Chapter 8: Dysrhytmia Interpretation & Management
1/22
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
23 Terms
When an electrical signal in the heart is aimed directly at the positive electrode, the nurse interprets that the deflection seen on the 12-lead ECG or rhythm strip will be
positive
Rationale: When assessing the 12-lead ECG or a rhythm strip, it is helpful to understand that the electrical activity is viewed in relation to the positive electrode of that particular lead. The positive electrode is the “viewing eye” of the camera. When an electrical signal is aimed directly at the positive electrode, an upright inflection is visualized. If the impulse is going away from the positive electrode, a negative deflection is seen, and if the signal is perpendicular to the imaginary line between the positive and negative poles of the lead, the tracing is equiphasic, with equally positive and negative deflection.
The nurse is interpreting the rhythm strip of a patient and measures the QRS complex as being three small boxes in width. The nurse interprets this width as
0.12 seconds
The nurse is interpreting a patient’s cardiac rhythm and notes that the PR interval is 0.16 seconds long. The nurse determines that this PR interval indicates
normal conduction from the SA node through the AV node.
The patient is complaining of midsternal chest discomfort and nausea. The nurse calls for a 12-lead ECG and notices that the ST segment is newly elevated in two related leads. The nurse should
call the provider because the ST segment may indicate myocardial injury.
Rationale: A displacement in the ST segment can indicate myocardial ischemia or injury. If ST displacement is noted and is a new finding, a 12-lead ECG is performed and the provider notified. The patient is assessed for signs and symptoms of myocardial ischemia.
The nurse is calculating the rate for a regular rhythm. There are 20 small boxes before each R wave. The nurse interprets the rate to be
75 bpm
The nurse is caring for an individual who is admitted for chest pain and shortness of breath. The patient states, “I can’t believe I’m having chest pain. I’m a marathon runner and in good shape.” During the night, the patient develops a sinus bradycardia with a heart rate of 40 beats/min. The nurse should
assess the patient for signs of decreased cardiac output.
The patient is admitted with a heart rate of 144 beats/min and a blood pressure of 88/42 mm Hg. The patient complains of generalized weakness and fatigue. He states, “Just let me sleep.” The nurse determines that the presence of the patient’s symptoms is due to
decreased cardiac output
Rationale: The fast heart rhythm may cause a decrease in cardiac output because of the shorter filling time for the ventricles. Vulnerable populations are those with ischemic heart disease who are adversely affected by the shorter time for coronary filling during diastole.
If the sinus node were diseased or ischemic and no longer firing as the heart’s primary pacemaker, the nurse would anticipate which normal compensatory mechanism?
Junctional escape rhythm, rate of 45
The patient complains of being lightheaded and feeling a “fluttering” in his chest. The nurse places the patient on the heart monitor and notices an atrial tachycardia at a rate of 160 beats/min. The patient’s blood pressure has dropped from 128/76 mm Hg to 92/46 mm Hg but appears stable at the lower pressure. The nurse should
call the provider and prepare the patient for medical or electrical cardioversion.
The nurse notices ventricular tachycardia on the heart monitor. The nurse’s first action should be to
determine patient responsiveness and presence of a pulse.
The nurse is speaking with the patient when the monitor shows that the patient is in ventricular fibrillation (VF). The nurse should
assess the patient and check the patient’s monitor leads.
rationale: Ventricular fibrillation (VF) is a chaotic rhythm characterized by a quivering of the ventricles, which results in total loss of cardiac output and pulse. Because this patient was in the process of speaking with the nurse, there is evidence of cardiac output being present, which would not be the case with VF. Because a loose lead or electrical interference can produce a waveform similar to VF, it is always important to immediately assess the patient for pulse and consciousness. The issue here is more likely a loose lead. Immediate BLS and ACLS interventions would only be required if the patient was truly in VF.
