiazepine receptors on the GABA neuron. Benzodiazepine receptor subtypes have slightly different actions:
- Alpha one is responsible for sedative effects.
- Alpha two is responsible for anti-anxiety effects.
- Alpha one, alpha two, and alpha five are responsible for anticonvulsant effects.
Benzodiazepines: Key Points
- BZOs will induce calm but will also affect higher-level thinking.
- Excitatory neurotransmitters, including norepinephrine, serotonin, acetylcholine, and dopamine, are necessary for alertness, memory, muscle tone, coordination, emotional responses, endocrine gland secretions, heart rate, and blood pressure control.
- BZOs increase GABA's inhibitory activity, leading to the decreased output of excitatory neurotransmitters resulting in the adverse effects related to BZO use.
alprazolam IR (Xanax)
Short-acting
Use: GAD, panic disorder
Half-life: 12-15 hours
Equivalence: 0.5 mg
Dosage:
- anxiety: 0.75-1.5mg/day in divided doses; max dose 4 mg/day.
- panic: 1.5mg/day in divided doses; dosing may exceed 4 mg, increase slowly.
Additional Information:
- rapid onset, less sedating.
- can cause sedation, fatigue, forgetfulness, hypersalivation.
- useful adjunct to SSRI/SNRI.
- recommended use: lowest effective dose for shortest period of time.
- risk for respiratory depression, especially when taken with CNS depressants.
- contraindicated in angle-closure glaucoma.
- tapered dosing when discontinuing, risk of seizures with withdrawal.
lorazepam (Ativan)
Short-acting
Use: agitation, anxiety
Half-life: 10-20 hours
Equivalence: 1 mg
Dosage:
- 2-6 mg/day; BID-TID dosing; max 10 mg/day.
- elderly: 1-2 mg/day in divided doses.
Additional Information:
- rapid onset
- can cause sedation and fatigue (anterograde anesthesia)
- safe with liver disease; use lower dosage with liver and renal impairment
- increased risk of drug hangover due to longer half-life
- increased depressive effects with opioids- do not prescribe together
- caution with sleep apnea
- contraindicated in angle-closure glaucoma, breastfeeding, and pregnancy
- tapered dosing when discontinuing
Clonazepam (Klonopin)
Long-acting
Use: panic disorder
Half-life: 30-40 hours
Equivalence: 0.5 mg
Dosage:
- 0.5-2 mg/day in divided doses or at bedtime
starts at 0.25 mg and increases slowly
Additional Information:
- rapid onset and less sedating, but does cause some sedation and fatigue
- longer duration of action
- only Category C benzodiazepine; not recommended with breastfeeding
- increases salivation
- contraindicated with liver disease
- easier to taper dosing than other BZOs due to the long half-life
diazepam (Valium)
Long-acting
Use: acute myocardial infarction-related anxiety, night terrors, alcohol withdrawal
Half-life: 20-50 hours
Equivalence: 10 mg
Dosage:
- 2-10 mg two times to four times daily
Additional Information:
- rapid onset
- available in rectal gel
- can cause sedation, fatigue, forgetfulness, and confusion
- contraindicated in angle closure glaucoma
- risk of dependence after 12 weeks
- risk for seizures with rapid discontinuation; taper 2 mg every 3 days
The PMHNP is prescribing alprazolam for a client with panic disorder. The PMHNP should be concerned if the client is also prescribed which medication?
zolpidem
duloxetine
buspirone
sertraline
zolpidem
Alprazolam presents a risk for respiratory depression, especially when taken concurrently with another central nervous system depressant like zolpidem. SSRIs, SNRIs, and buspirone may be taken with alprazolam.
Benzodiazepines: Oversedation
- Symptoms are usually dose-related.
- Symptoms include drowsiness, poor concentration, incoordination, muscle weakness, dizziness, and mental confusion.
- When benzodiazepines are taken for sleep at night, sedation effects may persist the next day, particularly for medications with longer half-lives.
- Tolerance to sedative effects usually develops over 1-2 weeks.
- Oversedation is associated with an increased risk of accidents, falls, and injury.
