Autonomic Nervous System (ANS)
1/107
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
108 Terms
Spinal Nerve
Group of nerve axons travelling together.
Contains the axons of different neurons.
FFF - Eyes
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
There is a dilation in the pupils and adjustment for far vision in this organ.
Allows you to scan the area.
FFF - Cardiovascular
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
Heart rate increases and force of contraction also increases, allowing more blood to be pumped to the skeletal muscle.
The ventricular myocardium receives only sympathetic innervation; the atrial myocardium receives both.
FFF - Blood Vessels (Arterioles + Veins)
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
BVs are composed of smooth muscle. The smooth muscle will constrict, regulating our BP.
FFF - Blood Vessels (Skeletal Muscle)
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
The smooth muscle will relax; it will dilate for more blood flow.
For oxygen increase.
FFF - Lungs
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
Bronchioles dilate and increase passage of air to reach lungs.
Inhibition of mucus secretion, making it easier to breathe.
FFF - Digestion
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
Even if there is food in the stomach, there is decreased GI motility and inhibition of digestive secretions.
FFF - Exocrine
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
Glands which release their secretions into ducts.
i.e. the sweat glands are stimulated, saliva is produced, but much thicker and rich.
FFF - Bladder
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
The bladder does not empty during sympathetic conditions (prevents voiding).
Urination during situations of extreme fear is not the sympathetic NS, but occurs due to the activation of both the sympathetic NS and the parasympathetic NS.
FFF - Endocrine
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
Releases epinephrine and norepinephrine.
FFF - Genitals
In the sympathetic fight, flight, or freeze response, particular responses are triggered across many different organs.
Males ejaculate and females contract their uterus.
Adrenal Gland
Composed of a outer cortex and inner medulla.
The adrenal medulla and cortex secrete different substances.
Receives only sympathetic innervation, not parasympathetic innervation.
Innervated by sympathetic preganglionic neurons.
Preganglionic Synapse at the Adrenal Medulla
Cell body in the CNS.
Short axon which innervates the adrenal medulla.
Neurotransmitter released from the pre-ganglionic neuron binds to receptors on the adrenal medulla, causing it to release its secretions into the bloodstream.
Releases epinephrine and norepinephrine.
Bloodstream to Adrenal Medulla
There is no postganglionic neuron.
The adrenal medulla itself acts like a modified sympathetic post-ganglionic neuron, but it does not have a axon or cell body.
The pre-ganglionic neuron innervates the adrenal medulla.
Effects of E and NE
By travelling in the blood, epinephrine and norepinephrine can each organs that do not receive nervous innervation.
They must first travel to the liver to be broken down, their effects on body tissues last longer.
Until the liver breaks them down, they remain active in the bloodstream, continuing to act on tissues.
Autonomic
Autonomous, carries out its functions involuntarily.
Autonomic Nervous System
Maintenance of homeostasis.
Components of the ANS are regulators which maintain a constant thermal environment.
Activation of emergency mechanisms (i.e. response to stress).
Housekeeping functions (i.e. digestion).
Fight or flight.
Peripheral Nervous System (PNS)
Carries information detected by receptors (i.e. pain or sound) to the CNS.
Carries information from the CNS to effectors, such as glands and muscles that carry out motions directed by the CNS.
Afferent/Sensory Division
Comprises of afferent nerves that carries information from the sensory receptors towards the CNS.
Includes touch, pain, and temperature, summarized under “somatosensory.”
Further divided into three systems: somatic sensory, visceral sensory, and special sensory.
Efferent/Motor Division
Divided into two different systems: somatic motor and autonomic motor.
Somatic motor:
Controls the voluntary movement of skeletal muscle and mediation of voluntary reflex arc.
Somatic Motor Division
Controls the voluntary movement of skeletal muscle and mediation of voluntary reflex arc.
Stems from the efferent/motor division.
Autonomic Motor Division
Further split into the sympathetic, parasympathetic, and enteric system.
Affects smooth muscle, cardiac muscle, and glands.
Stems from the efferent/motor division.
Enteric System
A nerve network in the walls of the GI tract innervated by autonomic nerves.
A part of the autonomic motor system.
Afferent Neurons
Relay sensory information to the CNS.
Efferent Neurons
Relay motor commands from the CNS to target tissues.
Cranial Nerves
Nerves that emerge directly from the brain, including the brainstem.
Does not emerge from the spinal cord.
There are 12 pairs, attached at the brain (including brainstem(=).
Contains both afferent and efferent fibers.
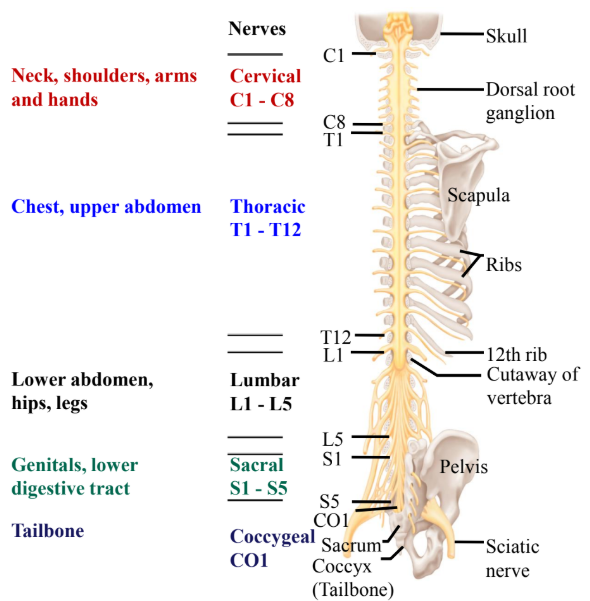
Spinal Nerves
31 pairs of spinal nerves that connect with the spinal cord.
Contains both afferent and efferent fibers.
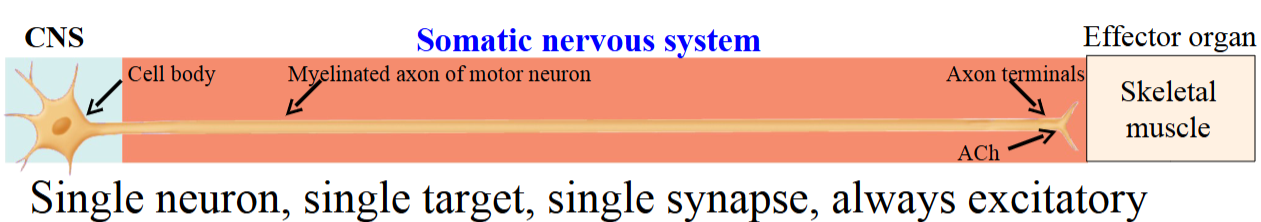
Somatic Efferent Nerves - 1
In the somatic nervous system (NS), motor information is transmitted from the CNS to skeletal muscle.
The somatic NS uses a single neuron, forming one synapse directly on the muscle.
Somatic motor neuron axons travel in cranial and spinal nerves to the muscle.
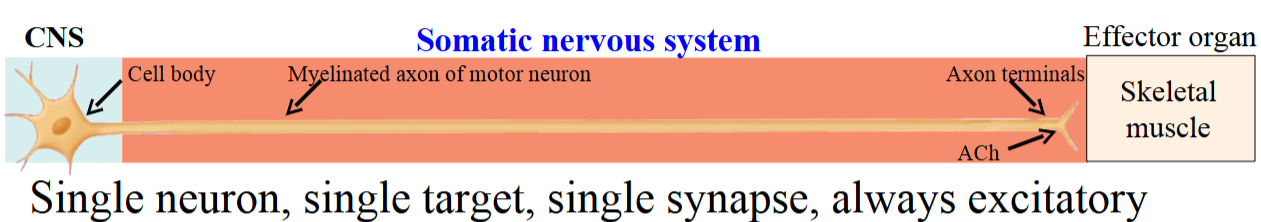
Somatic Efferent Nerves - 2
Activation of the neuron causes skeletal muscle contraction by releasing acetylcholine (ACh) at the axon terminals.
Inhibition of muscle contraction occurs in the CNS, not at the muscle.
Somatic afferent neuron axons are large and myelinated, allowing fast conduction.
Conduction in the somatic NS is faster than in the autonomic NS.
Autonomic Efferent Nerves - 1
Each autonomic pathway includes a preganglionic neuron with its cell body in the CNS.
The preganglionic axon extends to a ganglion, where it synapses with the postganglionic neuron.
Preganglionic axons are thinly myelinated; postganglionic axons are unmyelinated.
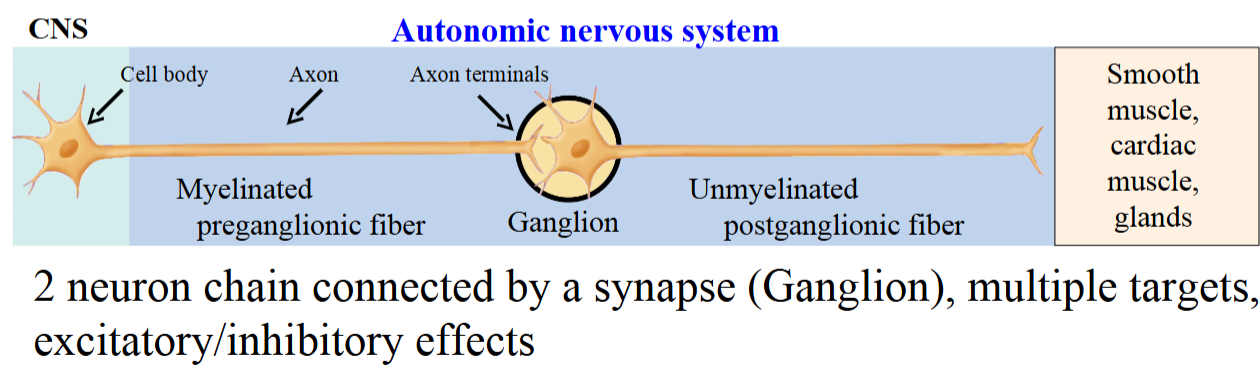
Autonomic Efferent Nerves - 2
Cell bodies of postganglionic neurons are clustered together in a structure named autonomic ganglia.
Over evolution, the postganglionic fiber lost its myelin, as ANS transmission does not need to be as fast as in the somatic NS.
Motor information travels from the CNS to target organs: smooth muscle, cardiac muscle, or glands.
The ANS can either excite or inhibit its targets.
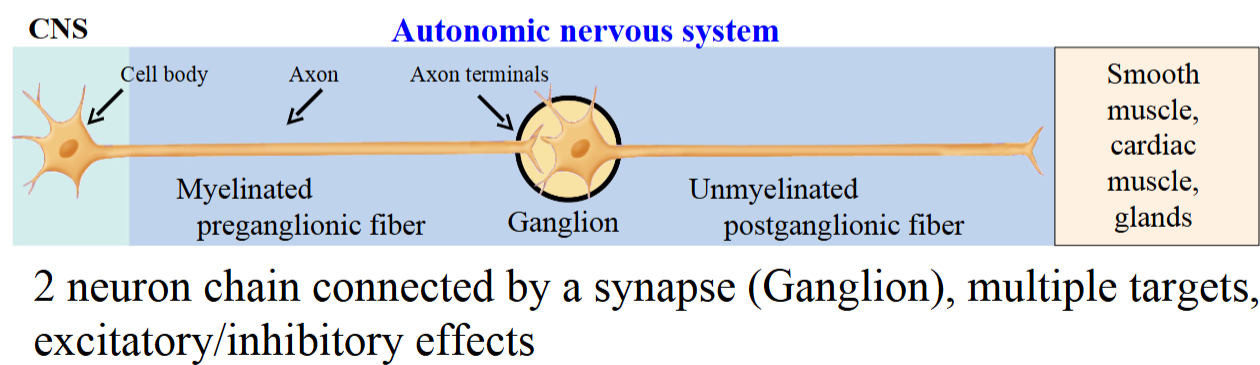
Ganglion
Cluster of neuron cell bodies outside the CNS.
