A Level CIE Biology: 14 Homeostasis
1/119
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
120 Terms
homeostasis
the process of maintaining constant internal body conditions
in order to function properly and efficiently, organisms…
have diff control systems that ensure their internal conditions are kept relatively constant
why is homeostasis important
ensures the maintenance of optimal conditions for enzyme action and cell function
sensory cells
detect information about the conditions inside and outside of the body
6 physiological factors controlled by homeostasis in mammals:
core body temp
metabolic waste e.g. co2 and urea
blood pH
conc of glucose in blood
water potential of blood
conc of respiratory gases (co2 and o2) in blood
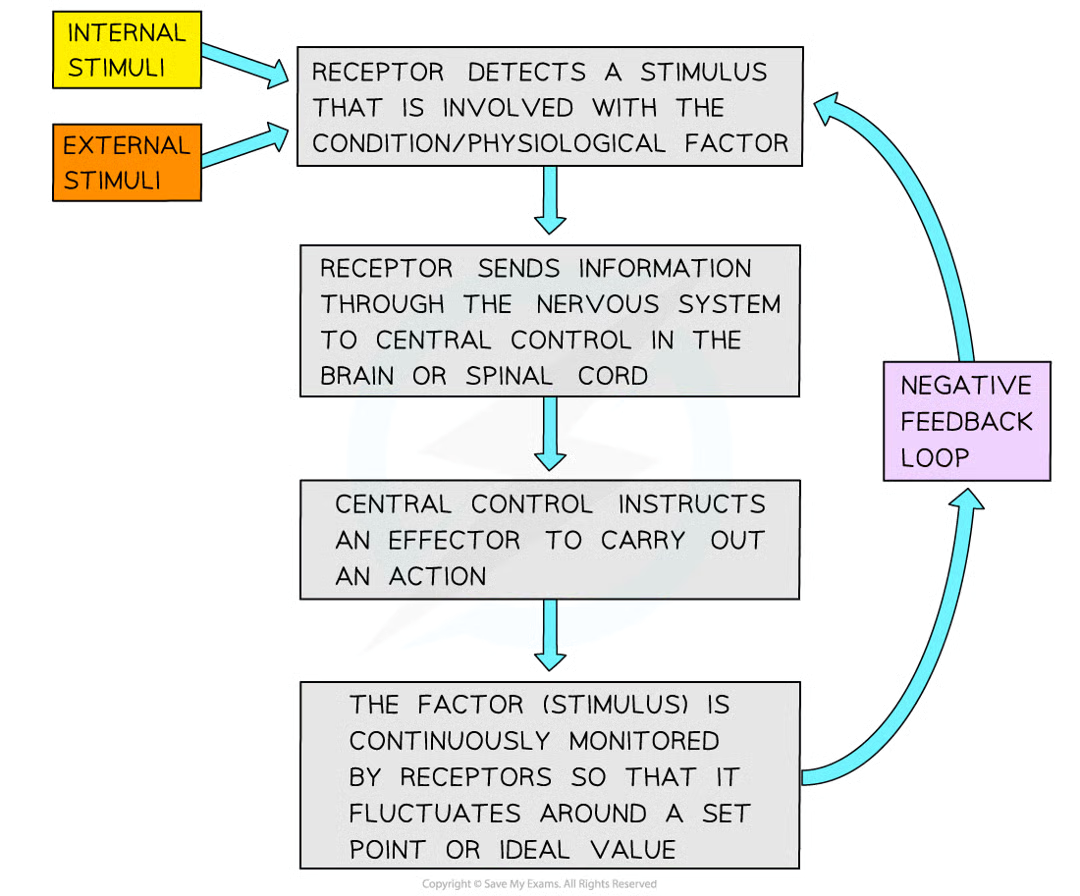
how is homeostatic balance (keep factors within certain limits) maintained
majority of homeostatic control mechanisms in organisms use negative feedback
3 things negative feedback control loops involve
receptor
coordination system
effector
receptor/sensor
detects stimulus that is involved with condition/physiological factorc
coordination system (nervous and endocrine)
transfer information between different parts of body
effector (muscles and glands)
carry out a response
3 outcomes of negative feedback loop:
factor/stimulus is continuously monitored
if increase in factor, body responds to make factor decrease
if decrease in factor, body responds to make factor increase
what 2 coordination systems does homeostasis in mammals rely on to transfer info between diff parts of body
nervous - info transmitted as electrical impulses that travel along neurones
endocrine - info transmitted as chemical messengers called hormones that travel in blood
what do metabolic reactions within body produceq
waste products
excretion
removal of waste products (e.g. co2 and urea)
where is urea produced
liver
why is urea produced
excess amino acids, if more protein eaten than required, excess can’t be stored in body.
why does deamination occur
amino acids within protein provides useful energy so amino group must be removed from each amino acid to make energy accessible
deamination 3
the amino group (-NH2) of an aa is removed, together with an extra hydrogen atom
these combine to form ammonia (NH3)
