GP- kidneys and ureters
1/122
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
123 Terms
what are the functions of the urinary system?
-maintenance of water, electrolytes, acid/base balance
-clearance of waste products
-conservation of nutrients
-erythropoietin production
-hormone degradation and excretion
-enzyme degradation
what are the 3 steps in urine formation?
1. glomerular filtration
2. tubular reabsorption
3. tubular secretion
the glomerular filtration rate (GFR) depends on:
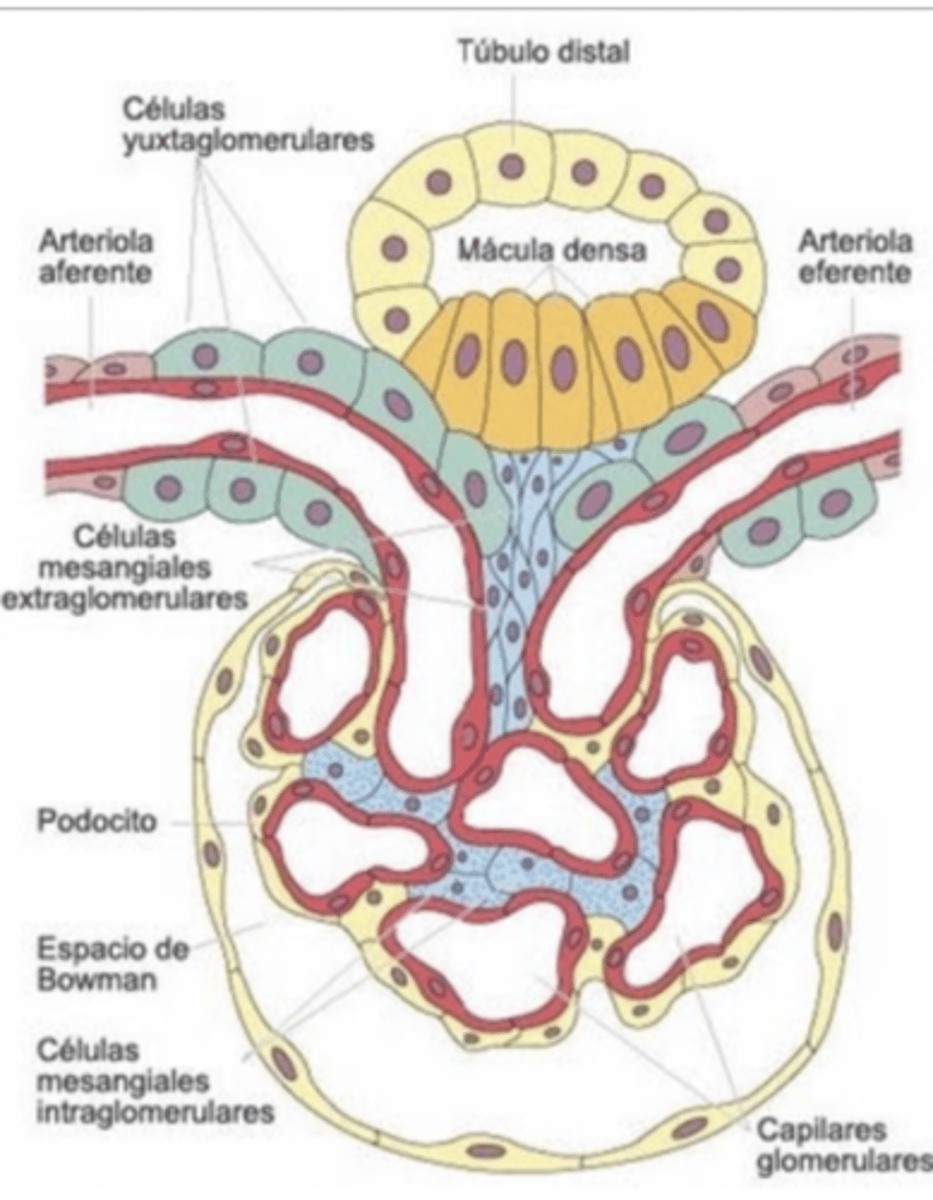
