Ch. 21 - Immune (Part 1)
1/67
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
68 Terms
Whats the ratio of bacterial cells to human cells in the body?
The body has at least 10x as many bacterial cells as human cells
Most are beneficial
Some potentially disease-causing
by volume, we are mostly human cells, but by number, we are mostly bacterial cells
Immune System
a cell population that inhabits all organs and defends the body from agents of disease
is a functional system, not an organ system
this system is especially concentrated in the lymphatic system
Lymphatic System
Network of organs and vein-like vessels that recover extracellular fluid
governs the movement of ECF in the body
Inspects it for disease agents
Activates immune responses
Returns fluid to the bloodstream
3 Functions/Properties of the Lymphatic System
Fluid Recovery
Immunity
Lipid Absorption
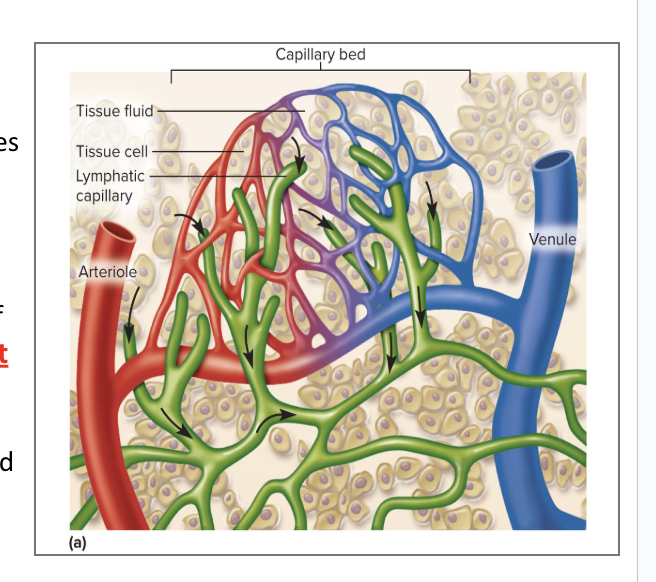
Fluid Recovery
Fluid continually filters from the blood capillaries into the tissue spaces
Blood capillaries reabsorb 85% of it
15% of the water and about half of the plasma proteins enter the lymphatic system and then are returned to the blood
gets rid of excess fluid from extracellular tissue matrix
is an alternative circulatory system
moves lymphatic and extracellular fluid around body
there are lymphatic capillaries intertwined in the blood capillaries
leftover liquid released form arterial capillaries gets absorbed by the lymphatic capillaries to process it and put it back in the bloodstream
Immunity
The ability to resist a disease
Excess filtered fluid picks up foreign cells and chemicals from the tissues
Passes through lymph nodes where immune cells stand guard against foreign matter
Activates a protective immune response