Somatic vs. Autonomic
Somatic | Autonomic | |
Control | Voluntary | Involuntary |
Effector Organ | Skeletal muscle | Smooth muscle, cardiac muscle, glands |
Response | Always excitatory (leads to connection) | Excitatory or inhibitory |
Efferent (motor) Pathway | One neuron | Two neuron chain connected by ganglion. |
Neurotransmitter | Acetylcholine (ACh) | ACh, norepinephrine, epinephrine, many others |
Myelination | Myelinated Fiber | Myelinated preganglionic fiber, unmyelinated postganglionic fiber |
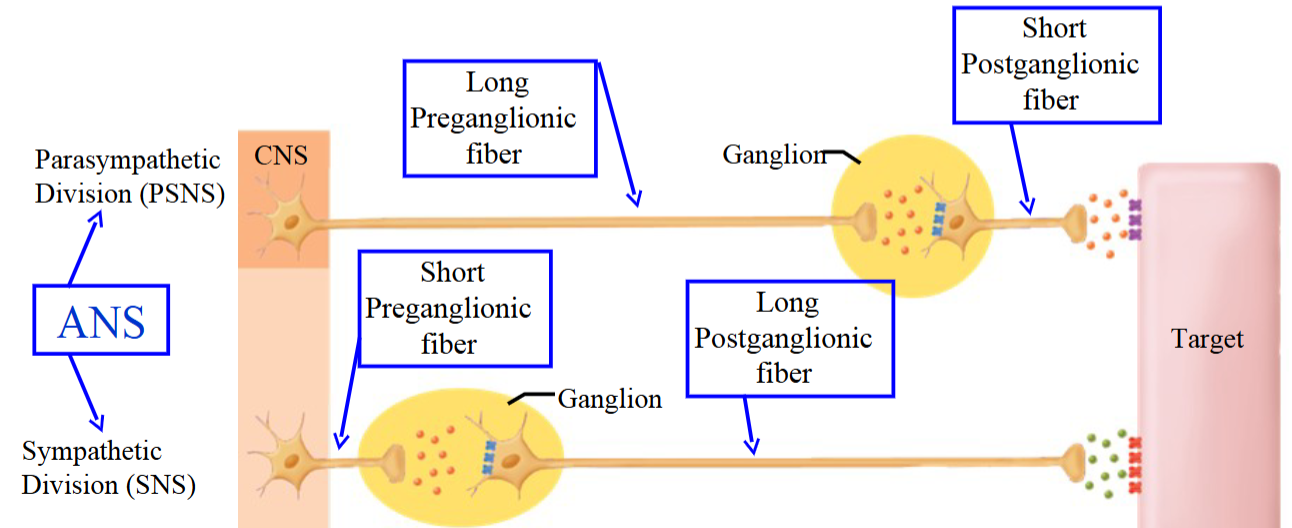
Sympathetic - Axon Length
Extensive branching allows for mass discharge, activating many organs at once.
Preganglionic neurons are short, synapsing at ganglia near the spinal cord.
Postganglionic neurons are long, extending to target organs.
This setup enables a non-isolated presynaptic response, where one neuron can influence many postganglionic fibers.
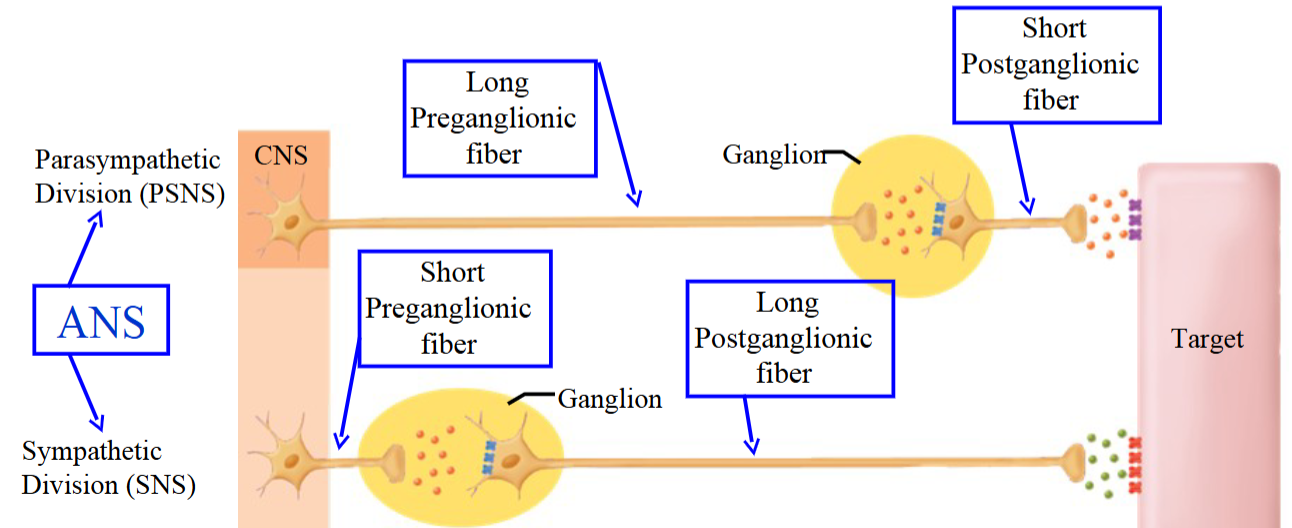
Parasympathetic - Axon Length
Ganglia are located very deep or within the walls of the target organ.
The preganglionic fiber is long due to the distance from the spinal cord to the ganglion.
The postganglionic fiber is short, as it only covers a small distance to the target.
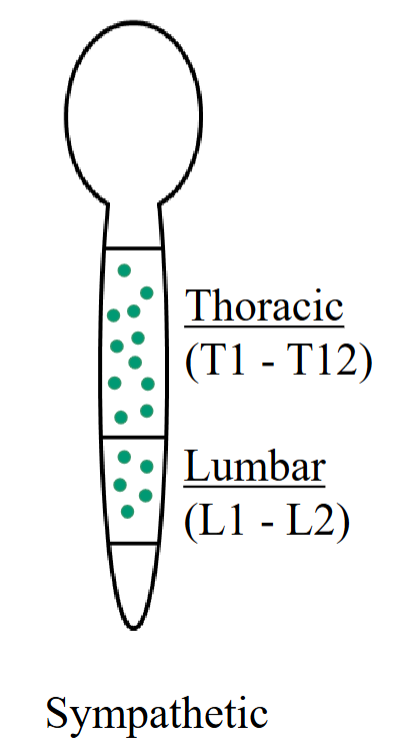
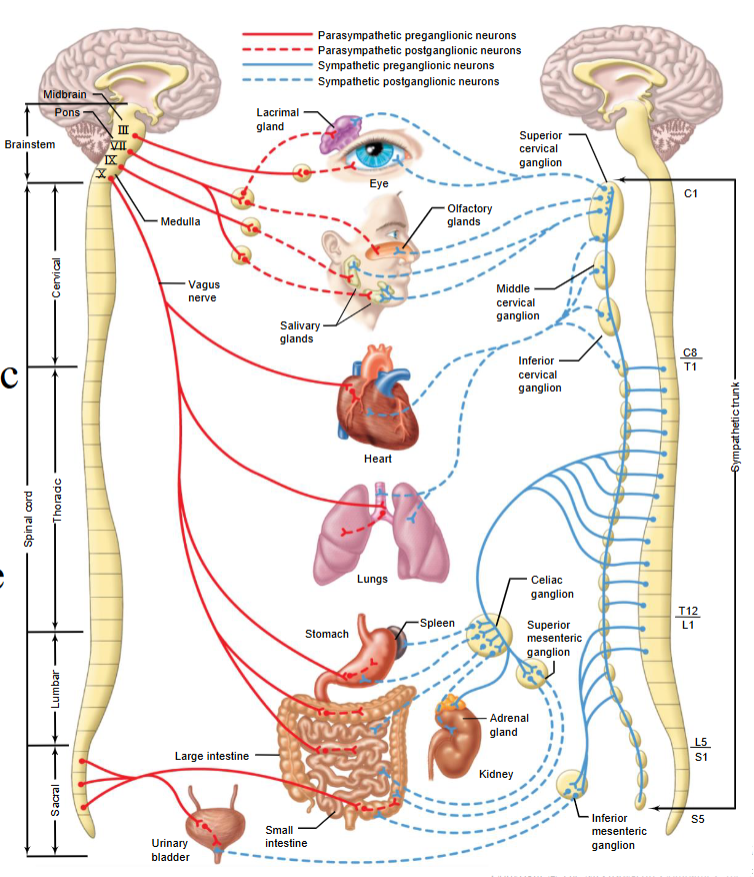
Cell Bodies of Preganglionic Fibers - Sympathetic
The cell bodies of the first neuron are found in the thoracic and lumbar regions of the spinal cord.
The cell bodies are found in the thoracic region from T1-T12.
In the lumbar region as well, from L1-L2.
Also called the thoracolumbar division.
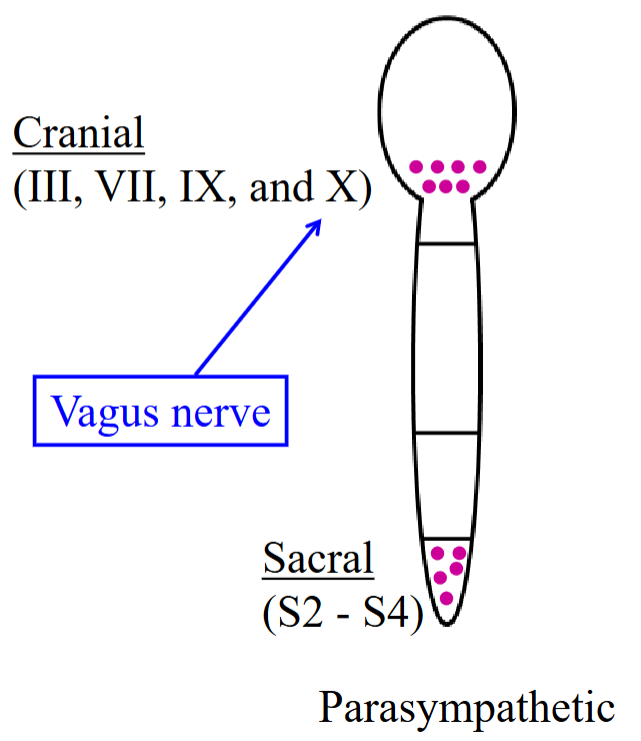
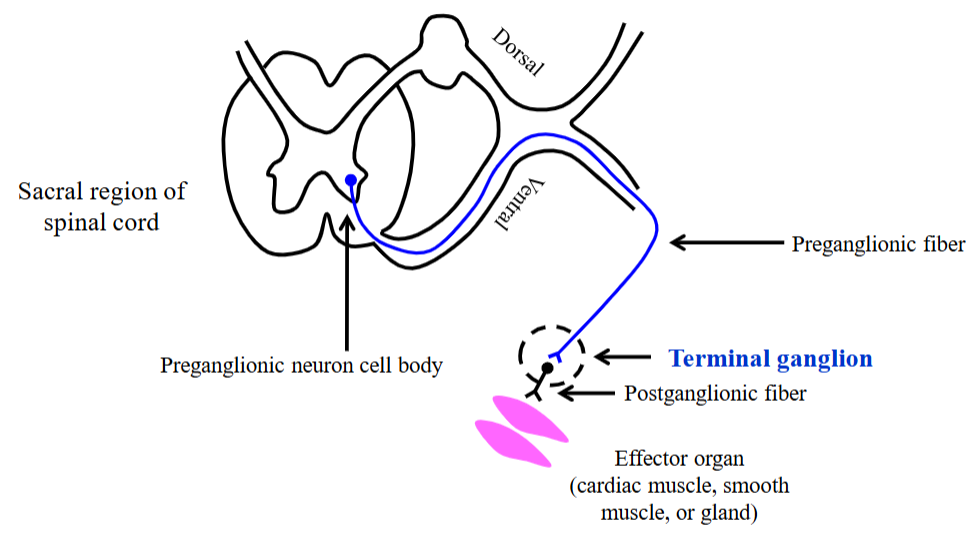
Cell Bodies of Preganglionic Fibers - Parasympathetic
Cell bodies are found in the cranial and sacral regions.