the remaining keto acid may enter the krebs cycle to be respired, be converted to glucose, or converted to glycogen/fat for storage
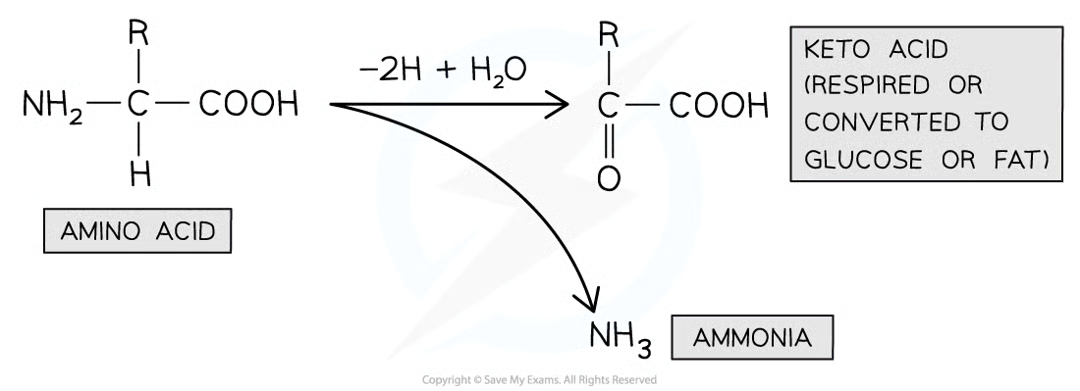
ammonia features 3
very soluble
highly toxic compound
produced during deamination
why is ammonia damaging if allowed to build up in blood 3
dissolves in blood to form alkaline ammonium hydroxide, disrupting blood pH
impacts reactions of cell metabolism e.g. respiration
interferes with cell signalling processes
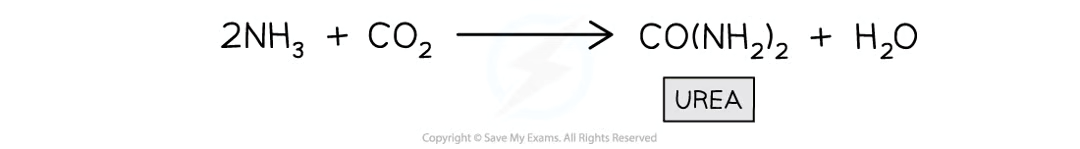
why is ammonia converted to urea
urea is less soluble and less toxic than ammonia
how is ammonia converted to urea
combined with co2
kidney 2 functions
osmoregulatory organ - regulate water content of blood (vital for maintaining blood pressure)
excretory organ - excrete toxic waste products of metabolism (e.g. urea) and substances in excess of requirements (e.g. salts)
humans have_ kidneys
2
excretory system diagram
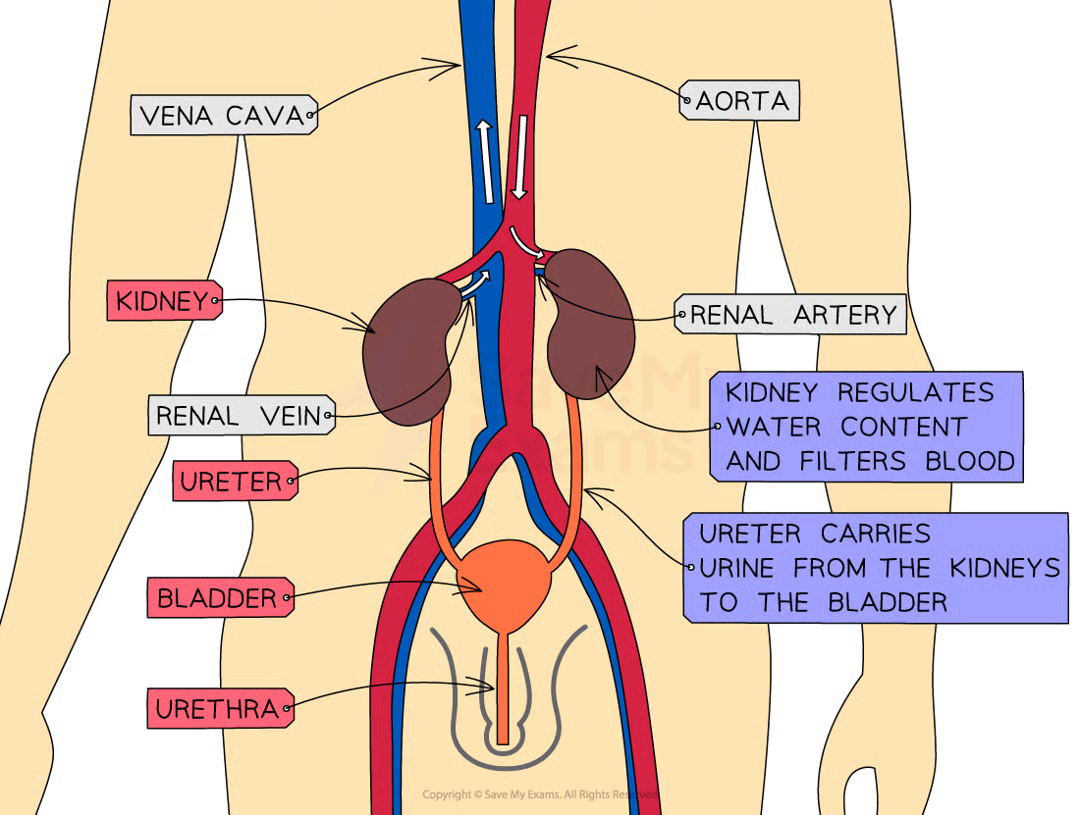
structures of excretory system
renal artery
renal vein
kidney
ureter
bladder
urethra
renal artery function
carries oxygenated blood (containing urea and salts) to the kidneys
renal vein function
carries deoxygenated blood (that has had urea and excess salts removed) away from the kidneys
kidney function
regulates water content of blood and filters blood
ureter function
carries urine from the kidneys to the bladder
bladder function
stores urine (temporarily)
urethra function
releases urine outside of the body
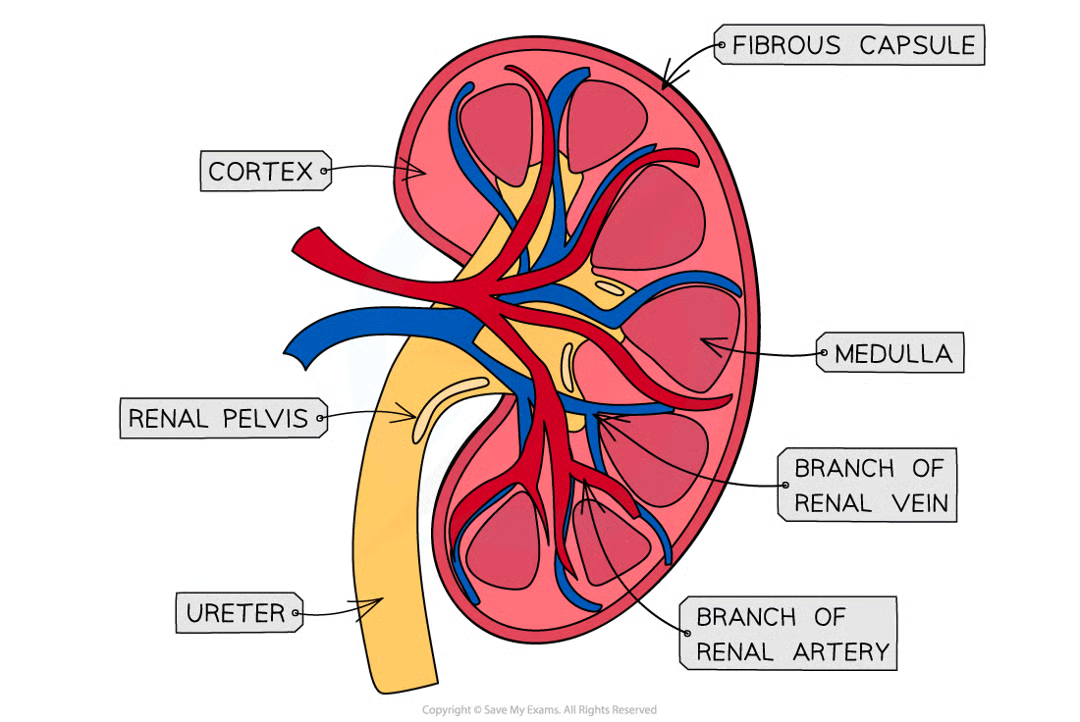
fibrous capsule
fairly tough outer layer that surrounds the kidney
3 main kidney parts beneath the fibrous capsule
the cortex (contains glomerulus as well as Bowman’s capsule, proximal convoluted tubule, and distal convoluted tubule of the nephrons)
the medulla (contains loop of Henle and collecting duct of the nephrons)
the renal pelvis (where the ureter joins the kidney)
nephron 3 features
thousands of tiny tubes in each kidney
functional unit of the kidney
responsible for urine formation
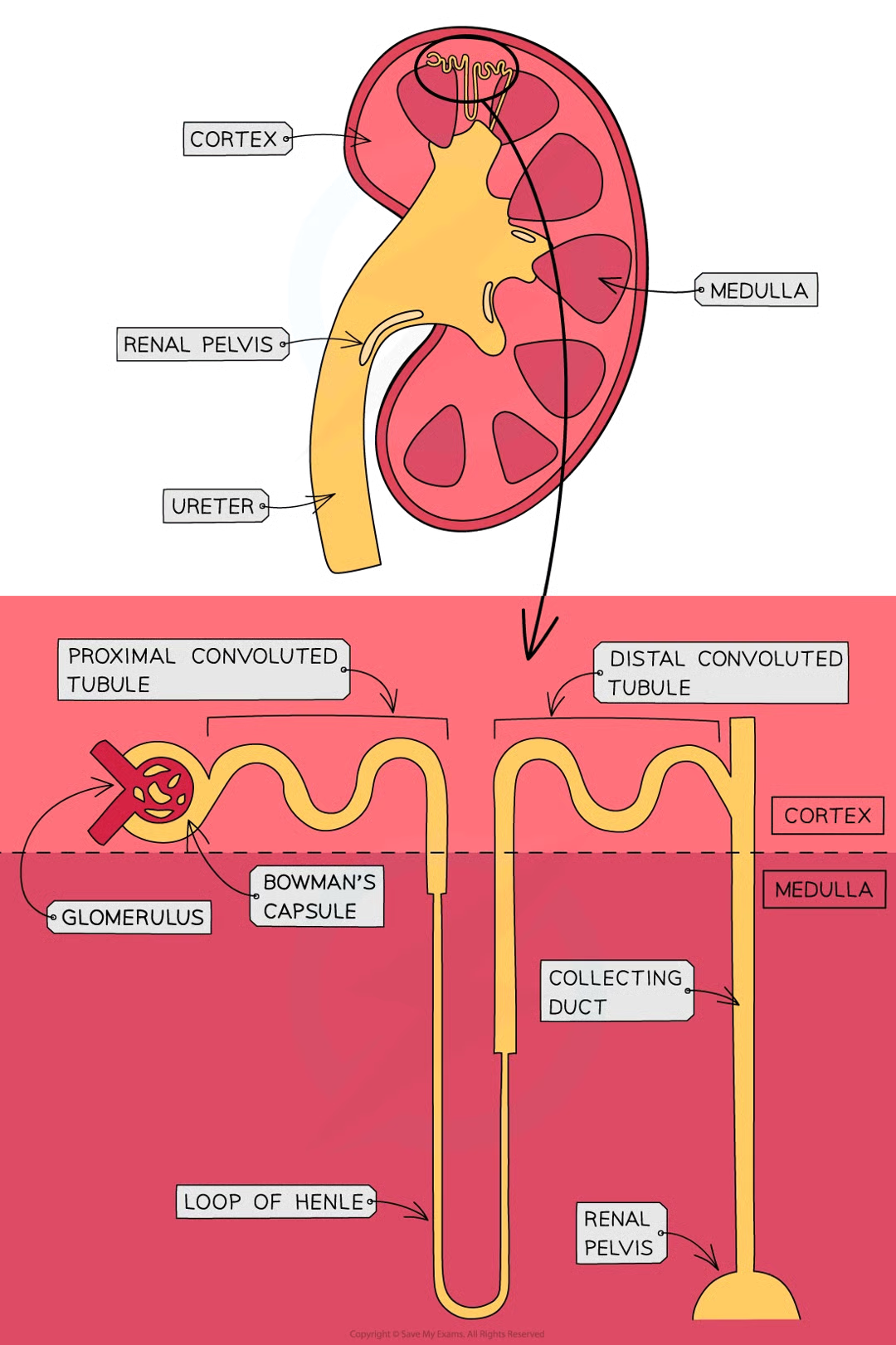
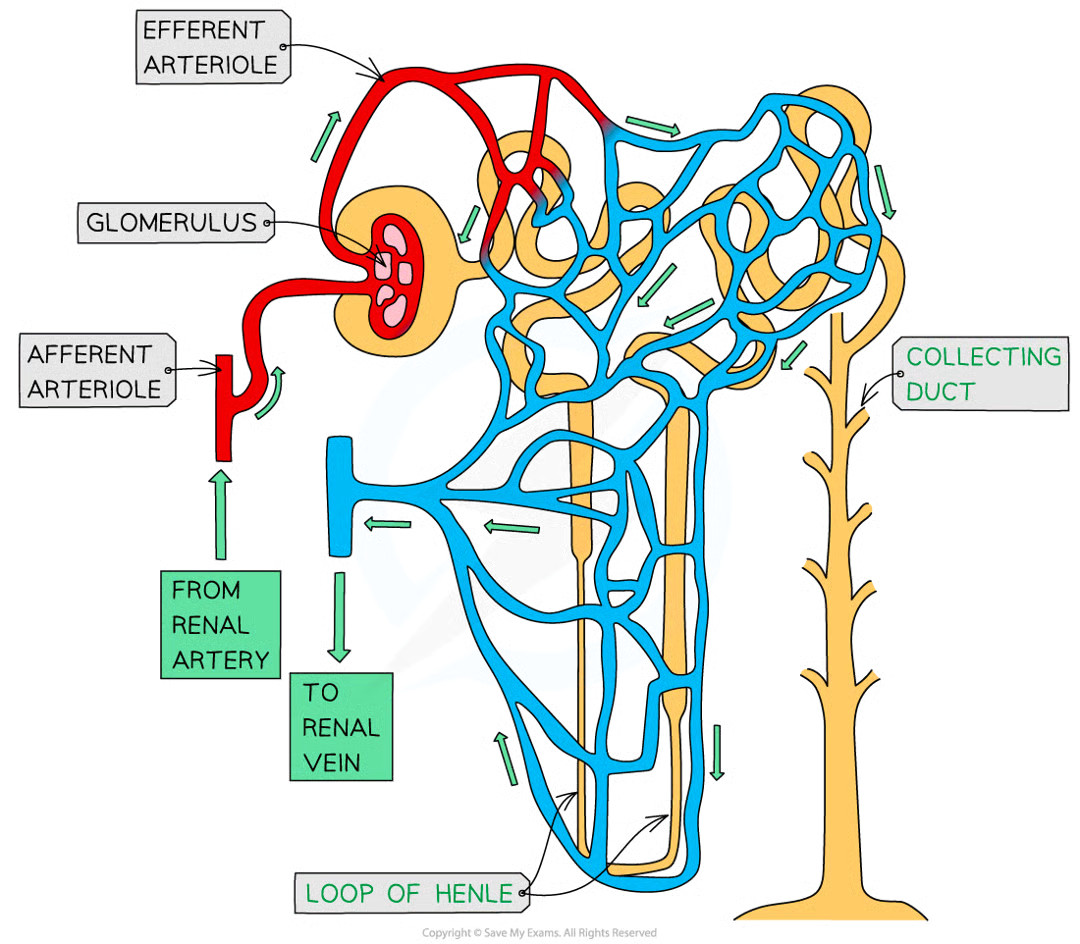
network of blood vessels associated with each nephron:
within bowmans, each nephron = glomerulus
each glomerulus is supplied w blood by an afferent arterial (which carries blood from renal artery)
capillaries of the glomerulus rejoin to form efferent arteriole