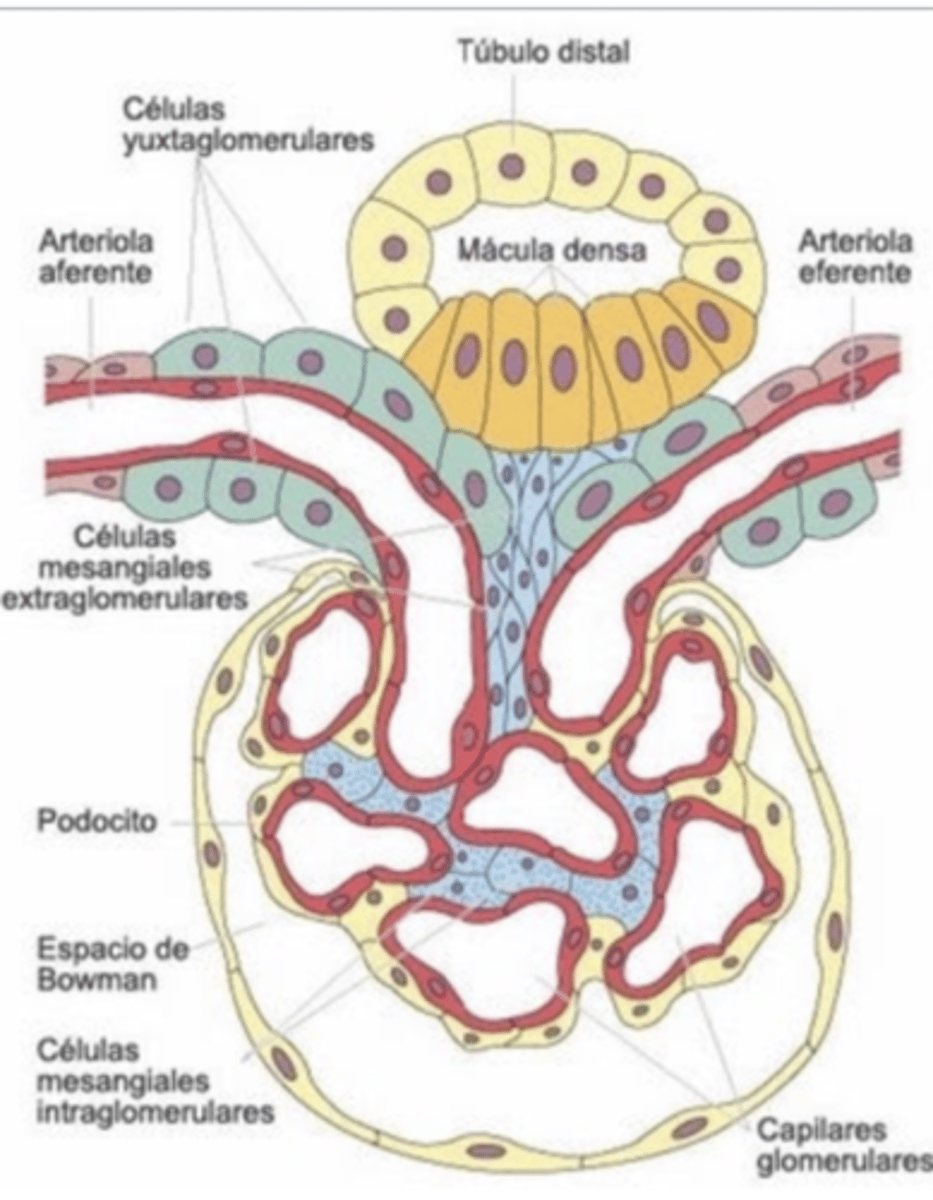
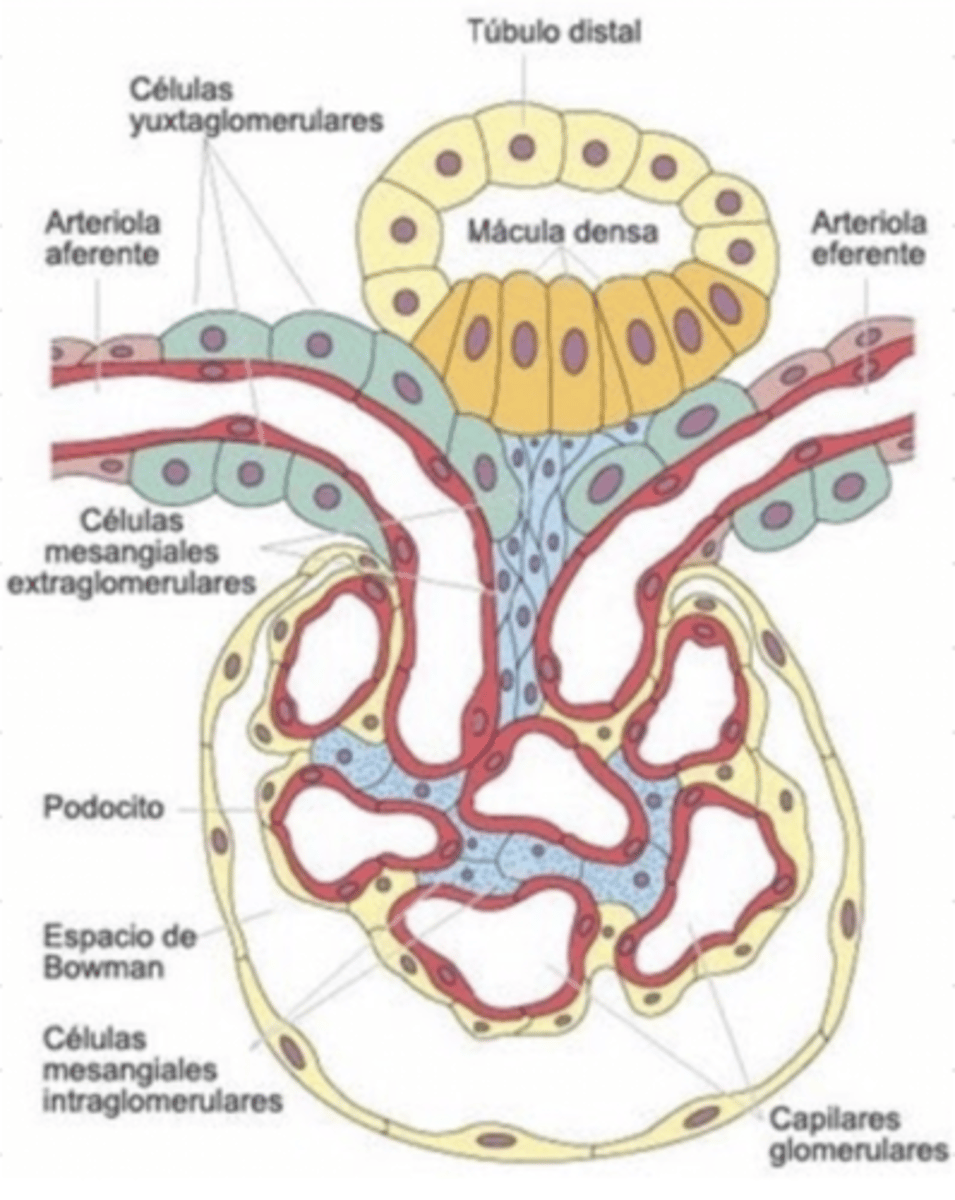
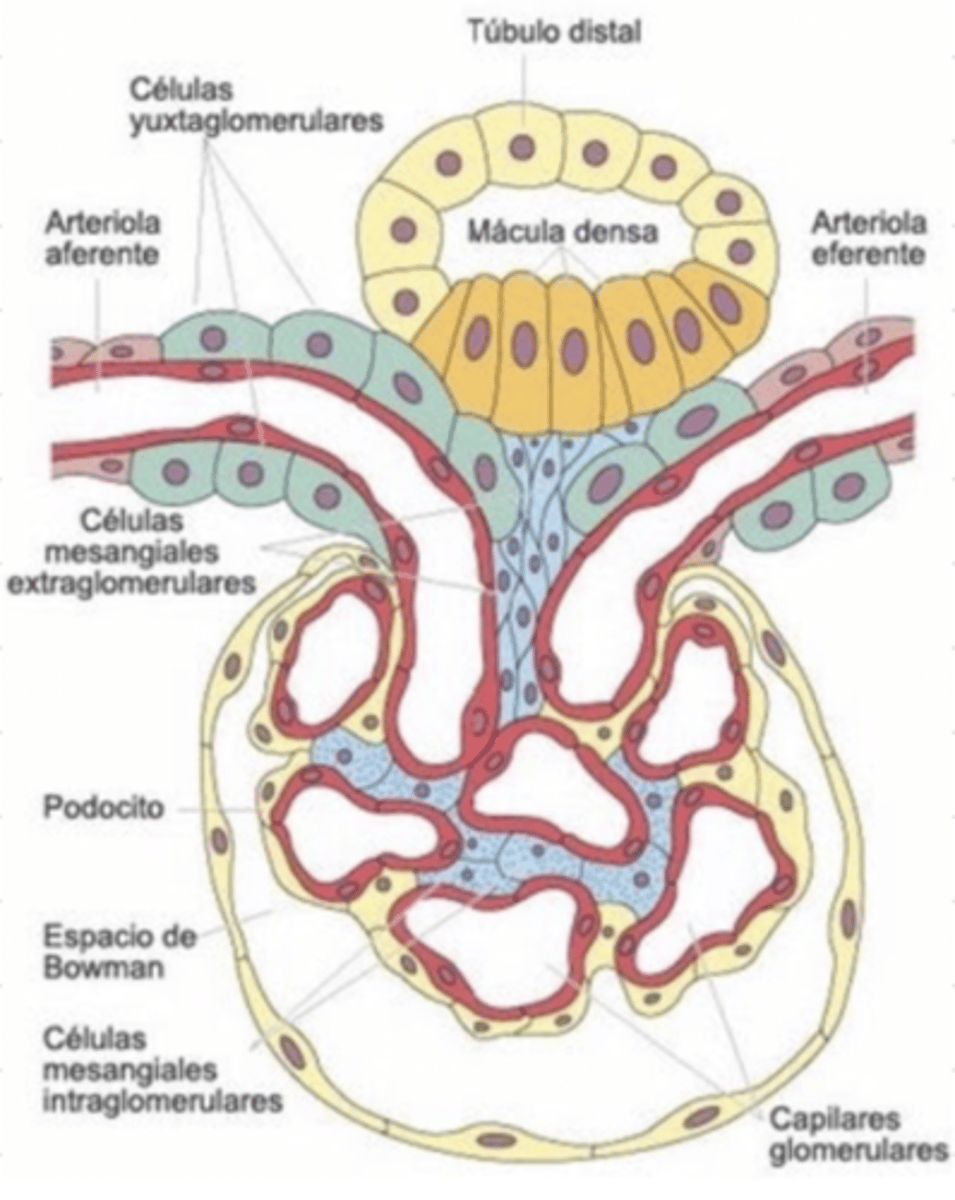
capillary hydrostatic pressure- blood enters through the afferent arteriole and exits via the efferent tubule. the hydrostatic pressure ↓ when the afferent tubule constricts. the hydrostatic pressure ↑ when the efferent tubule constricts. this is controlled by the juxtoglomerular apparatus
bowman's space fluid oncotic pressue
how does the GFR change with changes in the capillary hydrostatic pressure? how is the hydrostatic pressure changed?