We get immunity when we pick up those bacterial cells and filter them out using the lymphatic system, and then train our leukocytes to adapt/respond to that bacteria
Lipid Absorption
In the small intestine, we use dead end lymphatic capillaries called lacteals to absorb lipids that are not absorbed by the blood capillaries
Lymph
all the liquid we pull out of the EC matrix
aka all the liquid absorbed by the lymphatic system
Clear, colorless fluid, similar to plasma, but much less protein
chemically identical to plasma
Originates as extracellular fluid drawn into lymphatic capillaries
Its chemical composition varies in different places in the body (in intestines, after lymph nodes)
Lymphatic Vessels
Transport the lymph (the recovered fluid)
Lymphatic Tissues
Composed of aggregates (clusters) of lymphocytes and macrophages that populate many organs in the body
they hang out by the dirty fluid filters
Lymph nodes are the most abundant lymphatic tissue
often in connective tissues of mucous membranes
Lymphatic Organs
Defense cells are especially concentrated in these organs
thymus and red bone marrow are examples of lymphatic organs
anatomically well defined
Have a connective tissue capsule
Lymphatic Capillaries
These capillaries penetrate nearly every tissue of the body
Absent from cartilage, cornea, bone, and bone marrow
Capillary wall is made of endothelial cells overlapping each other like roof shingles
are closed at one end
Cells are tethered to surrounding tissue by protein filaments
Gaps between cells are large enough to allow bacteria and cells to enter lymphatic capillary
Overlapping simple squamous epithelium creates valve-like flaps that open when interstitial fluid pressure is high, and close when it is low
Lymphatic Vessels
Larger ones are composed of 3 layers:
Tunica interna: endothelium and valves
Tunica media: elastic fibers, smooth muscle