Brainstem and sacral region (spinal cord).
The axons of parasympathetic preganglionic fibers are contained in cranial nerves 3, 7, 9, 10.
Cell bodies of the first neuron are also found in the sacral region, S2-S4.
Thoracolumbar Nervous System
Originate in thoracic and lumbar regions (T1-T12; L1, L2).
Autonomic neurons carry motor information to their target tissues: smooth muscle, cardiac muscle, or glands.
These neurons regulate the contraction or activity of these tissues.
Part of the sympathetic nervous system.
Sympathetic Trunk/Chain
Have a special anatomical arrangement; lined into a chain pattern running parallel to the spinal cord on each side.
One of paired chains of interconnected sympathetic ganglia that lie on either side of the vertebral column.
Also called the paravertebral ganglion.
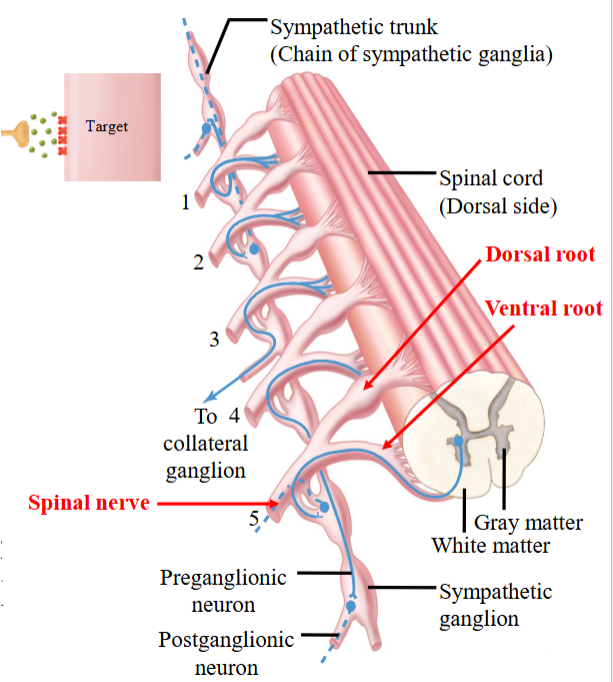
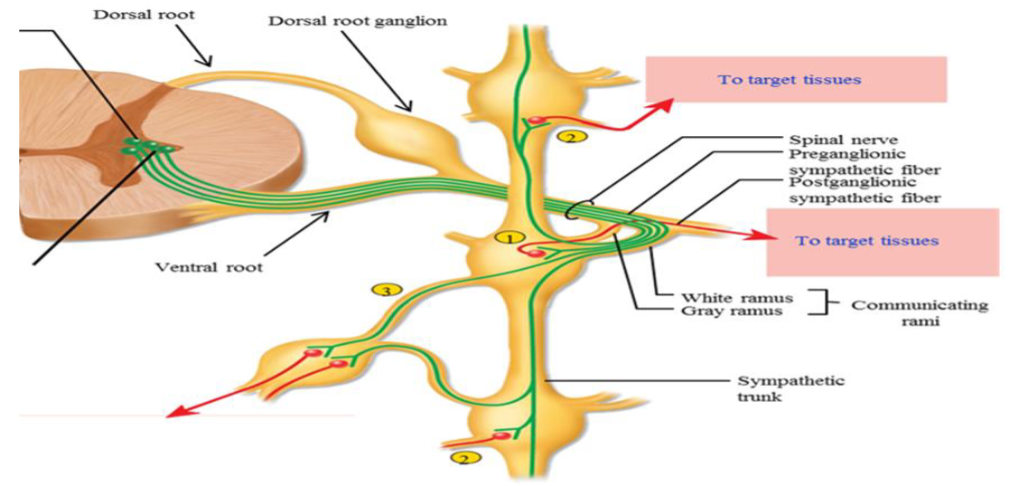
Sympathetic Preganglionic Axon - Spinal Nerve
The spinal nerve is formed where the dorsal and ventral roots combine.
The axon of the preganglionic neuron leaves the spinal cord through the ventral root.
After exiting via the ventral root, the axon leaves the spinal nerve and enters the sympathetic trunk.
Step 1.
Sympathetic Preganglionic Axon - Trunk
Once inside the sympathetic trunk, the preganglionic axon can take different possible routes:
Synapse at the same level.
Travel up or down the trunk and synapse at a different level.
Pass through without synapsing and synapse farther away, in front of the vertebrae.
Step 2.
Sympathetic Preganglionic Axon - Alternate Pathway (1)
A sympathetic preganglionic fiber leaves the spinal cord.
It passes through the sympathetic trunk without synapsing.
The fiber enters a splanchnic nerve.
It travels to a collateral (prevertebral) ganglion.
Sympathetic Preganglionic Axon - Alternate Pathway (2)
In the collateral ganglion, the fiber synapses with a postganglionic neuron.
Collateral ganglia are located near the viscera, important for innervating abdominal and pelvic organs.
The postganglionic fiber then travels to the target tissue.
Collateral Ganglion
Sympathetic ganglia located in front of the vertebral column, outside the sympathetic chain, near the viscera and arteries.
Celiac ganglion, superior mesenteric ganglion, and inferior mesenteric ganglion.
Innervates abdominal and pelvic viscera.
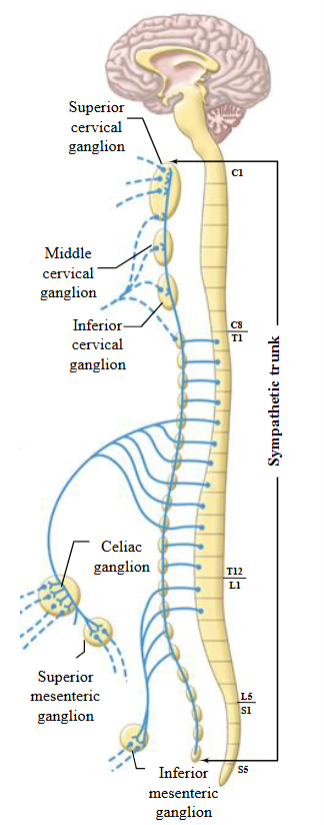
Sympathetic Neural Pathways
Synapse immediately with a post-ganglionic neuron in the sympathetic ganglion.
Travels up or down the chain and synapses in ganglia at other levels.
Pass through chain without synapsing, continue to collateral ganglion as splanchnic nerve.
Communicating Rami
Two branches which connect a paravertebral ganglion to a spinal nerve; includes white and gray rami.
Allows for communication because of the nerve fibers that travel between them.
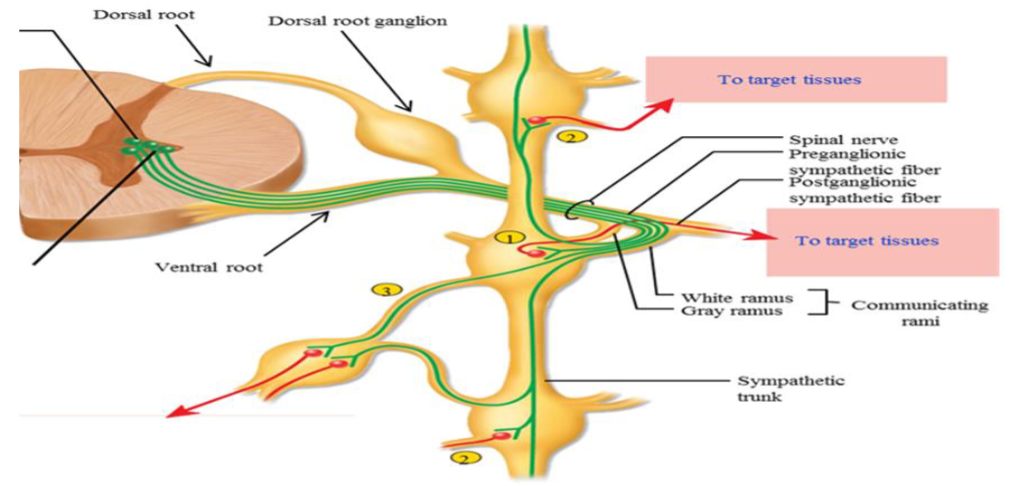
White Rami
Branch by which a myelinated preganglionic fiber leaves spinal nerve and enters a sympathetic ganglion.
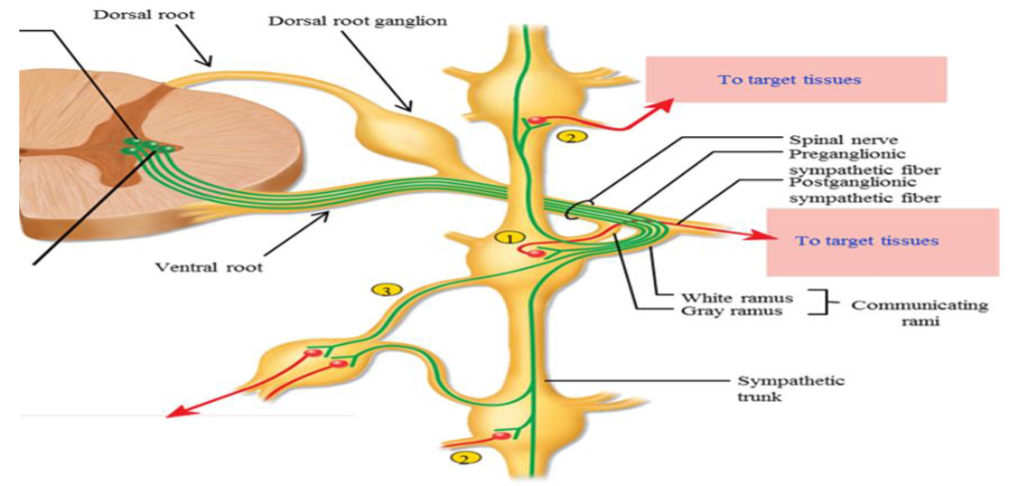
Gray Rami
Branch by which unmyelinated post-ganglionic fibers leave the ganglion to re-enter the spinal nerve.
Craniosacral Nervous System
Originate in brainstem and sacral regions (cranial nerves III, VII, IX, X and S2-S4).
Supply the visceral structures in the head by the oculomotor (III), facial (VII), glossopharyngeal (IX) nerves and the thorax and upper abdomen by the Vagus (X) nerve.
Vagus Nerve
Carries 75% of all parasympathetic fibers.