blood flows from efferent arteriole into network of caps that run closely alongside rest of nephron
blood from caps eventually flows into renal vein
2 stages of urine formation in the kidneys
ultrafiltration
selective reabsorption
where does ultrafiltration occur
bowman’s capsule
where does selective reabsorption occur
proximal convoluted tubule
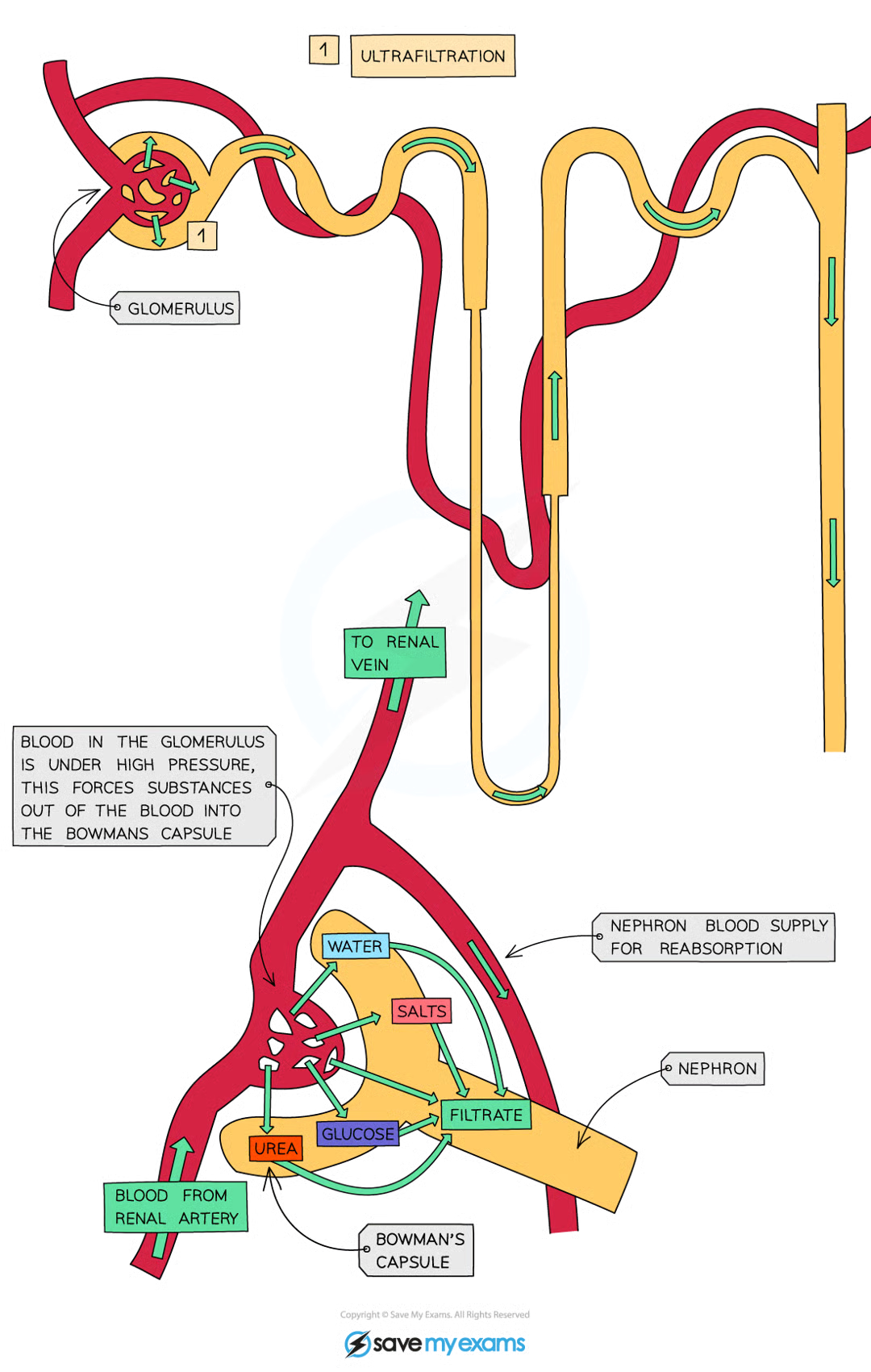
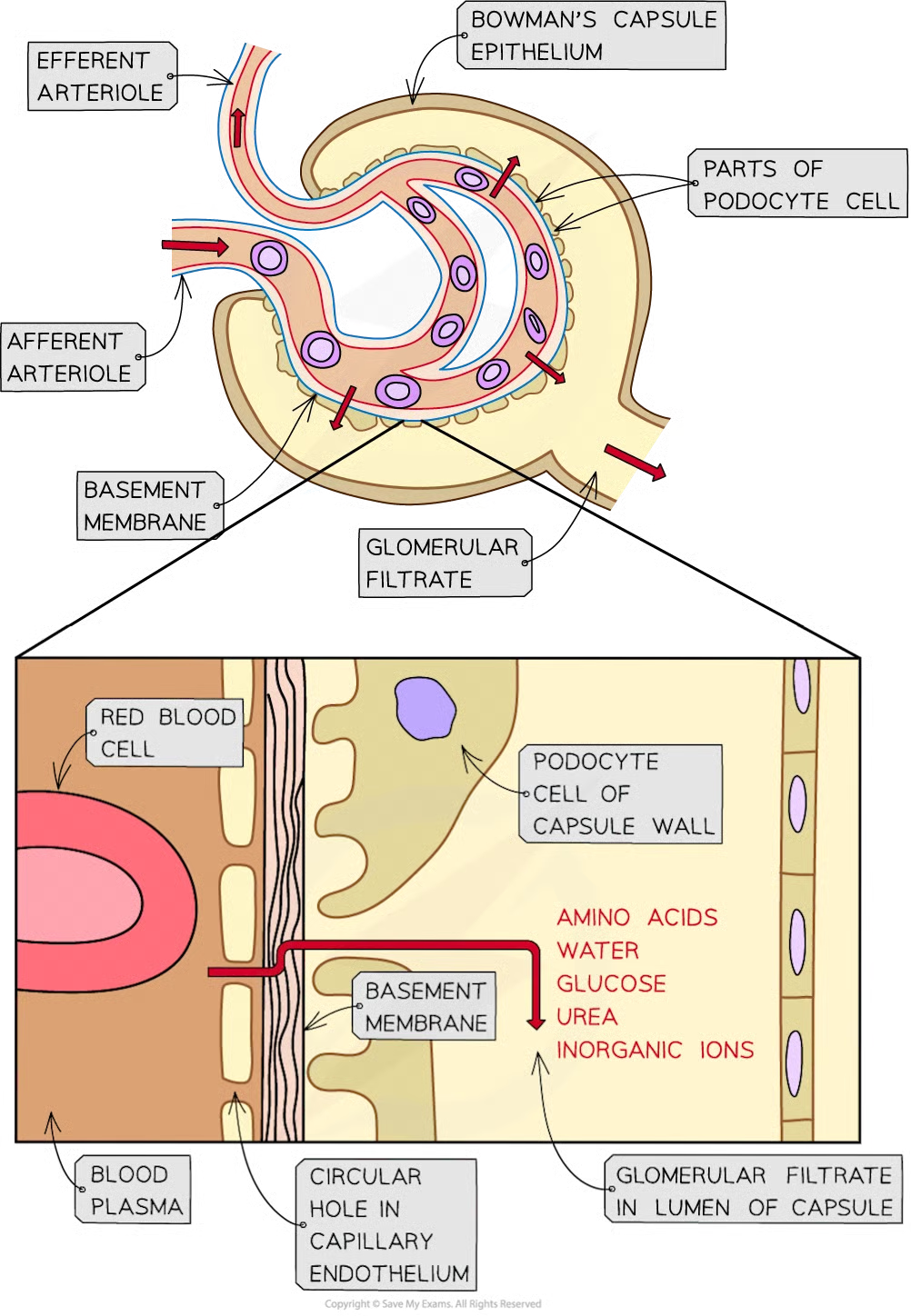
ultrafiltration:
small molecules (including aas, water, glucose, urea and inorganic ions) are filtered out of blood caps of glomerulus and into bowman’s capsule to form filtrate known as glomerular filtrate
selective reabsorption
useful molecules are taken back/reabsorbed from the filtrate and returned to the blood as the filtrate flows along the nephron
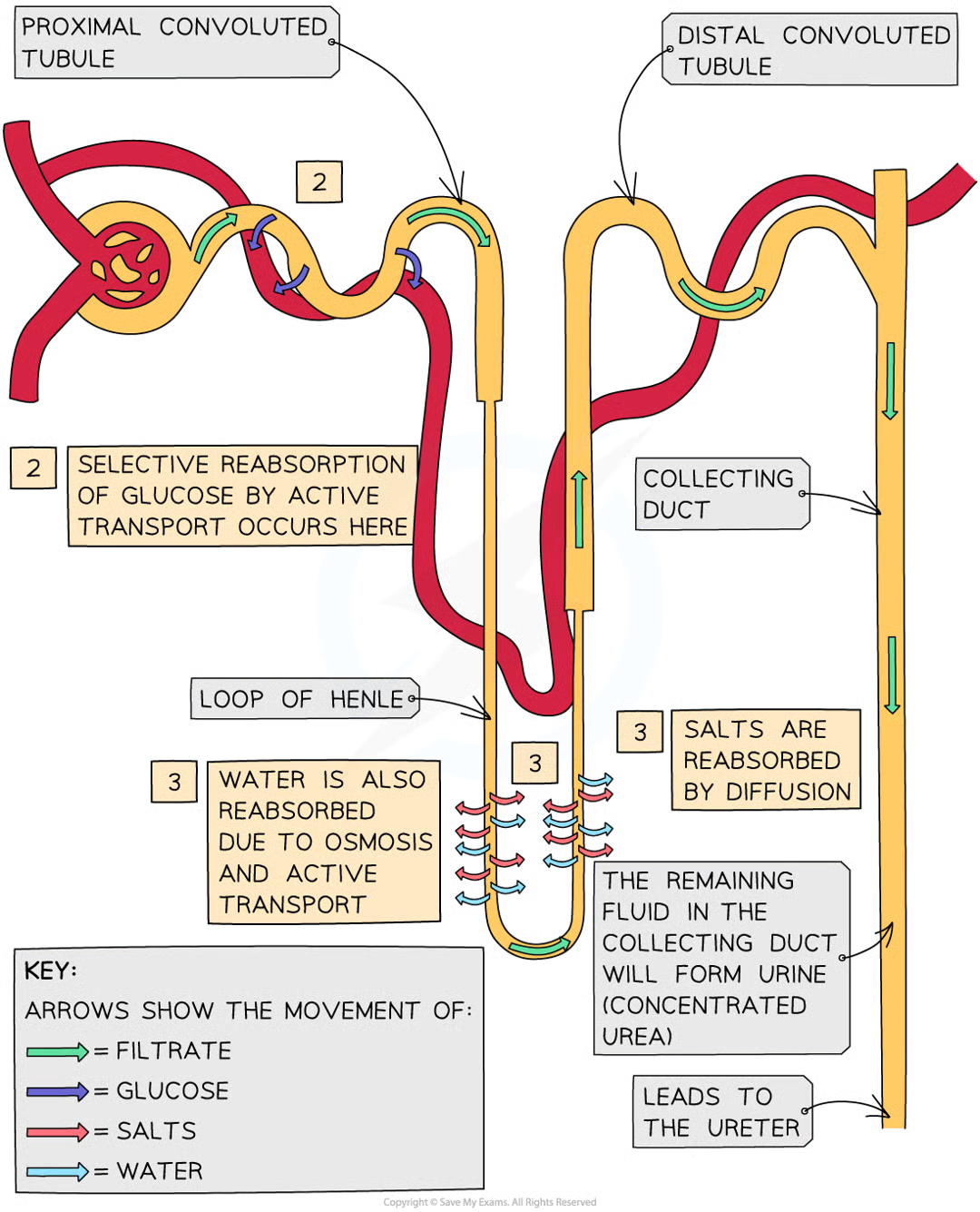
what happens after selective reabsorption (2)
after the necessary reabsorption of aa, water, glucose and inorganic ions is complete (even some urea is reabsorbed), the filtrate eventually leaves the nephron and is now referred to as urine
urine flows out of kidneys, along the ureters and into the bladder, where it is temporarily stored
ultrafiltration: where and why do arterioles branch off
they branch off the renal artery and lead to each nephron, where they form a knot of capillaries (glomerulus) sitting inside the cup-shaped Bowman’s capsule
ultrafiltration: why is pressure increasing further into the glomerulus
capillaries get narrower and increases pressure on blood moving through which is already at high pressure bc directly from renal artery connected to aorta
ultrafiltration: what is the effect of increasing pressure in glomerulus
smaller molecules being carried in the blood is forced out of caps into bowman’s capsule, where they form filtrate
ultrafiltration: how is the glomerular capillaries separated from the lumen on Bowman’s
by 2 cell layers with a basement membrane:
first cell layer: endothelium of the capillary - each capillary endothelial cell is perforated by thousands of tiny membrane-lined circular holes
next layer: basement membrane - made up of network of collagen and glycoproteins
second cell layer: epithelium of bowman’s capsule - these epithelial cells have many tiny finger-like projections with gaps in between them known as podocytes