Tunica externa: thin outer layer
Converge into larger and larger vessels
Collecting vessels course through many lymph nodes
are large vessels
6 lymphatic trunks drain major portions of the body
Trunks converge together to form the ducts
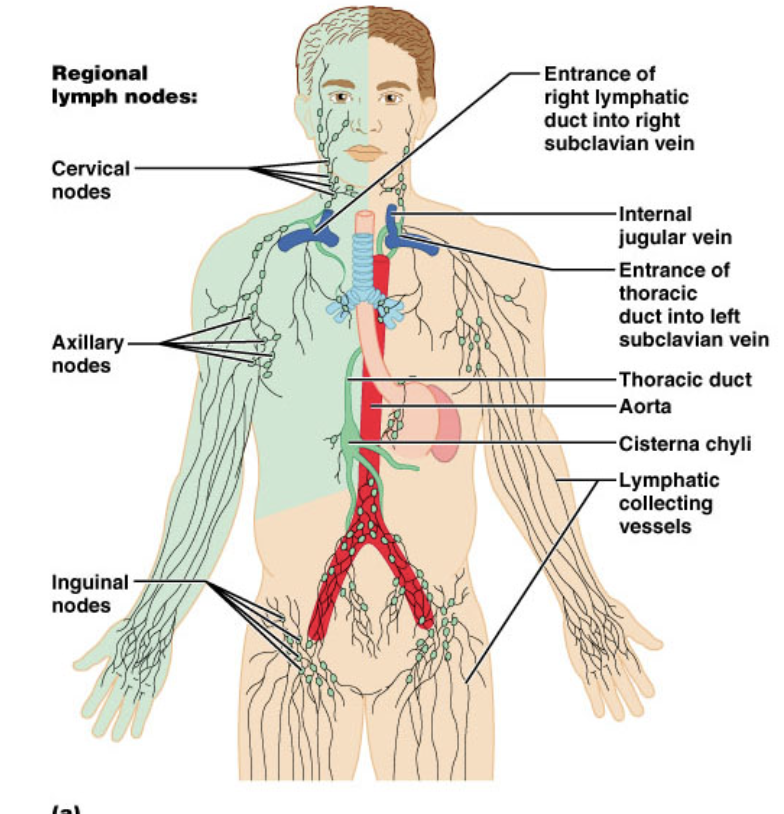
Two collecting ducts
Right lymphatic duct
Thoracic duct (left lymphatic duct)
Right Lymphatic Duct
receives lymph from right arm, right side of head and thorax
empties into right subclavian vein
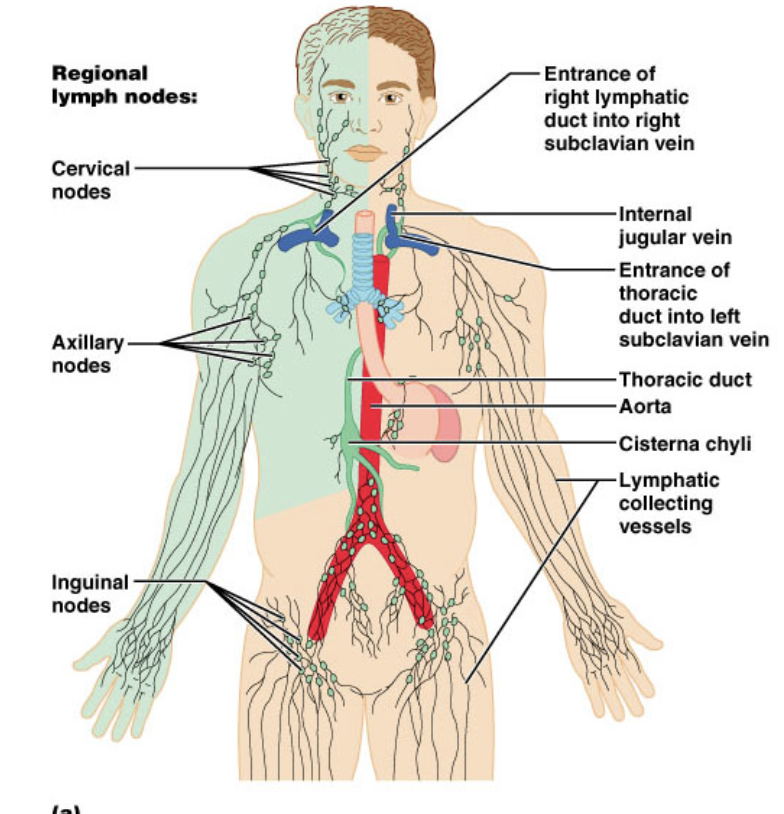
Thoracic Duct (Left Lymphatic Duct)
these ducts are larger and longer
begins as a prominent sac in abdomen called the cisterna chyli
receives lymph from below diaphragm, left arm, left side of head, neck, and thorax
empties into left subclavian vein
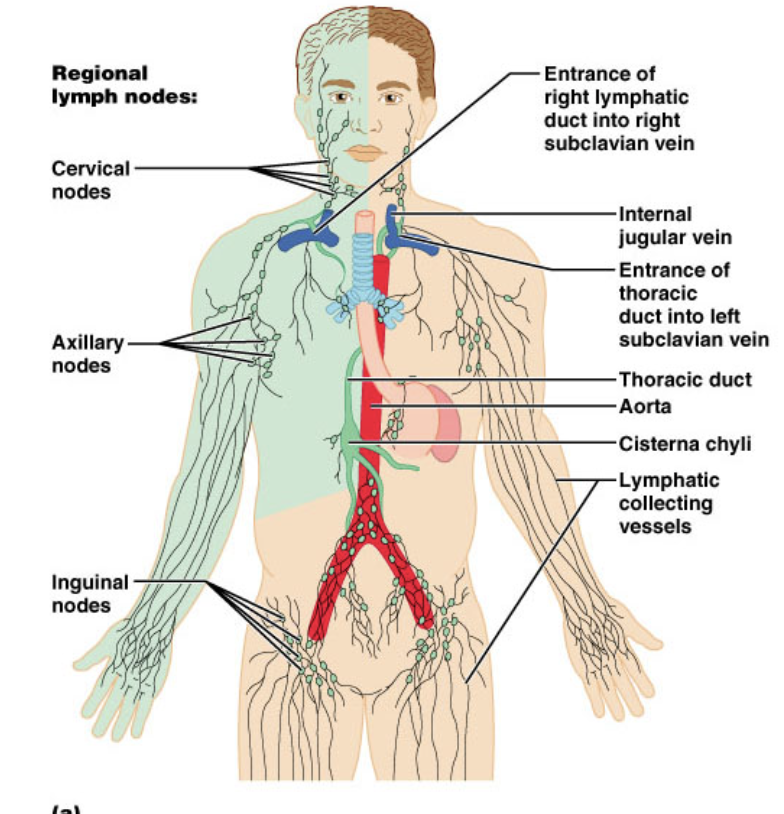
Subclavian Veins
collect from the ducts
the ducts drain into these veins
Flow of Lymph
Lymph flows under forces similar to those that control venous return, except no pump (heart)
Lymph flows at low pressure and slower speed than venous blood
Moved along by rhythmic contractions of lymphatic vessels
Stretching of vessels stimulates contraction
Flow is aided by skeletal muscle pump
Arterial pulsation rhythmically squeezes lymphatic vessels
One-Way Valves prevent backward flow
Rapidly flowing blood in subclavian veins, draws lymph into it
Exercise significantly increases lymphatic return
Categories of Lymphatic Cells:
Natural Killer (NK) Cells
T Lymphocytes (T cells)
B Lymphocytes (B cells)
Macrophages
Dendritic Cells
Reticular Cells
Natural Killer (NK) Cells
Large lymphocytes that attack and destroy bacteria, transplanted tissue, host cells infected with viruses or that are cancerous
like the hall monitor, up in everyones business
“do you belong here?, or are you doing what you need to do?”