Innervates heart, lungs, and regions of the intestinal tract.
Terminal Ganglion
A parasympathetic ganglion situated on or close to an innervated organ, the site where preganglionic nerve fibers terminate.
Parasympathetic Ganglionic Pathway
The ganglia, where the preganglionic fiber synapses with the postganglionic fiber is close to the effector organ.
May even be in the walls of the effector organ.
Preganglionic fiber is long and the postganglionic fiber is short.
Parasympathetic Pathway
Leaves the central root and travels to the target tissue, synapsing with the postganglionic fiber at a terminal ganglion.
This ganglion is located near or within the walls of the target tissue.
It is a two-neuron chain with a long preganglionic fiber and a short postganglionic fiber.
R&D - Eyes
Certain organs are impacted by the parasympathetic 'rest and digest' response.
Constriction of pupils and adjustment for near vision.
Regulates the amount of light getting in.
R&D - Cardiovascular
Certain organs are impacted by the parasympathetic 'rest and digest' response.
Heart rate decreases, and the force of contraction in the atrial myocardium is reduced.
The ventricular myocardium receives only sympathetic innervation.
The atrial myocardium receives both sympathetic and parasympathetic innervation.
R&D - Lungs
Certain organs are impacted by the parasympathetic 'rest and digest' response.
The rate of breathing is relaxed, there is a constriction of bronchioles.
R&D - Blood Vessels
Certain organs are impacted by the parasympathetic 'rest and digest' response.
Some BVs are composed of smooth muscle → can change its constriction to alter the diameter of the BV.
There is no innervation.
Exceptions include the penis and clitoris, which the BVs dilate.
R&D - Digestion
Certain organs are impacted by the parasympathetic 'rest and digest' response.
Increased motility, stimulation of digestive secretions.
R&D - Endocrine
Certain organs are impacted by the parasympathetic 'rest and digest' response.
There is no response from the adrenal medulla.
R&D - Exocrine Glands
Certain organs are impacted by the parasympathetic 'rest and digest' response.
Parasympathetic system has no effect on the sweat glands.
Stimulation of large volume of watery saliva, rich in enzymes.
R&D - Bladder
Certain organs are impacted by the parasympathetic 'rest and digest' response.
There is emptying of the bladder in parasympathetic stimulation.
R&D - Genitals
Certain organs are impacted by the parasympathetic 'rest and digest' response.
Under parasympathetic stimulation, the blood vessels for the penis and the clitoris will dilate and increase blood flow.
When the blood vessels in the penis dilate, this causes a erection.
Dual Autonomic Innervation
Most organs and tissues receive both sympathetic and parasympathetic innervation.
Parasympathetic fibers primarily travel via cranial nerve X (vagus nerve).
Sympathetic innervation arises from spinal cord levels T1 to L2 — the thoracolumbar outflow — and supplies the entire body.
Autonomic Tone
Background level of activity maintained by both sympathetic and parasympathetic divisions;.
Balance between sympathetic tone and parasympathetic tone shifts in accordance to the body’s needs.
Neither of them are completely “off”.
Reciprocal Activation
The activity of one system will increase and the activity of the other will decrease.
Sympathetic dominates during “fight or flight.”
Parasympathetic dominates during “rest and digest.”
This provides more control over our body responses.
Dual Innervation
Most organs and tissues receive both sympathetic and parasympathetic innervation.
Exceptions: Adrenal medulla, most blood vessels, sweat glands (sympathetic only).
Effects can be antagonistic or cooperative.
Can be excitatory or inhibitory, depending on tissue, neurotransmitter, and receptors.
Antagonistic Effects
A effect that occurs in the digestive tract for the SNS and the PSNS; can occur in other organs between the two systems as well.
Sympathetic: decreases GI motility, increases heart rate.
Parasympathetic: increases GI motility, decreases heart rate.
Cooperative Effects
A effect that occurs in the reproductive system for the SNS and the PSNS; can occur in other organs between the two systems as well.
Parasympathetic: Erection.
Sympathetic: Emission.
Another example includes the salivary glands.
Chemical Transmitters
If an autonomic fiber release acetylcholine, it is called cholinergic.
Acetylcholine is the neurotransmitter released from both the PSNS and SNS preganglionic neurons.
If an autonomic fiber releases norepinephrine, it is called adrenergic.
Chemical Transmitters - PSNS
The preganglionic neuron starts at the CNS and sends a signal down the axon, synapsing at a ganglion.
The neurotransmitter released is ACh.
ACh is also released from the parasympathetic postganglionic target tissues.
Binds to the receptors on the target tissues, producing a response.
Smooth muscle, cardiac muscle, and glands.
Chemical Transmitters - SNS1
Preganglionic neuron originates in the spinal cord and synapses quickly.
ACh is the neurotransmitter.
The postganglionic neuron releases norepinephrine to smooth muscle, cardiac muscle, and glands.
Different neurotransmitters will be used for different organs/tissues.
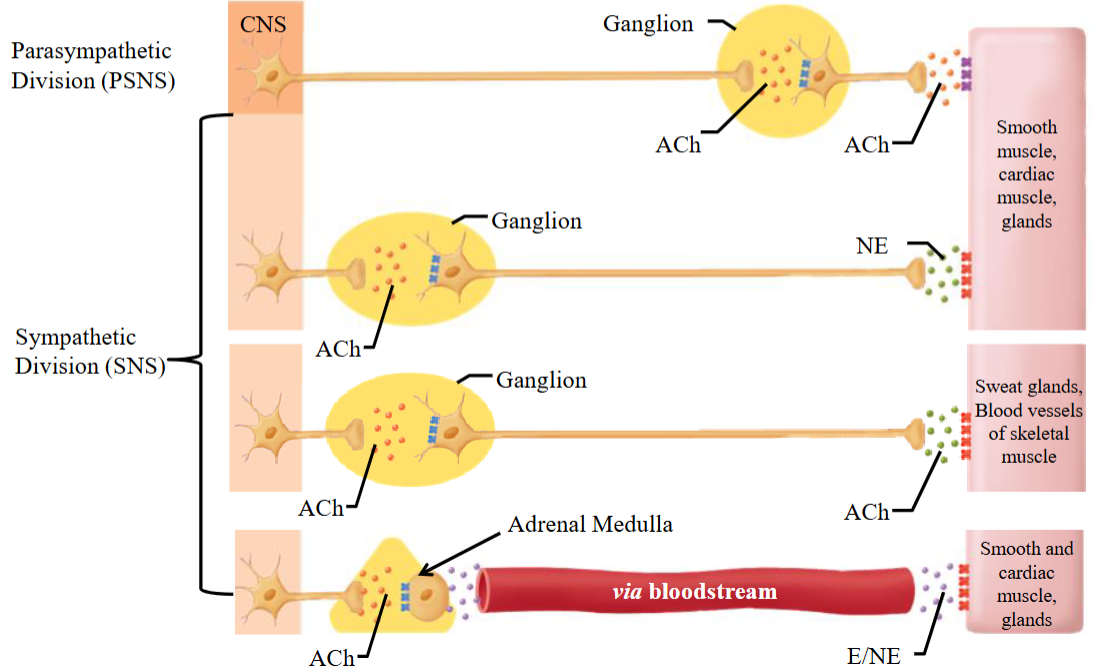
Chemical Transmitters - SNS2
Preganglionic neuron originates in the spinal cord and synapses quickly.
ACh is the neurotransmitter.
In the sweat glands and skeletal muscles, the postganglionic fiber releases ACh.
Different neurotransmitters will be used for different organs/tissues.
Chemical Transmitters - SNS3
Preganglionic neuron originates in the spinal cord and synapses quickly.
ACh is the neurotransmitter.
Receives only sympathetic stimulation.
Preganglionic fiber releases ACh onto the adrenal medulla.
Adrenal medulla acts as a modified postganglionic fiber, releasing epinephrine and norepinephrine.
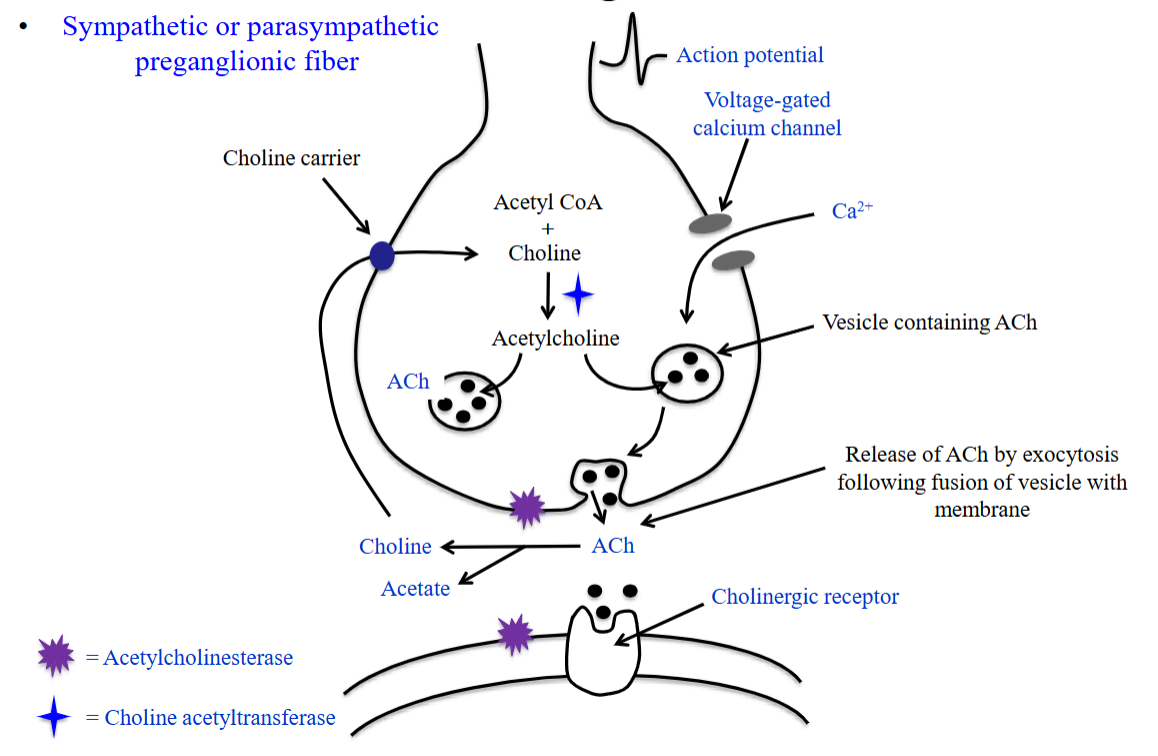
Cholinergic Nerve Terminal 1
Choline and acetyl-CoA form ACh, catalyzed by choline acetyltransferase.
ACh is packaged into vesicles in the nerve terminal.
Action potential (AP) opens voltage-gated Ca²⁺ channels at the synaptic terminal.
