PSL300 Final (copy)
1/97
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
98 Terms
4 Somatic senses
Touch
Temperature
Proception
Awareness of your body parts relative to each other
Nociception
Detection of tissue damage or threats, perceived as pain.
Somatosensory receptors
All on neuron cells
For sensations below your chin, the receptor cell bodies are in the dorsal root ganglia.
For sensations above the head, the receptor cell bodies are in the brain itself.
For both sensation locations, the part of the neurons that transduce the physical stimulus into an electrical signal are in the nerve endings. (Tips of skin, fibers, viscera)
Types of sensory receptors on skin
Free nerve endings
Detect mechanical stimuli, temperature, chemicals.
In the epidermis, the outermost layer of the skin.
Merkel receptors
Mechanoreceptors that are nerve endings in close contact with specialized epithelial cells called Merkel cells.
Fine texture and pressure.
Tonic so fire as long as the stimulus is present.
In the base of the epidermis
Encapsulated receptors
Two parts, Meissner which is in hairless parts, specific to light, touch, and low frequency vibrations. Are phasic so respond to changes in stimulus.
And Pacinian corpuscles which respond to pressure and high frequency vibrations. Also phasic.
Deeper in the dermis.
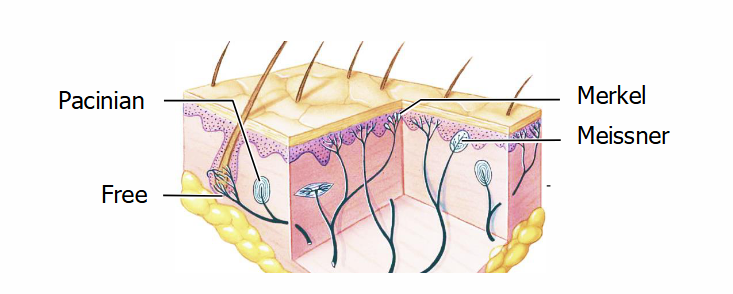
Merkel discs
The Merkel receptors.
Saucer shaped receptors at the bottom of the epidermis.
Very sensitive to deformations on the skin → good at detecting fine details and texture.
Tonic, making them good at signaling continuous contact on the skin.
Are more receptors phasic or tonic
Most receptors are phasic.
After 3 ms, the membrane goes back to its steady state in the phasic receptor areas.
This is why you dont feel your clothes on your skin
Meissner corpuscles
A type of egg-shaped encapsulated receptor near the top of the dermis.
Found in hairless regions like your tongue and lips.
Responsible for detecting light touch and low frequency vibrations.
They are phasic, so they detect changes in shear/movement.
Have loop endings that detect sideways shearing/when you move your hand sideways.
Pacinian corpuscles
An onion shaped encapsulated receptor deep in the dermis.
The nerve endings are arranged in a lot of layers, allowing them to detect very small displacements in skin.
Phasic, respond to vibrations or other fast-changing stimuli.
Receptor distribution
Palms, fingertips, and lips have a lot of densely packed receptors → have higher acuity ( ability to detect fine details and small differences)
Thermal receptors
A type of free-nerve ending.
Cold receptors respond maximally at ~30°C
Warm receptors at ~45°C
They are both phasic-tonic, allowing us to get used to water temperature.
Above 45 degrees, the pain receptors get activated but also the cold receptors for a second → leads to paradoxical cold where hot things feel cold for a second.
We have more cold receptors than warm, and few thermoreceptors in total
Nociceptors
A type of free nerve ending.
Some respond to chemicals released by damaged cells or serotonin released by platelets during injury.
Lots of nociceptors have ion channels in the transient receptor potential (TRP) channel family.
Ex. TRPV1 channels, called vanilloid receptors, respond to damaging heat and chemicals. TRPM8 channels respond to cold and to menthol.
Somatosensory afferent fibers
Carry signals from the sensory receptors to the CNS
Two main types.