find cells that don’t belong and kill them
T Lymphocytes (T cells)
made in thymus
do the dirty work
targets things with antibodies
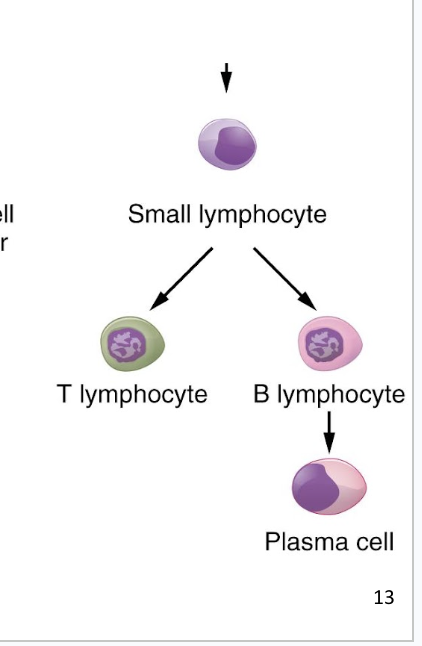
B Lymphocytes (B cells)
come from bone marrow
Activation causes proliferation and differentiation into plasma cells that produce antibodies
focus on making antibodies that will direct the T lymphocytes and tell them what to focus on
Macrophages
Large, very phagocytic cells of connective tissue
Develop from monocytes
Eat tissue debris, dead neutrophils, bacteria, and other foreign matter
Process foreign matter and display antigenic fragments to certain T cells, alerting immune system to the presence of the enemy
They are antigen-presenting cells (APCs)
decorate themselves in the pieces of what they ate
show the lymphatic cells “look what i found”
the lymphatic cells kinda ignore them
sometimes a lymphocyte will be activated by what the macrophage presents, but not often
Dendritic Cells
Branched, mobile APCs found in epidermis, mucous membranes, and lymphatic organs
Alert immune system to pathogens that have breached the body surface
are localized in our skin
primarily on outer wall
first line of defense in our body
go on parts of body that are exposed to external environment
Reticular Cells
Branched stationary cells that contribute to the stroma of a lymphatic organ
in reticular tissue (primarily the lymph nodes)
primarily stationary in the lymph nodes
are another form on antigen-presenting cells
alert lymphocytes of what they found
Diffuse Lymphatic Tissue
simplest form
Lymphocytes are scattered (not clustered)
Prevalent in body passages open to the exterior
Respiratory, digestive, urinary, and reproductive tracts
Mucosa-associated lymphatic tissue (MALT)
Lymphatic Nodules (Follicles)
Dense masses of lymphocytes and macrophages that congregate in response to pathogens
Constant feature of the lymph nodes, tonsils, and appendix
Aggregated lymphoid nodules
dense clusters in the ileum, the distal portion of the small intestine
Primary Lymphatic Organs
where lymphocytes concentrate/mature/are trained
Red bone marrow and thymus are primary lymphatic organs
Site where T and B cells become immunocompetent: able to recognize and respond to antigens
Secondary Lymphatic Organs
Lymph nodes, tonsils, and spleen are secondary lymphatic organs
Immunocompetent cells populate these tissues
still have high concentration of lymphocytes, but they don’t get as much “training”
Red Bone Marrow
Red bone marrow is involved in hemopoiesis (blood formation) and immunity
Soft, loosely organized, highly vascular material
Separated from osseous tissue by endosteum of bone
As blood cells mature, they push their way through the reticular and endothelial cells to enter the sinus and flow away in the bloodstream
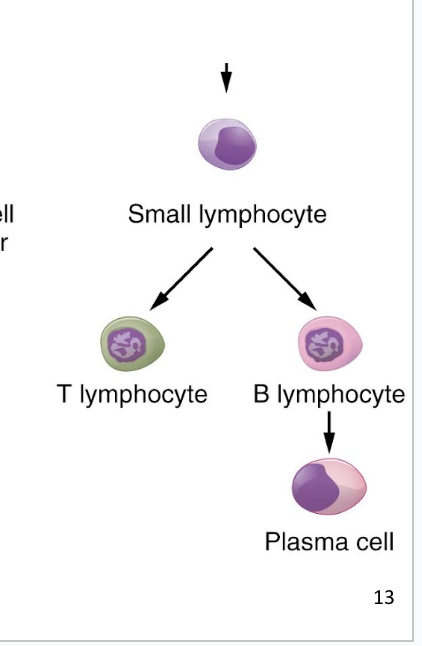
Thymus
member of the endocrine, lymphatic, and immune systems
Houses developing lymphocytes