ultrafiltration: what happens as blood passes through the glomerular capillaries
the holes in cap endothelial cells and the gaps between podocytes allow substances dissolved in blood plasma to pass into bowman’s capsule
glomerular filtrate
glomerular filtrate
the fluid that filters through from the blood into bowman’s with main substances passing out:
amino acids
water
glucose
urea
inorganic ions (mainly Na+, K+, Cl-)
ultrafiltration: why do red and white blood cells and platelets remain in the blood
too large to pass through the holes in capillary endothelial cells
ultrafiltration: basement membrane
acts as filter as it stops large protein molecules from getting through
ultrafiltration diagram
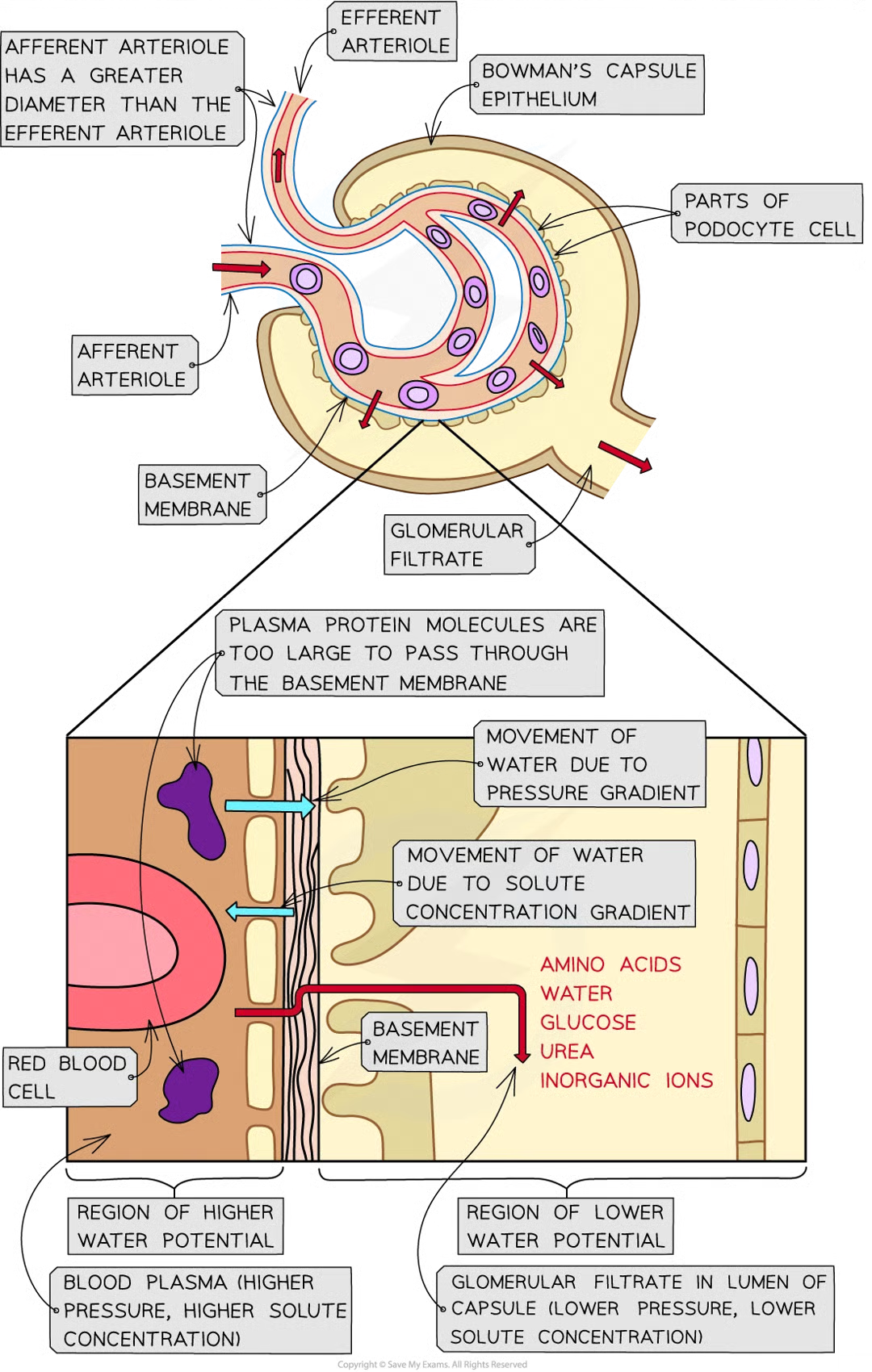
why does ultrafiltration occur
due to differences in water potential between plasma in the glomerular caps and the filtrate in the bowmans (water moves down water potential gradient, from region of high wp to lower wp. wp increased by high pressure, decreased by solutes)
2 factors affecting water potential
pressure
solute concentration
how pressure affects wp in glomerulus and bowmans
as afferent arteriole is wider than efferent, bp high in glom caps
wp of blood plasma in glom caps is raised above wp of filtarte in bowmans
water moves down wp gradient from blood plasma in glom caps into bowmans
how solute concentration affects wp in glom and bowmans
basement membs allow most solutes within blood plasma to filter into bowmans, plasma protein mols are too big to get thru and stay in blood
solute conc in blood plasma in glom caps higher than the filtrate in bowmans capsule
wp of blood plasma lower than that of filtrate in bowmans
water moves down wp gradient from bowmans cap into blood plasma in glom caps
the effect of pressure gradient outweighs…
effect of solute gradient, therefore wp of blood plasma in glom > wp of filtrate in bowmans so blood flows thru glom, overall movement of water down wp gradient from blood into the bowmans capsule
selective reabsorption
many of substances in glomerular filtarte need to be kept in body
substances reabsorbed into blood as filtrate passes along nephron
only certain substances reabsorbed
where is glucose reabsorbed
proximal convoluted tubule
lining of proximal convoluted tubule composition
