Psych 3501 Exam 3: Journal Club 3
1/5
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
6 Terms
Background
Comorbid PTSD + MDD associated with worse outcomes
PTSD & MDD associated with sleep disruption
Majority of PTSD or MDD have sleep disruptions
Sleep disruption predict the onset of depression
After PTSD treatment, the majority still have residual sleep disturbances
Limitations of RCT strict exclusions
RCT: looking for very specific group of people
Social rhythm model of mood dysregulation
Aim: examine the efficacy of group CBSRT in veterans with PTSD + MDD + sleep disruption
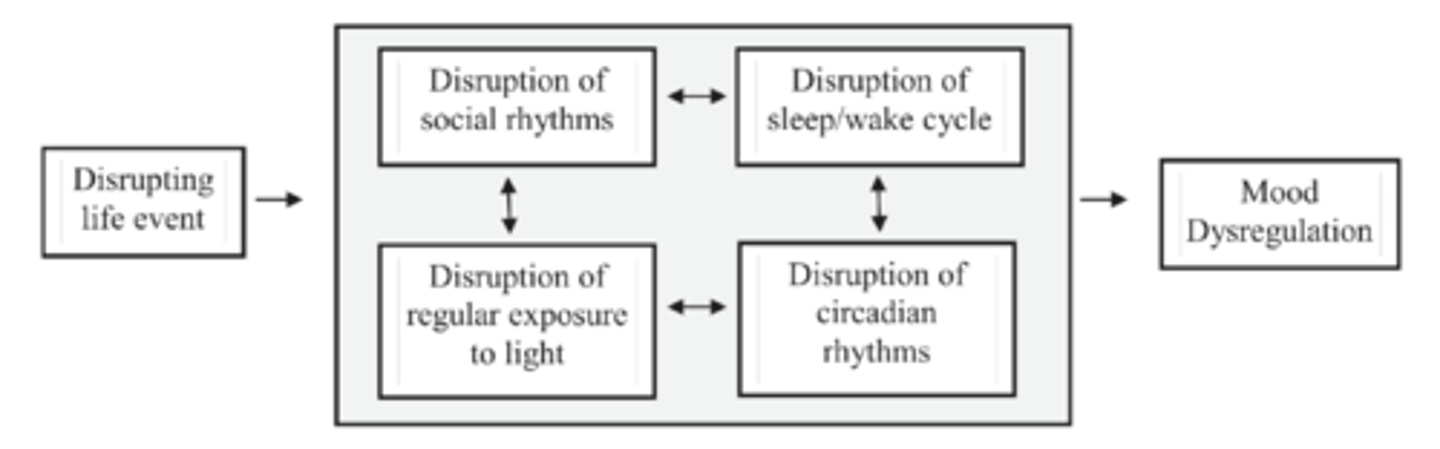
Basic idea: stressful life events disrupt social rhythms which provide time cues to circadian rhythms, contributing to mood dysregulation
Give attention to the role of light as the primary time cue for the circadian clock
Methods: participants
N = 24 male veterans
75% white
Age 54.17 +/- 9.89
PTSD, MDD (moderate symptom severity +), sleep disruption
Meet criteria and at least moderate severity for both disorders
Experiencing sleep disruptions
Exclusion criteria
- Psychotic, bipolar, substance use disorder
- Shift work
- Severe sleep disorder, neurological disorder, other untreated medical condition
- Unstable medication
- Currently engaged in CBT for PTSD
Methods: procedure
12 weeks of group CBSRT, ~ 2 hours per session
First hour: homework review
Second hour: introducing new skills
Session 1-2: CBT strategies
- Cognitive restructuring, mood monitoring, etc.
Session 5: create new social rhythm
- Create a stable social rhythm schedule
Session 6-8: increase contact with zeitgebers
- Provide consistent time cues to the biological clock
Session 8-10: sleep medicine strategies
- Stimulus control, imagery rehearsal therapy for nightmares
Session 10-12: relapse prevention, summary
- What was learned, going over strategies for relapse prevention
Methods: measures
Screening measures
Structured clinical interview for DSM-IV
Polysomnography
- Information about possible sleep disorders
Process measures
Social rhythm metric
Both as a therapeutic measure & to examine the change process
Outcome measures
Daily sleep diary
Hamilton Rating Scale for Depression
Clinician administered PTSD scale
Results
Sleep onset latency, wake after sleep onset, # of awakenings, sleep quality, and nightmares improved from pre to post treatment; gains maintained at 3 months
PTSD symptoms improved from pre to post treatment; gains maintained at 3 months
Depression symptoms improved from pre to post treatment; mixed evidence for gains maintained at 3 months
Social rhythm stability increased from pre to post treatment
Increased social rhythm stability correlated with change in PTSD symptoms but not depression symptoms
- CBSRT should reduce symptoms of PTSD and MDD through improving social rhythm stability