Oral Pathology LO 10 part 1
1/52
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
53 Terms
Opportunistic diseases
Immunodeficiency can lead to ———————— diseases.
Endocrine system
The ———————— system consists of a group of integrated glands and cells that secrete hormones. The amount of hormone circulating in the blood triggers factors that control production.
Hyperpituitarism
Excess hormone production by the anterior pituitary gland. Caused most often by a benign tumour, a pituitary adenoma, that produces growth hormone. Gigantism results if it occurs before the closure of long bones before puberty. Acromegaly results when hypersecretion occurs during adult life- after puberty. What is this condition of the pituitary gland called?
Hyperpituitarism
Poor vision, light sensitivity, enlargement of hands and feet, increased rib size.
Enlargement of maxilla and mandible that may cause separation of the teeth and malocclusion. Frontal bossing and an enlargement of nasal bones, enlargement of maxillary sinuses leads to voice deepening.
May have thickened lips and macroglossia.
These are all clinical features of what condition?
Hyperthyroidism
This is an excessive production of thyroid hormone. More common in women than men, in 30s and 40s. Most common type is Graves' disease. Oral manifestations: may lead to premature exfoliation of deciduous teeth and premature eruption of permanent teeth, osteoporosis may affect alveolar bone, caries and periodontal disease may appear and develop more rapidly in these patients. Burning tongue.
Graves' disease
An autoimmune disorder in which antibodies, thyroid-stimulating immunoglobulins (THIs), stimulate thyroid cells. The thyroid gland enlarges. Too much thyroid hormone is produced, causing an increase in the patients metabolism. Clinical features: thyroid enlargement (goiter), rosy complexion, erythema of the palms, excessive sweating, fine hair, softened nails, Exophthalmos- bulging eyes, anxiety, weakness, restlessness, cardiac problems. Thyroid storm.
Thyroid storm
A serious flood of hormones that occurs during stress- can alter vitals and can be fatal. CAN HAPPEN IN DENTAL CHAIR. This condition is associated with hyperthyroidism.
Hypothyroidism
A decreased output of thyroid hormone. Most common endocrine condition. Causes include: developmental disturbances, autoimmune destruction of thyroid: Hashimoto thyroiditis, iodine deficiency, drugs, treatment for hyperthyroidism. Oral manifestations: infants: thickened lips, enlarged tongue, delayed eruption of teeth. Adults: enlarged tongue.
Hyperparathyroidism
Results from excessive secretion of parathyroid hormone (PTH) from the parathyroid glands. PTH plays a role in calcium and phosphorus metabolism. May be the result of hyperplasia of parathyroid glands, a benign tumours of one or more parathyroid glands, or a malignant parathyroid tumour. Much more common in women. PTH increases the uptake of dietary calcium from the GI tract and is able to move calcium from bone to circulating blood when necessary.
Hypercalcemia
This condition is associated with hyperparathyroidism. Elevated blood levels of calcium- can lead to muscle and heart problems.
Hypophosphatemia
This condition is associated with hyperparathyroidism. Low levels of blood phosphorus.
Hyperparathyroidism
Mild cases may be asymptomatic, or may cause joint pain or stiffness. Lethargy and coma may occur with severe disease. Kidney stones. Affects skeletal system and GI system. Oral manifestations: bone changes: loosening of teeth, well defined unilocular or multilocular radiolucencies. “Ground glass” appearance, loss of lamina dura, microscopically, lesions appear to be central gain cell granulomas (CGCGs). These are all clinical features of what condition?
Diabetes mellitus
A chronic disorder of carbohydrate metabolism characterized by abnormally high blood glucose levels. Results from a lack of insulin or defective insulin that does not work to lower blood glucose levels, or increased insulin resistance caused often by genetic factors/obesity.
Type I (no insulin), Type II (insulin resistance), Gestational (pregnancy), pre-diabetic. Hyperglycemia=high blood glucose levels.