- Clients should be aware of risks when driving/operating machinery and that they can be charged with driving under the influence.
Benzodiazepines: Memory Impairment
Use of BZOs can:
- cause lack of concentration and attention
- cause difficulty acquiring new information
- cause difficulty remembering recent events and time sequence
- cause "blackouts"
- interfere with the normal psychological adjustment to trauma if used for more than a few days
- inhibit the grieving process when used for loss or bereavement
- impair learning of alternative stress-coping strategies for anxiety states and agoraphobia
Key points:
- BZOs are often used during surgery or medical procedures where memory impairment and amnesia may be beneficial.
- BZOs are often prescribed for acute stress-related situations and are appropriate for the short-term treatment of grief, such as a loss of a spouse. However, continued BZO use can affect the grief process and prolong grief.
Benzodiazepines: Depression
- Long-term benzodiazepine use may inhibit emotional centers in the brain.
- Complaints include an inability to feel pleasure or pain.
- Depression may increase suicide risk.
Benzodiazepines: Tolerance & Dependence
Tolerance
- Benzodiazepine receptors become less responsive in the continued presence of BZOs.
- Tolerance develops with regular use and can occur in as little as 2 weeks.
- A higher dose is required to obtain the effect initially provided by a lower dose.
- When prescribed for sleep, sleep complaints return after a few weeks of regular use.
Dependence
- Benzodiazepines can be psychologically and physically addictive.
- Physical and psychological dependence can develop within a few weeks of regular or repeated use.
Benzodiazepines: Paradoxical Effects
- increased anxiety
- irritability
- hyperactivity
- aggression
- insomnia
- nightmares
- hallucinations at the onset of sleep
- cases of assault and homicide have been reported
Key Education Points for Benzodiazepines
- rationale for benzodiazepine prescription
- expected length of treatment (short term only)
- avoiding alcohol
- adverse effects
- risks of tolerance and dependence
- avoiding driving while taking this medication
Safety and Prescribing Guidelines: Ground Rules
- Client uses only one pharmacy.
- BZO should be prescribed by only one provider.
- Check the state prescription monitoring program (PMP) controlled substance database.
- No early refills.
Safety and Prescribing Guidelines: Do Not Prescribe
Do not prescribe if the client is concurrently taking:
- opioids
- other benzodiazepines
- z-drugs (medications for sleep)
- muscle relaxants
- marijuana
Safety and Prescribing Guidelines: Schedule Regular Follow-Up
The frequency of follow-up is based on client risk:
- older and younger clients
- clients with a history of substance use disorder
Required components during follow-up:
- Symptom assessment
- PMP prescription monitoring
- Review urine drug screening
- Care plan with informed consent
- Appropriate documentation
Safety and Prescribing Guidelines: Prescribe for Short Course Only
2-4 weeks
Longer treatment requires a clear, written plan with a rationale
Tapering and Deprescribing Benzodiazepines
- Withdrawal symptoms may occur if long-term BZO use is ceased abruptly.
- Tapering the dose to discontinuation may reduce the risk of withdrawal symptoms.
- Before tapering, assess the client's underlying condition and discuss alternate therapies.
- Withdrawal symptoms tend to occur faster with shorter-acting agents (within 2 to 3 days) than with longer-acting agents (within 5 to 10 days).
- The Ashton Model recommends reducing daily dosing by 10-20% every 1-2 weeks.
Lifespan Considerations: Pregnancy
- Paroxetine is contraindicated in pregnancy due to the risk of atrial septal defects.
- Hydroxyzine is contraindicated in the 1st trimester.
- Benzodiazepines cross the placenta, so there is an increased risk of neonatal complications even with therapeutic doses.
Use of benzodiazepines during pregnancy can cause:
- intrauterine growth restriction
- oversedation at birth can cause floppiness, difficulty breathing, and difficulty feeding
- potential for learning disabilities, autism, and attention-deficit/hyperactivity disorder (ADHD)
- neonatal withdrawal syndrome
Lifespan Considerations: Breastfeeding
Contraindicated when breastfeeding:
- gabapentin
- benzodiazepines
- histamine receptor agents
- alpha 2 ligands
Lifespan Considerations: Older Adult
- With advancing age, a decline in renal and liver function may contribute to the prolonged elimination of medications leading to increased sedative effects and fall risk. Consider decreasing the dosage of sedative-hypnotics when prescribing for older adults; taper whenever possible.