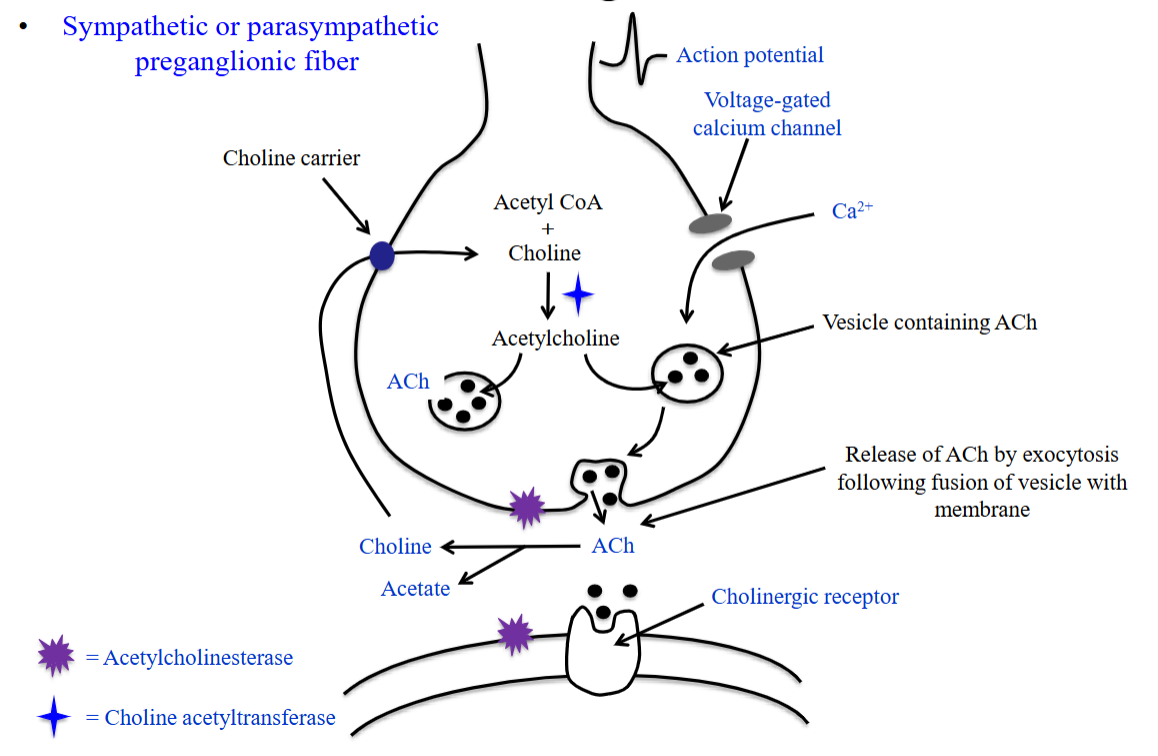
Cholinergic Nerve Terminal 2
Ca²⁺ influx (down its gradient) triggers vesicle fusion with the membrane.
ACh is released by exocytosis.
ACh binds cholinergic receptors on the postsynaptic cell.
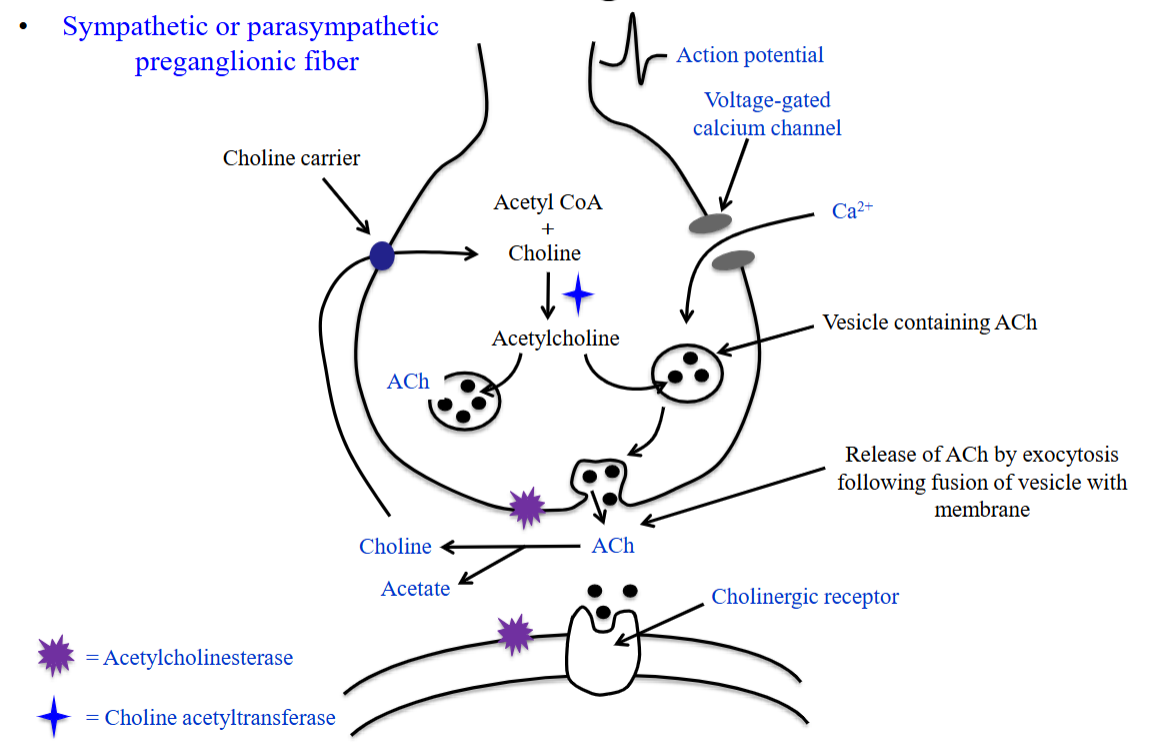
Cholinergic Nerve Terminal 3
Remaining ACh in the synapse is broken down by acetylcholinesterase into choline and acetate.
Choline is recycled into the presynaptic neuron via a carrier system; acetate is degraded to CO₂ and H₂O.
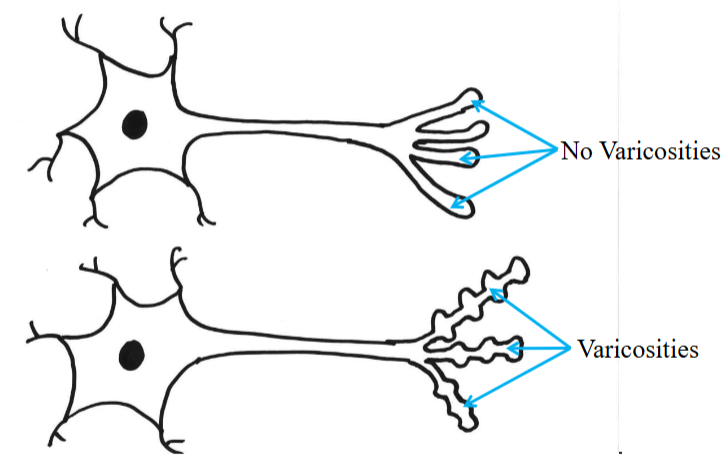
Varicosity
Postganglionic fibers in the SNS/PSNS branch in target tissue, forming multiple swellings along the axon.
These swellings contain neurotransmitter vesicles and release neurotransmitters along the axon’s length when stimulated.
This allows the signal to affect a large area of the effector tissue and influence many cells at once.
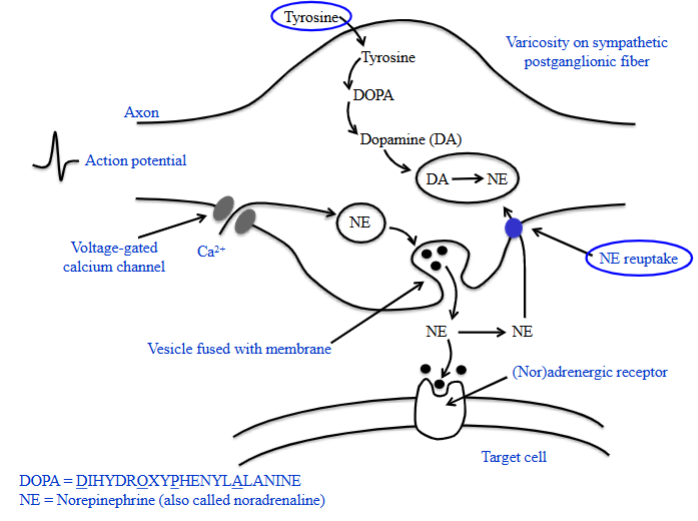
Adrenergic Nerve Terminal 1
Tyrosine is taken up into the sympathetic nerve ending (varicosity) by a specialized transport system.
Inside the varicosity, enzymes convert tyrosine to DOPA, then dopamine.
Dopamine enters vesicles and is converted to norepinephrine, which is stored until needed.
An action potential triggers Ca²⁺ channel opening, increasing intracellular Ca²⁺.
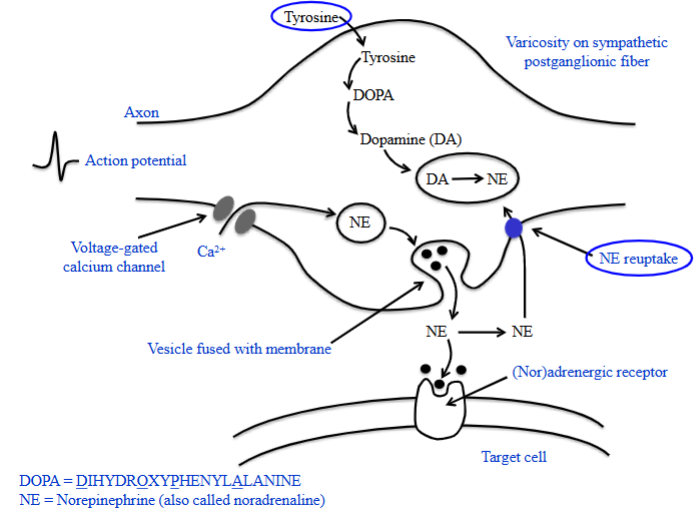
Adrenergic Nerve Terminal 2
Elevated Ca²⁺ causes vesicles to fuse with the membrane, releasing norepinephrine by exocytosis.
Norepinephrine binds to adrenergic receptors on the target cell membrane.
Excess norepinephrine is either reuptaken into the varicosity for reuse or diffuses away to be broken down by enzymes in surrounding tissues.
Acetylcholine
All autonomic ganglia (parasympathetic and sympathetic).
Parasympathetic postganglionic endings.
A few sympathetic postganglionic endings.
i.e. sweat glands, blood vessels of skeletal muscle.
Norepinephrine
Most sympathetic postganglionic endings.
Released from adrenal medulla (also epinephrine; hormones).
Cholinergic Receptors
Binds ACh.
Nicotinic and muscarinic receptors.
Nicotinic Receptors
NM → Found in skeletal muscle “nicotinic muscle.”
NN → Found on the postsynaptic cell bodies in all autonomic ganglia (sympathetic and parasympathetic) “nicotinic nerve.”
N-AChR represents nicotinic acetylcholine receptor.
Muscarinic Receptors
M1, M2, M3, M4, and M5.
Found on effector cell membranes (smooth muscle, cardiac muscle, glands).
Metabotropic.
Called muscarinic acetylcholine receptor, or M-AChR.
Adrenergic Receptors
Bind NE/E.
Two subtypes termed α and β.
α (α₁, α₂) and β (β₁, β₂, β₃) receptors.
Found on effector cell membranes (smooth muscle, cardiac muscle, and glands).
Called Adrenergic R, a receptor for norepinephrine and epinephrine.