Secretes hormones regulating their activity
has lots of reticular tissues so it can filter lymphatic fluid and train lymphocytes
Bilobed organ located anterior to the aortic arch
Degeneration (shrinkage) with age
turns into fat and scar tissue as we age
thymus is the size of our heart when born, but shrinks with age
Thymus Structure
has trabeculae (septa) that divide the gland into several lobes
Lobes have a cortex and a medulla populated by T lymphocytes
Epithelial cells seal off cortex from medulla forming a blood–thymus barrier
Produce signaling molecules that regulate the immune system
thymosin, thymopoietin, thymulin, interleukins, and interferon
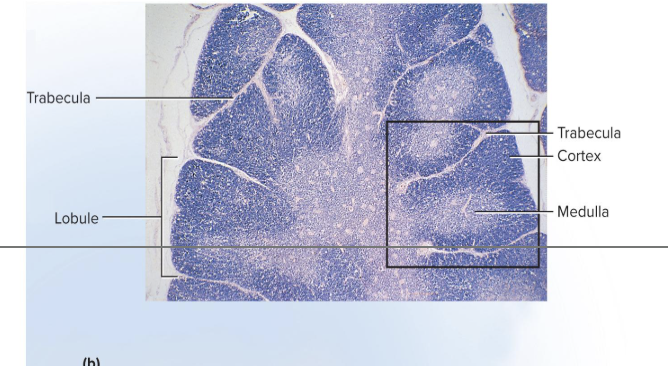
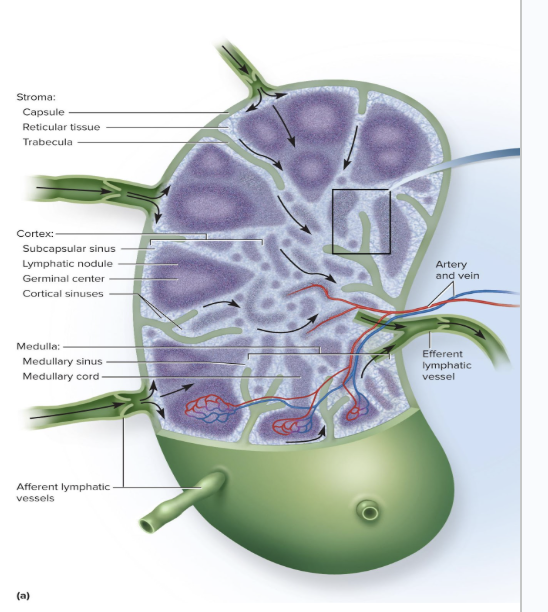
Lymph Nodes
where we have lymphatic vessels coming together, and a lot of reticular tissue to filter the lymph
Serve two functions
Cleanse the lymph
Act as a site of T and B cell activation
more vessels going in than going out
allows for fluid to be gently pressurized so it can be pushed through reticular tissue to be filtered
the debris left over after being filtered is eaten up my macrophages which present them to the B and T lymphocytes
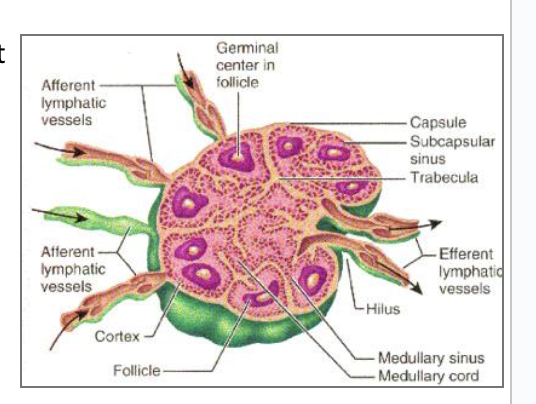
Lymph Node Structure
are the most numerous lymphatic organ
About 450 in typical young adult
Elongated, bean-shaped structure with hilum
has trabeculae that divide interior into compartments
divided into cortex and medulla
Creates germinal centers where B cells multiply and differentiate into plasma cells
Several afferent lymphatic vessels lead into the node along its convex surface
Lymph leaves the node through one to three efferent lymphatic vessels that leave the hilum
Metastasis
cancerous cells break free from original tumor, travel to other sites in the body, and establish new tumors
Metastasizing cells easily enter lymphatic vessels
Tend to lodge in the first lymph node they encounter
Multiply there and eventually destroy the node
Swollen, firm, and usually painless
Tend to spread to the next node downstream
Treatments for Breast Cancer
lumpectomy, mastectomy, along with removal of nearby axillary nodes
lumpectomy is when surgeons take a radioactive dye that is preferentially metabolized by cancer cells so they can remove that specific area
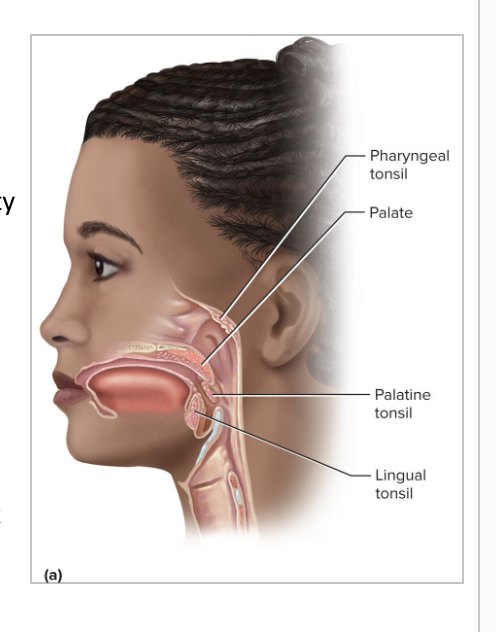
Tonsils
patches of lymphatic tissue located at the entrance to the pharynx (back of throat)
Guard against ingested or inhaled pathogens
Covered with epithelium
Have deep pits: tonsillar crypts lined with lymphatic nodules
Can get tonsillitis and/or a tonsillectomy
3 main sets of tonsils
Palatine Tonsils
Lingual Tonsils
Pharyngeal Tonsils
Palatine Tonsils
Pair at posterior portion of the oral cavity
Most often infected
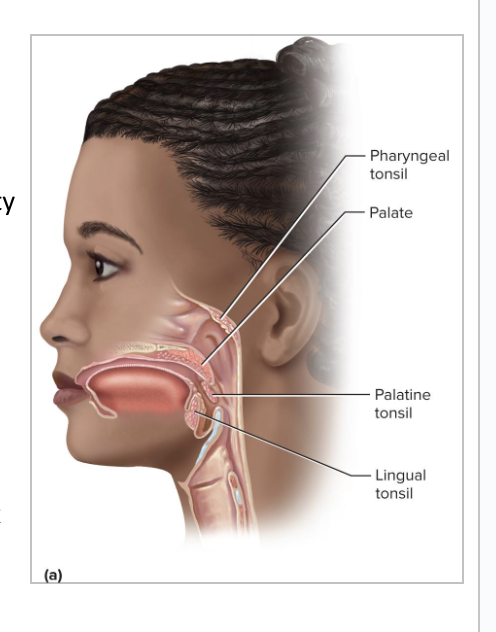
Lingual Tonsils
Pair at root of the tongue
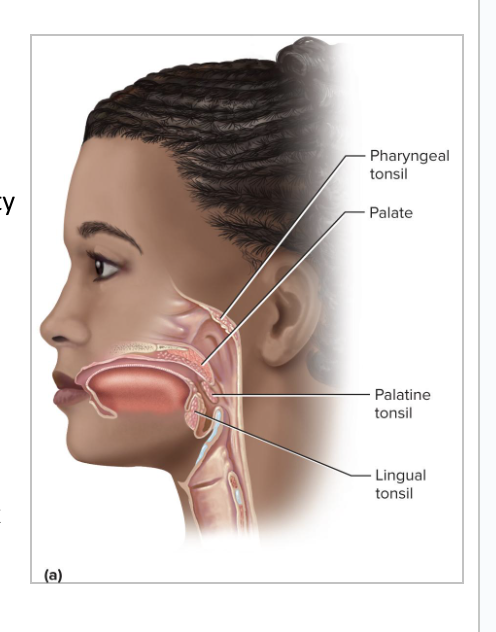
Pharyngeal Tonsils