Pancreas
Glucose signals beta cells of what organ to make insulin?
Ketoacidosis
Extremely high blood sugar levels can result in a life threatening condition called ————————. ———————— is the production of ketone acid that lowers the blood pH. Acute condition can lead to coma and death.
Immunosupression
When the blood pH is lowered due to Ketone acid, WBCs such as macrophages (phagocytic activity is reduced), neutrophils (chemotaxis is delayed), and lymphocytes are adversely affected. Uncontrolled diabetes leads to ——————————. ALWAYS ensure sugar levels are controlled before DH treatment.
126 mg/dL
To diagnose someone as diabetic, their fasting blood glucose would be greater than or equal to ——— mg/dL.
100-125
To diagnose someone as prediabetic, their fasting blood glucose would be between ——— and ——— mg/dL.
Type 1: insulin dependant diabetes mellitus (IDDM)
This condition is thought to be an autoimmune disease. Associated with Addison disease, Graves' disease, and pernicious anemia. Insulin-producing cells of the pancreas (beta cells) are destroyed. This is the least common type of diabetes, but most severe. Can occur at any age; the peak is at 20 years. Polydisia, polyuria, and polyphagia are associated with this condition. Patients require insulin their entire lives
Polydipsia
Excessive thirst and intake of fluid.
Polyuria
Excessive urination.
Polyphagia
Excessive appetite.
Type 2: Non-insulin dependant diabetes mellitus (NIDDM)
This condition is characterized by insulin resistance. 97% of all diabetic patients have this type of diabetes (most common type). Gradual onset. Usually occurs in patients 35-40 years of age or older. Role of dentists and dental hygienists: patient education on periodontal/infection risk.
Gestational diabetes (GD)
This occurs during pregnancy. Results in high blood sugar levels affecting fetus development. Disappears after pregnancy in most cases. Increased birth weight of child is likely. Mother and child have a higher risk of developing type 2 diabetes later in life.
Diabetes type 2
Atherosclerosis, a thickening of blood vessel wall from fibrofatty plaques, can lead to impaired circulation, causing impaired oxygenation and nutrition in tissue. This increases the risk of ulceration and gangrene of the feet, high blood pressure, kidney failure, and stroke. Diabetic retinopathy in the eye can lead to blindness. The nervous system may be affected. The person may have decreased resistance to infection. Oral complications: candidiasis, mucorycosis: a rare oral fungal infection that affects the palate and maxillary sinuses. Bilateral asymptomatic parotid glans enlargement, Xerostomia, periodontal disease, accentuated response to plaque, slow wound healing, increased susceptibility to infection. These are all clinical features of what condition?
Addison disease (primary hypoadrenocorticism)
Insufficient production of adrenal steroids. Causes adrenal gland destruction include: malignant tumour, tuberculosis, deep fungal infections, HIV infection, autoimmune disease, unknown. To compensate, the pituitary gland increases production of adrenocorticotropic hormone (ACTH). Clinical features of this disease: stimulation of melanocytes- bronzing of the skin, melanotic macules on oral mucosa. Tx: steroid replacement therapy.
Hypercortisolism (Cushing Syndrome)
This disorder is caused by sustained increase in glucocorticosteroid levels. Signs develop slowly. Weight gain is the most significant and obvious clinical feature. Other signs include: hypertension, hyperglycemia, mood alterations, decreased ability to respond to stress.
Anemia
A reduction in the oxygen carrying capacity of blood. Results in oxygen deprivation of tissues "oxygen debt". Most often related to a decrease in the numbers of circulating RBCs.
Nutritional —————s: iron, folic acid, vitamin B12.
Suppression of bone marrow in stem cells.
Clinical features: pallor of the skin and oral mucosa, angular cheilitis, erythema and atrophy of oral mucosa, loss of filiform and fungiform papillae of the dorsum of the tongue.