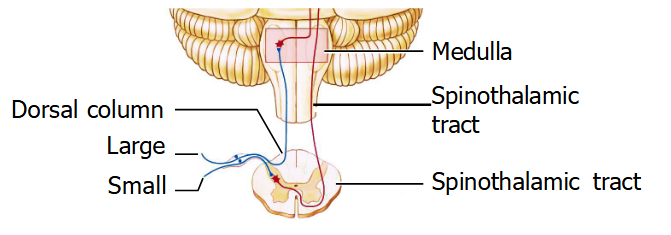
Small fibers
Small fibers include the C and A delta fibers and come from free nerve endings.
C fibers are unmyelinated → no conducting sheath so produce slow action potentials at 2 m/s
The A delta fibers are thicker and myelinated → can conduct faster action potentials at 30 m/s.
They respond to different adequate stimuli
Small fibers carry information about things like pain and temperature → enter spinal cord → synapse onto secondary order neurons at dorsal horn → axons cross the midline → ascend contralaterally in the spinothalamic tracts, located in lateral part of the spinal cord.
evoke simple responses to specific stimuli like moving your hand when you feel something hot, shooing a bug away.
can be handled in the spinal cord, without immediate input from the brain
Large fibers
Large fibers include A Beta fibers and come from Merkel disks or encapsulated mechanoreceptors such as Meissner or Pacinian corpuscles
Myelinated and very fast signal conduction at 70 m/s
Large fibers carry information from your mechanoreceptors → go up the spinal cord ipsilaterally (go up the same side that the entered) → at the spinal cord, they turn upwards → go through dorsal columns → at the medulla, synapse into secondary order neurons → axons cross the mid line contralaterally (go the the opposite side) → somatosensory cortex.
provide feedback to the brain, especially to motor cortex, as it manipulates objects
Their information has to travel a long way (up to the brain) quickly
Movement of signals
Signals from the spinal cord pass through the thalamus → thalamus directs signals to the appropriate region of the brain.
Signals below the chin are directed by ventroposterolateral (VPL) nucleus
Signals above the chin are directed by the ventroposteromedial nucleus (VPM)
Both pass to the primary sensory cortex called S1.
In the parietal lobe.
Somatotropic, so Neighboring areas of skin project to neighboring cells in cortex
This makes S1 a map of contralateral body surfaces, but it is distorted cuz areas of high sensitivity and acuity (such
as hands and lips) get more space.
Lateral inhibition of somatosensory fibers
lateral inhibition enhances spatial differences
If you step into a very hot bath, you feel the most discomfort not in your foot but at the line formed by the water surface around your leg, because that is the temperature edge
Pain
There are 2 types of pain that can be responded to
Fast (carried by A delta fibers) and slow (carried by C fibers)
We have two types of pain because of the different responses that can be elicited.
Quick withdrawal, a spinal reflex
Prolonged immobilization that leads to healing.
Descending pathways through the thalamus can block nociceptive cells in the spinal cord in situations where you need to ignore pain to survive.