↑ hydrostatic pressure = ↑ GFR
this happens when the efferent arteriole constricts
↓ hydrostatic pressure = ↓ GFR
this happens when the afferent arteriole constricts
the constrictions of the arterioles are controlled by the juxtaglomerular apparatus
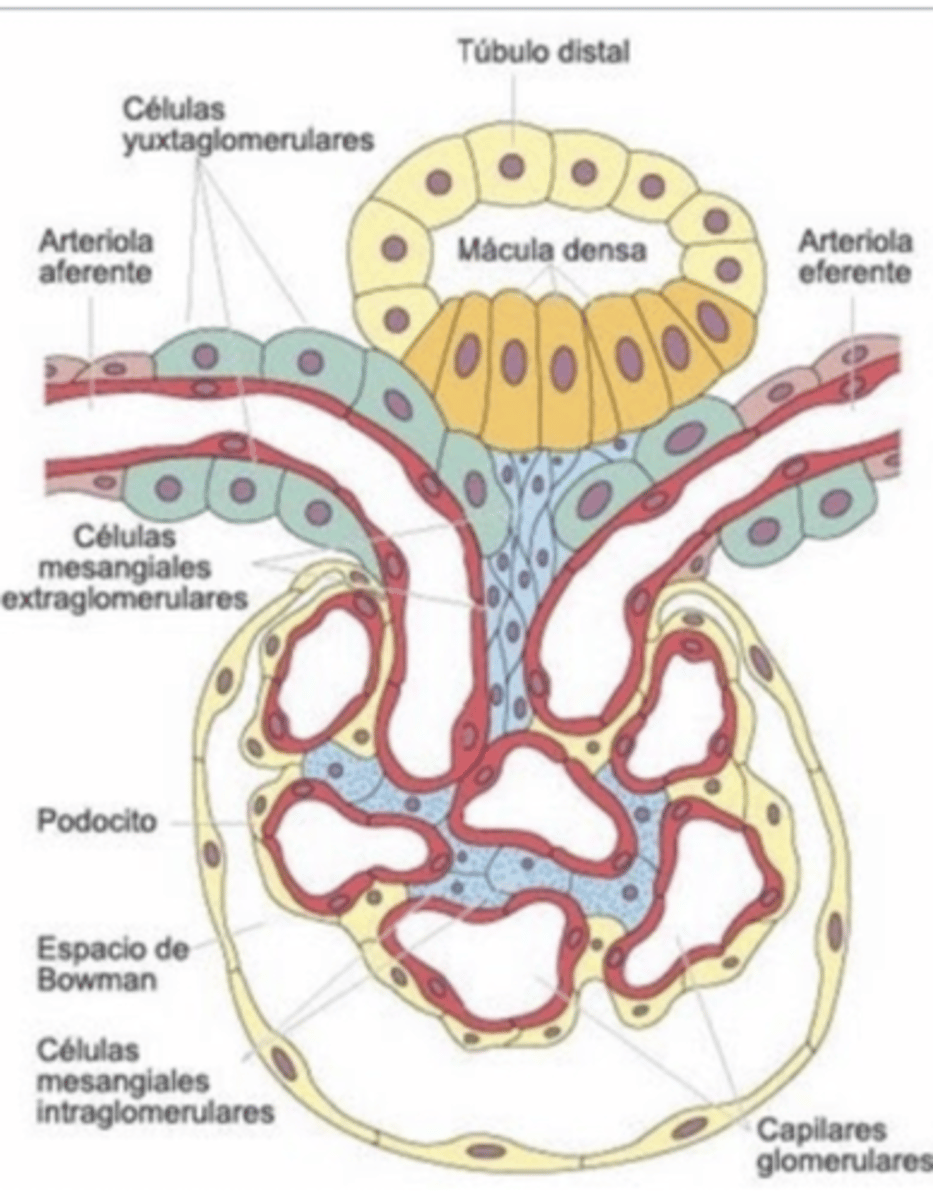
what does the juxtaglomerular apparatus do?
controls renal blood flow, and therefore glomerular filtration
it controls the constriction of the afferent/efferent arterioles, which causes a change in hydrostatic pressure, and therefore in the GFR
how does the constriction of the efferent arteriole affect the GFR?
↑ GFR
because it ↑ the hydrostatic pressure
how does the constriction of the afferent arteriole affects the GFR?