aka adenoids
Single tonsil on wall of nasopharynx
Spleen
the body’s largest lymphatic organ
Two types of tissue
Red pulp : sinuses filled with erythrocytes
spleen is mostly red pulp
White pulp: lymphocytes, macrophages surrounding small branches of splenic artery
Spleen is highly vascular and vulnerable to trauma and infection
Ruptured spleen requires splenectomy, but this leaves person susceptible to future infections, premature death
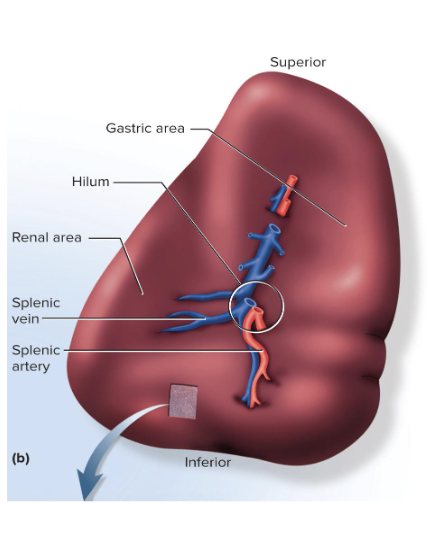
Functions of the Spleen:
Lets healthy RBCs come and go
For old, fragile RBCs, spleen is a “erythrocyte graveyard”
Blood cell production in fetus happens in the spleen (and in very anemic adults)
White pulp monitors blood for foreign antigens and keeps an army of monocytes for release when needed
Stabilizes blood volume through plasma transfers to lymphatic system
Pathogens
agents capable of producing disease
Include viruses, bacteria, and fungi
3 lines of defenses against pathogens:
First line of defense:
skin and mucous membranes
aka the physical barrier
difficult for pathogens to pass through the skin
Second line of defense: several innate defense mechanisms
Leukocytes and macrophages, antimicrobial proteins, natural killer cells, inflammation, and fever
generically targets cells that don't belong, does not target specific species of pathogens
Third line of defense: adaptive immunity
Defeats a pathogen and leaves the body with a “memory” of it so it can defeat it faster in the future
targets one specific strain of one specific pathogen
Innate Defenses
built-in defenses that guard equally against a broad range of pathogens
They can’t remember pathogens
3 kinds of innate defenses:
Protective proteins
Protective cells
Protective processes
They are local, nonspecific, and lack memory
innate immune system is very energy intensive
Adaptive Immunity
body must develop separate immunity to each pathogen
Body adapts to a pathogen and wards it off more easily upon future exposure (memory)
adaptive immune system is more efficient, but has less variety
Skin as an External Barrier:
Makes it mechanically difficult for microorganisms to enter the body
Toughness of keratin
Too dry and nutrient-poor for microbial growth
Has an acid mantle
thin film of lactic and fatty acids from sweat and sebum that inhibits bacterial growth
staphylo - can grow in the acid mantle
oil glands release sebum that contains proteins that are inherently antimicrobial
Peptides in the skin that kill microbes:
Dermicidin, defensins, and cathelicidins
Mucous Membranes as External Barriers
Digestive, respiratory, urinary, and reproductive tracts are open to the exterior and protected by mucous membranes
Mucus physically traps microbes and moves them away to be disposed of
Contains lysozyme
enzyme that destroys bacterial cell walls
Cells involved with the second stage of defense:
Phagocytes
Neutrophils
Eosinophils
Basophils
Monocytes
Lymphocytes