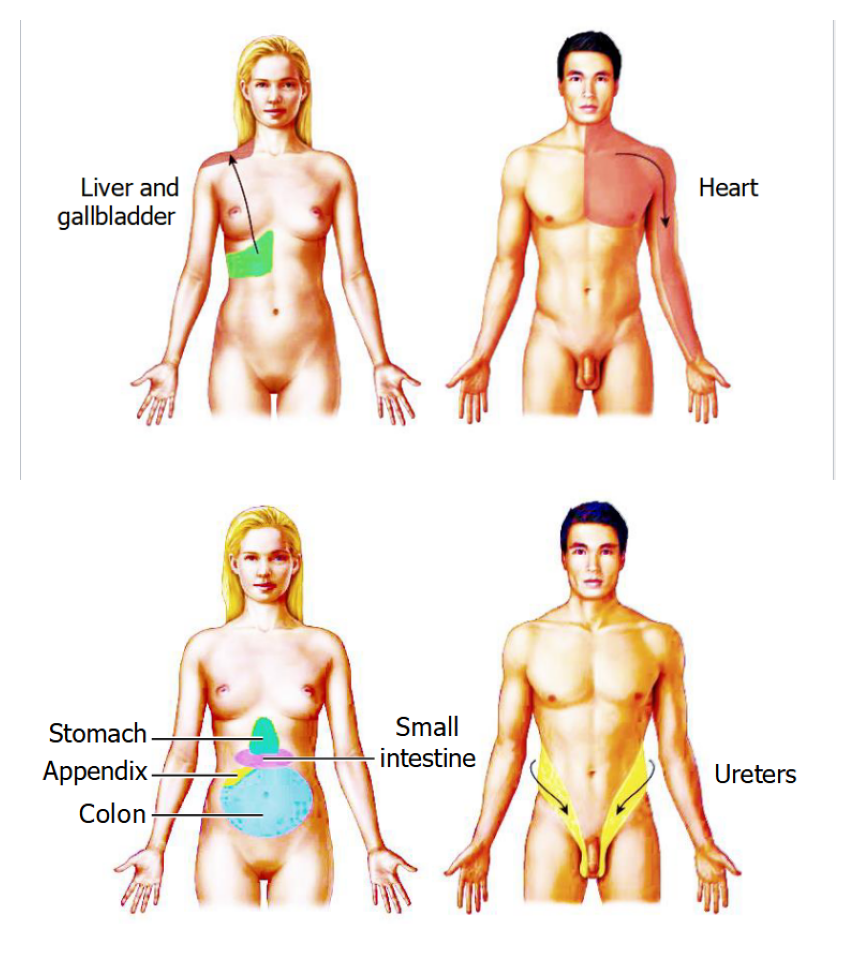
Pain that happens in your internal organs is called referred pain.
Nociceptors from different locations converge on a single ascending tract → tract sends signals to the brain → the brain doesn’t know where the stimulus came from
It assumes the problem is on a body surface cuz that is more common than organ pain.
When you get pain, the c fibers carry the pain to the secondary neurons → those secondary neurons are inhibited by a beta fibers through interneurons → activation of a beta fibers can dampen or block pain.
Pain and the body region
Drugs and pain
aspirin (Acetylsalicylic acid) inhibits prostaglandins and inflammation, and slows transmission of pain signals.
Opioids (such as morphine and codeine) decrease transmitter release from primary sensory neurons and postsynaptically inhibit secondary sensory neurons
The body makes natural painkillers such as endorphins, enkephalins, and dynorphins.
Smell
Sensed by olfactory receptors in the olfactory epithelium
The epithelium is on top of the nasal cavity and is pigmented
The pigment is correlated with sensitivity → more vibrant = more sensitive.
Each olfactory neuron has a dendrite that goes into the olfactory epithelium → forms the nonmotile cilia (tiny hairs that do not move) → increases the surface area in the olfactory epithelium → higher chance of catching odorants.
Olfactory receptors
The olfactory receptors have specificity for each type of odorant
We have 400 types of receptors = 400 types of odors
These receptors are also g protein coupled
odorant binds → Golf is activated → cAMP concentration increases → receptor neurons depolarized → AP to the olfactory bulb
Have weird properties
continually sipping in fluid and sending it along the nerves into the brain.
Called pinocytotic
hey are short-lived, degenerating after a month or 2, to be replaced by new ones from below
They send their axons into the brain through tiny holes in the cribriform (“sievelike”) plate (the bone at the base of the cranial cavity)
Olfactory bulb
extension of the cerebrum on the underside of the frontal lobes.
Once the action potential from the receptor is sent to the bulb, the axons forms the olfactory nerve, or cranial nerve I
In the frontal and temporal lobe
Convergence from many receptors can also happen onto one bulb → increases sensitivity but decreases spatial accuracy.
The olfactory bulb can project onto the limbic system
Used to be used for detecting danger and food but we don’t need that anymore so now smells just can bring up past emotions.
Pheremones
chemicals released by an animal into the environment which affect the physiology or behavior of other members of its species
Rodents have an olfactory structure in the nasal cavity called the vomeronasal organ (VNO), which is involved in their behavioral responses to sex pheromones
In humans, the VNO disappears during fetal development, but we do respond to airborne chemical signals.