single layer of epithelial cells
microvilli
co-transporter proteins
high number of mitochondria
tightly packed cells
where are water and salts reabsorbed
via loop of henle and collecting duct
4 adaptations of pct epithelial cells
many microvilli present on luminal membrane (cell surface membrane that faces lumen)
many co-transporter proteins in luminal membrane
many mitochondria
cells tightly packed together
how does many microvilli present help reabsorption
increases s.a. for reabsorption
how does cotransporter proteins help reabsorption
each type of co-transporter protein tarnsports specific solute (e.g. glucose or particular amino acid ) across luminal membrane
how does many mitoch help reabs
provide eneryg for sodium potassium pump proteins in basal membranes of cells
how do cells tightly packed help reabs
no fluid can pass between cells (all suibstances reabsorbed must pas through cells)
how does selective reabs occur
blood caps located close to outer surface of pct
as blood in caps comes staright from glomerulus it has very little plasma and has lost much of water, inorganic ions and other small solutes
basal membs of pct epithelial cells are sections of cell memb that are closest to the blood caps
na+k pumps in these basal membs move sodium ions of epithelial cells and into blood where they are carried away
this lowers conc of sodium ions inside epithelial cells so diffuse down conc grad through luminal memb from filtrate through cotarnsporter proteins in membrane
several cotarnsporters each tarnsports sodium ion and another solute from filtrate e.g. glucose or aa
once inside epithelial cells these solutes diffuse down conc grads passing thru transport proteins in basal membs into blood
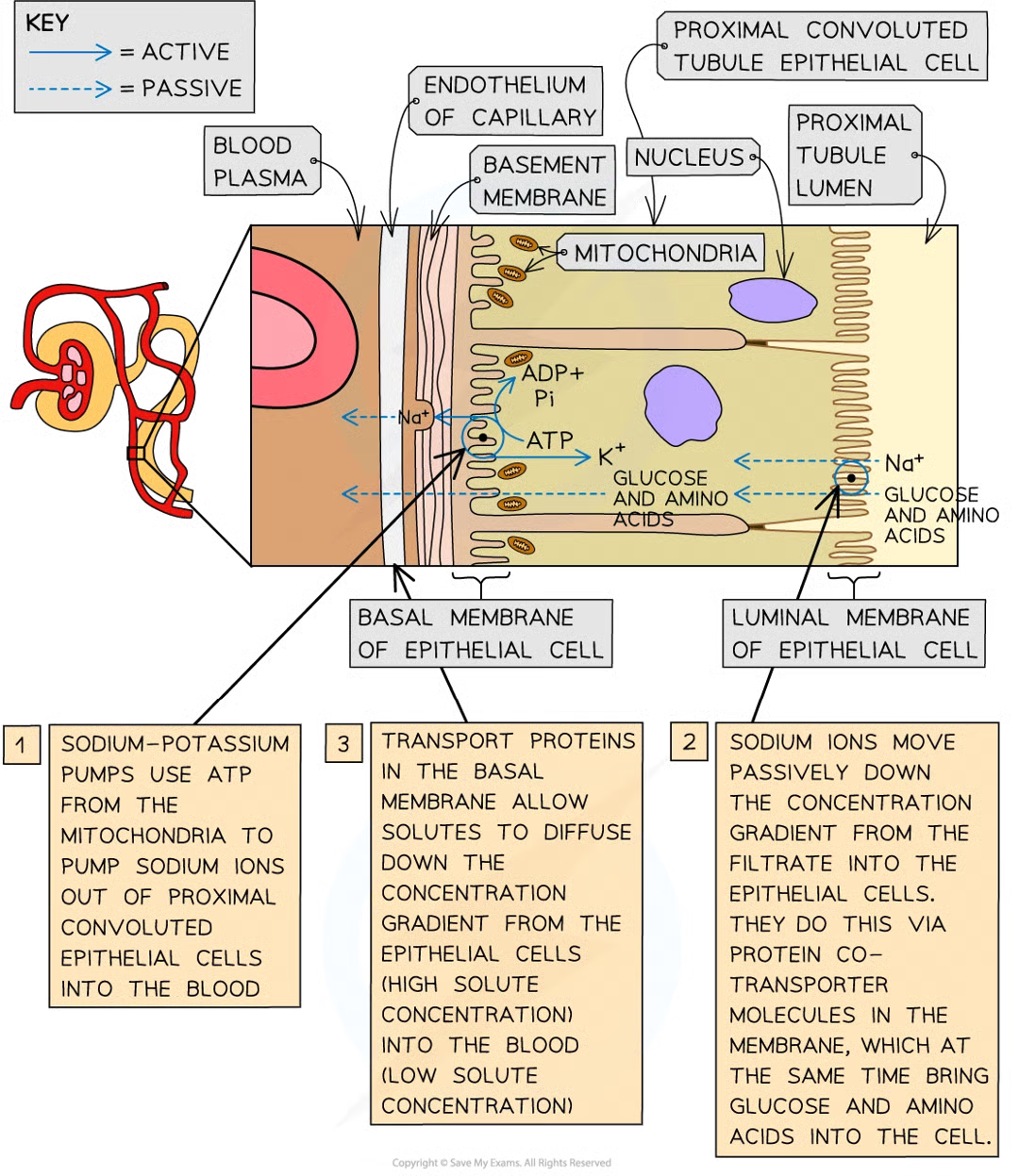
how much glucose is reabs from glom filtrate
ALL reabs into blood so none in urine
what is reabsorbed
glucose, aa, vitamins, inorganic ions
how is water potential gradient created and what is the effect
movement of all solutes from pct into caps increases wp of filtarte and decreases the wp of the blood in the caps. causes water to move into blood by osmosis
is urea reabsorbed
significant amount. conc of urea in filtrate higher than in caps causing urea to diffuse from filtrate back into blood.
how are salts and water reabs