Neutrophils
Wander in connective tissue killing bacteria*
2 Mechanisms to Destroy:
Can kill using phagocytosis and digestion
Can kill by producing a cloud of bactericidal chemicals
they release bleach and hydrogen peroxide next to a bacteria
this destroys the bacterial cell, as well as its own plasma membrane, destroying themselves too
called a respiratory burst
Eosinophils
Found especially in mucous membranes
Guard against parasites, allergens (allergy-causing agents), and other pathogens
Kill tapeworms and roundworms by producing superoxide, hydrogen peroxide, and toxic proteins
they don't self destruct when producing the oxidizing chemicals like neutrophils do
recruit basophils and mast cells
they release histamine for an inflammatory response
Phagocytize antigen–antibody complexes
Limits action of histamine/ inflammatory response
Basophils
Secrete chemicals that recruit other cells to site of infection
Leukotrienes: activate and attract neutrophils and eosinophils
Histamine: a vasodilator, which increases blood flow
Speeds delivery of leukocytes to the area
Heparin: inhibits clot formation
Clots would slow leukocyte mobility
Mast Cells
Mast cells also secrete these substances (leukotrienes, histamine, and heparin)
Type of connective tissue cell very similar to basophils
basophils often differentiate into mast cells
Lymphocytes
most dynamic component of the adaptive immune system
Three basic categories: T, B, and NK cells
Circulating blood contains
80% T cells
15% B cells
5% NK cells
Many diverse functions
NK cells are a part of the innate system and the adaptive immune system
all others are part of adaptive immunity;
helper T cells also function in both
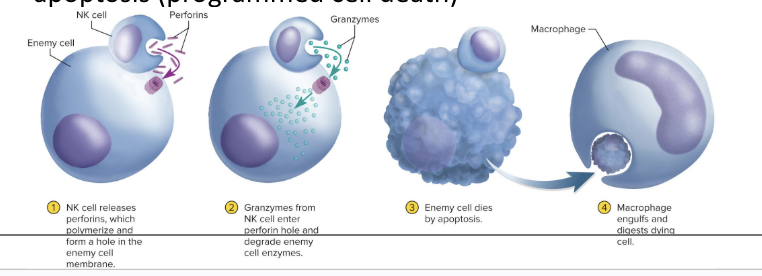
Natural Killer Cells and How They Work:
involved in both innate and adaptive immunity
patrols connective tissue of the body
primarily binds to things that might not belong to the body,
if the thing it binds to doesnt have the correct id tag, the NK cell will kill it
releases perforins which will form a pore in the membrane of the target cell
Then the NK cell secretes granzymes into the pore and starts to break up proteins in the target cell
the proteins lose structure and function, causing cell to go through apoptosis
Monocytes
move from the blood into connective tissues and transform into macrophages
Macrophage System
all the body’s phagocytic cells, except leukocytes
Includes
Wandering macrophages
Fixed macrophages
Wandering Macrophages
Macrophages that actively seek pathogens
Widely distributed in loose connective tissue
patrol the body looking for things that don’t belong
look for chemical messengers released from WBCs
Fixed Macrophages
Macrophages that only phagocytize pathogens that come to them
are stuck in a specific organ
Examples include:
Microglia —in central nervous system
Alveolar macrophages —in lungs
Hepatic macrophages —in liver
Antimicrobial Proteins