2019 American Geriatric Society (AGS) Beers Criteria include the following recommendations:
- avoid barbiturates (increased dependence, tolerance, risk of overdose)
- avoid benzodiazepines (increased sensitivity, decreased metabolism)
- avoid gabapentin and pregabalin (falls due to sedation)
- avoid hydroxyzine (clients with dementia, cognitive impairment, delirium, lower urinary symptoms, or benign prostatic hyperplasia [BPH])
Lifespan Considerations: Children
- Anxiety disorders often begin in childhood and are often comorbid with depression or bipolar disorder.
- For children and adolescents, psychotherapy is the first choice of treatment.
- SSRIs may be used for severe symptoms or when psychotherapy is not effective.
- There is an increased risk of suicide in clients less than 30 years using SSRIs.
- Gabapentin is not approved for anxiety in children, it may only be used for seizures.
Sofia presents to the PMHNP with a report of being overwhelmed with stress and worry. Sofia reports she has always dealt with these feelings, but it has been worse since she has taken a more advanced role in her work with significant responsibility. She has difficulty relaxing and is often fatigued. The PMHNP diagnoses Sofia with generalized anxiety disorder.
Which is the best choice for the PMHNP to prescribe for Sofia?
Sertraline 25 mg po once daily
Alprazolam 1 mg po three times daily
Buspirone 7.5 mg po twice daily
Duloxetine 60 mg po daily
Sertraline 25 mg po once daily
Anxiety can often be treated with antidepressants. The best choice for Sofia is the SSRI, sertraline, because it is half the recommended dose for depression. The duloxetine dosage listed is an appropriate dose for depression. When treating anxiety, dosage should start at 30 mg and be titrated up. Buspirone is not the first drug of choice and it is typically used short term. A benzodiazepine should not be the first drug of choice.
Sofia was prescribed sertraline 25 mg po once daily. Sofia's dosage was increased to 50 mg after week 1, increased to 100 mg after week 2, and increased to 150 mg after week 3. At Sofia's 4-week follow-up visit, she is tolerating the medication well and symptoms are slightly improved. Which is the best action by the PMHNP?
Maintain the sertraline dose at 150 mg
Increase the sertraline dose to 200 mg
Switch drug therapy to another SSRI
Augment drug therapy with another drug
Increase the sertraline dose to 200 mg
The PMHNP should increase the sertraline dose to the maximum dose of 200 mg because the client has slightly improved symptoms. It may take several months for the client to see full relief, so it is best to wait before adding additional drugs or switching drugs.
At Sofia's 12-week follow up visit, the client is taking the maximum dose of sertraline and is experiencing improvement in symptoms, but not full relief from symptoms. Which is the best action by the PMHNP?
Transition to duloxetine
Transition to fluoxetine
Augment with buspirone
Augment with alprazolam
Augment with buspirone
The client has improvement in symptoms, but not full relief, so the best action is to augment the current therapy. Buspirone offers anxiety relief but does not have the effects of a CNS depressant or cause dependence like benzodiazepines. Buspirone does take approximately 4 weeks to reach full therapeutic effects. If the client did not experience an improvement in symptoms, switching to another SSRI would be the best action.
Jill, a 23-year-old graduate student, presents with reports of panic attacks and worry "my whole life." She reports that she can bring on panic attacks herself when she worries. This happens almost every day and some days it is so bad she cannot go to work or school. She was offered a few Xanax by a friend, and she wants a prescription because "they really help." The PMHNP diagnoses Jill with Generalized Anxiety Disorder (GAD).