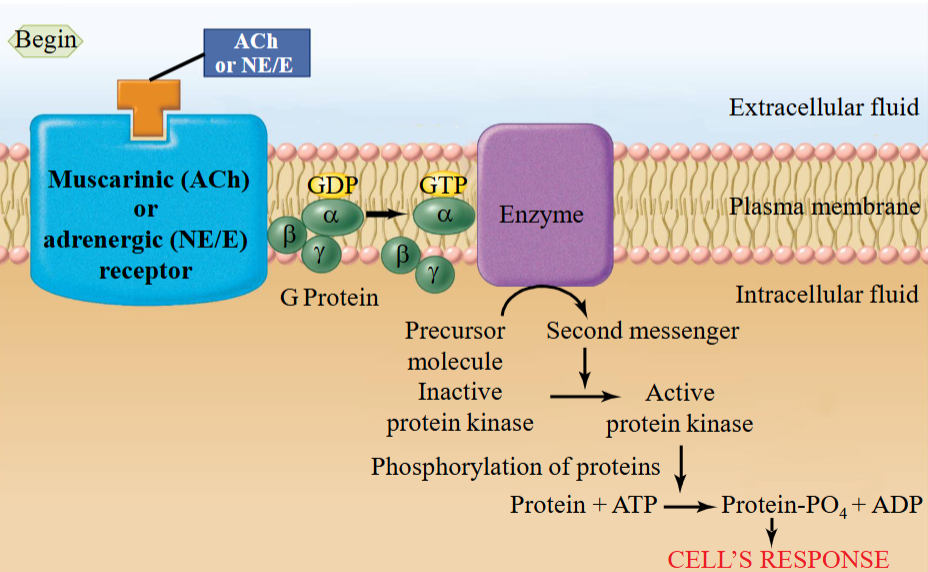
Metabotropic
This means that the receptor is couped to a signal transduction mechanism.
Binding of ACh causes excitation of inhibition of target through G-protein coupled mechanisms.
The receptors found on target tissue, whether muscarinic and adrenergic receptors, act through G-protein coupled mechanisms.
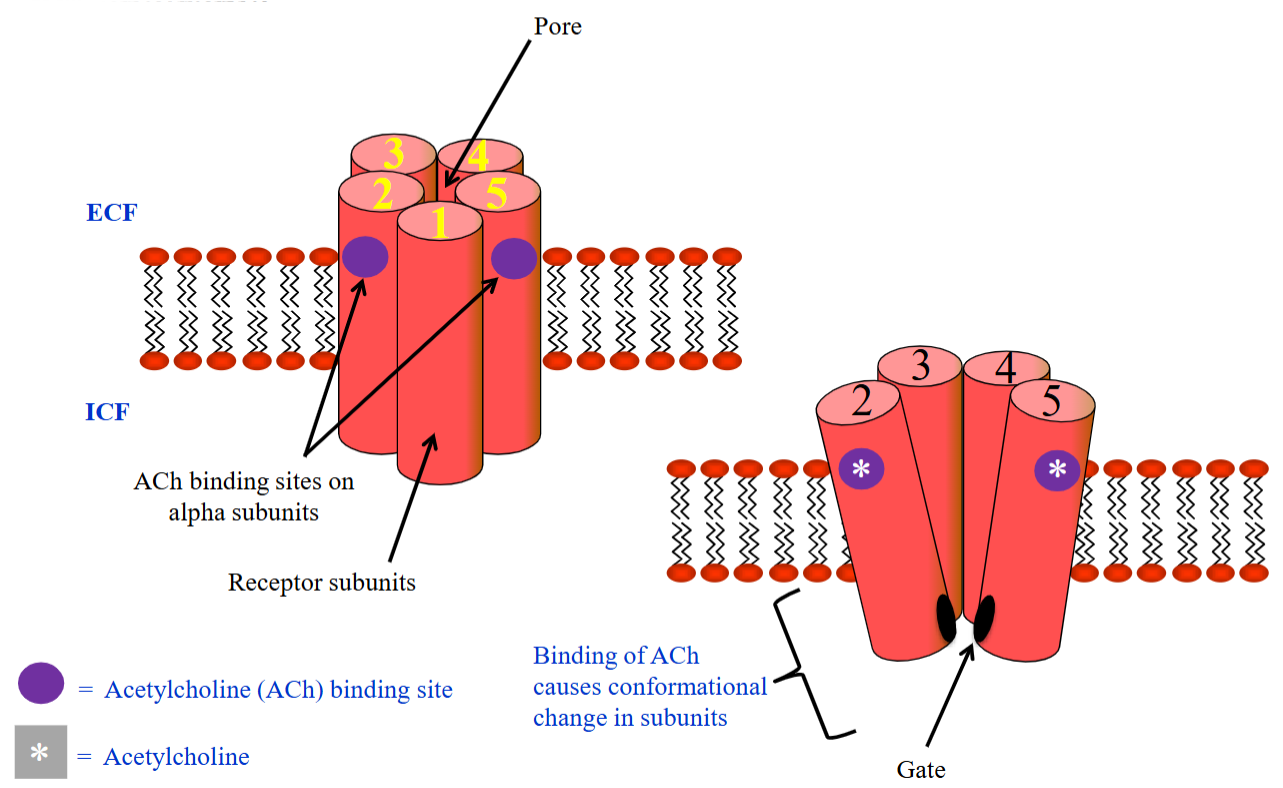
Ionotropic
Ligand-gated ion channels; a single protein acts as both receptor and channel.
ACh binding opens cation channels (Na⁺, K⁺); greater Na⁺ influx causes depolarization (EPSP).
Can produce EPSPs or IPSPs, depending on ion selectivity.
Ions move down their electrochemical gradient.
Acetylcholine is the main transmitter found at all autonomic ganglia.
The preganglionic neuron releases acetylcholine.
The cell bodies of all postganglionic neurons in the parasympathetic and sympathetic neurons is the NN type of nicotinic receptor.
Even the adrenal medulla.
Receptors - PSNS
The preganglionic neuron is long and releases ACh at the ganglion.
It binds to N-AChRs on the postganglionic neuron.
The postganglionic neuron releases ACh onto smooth muscle, cardiac muscle, and glands.
The target tissues have M-AChRs.
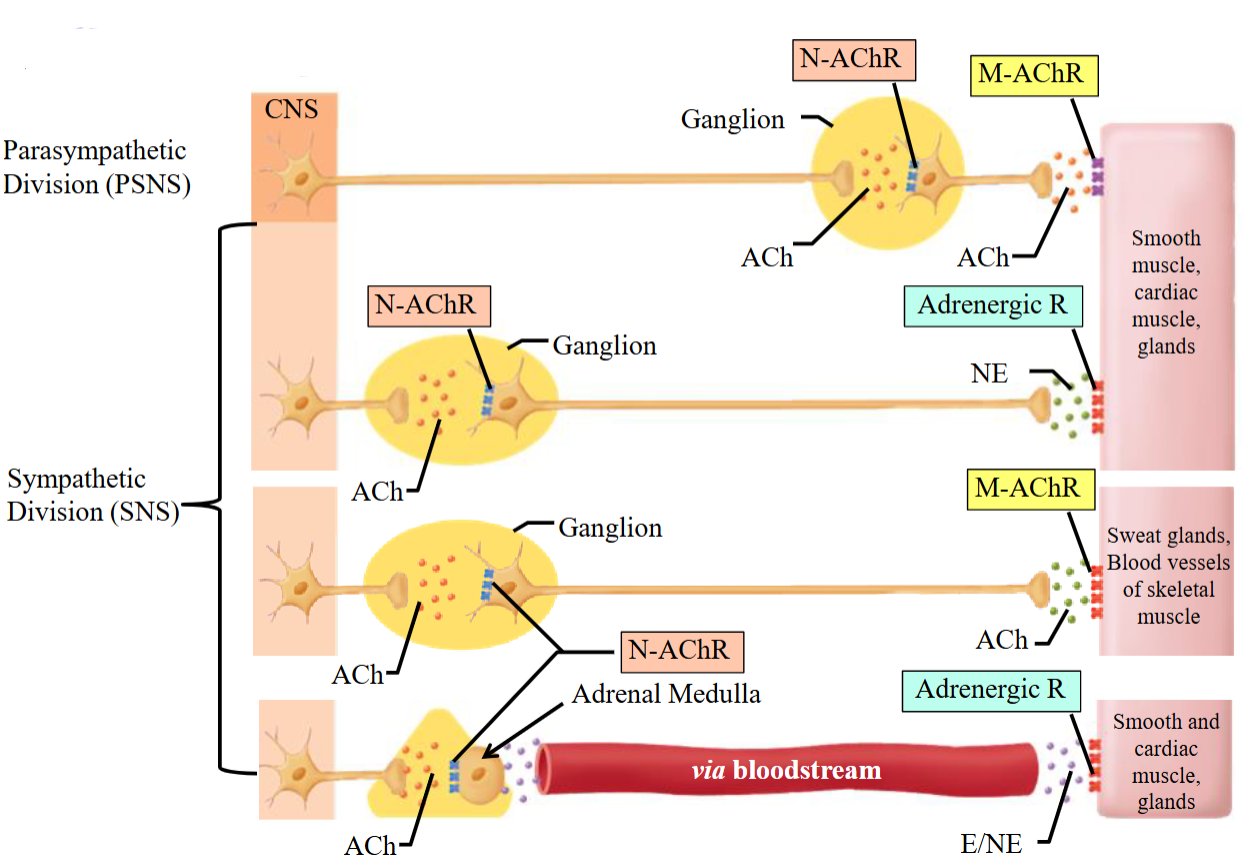
Receptors - SNS1
Preganglionic neurons in the SNS are short and release ACh in the ganglion.
The postganglionic neuron’s dendrites (in the ganglion) have N-AChRs to receive this signal.
They release norepinephrine onto smooth muscle, cardiac muscle, and glands.
Adrenergic R receive the norepinephrine and innervate the target organs.
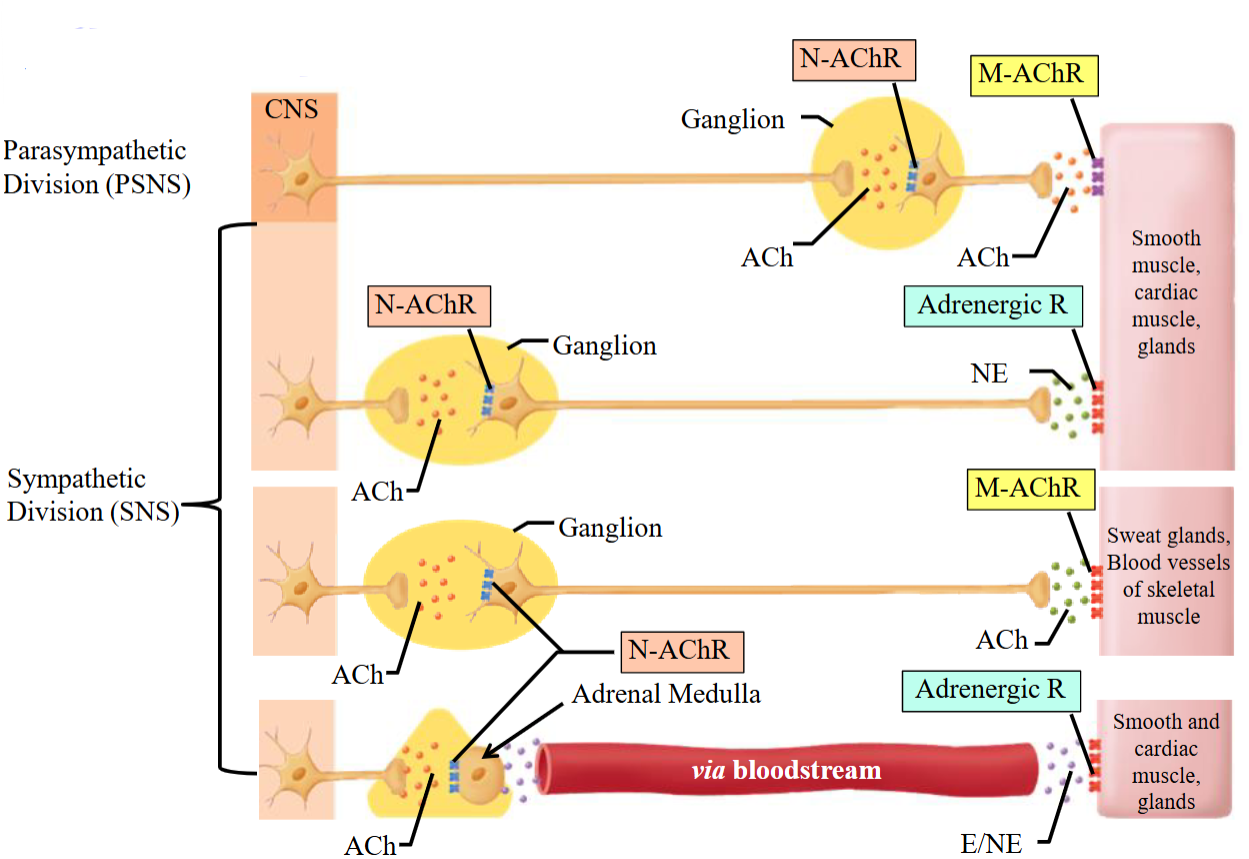
Receptors - SNS2
Preganglionic neurons in the SNS are short and release ACh in the ganglion.