The patient with a pacemaker shows pacemaker spikes that are not followed by a QRS. The nurse interprets this as
failure to capture
rationale: When the pacemaker generates an electrical impulse (pacer spike) and no depolarization is noted, it is described as failure to capture. Failure to pace or fire occurs when the pacemaker fails to initiate an electrical stimulus when it should fire. The problem is noted by absence of pacer spikes on the rhythm strip. Failure to sense manifests as pacer spikes that fall too closely to the patient’s own rhythm, earlier than the programmed rate. The demand mode paces the heart when no intrinsic or native beat is sensed.
The patient has a temporary transvenous, demand-type ventricular pacemaker. The rate on the pacemaker is set at 60 beats/min. Which of the following situations would be of concern?
A pacemaker spike is seen on the T wave of the preceding beat.
rationale: Failure to sense manifests as pacer spikes that fall earlier than the programmed rate. This can cause an artificial R-on-T phenomenon similar to when a PVC occurs during the T wave, and ventricular tachycardia may occur.
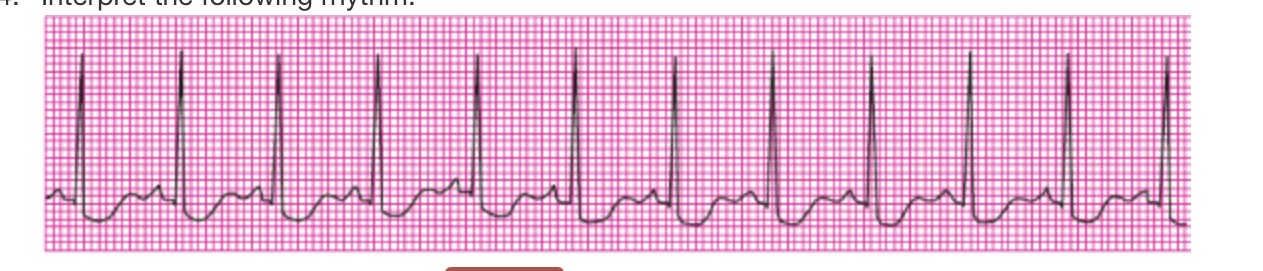
interpret the rhythm
sinus tachycardia
Sinus tachycardia results when the SA node fires faster than 100 beats/min. In sinus bradycardia, the rate is less than 60 beats/min. In atrial flutter, the atrial focus fires at an extremely rapid, regular rate, between 240 and 320 beats/min. The P waves are called flutter waves and may have a sawtooth appearance.

interpret the rhythm
a flutter
interpret the rhythm
junctional escape rhythms
A junctional escape rhythm has either an inverted P wave and short PR interval (less than 0.12 seconds) preceding the QRS complex, no P wave, or a P wave that follows the QRS complex. Heart rate is 40 to 60 beats/min. The rhythm is regular.