Taste
Taste receptor cells are clustered into taste buds.
Each taste bud has around 100 receptors which are epithelial cells instead of neuronal cells → each taste bud has at least 5 receptor types
Types of taste receptors
Sweet receptor cells detect sugar (energy)
Umami receptor cells detect amino acid glutamate (indicating protein)
Bitter receptor cells detect poison
Salty and sour receptor cells detect Na+ and H+ — 2 important ions
The tongue may also have receptors for fatty acids
They don’t have specific locations, are all over the tongue.
Types of taste receptor cells
Type I cells may sense salt
Type II cells sense sweet, bitter and umami
Type II cells release ATP, which acts on neurons and type IIIs
Type III cells sense sour
Only type III cells form synapses with sensory neurons, activating them with serotonin
Cells for sweet, umami, and bitter have receptor molecules coupled to a G protein called gustducin → activates signal pathways → increases intracellular [Ca2+] → Triggering release of ATP.
Detection of salt and sour involves ion channels which are not linked with G proteins
Taste signal pathways
Receptor cells in the taste buds excite fibers of cranial nerves VII (facial nerve), IX (Glossopharyngeal nerve), and X (Vagus nerve) → synapse in medulla and thalamus en route to the cortex
TRP receptors in the walls of the mouth excite cranial nerve V, the trigeminal
Info about temperature, texture, etc. not taste
Hypothalamus as the control center
Controls feeding, plasma osmolality, body temperature, and sexual and stress responses
But the control over these has negative feedback that inhibits it.
Some of the control systems are needed to stay steady to maintain homeostasis.
Can do this control neurally or hormonally
Nuclei within the hypothalamus send neural signals to each other and to other parts of the brain
Synthesizes hormones which it transports down axons to the posterior pituitary, where they are released into the blood.
makes releasing hormones that travel through portal to the anterior pituitary, where they trigger the release into the blood of other hormones, made in the pituitary capillaries
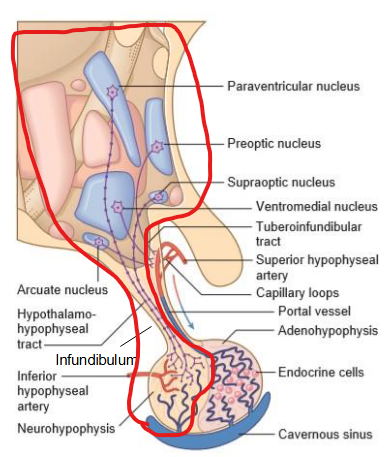
Hypothalamus control of anterior pituitary
Anterior pituitary doesn’t act alone, it is tightly regulated by parvocellular neurosecretory neurons.
Found in regions of arcuate nucleus, paraventricular nucleus, and preoptic nucleus.
These neurons send short axons to the median eminence → hormone released to primary capillary plexus supplied by superior hypophyseal artery → blood drains to hypophyseal portal veins → signals carried to secondary capillary plexus in the anterior pituitary → endocrine cells in surrounding respond by releasing their own hormones.
Allows for precise localized control of hormone secretion.
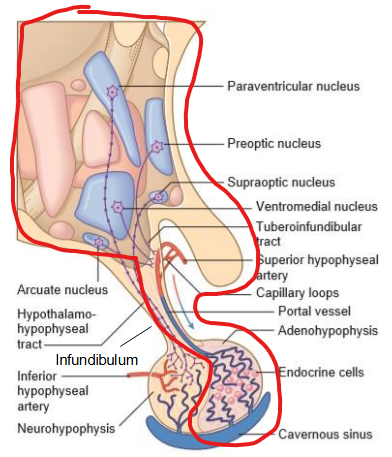
Hypothalamus control of posterior pituitary
The posterior pituitary contains the axon terminals of the paraventricular nucleus and supraoptic nucleus.
Axons pass through infundibulum → forms the hypothalamohypophyseal tract → ends in capillaries supplied by inferior hypophyseal artery.