↓ GFR
because it ↓ the hydrostatic pressure
what substances are reabsorbed in the proximal tubule?
glucose (100%)
amino acids (100%)
proteins
H2O
Na+ (65%)
HCO3 (80-90%)
Ca2+ (60%)
P (85%)
K+ (60-70%)
where in the nephron is glucose reabsorbed?
proximal tubule
where in the nephron are amino acids reabsorbed?
proximal tubule
is glucose reabsorbed or secreted?
reabsorbed (100% in the proximal tubule)
are amino acids reabsorbed or secreted?
reabsorbed (100% in the proximal tubule)
what substances are reabsorbed in the loop of henle?
NaCl (25%)
H2O (15%)
Mg (15%)
where is H2O reabsorbed in the nephron?
proximal tubule, loop of henle, distal tubule, collecting duct
(throughout the entire nephron)
where is NaCl reabsorbed in the nephron?
loop of henle
is NaCl reabsorbed or secreted?
25% reabsorbed in the loop of henle
what substances are reabsorbed in the distal and collecting tubules?
Na+ (5%)
H2O
is Mg reabsorbed or secreted?
15% reabsorbed in the loop of henle
what hormone regulates the secretion of H2O in the distal tubule and collecting duct?
ADH
what waste products are secreted by the nephron, composing the urine?
ammonia
uric acid
H+
K+
creatinine
(all of these will intoxicate the animal if not secreted)
if the animal has renal failure and cannot secrete the waste products, what happens?
the animal will be intoxicated by the waste products, and will most likely die from ammonia intoxication
what is diuresis?
urine production
what is the normal diuresis quantity of dogs, cats, and horses?
dogs: 20-40ml/kg/day
(or 1-2ml/kg/hr)
cats: 28 ml/kg/day
horses: 15-30 ml/kg/day
these values are measured by putting an intraurethral catheter and collecting the urine
what is polyuria?
what can cause this?
↑ production of urine
causes:
↑ water intake
stress
diuretics
↑ urine osmolarity (DM, CRF, HAC)
diabetes insipida
sepsis
what physiological changes cause polyuria?
↑ water intake
stress
what can cause polyuria?
physiological:
↑ water intake
stress
pharmacological:
diuretics
mannitol
pathological:
↑ urine osmolarity (DM, CRF, HAC)
diabetes insipida
sepsis
diabetes insipida has what main urinary related clinical sign?
polyuria, due to ADH deficit
diabetes mellitus has what main urinary related clinical sign?
polyuria, due to increased urine osmolarity
polydipsia due to polyuria
chronic renal failure will lead to _____uria (oly/poly)
polyuria
cushing's disease will lead to _____uria (olig/poly)
polyuria
what is oliguria? what can cause this?
↓ urine production (<0.25 ml/kg/hr)
causes:
↓ water intake
↓ GFR (due to glomerular disease, heart failure, shock, etc)
partial urinary tract obstruction
an animal producing 0.08-0.25 ml/kg/hr of urine has ______uria
oliguria
an animal producing <0.08ml/kg/hr of urine has ______uria
anuria
what pathologies lead to a ↓ GFR, which causes oliguria?
heart failure
glomerular disease
shock
what pathological reasons might an animal have oliguria?
↓ GFR, due to heart failure, glomerular disease, shock, etc
partial urinary tract obstruction
what is anuria? what cause cause this?
no urination (<0.08 ml/kg/hr)
causes:
dehydration
severe hemorrhage
acute tubular necrosis
acute renal failure
calculi
tumors
what are the different etiologies of anuria?
pre-renal:
dehydration
severe hemorrhage
renal:
acute tubular necrosis
acute renal failure
post-renal:
calculi
tumors
what is polaquiuria?
↑ frequency of urination with ↓ urine quantity
usually due to pain
↑ frequency of urination with ↓ urine quantity is called...
polaquiuria
if an animal is urinating <0.08ml/kg/hr, we call this ______uria
anuria
dehydration can cause _____uria
oliguria or anuria
pain commonly causes ____uria
polaquiuria
calculi or tumors in the urinary tract can cause...
polaquiuria (if painful), anuria (if completely obstructing), or oliguria (if partially obstructing)
acute tubular necrosis will cause ______uria
anuria
what is dysuria?