filtrate drips thru loop of henle, necessary salts reabs back into blood by diffusion and water follows by osmosis and is reabsorbed
water also from colelcting duct in diff amts depending on how much water body needs at that time.
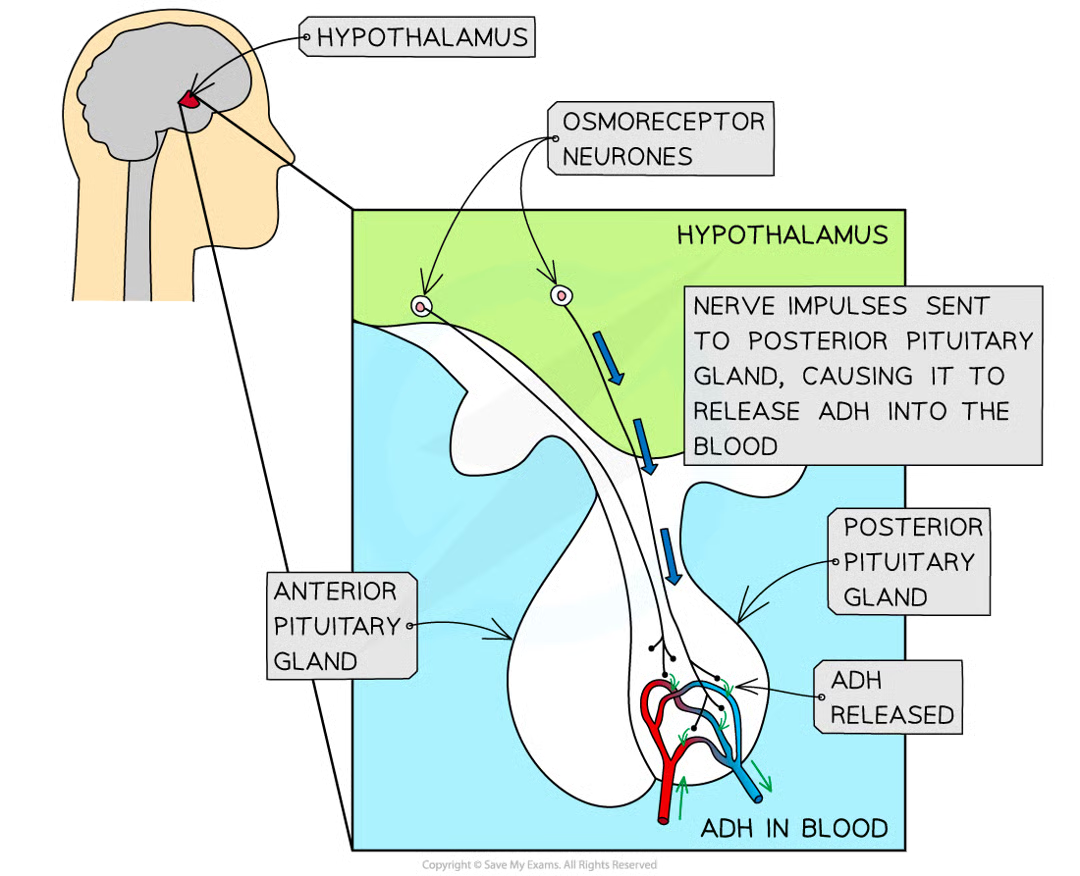
osmoregulation
control of water potential of body fluids, key part of homeostasis
what is involved in osmoregulation
specialised sensory neurones known as osmoreceptors which monitor wp of blood (found in hypothalamus)
what do osmoreceptors do
detect a decrease in wp of blood
nerve impulses sent along sensory neurones to posterior pituitary gland (below hypothal)
stimulate posterior pithuitary gland to release antidiuretic hormone (ADH)
adh enters blood and travels through body
adh causes kidneys to reabsorb more water
reduces loss of water in urine
effect of adh on the kidneys
water reabsorbed by osmosis from filtrate in nephron
reabs occurs as filtrate passes thru structures known as collecting ducts
adh causes luminal membs - those facing lumen of nephron- of collecting duct cells to become more permeable to water
adh does this by causing increase in no. aquaporins (water-permeable) in the luminal membranes of collecting duct cells
as the filtrate in nephron travels along the collecting duct, water move from collecting duct (high wp) through aquaporins into tissue fluid and blood plasma in medulla (low wp)
as filtrate in colelcting duct loses water it becomes more concentrated
small vol of concentrated urine is produced. flows from kidneys thru ureters and into bladder
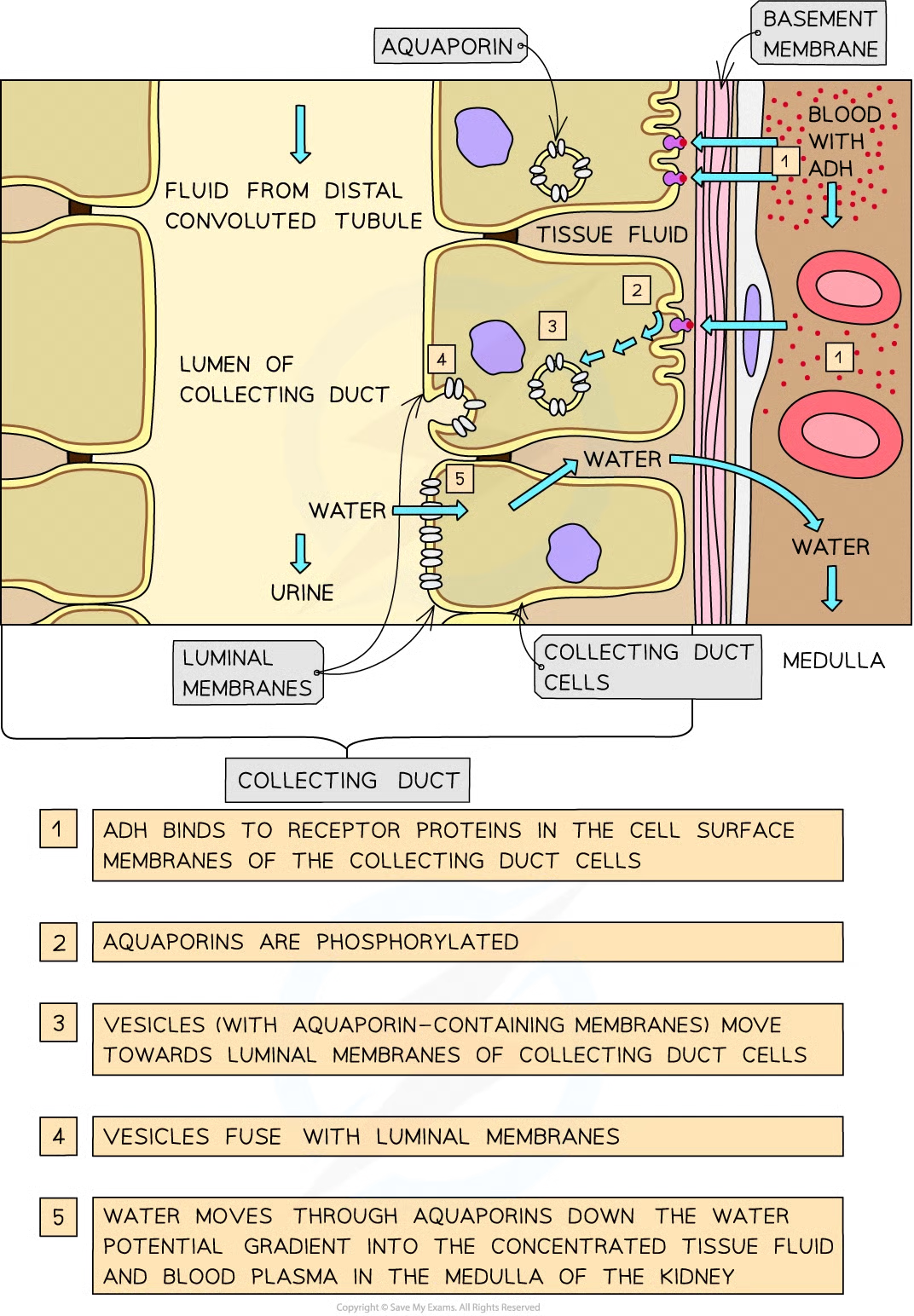
how does adh cause increase in no. aquaporins
collecting duct cells contain vesicles, teh membs of which contain many aquaporins
adh mols bind to receptor proteins activating signalling cascade that leads to phosphorylation of aquaporin mols
aquaporins activated = vesicles fuse with the luminalmembs of collecting duct cells
increases perm of membrane to water
what happens if wp of blood too high
osmoreceptors in hypothalamus not stimulated
no nerve impulses sent to posterior pituitary gland
no adh released
aquaporins moved out of luminal membranes of collecting duct cells
collecting diuict cells are no longer permeable to water
filtrate flows along collecting duct but loses no water as is very dilute
large vol of dilute urine produced