Which is the best medication for the PMHNP to prescribe?
escitalopram
buspirone
alprazolam
bupropion
escitalopram
Escitalopram is the only listed SSRI which is the appropriate drug class for GAD. Bupropion is an SNRI. Medications that contain norepinephrine can increase anxiety. Jill has chronic anxiety, not acute anxiety. Benzodiazepines should be prescribed only for short-term use, less than 4 weeks as an adjunct until the SSRI achieves efficacy. Buspirone seems like a good choice because this medication targets 5HT1A; however, this medication is used as an adjunct therapy, not monotherapy.
Mary Ann is a 55-year-old woman who scheduled an appointment with the PMHNP a month before a planned vacation to Hawaii. Mary Ann states, "I have been on a plane once before, and I had a major panic attack. It was terrible." She is concerned about having another panic attack on the long transpacific flight. She is in good health and is not taking any medications. Which is the best choice for the PMHNP to prescribe?
alprazolam #4 tabs PRN
buspirone daily
alprazolam #14 tabs PRN
citalopram #4 tabs PRN
alprazolam #4 tabs PRN
Alprazolam #4 tabs PRN is the best choice for anxiety in a specific high anxiety situation such as flying. Benzodiazepines can be prescribed for PRN use. Limiting the number of pills is appropriate to help prevent misuse and diversion of the medication. In this case, medication was provided for departure and return. Using a daily medication is not necessary since Mary Ann does not have chronic anxiety. Providing an SSRI PRN is not appropriate as it may take up to 6 weeks for efficacy.
Andrea is a 65-year-old woman who presents for care because "her nerves are a mess." Her husband was diagnosed this week with Stage IV pancreatic cancer and has less than a month to live. Andrea can not eat or sleep. She cries constantly and "her heart is broken." Andrea is on no medications. Which is the best choice for the PMHNP to prescribe?
citalopram daily and alprazolam #15 tabs PRN
trazadone daily and alprazolam #15 tabs PRN
mirtazapine daily
venlafaxine daily
citalopram daily and alprazolam #15 tabs PRN
Citalopram and alprazolam are the best choice. Starting an SSRI with a PRN benzodiazepine is appropriate to help coping while waiting for the full effects of citalopram. Venlafaxine, an SNRI, contains norepinephrine which can increase anxiety. Trazadone may help with sleep, but the dosing required for depression and anxiety would result in increased sedation, which can increase fall risk in older adults. Mirtazapine is appropriate for the loss of appetite, but the complaint is < 1 week. Mirtazapine is associated with weight gain and is not first-line treatment for anxiety.
____________________ are the treatment of choice for medication management of anxiety.
Antidepressants
_______________________ should be used short-term because of the adverse effects such as sedation, tolerance, and dependence.
Benzodiazepines (BZOs)
What medication is as effective as benzodiazepines but does not cause sedation?
Buspirone
Which drug classifications can be used off-label for anxiety?
- alpha 2 ligands
- beta-blockers
- histamine receptor agonists.
Clients prescribed antidepressants should be monitored for symptoms of _----_______________ _____________.
suicidal ideations
Antidepressants and BZOs should be tapered when discontinuing to prevent-
- withdrawal symptoms
- rebound anxiety
- seizures
Recommended length of benzodiazepine treatment
2-4 weeks
How to wean off benzodiazepines
- The Ashton Model recommends reducing daily dosing by 10-20% every 1-2 weeks.
- Example: 2mg alprazolam IR (Xanax) -> 1mg tablet 1.5 for 7 days -> 1 tablet for 7 days -> ½ tablet for 7 days
Benzodiazepine Diversion Prevention Practices
Set Ground Rules:
- The client uses only one pharmacy.
- Only one provider should prescribe BZO.
- Check the state prescription monitoring program (PMP) controlled substance database.
- No early refills.
Required components during follow-up:
- symptom assessment
- PMP prescription monitoring review
- urine drug screening
- care plan with informed consent
- appropriate documentation
Which medication is approved for nightmares associated with PTSD?
Prazosin (alpha 1 adrenergic blocker)
Which two medications are FDA-approved for the treatment of PTSD?
Sertraline (Zoloft) and Paroxetine (Paxil)- both SSRIs
What medication class is the first-line treatment for OCD?
SSRIs: fluoxetine, fluvoxamine, sertraline, or paroxetine