Proteins that inhibit microbial reproduction and provide short-term, innate immunity to bacteria and viruses
Two families of antimicrobial proteins:
Interferons
Complement system
Interferons
antimicrobial proteins that are secreted by cells infected by viruses and interfere with viral propagation
They alert neighboring cells and protect them from becoming infected
Bind to surface receptors on neighboring cells
Activate second-messenger systems within
second cell will then start making proteins that will help fight against the virus
The first cell receives no benefit from the interferon it creates (paracrine signal)
Interferons also activate NK cells and macrophages
These destroy the infected cell before it can transfer newly replicated viruses
Activated NK cells destroy malignant cells
interferons are specific to the virus
Complement System
a group of 30 or more globular proteins that make powerful contributions to both innate immunity and adaptive immunity
Synthesized by liver
Circulate in the blood in inactive form
Are activated by presence of a pathogen
When activated, there is positive feedback loop that ultimately destroys the target cell
What are the 4 methods of pathogen destruction that occur when a complement system is activated?
Inflammation
Immune clearance
Phagocytosis
Cytolysis
Inflammation in Complement Systems
C3a protein stimulates mast cells and basophils to secrete histamine and other inflammatory chemicals
Activates and attracts neutrophils and macrophages
Speeds pathogen destruction in inflammation
bc there is increased blood flow so more WBC can get to the area
Immune Clearance in Compliment Systems
C3b causes pathogen to get linked/clumped together
C3b protein binds with antigen–antibody (Ag-Ab) complexes to red blood cells
These RBCs circulate through liver and spleen
Macrophages of those organs strip off and destroy the Ag–Ab complexes leaving RBCs unharmed
Main way of clearing foreign antigens from the bloodstream
idea is that one viral protein is not a big target, but when they are grouped together in one location, that will elicit a much stronger response from immune system
Phagocytosis in Complement Systems
Neutrophils and macrophages cannot phagocytize “naked” bacteria, viruses, or other pathogens
SO, C3b assists them by opsonization
Coats microbial cells and serves as binding sites for phagocytes
Makes the foreign cell more appetizing to be eaten up by phagocytes
Cytolysis in Complement Systems
complement proteins can attach together and make a pore
C3b protein splits complement protein C5 into C5a and C5b
C5b binds to the enemy cell
Attracts more complement proteins until a membrane attack complex forms
Forms a hole in the target cell
Electrolytes leak out
water flows in rapidly
cell ruptures
Complement Activation
when the complement system is activated, it can do 4 different things:
Inflammation
Immune Clearance
Phagocytosis
Cytolysis