The postganglionic neuron’s dendrites (in the ganglion) have N-AChRs to receive this signal.
The postganglionic neuron releases ACh to sweat glands and BVs of skeletal muscle.
The target organs have M-AChR receptors.
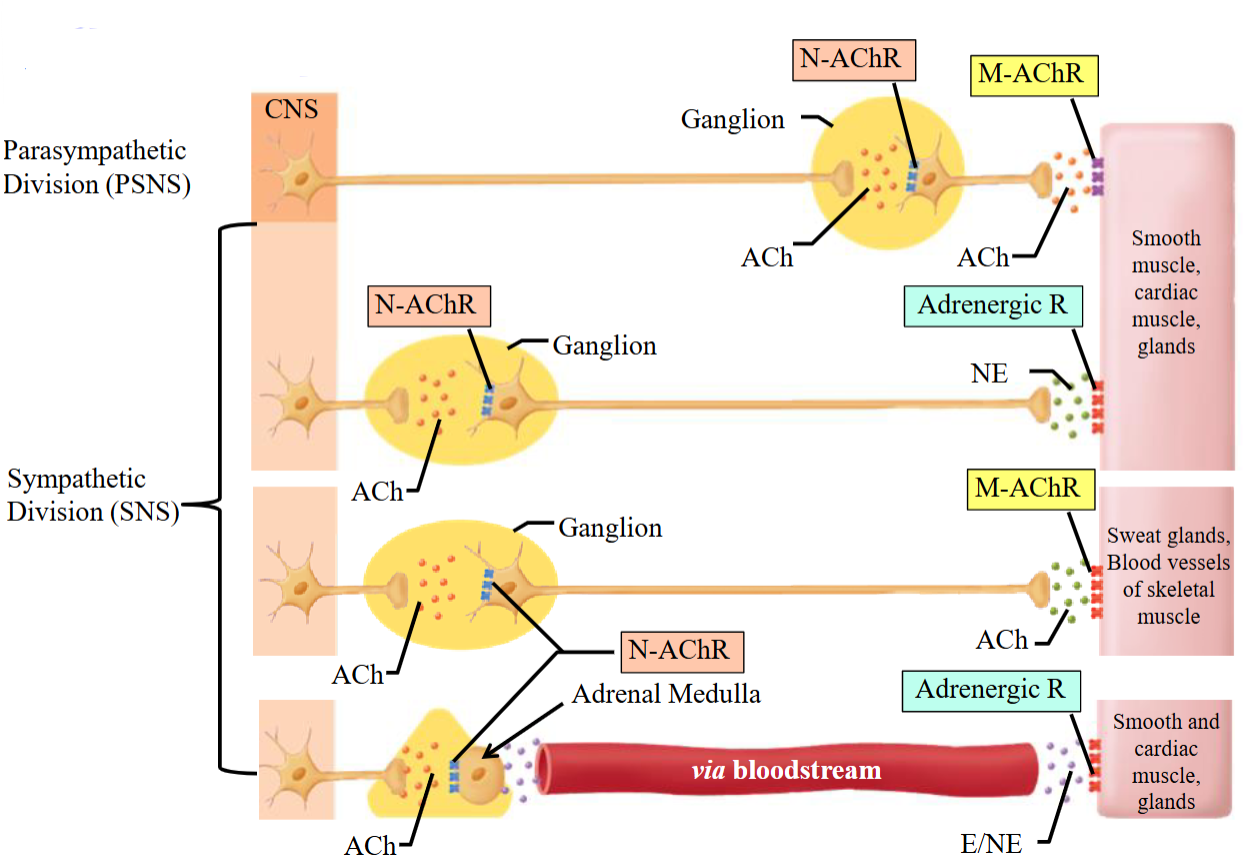
Receptors - SNS3
No postganglionic neuron; the preganglionic neuron releases ACh to the adrenal medulla via N-AChR.
The adrenal medulla releases epinephrine and norepinephrine into the bloodstream, affecting smooth muscle, cardiac muscle, and glands.
Target organs have adrenergic receptors.
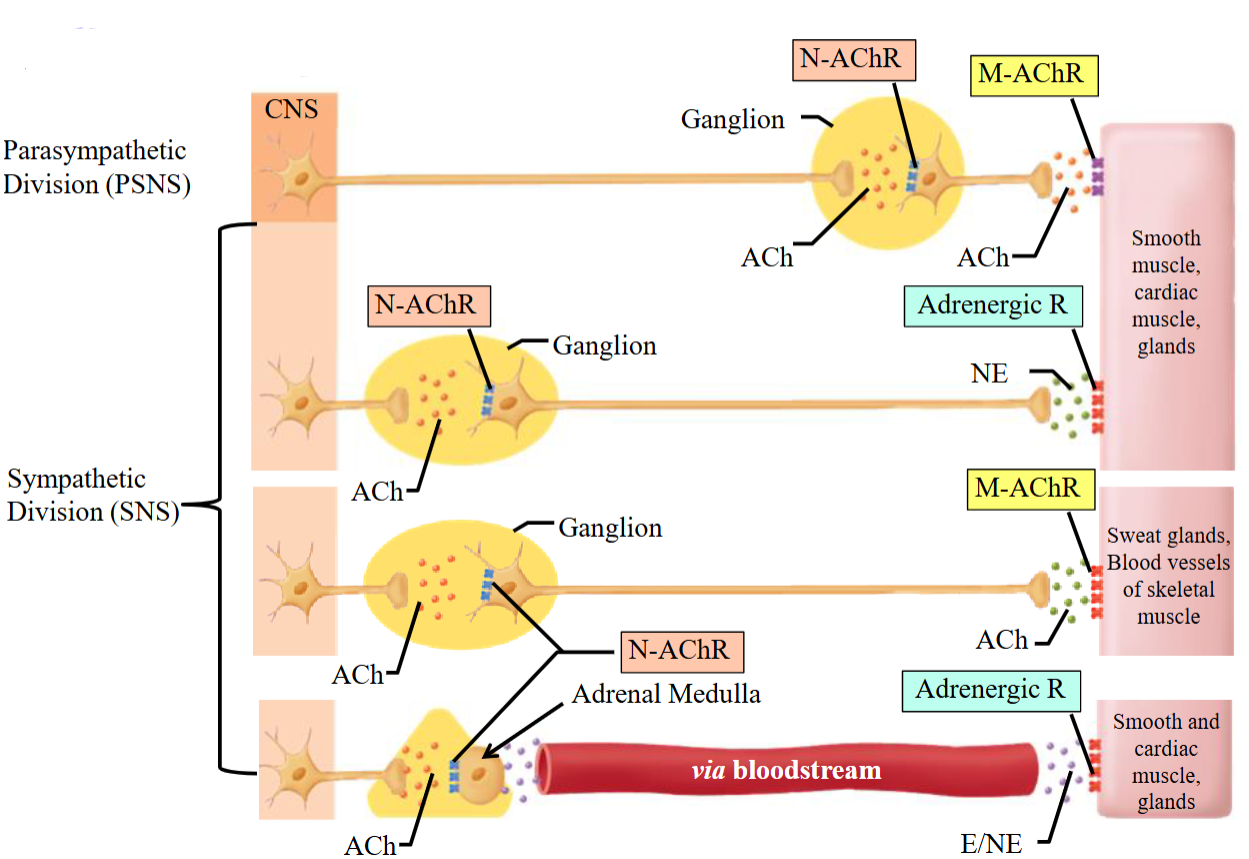
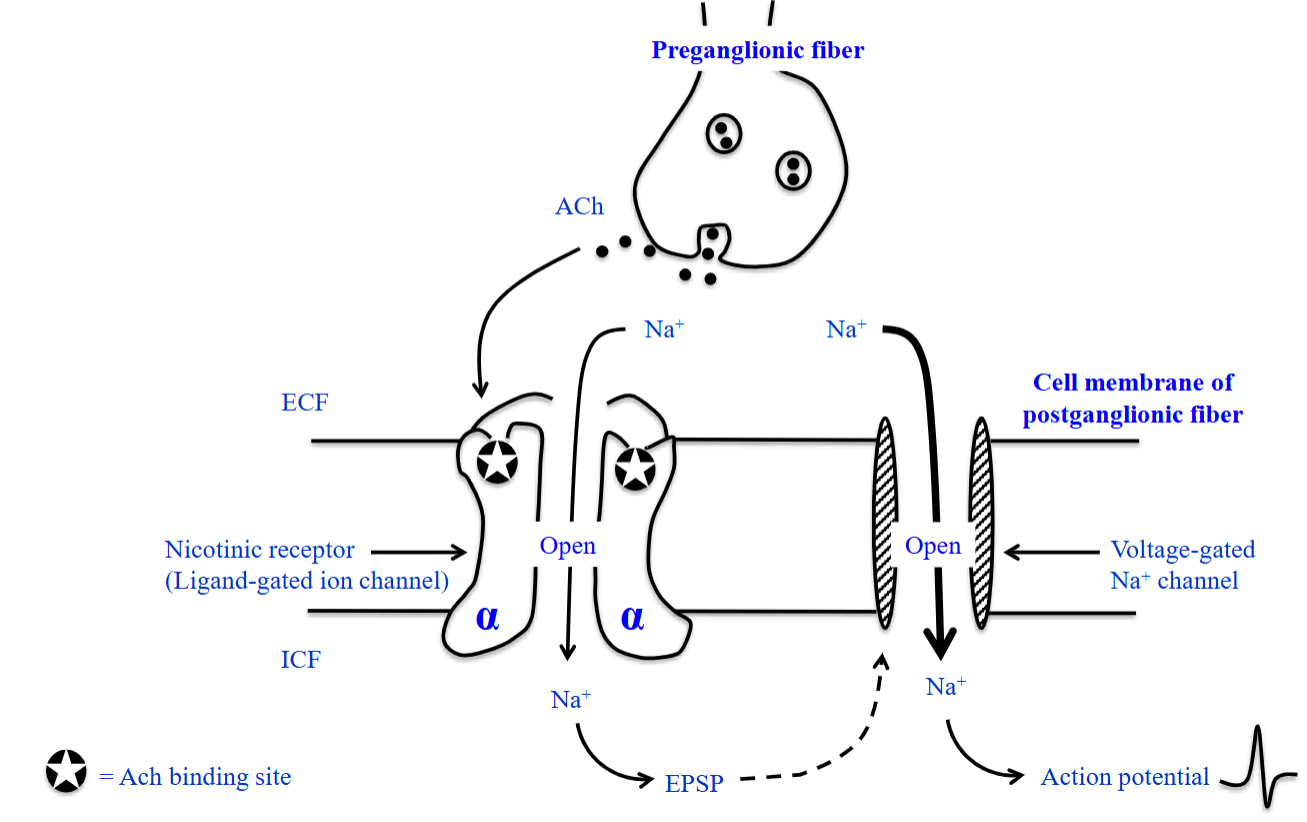
NN Type Nicotinic Receptor
Made of 5 subunits forming a ring-shaped pore in the PM.