Iron deficiency anemia
An insufficient amount of iron is supplied to bone marrow for RBC development. Most common form of anemia. Possible causes: iron deficiency in diet, blood loss, poor absorption, pregnancy/infancy.
Plummer-vision syndrome
This condition may result from long-standing iron deficiency anemia. Symptoms include: nonspecific (weakness, fatigue), shortness of breath, cardiac palpitations, dysphagia, glossitis, angular cheilitis exacerbated by oral candidiasis, atrophy of papilla on dorsal of tongue, atrophy of upper alimentary tract (mouth, pharynx, larynx, etc.), predisposition to developing esophageal and oral cancer.
Hematocrit
This is the volume of RBCs in the blood.
Microcytic
If your red blood cells are smaller than normal, they are:
Hypochromic
If your RBCs are lighter in colour than normal, they are:
Pernicious anemia
Anemia caused by deficiency in intrinsic factor. Intrinsic factor is secreted by parietal cells in the stomach; it is necessary for absorption of vitamin B12. Probably an autoimmune disorder in most situations. May be caused by removal of stomach, gastric cancer, or gastritis. Vitamin B12 is not absorbed well as a result. Vitamin B12 is needed for DNA synthesis.
Lack of DNA synthesis, unable to turnover epithelium.
Why would someone with pernicious anemia get mucosal ulceration?
Megaloblastic anemia
Immature abnormally large RBCs with megaloblasts (nuclei); immature and non-functioning. (Pernicious anemia is a version of this type of anemia).
Lack of hydrochloric acid
A person who has pernicious anemia would have their blood tests show gastric achlorhydria. What does that mean?
Folic acid and vitamin B12 deficiency anemia.
These 2 types of anemia are from dietary deficiencies. Is association with malnutrition and increased metabolic requirements. May be found with alcoholism or pregnancy.
Thalassemia
A group of inherited disorders of hemoglobin synthesis. Results in insufficient hemoglobin and reduced blood oxygen levels. An autosomal dominant inheritance pattern. Clinical features: yellow skin pallor, fever, malaise, weakness, enlarged spleen and liver, prominent cheekbones, depression of the bridge of the nose, prominent maxilla, protrusion or flaring of maxillary anterior teeth, thinning of lamina dura, and circular radiolucencies in alveolar bone.
Hemochromatosis
Deposition of excessive iron throughout the body.
Chelation
This is a therapy to help remove excess iron in the blood.
Sickle cell anemia
Inherited blood disorder, predominantly in black individuals and those of Mediterranean or Asian origin. Occurs before age 30 and is more common in women than men. RBCs develop a sickle shape when there is decreased oxygen. Can be triggered by exercise, exertion, administration of general anesthetic, pregnancy, or stress. The cells dump together and form a clot, this is known as a sickle cell crisis.
Aplastic anemia
A severe depression of bone marrow activity causes a decrease in all circulating blood cells. Leads to oxygen deprivation. Primary ————— anemia: unknown cause. Secondary ————— anemia: result of a drug or chemical agent. Clinical manifestations: fatigue, weakness, tachycardia, low platelets: bruising, hematomas, retinal and cerebral hemorrhages, predisposed to infections.
Aplastic anemia
Infection, spontaneous bleeding, petechiae, purpuric spots, ecchymosis. These are all oral manifestations of what condition?