difficulty urinating
incomplete/painful urination due to a lower urinary tract pathology
the incomplete/painful urination due to a lower urinary tract pathology is called ______
dysuria
dysuria results from a problem where?
lower urinary tract
what is vesical tenesmus?
feeling of incomplete emptying of the urinary bladder after urination
the feeling of incomplete emptying of the urinary bladder after urination is called.....
vesical tenesmus
what is urinary incontinence?
lack of control over urination
an animal that cannot control its urination has ______
urinary incontinence
what can cause urinary incontinence?
hormonal:
↓ testosterone/ estrogen (due to early castration)
mechanical:
bladder tumors
calculi
prostate disease
neurological:
CNS lesions
peripheral nerve lesions
if we castrate a puppy/kitten too early, this inhibits the secretion of testosterone and estrogen, which will commonly lead to what urinary problem?
urinary incontinence
what neurological problems may cause urinary incontinence?
CNS lesions
peripheral nerve lesions
what mechanical problems can cause urinary incontinence?
bladder tumors
calculi
prostatic disease
how can we perform a clinical evaluation of the urinary system?
1. hematology and biochemistry profile
2. urinalysis and urine sediment exam
3. xrays
4. ultrasound of kidney, bladder, and urethra
5. biopsy
if performing a biochemistry test to assess the urinary system, what values do we check?
BUN (urea)
serum creatinine
these can tell us the functionality of the GFR
if performing a urinalysis to assess the urinary system, what values do we check?
to check tubular function:
concentration/dilution
electrolytes
glucose
protein
casts
to check glomerular function:
urine protein (albumin, creatinine)
RBCs
if we want to assess the # of functional nephrons, what do we want to assess?
the GFR.
we do this by performing a biochemistry exam and looking at BUN and serum creatinine
if substances that should be excreted in the urine are present or ↑ in the blood, this indicates_______
inadequate GFR (which can indicate ↓ functional nephrons)
what is BUN?
urea
final product of protein catabolism
excreted by the kidneys and GI
if ↑ in the blood, most likely due to a kidney disorder (also possibly ↑ protein diet or GI hemorrhage)
↑ BUN means:
kidney disorder
↑ protein diet
GI hemorrhage
what is serum creatinine?
a product of muscle metabolism (muscular animals have more creatinine)
removed almost 100% by glomerular filtration
which, BUN or serum creatinine can be due to a kidney problem, hydration status, or diet?
BUN
serum creatinine is only affected by the kidneys
which, BUN or creatinine, is a better parameter for GFR measurement, because it is only affected by glomerular filtration?
serum creatinine
(BUN can also be affected by a GI hemorrhage or ↑ protein diet)
what is azotemia?
↑ BUN and ↑ creatinine
there are 3 types:
1. pre-renal
2. renal
3. post-renal
↑ BUN and ↑ creatinine is called...
azotemia
what is prerenal azotemia?
hemodynamic azotemia, due to dehydration and hypovolemia.
-↓ renal blood flow
-↓ perfusion pressure
-↑ vascular resistance
easy to treat, but can lead to ARF
hallmarks:
-mild azotemia
-↑ urine specific gravity
-↓ urine Na+
increased BUN and creatinine in the blood due to dehydration/hypovolemia is called.....
pre-renal azotemia
if an animal with ↑ BUN and creatinine also has a high specific gravity and ↓ Na+ in the urine, what do we call this?
pre-renal azotemia
(due to dehydration/ hypovolemia)
what is renal azotemia?
↑ BUN and creatinine due to acute renal failure, which leads to irreversible parenchymal damage.
it is caused by ischemic, toxic, or inflammatory insult
↑ BUN and creatinine caused by Acute renal failure is called....
renal azotemia
what can cause renal azotemia?
acute renal failure, due to ischemic, toxic, or inflammatory insult
what is post-renal azotemia?