flows from kdineys through ureters and into bladder
why may cells not be able to function normally for resp
conc of glucoise in blood decreases below certain level so cells may not have enough glulcose for respirationwhy
why is it bad if conc of gluciose in blood increases above certain level
disrupts normal function of cells potentially causing major problems
what is blood glucose conc controlled by
2 hormones secreted by endocrine tissue in the pancrease made up of group cells = islets of Langerhans
2 cell types of islets of langerhans
alpha cells that secrete hormone glucagon
beta cells that secrete hormone insulin
what do alpha and beta cells do
act as receptors and initiate response for controlling blood glucose conc (cell signalling)
what do alpha and beta cells in pancrease do if decrease in blood glucoe conc occurs
they detect it
alpha secretes glucagon
beta stops the secreting of insulin
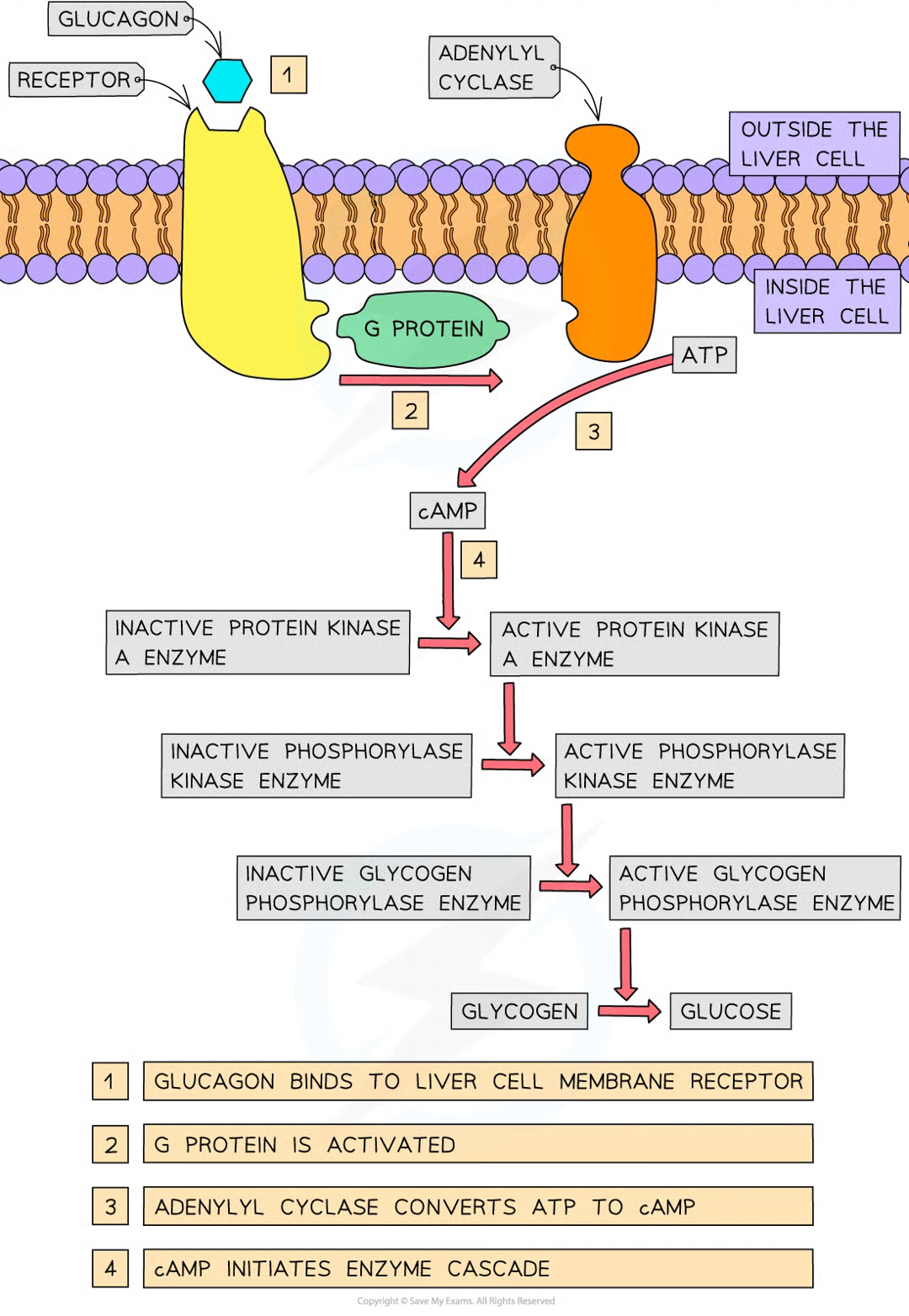
decrease of insulin conc and increase of glucagon conc effect
less insulin = reduces use of glucose by liver and muscle cells
glucagon binds to receptors in cell surface membranes of liver cells
binding causes conformational change in receptor protein that activates a g protein
activated g protein activates enzyme adenylyl cyclase
active adenylyl cyclase catalyses conversion of atp to second messenger = cyclic AMP
cAMP binds to protein kinase A enzymes, activating them
active protein kinase A enzymes activate phosphorylase kinase enzymes by adding phosphate groups to them
active phosphorylase kinase enzymes activate glycogen phosphorylase enzymes
active glycogen phosphorylase enzymems catalyse breakdown of glycogen to glucose (glycogenolysis)
amplifies og signal from glucagon and = extra glucose released by liver to increase blood glucose conc to normal level
what happens when blood glucose conc increases above normal range
detected by beta cells in pancrease
conc of glucose is high glucose mols enter beta cells by facilitated diffusion
cells respire glucose and produce atp
high conc atp causes potassium channels in beta cells to close producing change in membrane potential
this change in memb potential causes voltage-gated calcium cahnnels to open
influx of calcium ions so beta cells secrete insuline (insulin containing veiscles move towards csm where release insuiln into caps