The axons have herring bodies that store neurosecretory materials → released by stimuli → fire action potentials.
Allows hypothalamus to act as sensor and immediate responder.
Hypothalamus control of eating
Controls how much caloric intake you have.
Uses the ventromedial hypothalamus and lateral hypothalamus
Both controlled by neurons of the arcuate nucleus
One of the neurons called arcuate NPY drives feeding
Another neuron called arcuate POMC inhibits feeding.
Damage to the hypothalamus can disrupt this feeding
Damage to the ventromedial hypothalamus causes over eating
Damage to the lateral hypothalamus causes under eating
Arcuate NPY function
When fasted, arcuate NPY neurons encourage feeding.
Releases NPY, GABA, and sometimes AgRP
The arcuate NPY projects onto other hypothalamic areas.
PVN (paraventricular nucleus), a satiety or anorexigenic center that usually sends signals to the sympathetic nervous system to cause sympathetic activity → high sympathetic activity inhibits feeding.
Arc-NPY sends signals to PVN → PVN inhibited → low excitation of the sympathetic nervous system → feeding not inhibited.
LH (Lateral hypothalamus), a feeding center.
Arc-NPY sends signals to LH → LH excited → orexin released at synapses → PVN inhibited and feeding stimulated.
Arcuate POMC function
After a meal, arcuate POMC neurons inhibit feeding.
POMC is cleaved to make α-melanocyte stimulating hormone (α-MSH)
Arcuate POMC also projects on other hypothalamic regions.
α-MSH excites PVN → excite sympathetic nervous system → high sympathetic activity decreases feeding
α-MSH excited VMH (ventromedial hypothalamus) → excited sympathetic nervous system → high sympathetic activity decreases feeding
α-MSH inhibits dorsomedial hypothalamus (DMH) → sympathetic nervous system not inhibited → feeding inhibited
Arc-NPY inhibits Arc-POMC
Leptin
Helps the hypothalamus infer body weight.
Leptin is released by fat cells → more fat = more leptin
Cells in your anorexigenic centers have receptors for leptin → mutations in leptin receptors can cause obesity.
Leptin directly inhibits Arc-NPY and LH → feeding not activated. At the same time, directly excited PVN → sympathetic activity increased → feeding inhibited.
Leptin also directly excited Arc-POMC, PVN, and VMH → increased sympathetic activity → feeding inhibited. At the same time, directly inhibits DMH → sympathetic activity not inhibited → feeding not activated.
Can’t tell your brain when to stop eating though because its too slow
fed vs fasted
Increases in blood glucose
Eat → blood glucose increases → Arc-POMC excited, LH inhibited → further feeding inhibited
Sensors in the wall of the small intestine
Detect stretch and sugar and protein → release of cholecystokinin (CCK), peptide YY (PYY), and glucagon-like peptide 1 (GLP-1) → go through blood → excite Arc-POMC, PVN, and VMH and inhibit DMH
They also excite the vagus nerve, which excites VMH via the nucleus tractus solitarius, NTS
These hormones act in a fed state to inhibit feeding
But when you’re fasted, Ghrelin is released by the stomach wall → Arc-NPY and LH excited, PVN inhibited.
Release is stopped by stomach stretch
Circadian rhythm
Since the earth rotations cause changes in the environment (light during day, dark during night), we have evolved to have circadian rhythms (forage in the day, sleep at night).