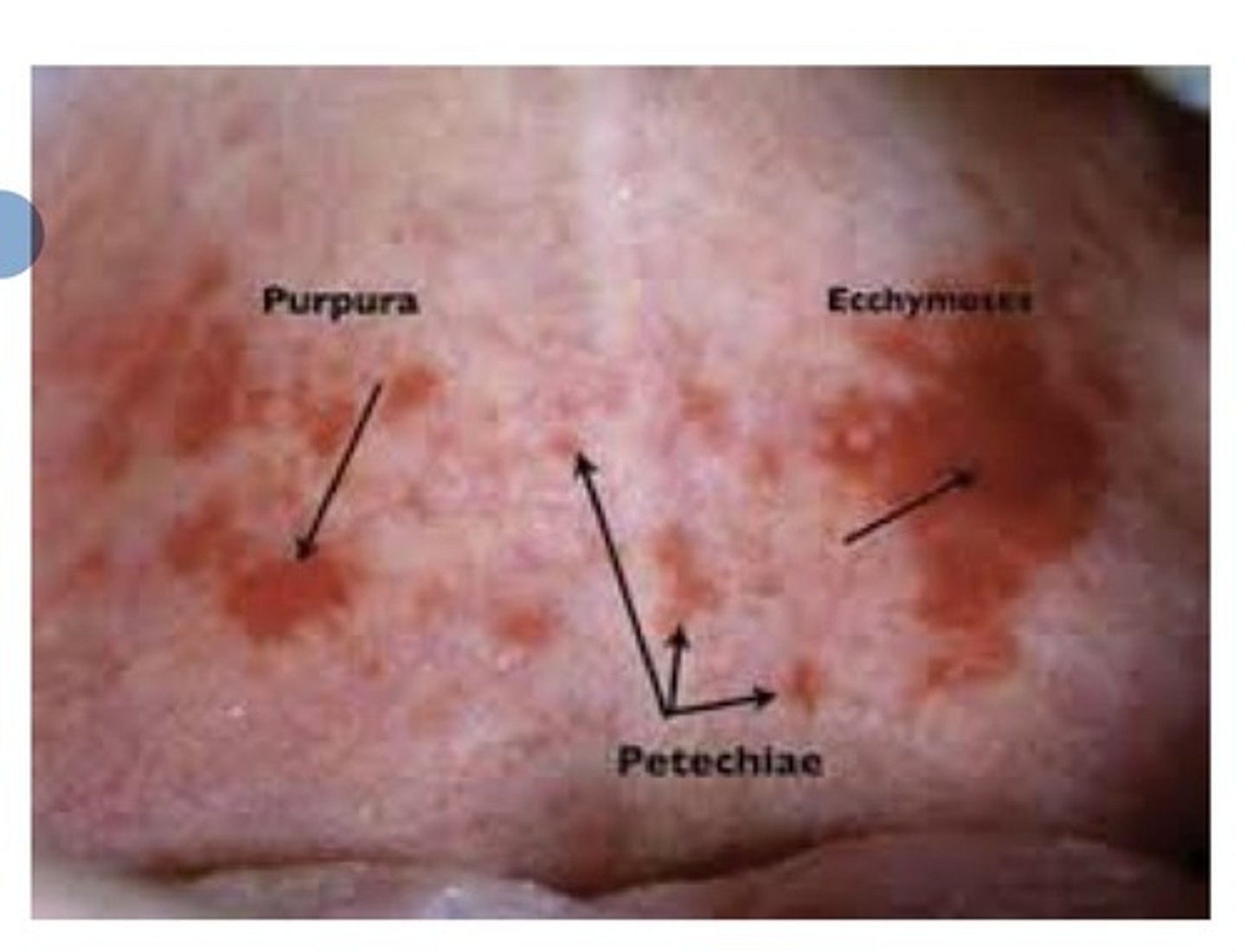
0-4mm
Petechiae are pinpoint areas of subdural blood collection. They are — to — mm.
1cm+
Ecchymosis is large areas of subdural blood collection, how large are these areas?
4-10mm
Purpuric spots are — to —mm large areas of subdural blood collection.
WBCs
Leukopenia is a decrease in:
Thrombocytopenia
This is a decrease in platelets
Primary
————— aplastic anemia is usually progressive and fatal.
Secondary
——————— aplastic anemia usually involves removing the cause.
Polycythemia
Characterized by increase in the number of circulating RBCs. There are 3 forms:
———————— Vera: primary ————————
Secondary ————————
And relative ————————.
Primary polycythemia (polycythemia Vera)