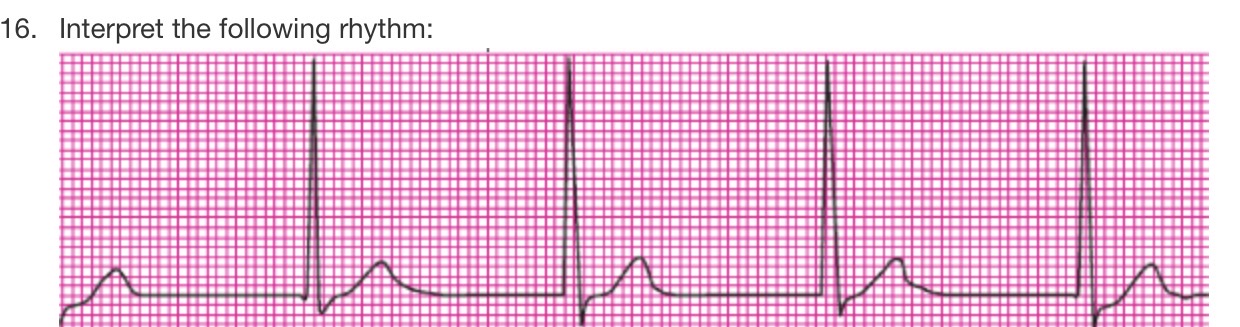
interpret the rhythm
sinus rhythm with multifocal PVC’s
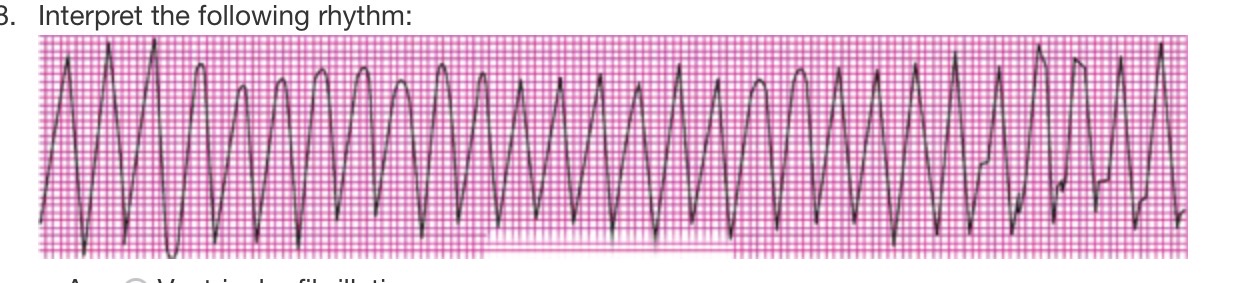
interpret the rhythm
v tach
Ventricular tachycardia (VT) is a rapid, life-threatening dysrhythmia originating from a single ectopic focus in the ventricles. It is characterized by at least three PVCs in a row. VT occurs at a rate greater than 100 beats/min.

interpret the rhythm
v fib
Ventricular fibrillation (VF) is a chaotic rhythm characterized by a quivering of the ventricles, which results in total loss of cardiac output and pulse. VF produces a wavy baseline without a PQRST complex.

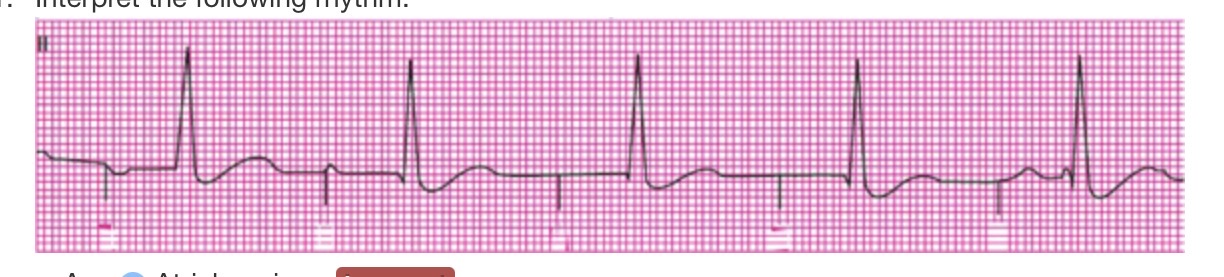
interpret the rhythm
2nd degree AV block-Mobitz I
Also called Wenckebach phenomenon, second-degree AV block type I is represented on the ECG as a progressive lengthening of the PR interval until there is a P wave without a QRS complex. The AV node progressively delays conduction to the ventricles, resulting in a longer PR interval until finally a QRS complex is dropped
The patient is admitted with an anterior wall myocardial infarction. With this diagnosis, the nurse would expect to see Q waves in which leads? (Select all that apply.)
III
V3
Pathological Q waves are found on ECGs of individuals who have had myocardial infarctions, and they represent myocardial muscle death.
interpret the rhythm
atrial ventricular pacing
The patient is admitted with the diagnosis of “Junctional Rhythm.” The nurse places the patient on the cardiac monitor expecting to see: (Select all that apply.)
P waves with a PR interval of 0.16 seconds.
P waves with a PR interval less than 0.12 seconds.
no P waves but a narrow QRS complex.