These circadian rhythms are endrogenous
Continue even when the environment is constant
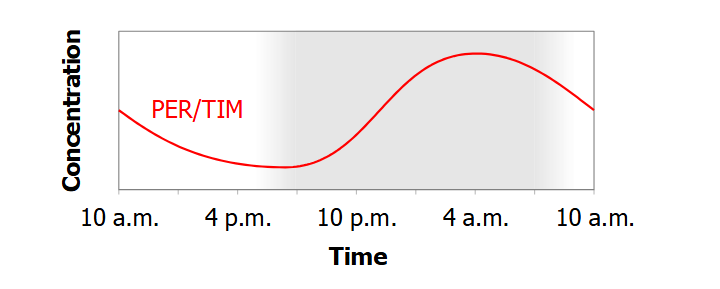
Genes involved in circadian rhythms in flies
per (period) on the X chromosome has a 24 hour cycle:
transcribed at night → per mRNA peaks at 10 pm → protein product PER peaks 6 hours later (4 am) → PER represses transcription of per
Together, per and PER form a transcription-translation feedback loop, or TTFL
tim (timeless) behaves similarly:
transcribed at night → TIM protein peaks later in the day → TIM + PER dimerize to form PER/TIM → represses transcription of both per and tim → at 4 am, per and tim mRNA expression low → no new PER/TIM made → PER/TIM levels drop → per and tim transcription no longer repressed → per and tim transcription restarts → cycle repeats.
if PER or TIM is absent → the TTFL is broken → no oscillation → no functional circadian rhythm.
how do PER/TIM work in flies
A gene called clk (clock) codes for CLK protein.
A gene called cyc (cycle) codes for CYC protein.
CYC and CLK form a dimer in the day called CLK-CYC → binds DNA and stimulates transcription of per and tim.
In the night, PER/TIM blocks CLK-CYC binding to DNA → represses transcription of per and tim.
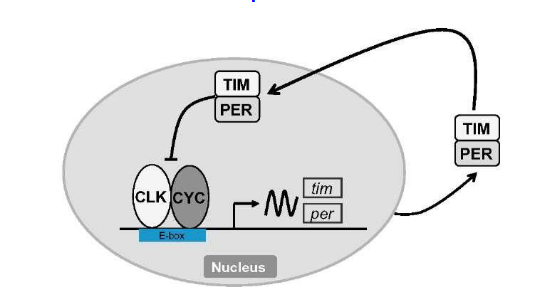
Why is the cycle not shorter than 24 hours in flies
Normally, translation and transcription are super fast and efficient so you would expect cycle to be very short.
BUT, protein called DBT binds to PER → breaks it down → PER levels rise slower → cycle 24 hours
human circadian rhythm
In humans, PER forms a dimer with CRY instead of TIM.
Also, mammalian homologs of clk, cyc, and dbt are called clk, bmal1, and ck1ε.
CLK/BMAL1 dimer stimulates transcription of per and cry when not blocked by PER/CRY.
CK1ε slows the rise of PER protein levels
synchrony of cellular clock
Kept in sync by cues called zeitgeber.
The main one is light sensed by melanopsin retinal ganglion cells → project onto the master clock which is the suprachiasmatic nucleus (SCN) of the hypothalamus
melanopsin ganglion signals → SCN neurons → neurons fire → clock reset through breakdown of PER/CRY
If the drop of PER/CRY happens after 4 am when the levels are already falling, the clock gets pushed forward (shorter than 24)
If the drop happens when the levels are rising, the clock is set back (longer than 24)
The SCN neurons that receive the signals forward the signals to other neurons in the SCN → pass to other parts of the brain → neural and hormonal signals sent to the whole body
Understand light vs dark.
Called entrainment
In the dark, SCN neurons project onto pineal body behind diencephalon → secretes melatonin
sleepiness
Depends on the master clock
In the daylight, SCN indirectly excites neurons in LH → orexin released → less tired.
Less orexin = more tired/narcolepsy.
In the darkness, LH cells project throughout the brain → MCH (melanin-concentrating hormone) is released → sleep is induced.
Orexin neurons and MCH neurons inhibit each other
Depends on sleep pressure
When awake, ATP is broken down → adenosine is built up → makes you tired.
When sleeping, ATP levels restored → adenosine falls → less tired.
Caffeine blocks adenosine receptors but does not lower adenosine levels, so when the caffeine wears off, we “crash”.
Stages of sleep
First theres 3 stages of non-REM (NREM) sleep
Dreamless with slower brain waves.
Stage 3 is deep NREM.
After NREM, there is REM sleep.