Composed of α, β, γ, and δ subunits in various combinations.
The α-subunits contain the ACh binding sites; at least two α-subunits are required to bind ACh.
Nicotinic Receptors ACh Binding - 1
Binding of ACh to NN receptors.
These receptors are found on the cell membrane of the postsynaptic neurons in both the SNS and PSNS systems.
Both SNS and PSNS preganglionic neurons produce, store, and release ACh.
Nicotinic Receptors ACh Binding - 2
ACh is released from the preganglionic neuron and binds to a receptor on the posganglionic neuron.
Binding of ACh to each of the two α-subunits causes the ion channel in the center of this module.
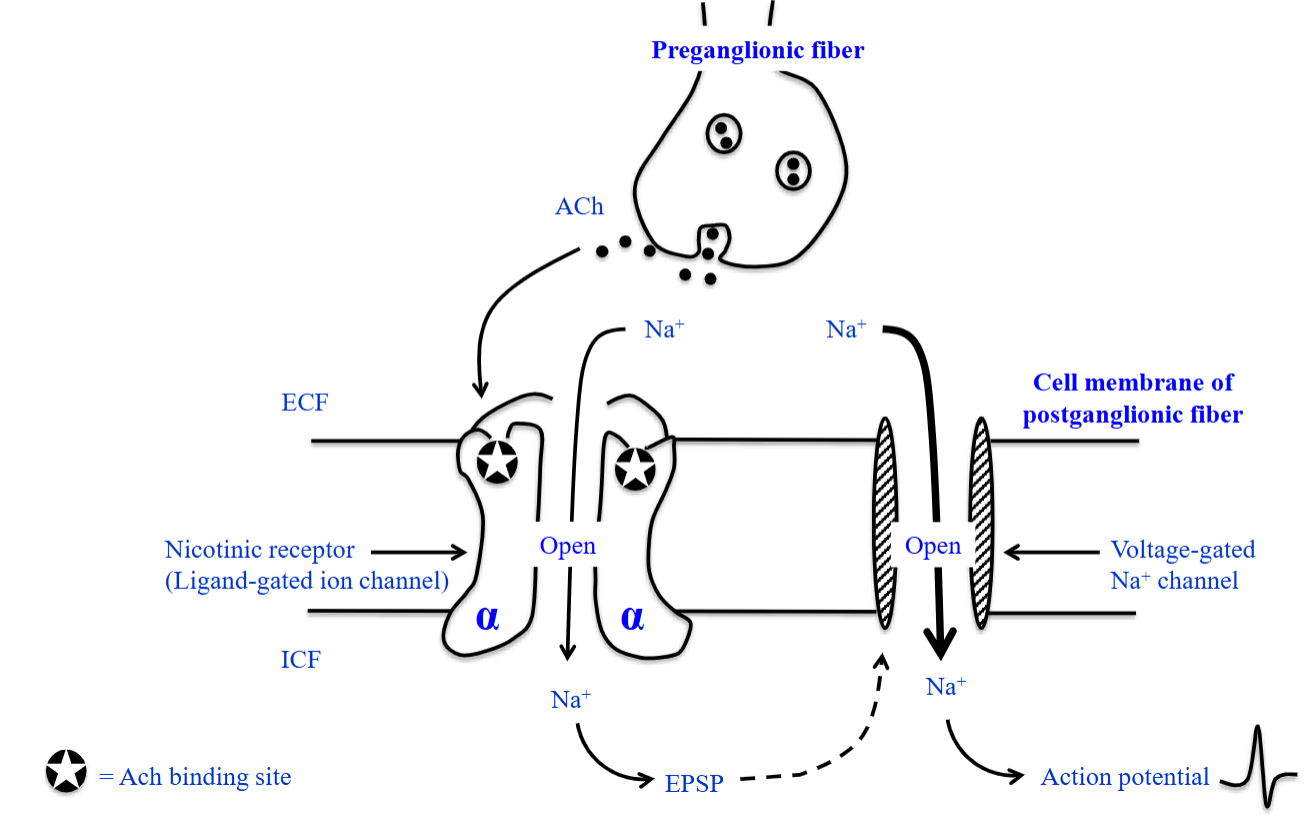
Nicotinic Receptors ACh Binding - 3
Channel opens and ions flow in.
Nicotinic receptors are cation channels, allowing the movement of specific cations.
Na⁺ enters the cell causing a EPSP.
If the EPSP is big enough, it will open the voltage-gated Na⁺ channels.
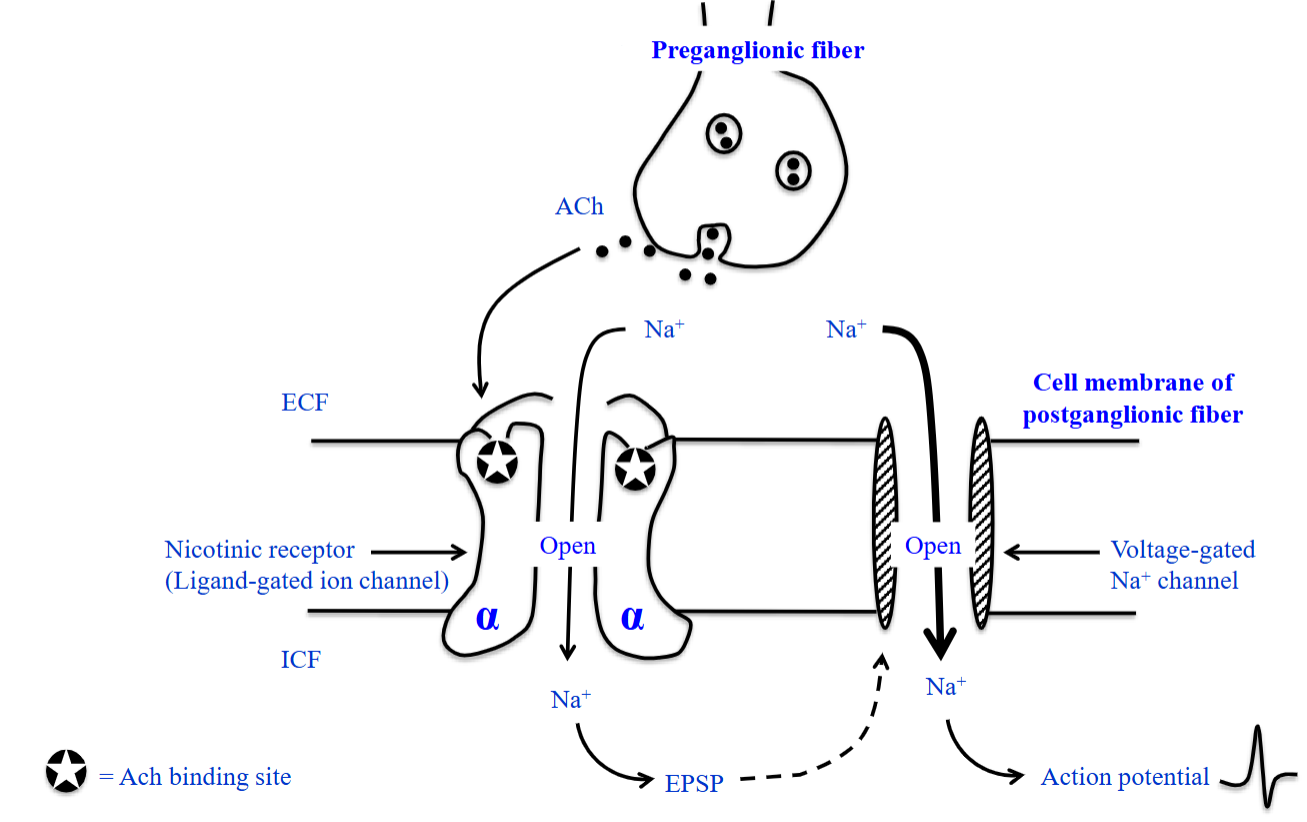
Nicotinic Receptors ACh Binding - 4
Huge influx of Na⁺ may reach threshold to reach a AP.
The activity of a transmitter molecule (ACh) released from preganglionic neurons is translated through its binding to nicotinic receptors into a AP in the postganglionic neuron.
Structure of Muscarinic & Adrenergic Receptors
Seven transmembrane spanning domains of these receptors.
Consists of a single polypeptide chain that threads back and forth the PM 7 times.
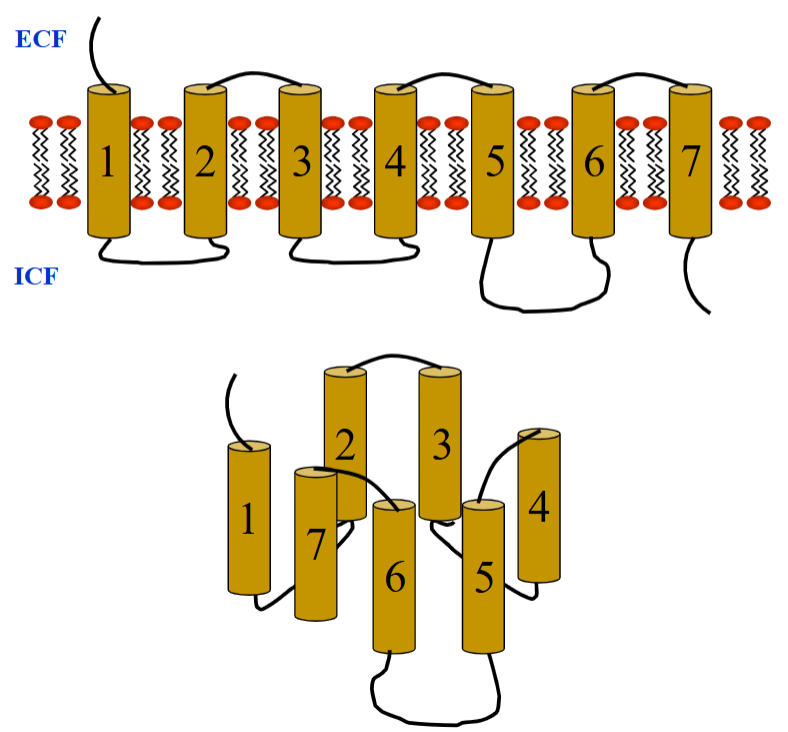
Muscarinic & Adrenergic Receptors
ACh binds muscarinic receptors; NE/E bind adrenergic receptors—both trigger G-protein-coupled responses.
Although ACh and NE/E act on different receptors, both are metabotropic (G-protein-coupled), not ionotropic.
Ligand binding activates G-protein; α-subunit dissociates and targets enzyme or ion channel.
This produces second messengers and a cellular response.
Convergence
Numerous presynaptic neurons form synapses with a single postsynaptic neuron.
Multiple presynaptic neurons affect the activity of one postsynaptic neuron.