once in blood insulin circulates around body
stimulates uptake of glucose by muscle cells fat cells and liver
what does insulin do
increase of uptake of glucose into target cells by binding to sepcific receptors on membranes of these target cells which stimulates the cells to add more glucose transporter proteins to their csm increasing the permeability of the cells to glucose
target cells of insuilin
muscle cells, fat storage cells, adipose tissue, liver cells (all have specific insulin receptors on csm)
glucose transporter proteins
glut proteins
when are glut proteins added
(high blood sugar) when insulin binds to surface receptors, vesicles move to csm and fuse iwth it
when are glut proteins stored
when blood glucose lvls are low, they are stored inside the membranes of vesicles
why does rate of facilitated diffusion of glucose into target cells increase
bc of increased glut proteins
what enzymes do insulin activate and what do they do
glucokinase - phosphorylates gluciose, trapping it inside cells
glycogemn synthase - glycogen synthase converts glucose into glycogen in a process knwon as glycogeneiss
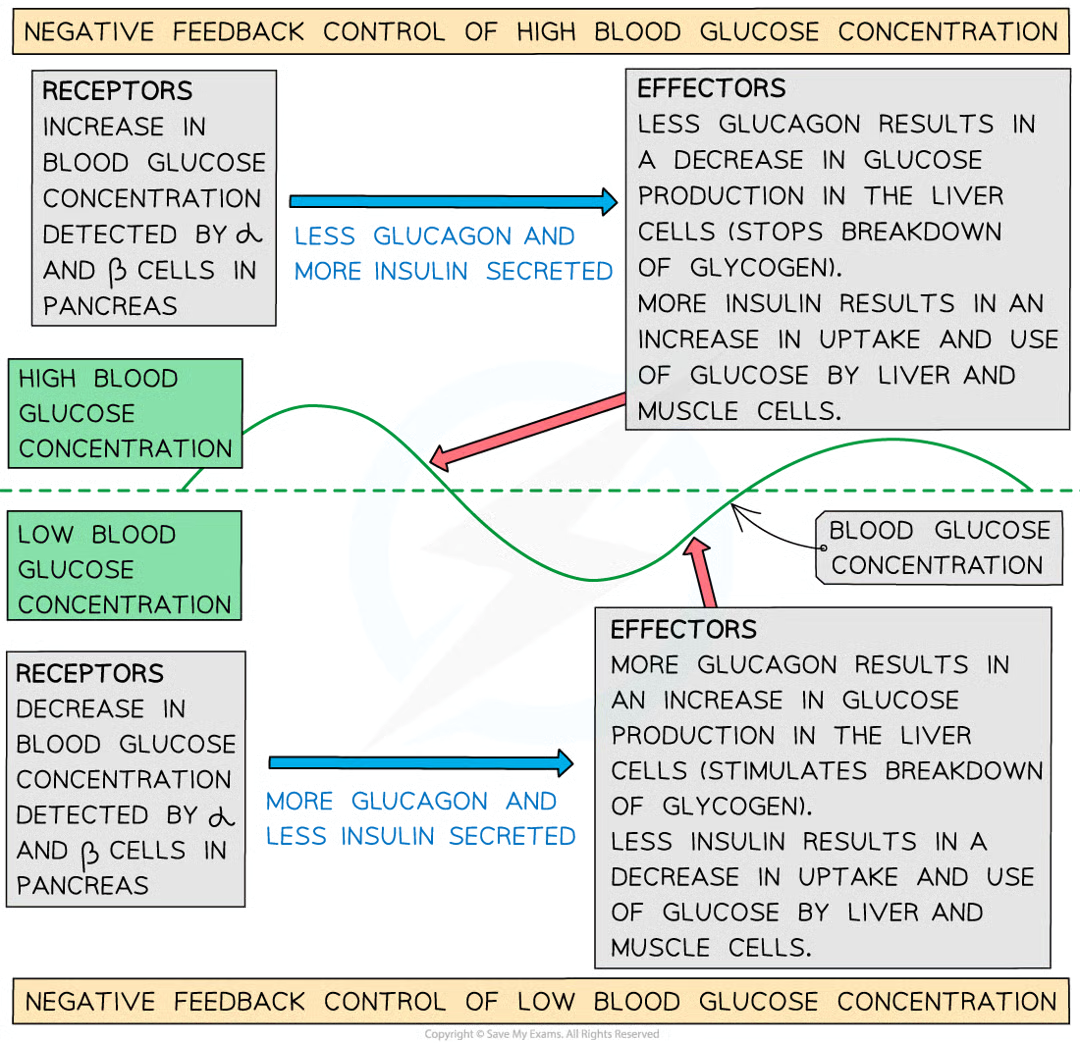
what is blood glucose conc reguilated by
negative feedback control mechanisms
what is the pattern for negative feedback systems:
recepetors detect whether specific level is too low ro too high
this info communicated thru hormonal or nervous system to effectors
effectors react to counteract change by bringing level back to normal
conntrol of blood glucose conc as negative feedback
alpha and beta cells in pancrease act as receptors
release hormones glucagong secreted by alpha cells and insulin secreted by beta cells
liver cells act as the effectors in response to glucagon and liver, muscle and fat cells act as the effectors in response to insulin
diabetes
people can’t control their blood glucose conc to remain within normal safe limits
indicator of diabetes
glucose in urine.
if blood conc increases above renal threshold…
not all glucose from filtrate in pct reabsorbed and some left in urine = presence of glucose in urine
what can test for presence of conc of glucose in urine
test strips
what is the test strip made up of
2 enzymes immobilised on small pad at one end of test strip:
glucose oxidase
peroxidase