Have dreams, eyes move, high brain waves, muscle tone vanishes so you dont actually act out your dreams.
The first REM stage happens after 90 mins and as you continue to sleep, sleep becomes shallower and REM takes up more time.
Reflexes
Are innate, so genetically determined
You lose a lot of them as you age
A sensory stimulus in the CNS results in a response to perform a certain task.
has feedback loops to regulate things like force and position.
Can be monosynaptic
Stimulus → receptor → signal sent to sensory neuron → synapse into the spinal cord with no input from the brain → send to efferent neuron → target cell → response
Can be polysynaptic
Stimulus → receptor → sensory neuron → synapse to interneuron → synapse to spinal cord → efferent neuron → target cell → response
Stretch reflex
Stretch → Contract
Stimulus = Passive stretch of a muscle because of a load or contraction
Response = Active contraction of that muscle
Place load on hand → muscle spindles activated → motoneurons activated → contract the muscle that was stretched
Properties
Needed for stabilizing posture
Strongest in postural muscles
Faster in forearm muscles than ankles.
Spinal reflex
Supressed during movement
Golgi tendon reflex
Stretch → Relax
Stimulus = Active tension in the muscle
Response = Relaxation of the muscle
Unlike stretch reflex, this is polysynaptic
Golgi tendon organ (GTO) synapses onto interneurons → interneurons inhibit motoneurons of the muscle
Goal is to regulate amount of activity alongside the stretch reflex
If there is an excessive load → golgi tendon organ fires → interneurons activated → motoneurons inhibited → muscle relaxes → load dropped
Properties
Prevents movement
Stabilizes posture
Flexion withdrawal reflex
Touch hot stove → flex hand
Stimulus = Noxious injury of limb
Response = Flex joints that are proximal to the stimulus, extend joints distal to stimulus
Also multisynaptic
Nociceptors synapse onto interneurons
Pain receptors get activated in your forearm → proximal joint flexes, distal joint extends → arm is withdrawed.
Reciprocal inhibition
Activation of one motor nucleus inhibits an antagonistic motor nucleus.
Ex. if the flexor motoneurons are activated, antagonist extensors are inhibited.
But when you also need the antagonistic motor nucleus, the circuit can be suppressed.
Patellar Tendon Reflex
Bang knee → kick
When patellar tendon is tapped → quad is stretched → quad contracts
At the same time, the hamstring contractions are being inhibited to allow for movement.
If hamstring was not inhibited and also contracted, there would be no movement.
Cross extension reflex
Step on something sharp → flex leg → extend other leg.
nociceptors activated in one leg → flexor muscles same side as pain activated → leg withdraws. signal also travels contralaterally to the other side using commissural interneurons → extensor muscles activated → other leg stiffens for added support
Extensor thrust reflex
Stimulus = pressure on sole
Response = Activation of leg extensors
The mechanoreceptors project signal to intermediate zone interneurons → extensor motoneurons activated
Only active during stance.
This reflex is influenced by the corticospinal tract.
vestibulo-spinal reflex
Stimulus = downward deviation of head on one side → otolith afferents on
Response = downhill limbs extend
CPG
Central pattern generator.
Since reflexes can only help us perform simple movements, we need CPGs to program our posture and movement.
Mostly needed for locomotion, motor control, and behavioral responses
They are located in the spinal cord and in brainstem, and activated in order of relevance.
Leg step cycle
Walking involves a cycle of flexing and extending the legs.
Alternate between:
Swing phase = Toe off the ground, heel strikes the ground
Stance phase = Heel strikes ground, toe off ground
The cycle is programmed by the CPG in the intermediate zone of the lumbar spinal cord
Each leg has two burst generators within its CPG
Flexor Burst Generator (FBG): drives flexor motor neurons → leg swings
Extensor Burst Generator (EBG): drives extensor motor neurons → leg extends
FBG and EBG inhibit each other
Swing Phase
The swing phase is the flexion phase
Driven by the flexor burst generator (FBG)
FBG is connected to the flexor motor neurons in the ventral horn → Activate FBG → Activate the flexor motor neurons → Leg flexes → Leg can swing.