↑ BUN and creatinine due to obstruction of the urine flow and retention of these products within the body
these are caused by obstructions of the lower urinary tract, such a uroliths, mucous plugs, blood clots, and masses (intra or extra luminal)
↑ urea and BUN caused by lower urinary tract obstruction is called...
post renal azotemia
what may cause a lower urinary tract obstruction? this can lead to what abnormal values in a biochemistry test?
uroliths
mucous plugs (cats)
blood clots
intra/extra luminal masses
azotemia (↑ BUN and creatinine)
the sudden loss of renal function is called....
acute renal failure
is acute renal failure reversible?
potentially, if it is diagnosed and treated quickly
there are ____ clinical stages of acute renal failure.
3:
induction
maintenance
recovery
is acute renal failure a serious condition?
yes
______% of acute renal failure is pre-renal
60-70
25% of acute renal failure is due to a problem with the _______
kidneys (tubules, interstitium, or glomeruli)
___% of acute renal failure is caused by obstruction of outflow of urine (post renal)
5%
what is the most common cause of acute renal failure?
↓ renal perfusion (without renal cell injury)- pre-renal acute renal failure. this can be caused by diarrhea/vomiting, cardiac failure, hemorrhage, dehydration, hypoalbuminemia, thrombosis in renal arteries, or septic shock
this makes up 60-70% of acute renal failure cases
pre-renal acute renal failure will appear with what abnormal values on the blood and urine test?
↑ ↑ BUN : creatinine ratio
↓ urine Na+
↑ urine osmolarity
a very high BUN and low creatinine (↑ BUN:creatinine) indicates what type of renal failure?
pre-renal acute renal failure
what type of renal failure can diarrhea/vomiting, dehydration, cardiac failure, hemorrhage, thrombosis, septic shock, and hypoalbuinemia cause?
pre-renal acute renal failure
because they will cause a decrease in renal perfusion
we see these results in the blood and urine tests:
↑ BUN : creatinine
↓ urine Na+
↑ urine osmolarity
what can we suspect is the diagnosis?
pre-renal acute renal failure
(due to ↓ renal perfusion)
what problems in the kidneys can cause acute renal failure?
acute renal nephritis- caused by allergy, autoimmune, embolism, ascending infection
glomerulonephritis- caused by inflammation, immune-mediated, neoplasia, or diabetes
amyloidosis- this is progressive and irreversible
amyloidosis can cause what type of renal failure?
acute renal failure, because it accumulated between the renal cells and compresses them
this is progressive and irreversible
what are possible causes of acute renal nephritis?
allergy
autoimmune
embolism
ascending infection
what might cause glomerulonephritis?
inflammation
immune mediated
neoplasia
diabetes
what can cause post-renal acute renal failure?
obstructions
uroliths, neoplasia, tumors, adhesions, bladder displacement
trauma
how does acute renal failure appear in a blood and urine test if it is due to a problem within the kidney?
↑ BUN and creatinine
presence of renal tubular epithelial cells, RBCs, WBCs, or casts in the urine sediment
proteinuria
if we perform a blood and urine test on an animal and see:
↑ BUN and creatinine
presence of renal tubular epithelial cells, RBCs, WBCs, or casts in the urine sediment
proteinuria
what is most likely the cause?
intrinsic acute renal failure (caused by acute renal nephritis, glomerulonephritis, or amyloidosis)
what abnormalities are present in the blood and urine tests of an animal with post renal acute renal failure?
↑ BUN and creatinine
obstruction shown in imaging
hematuria
what are the 3 stages of acute renal failure?
1. induction
renal insult, cellular damage
2. maintenance
loss of nephron function, oliguria (bc cannot reabsorb H2O)
3. recovery (not always)
return to normal tubular function, resolution of azotemia, polyuria → normal diuresis, nephron repair
if in the recovery stage of acute renal failure the nephrons become fibrotic, what happens?
development of chronic renal failure
what are the clinical signs of acute renal failure?
uremic syndrome (due to acidosis- ↑ H+)
-vomiting and diarrhea
-lethargy
-anorexia
-depression
-coma
-oral cavity ulceration
-halitosis
-oliguria → polyuria
what is uremic syndrome?
a set of clinical signs associated to severe kidney failure or post renal obstruction due to accumulation of uremic toxins in the blood
-vomiting/diarrhea
-lethargy
-anorexia
-depression
-coma
-oral cavity ulceration
-halitosis