When the FBG is active, the EBG is inactive so you can be in the swing phase instead of the stance phase
The swing/flexion phase has a fixed duration regardless of speed.
When FBG is active, it builds up inhibition on itself → eventually, when the inhibition is strong enough, the FBG is forced to stop firing action potentials → Flexor motor neurons now inactive → extensor burst generator not inhibited → Can switch to stance phase
Stance phase
The stance phase is the extension phase.
Driven by the extensor burst generator.
EBG is connected to the extensor motor neurons in the ventral horn → Activate EBG → extensor motor neurons activated → Leg extends → leg is in stance
EBG inhibits FBG
This is where speed of walking is adjusted
The stance phase is regulated by the mechanoreceptors on the back of the foot.
They feed/send information to the nervous system to tell it that the foot has striked the ground and we are in the stance phase.
Allows your brain to time the swing phase.
The stance phase is made of reflexes as well.
Stretch reflex
Golgi tendon reflex
extensor thrust reflex.
Transition to swing phase
For the swing phase to start, there is criteria
Leg is not bearing weight
Hip is extended
Opposite leg is in stance (bearing weight)
The two legs can coordinate this through crossed projections to the CPGs on opposite sides.
arm swings
Coordinated by CPGs in the cervical cord.
Flexion phase synchronous with contra-lateral flexion in leg
Phase-linking via propriospinal tracts (from one segment of cord to another)
Posture
Organized in reticular formation of pons and medulla
Depends on:
Somatosensory system: Detects posture, pressure, and movement.
especially proprioception cuz that is awareness of your body parts in relation to each other.
Vestibular system: Detects your head position and acceleration
Visual system: slower system, but important vertical cues and motion cues
Red nucleus
contains Rubrospinal cells that activate localized synergies, especially in distal limbs and in the face (e.g. gripping and twisting movements of hands).
Unlike the reticulospinal and vestibulospinal tracts, the red nucleus is responsible for fine and specific limb control.
Synergy
group of muscles contracting together for a specific purpose
reticulospinal tract synergies are widespread to make support postures but rubrospinal synergies are more localized.
Motor cortex
Located in the precentral gyrus
Has somatotopic organization, meaning different parts are responsible for different body parts.
but the areas of the cortex do not correlate to the size of the parts they control.
Most of the axons that are descending from the axon to the spinal cord first pass through interneurons → allows for communication with motor neurons.
But some neurons of the motor cortex can communicate directly with the motor neurons without the interneurons.
distal limb muscles (fingers, hands)
speech muscles
Path:
Motor cortex commands go through brainstem → crosses the midline → goes through lateral white matter → activates motoneurons either directly or through interneurons
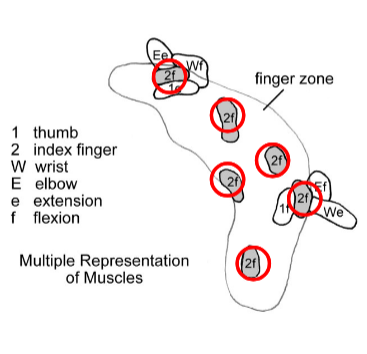
Multiple Representation
You can go to many different zones in the motor cortex and elicit the same movement
ex. finger flexion can be triggered from a bunch of different points in the finger zone.
These zones also have synergies.
A combination of different movements to make one thing like holding a pen.
Motor field
Set of motor nuclei that synapse onto one corticospinal axon (The axon that connects motor cortex to the spinal cord)
Happens across multiple spinal segments
Made of lots of synapses, and most are silent as in don’t contribute to activity.
Motor field has plasticity
Since its made of multiple motor nuclei, corticospinal axon has access to multiple parts of the body → can unsilence synapses to control a certain part of the body when it needs to.
Somatosensory Inputs
Input can only come from pathways with direct access to the motor cortex.
cutaneous (skin) input comes from somatosensory association areas → helps motor cortex know about posture + motion
Proprioceptive (joint) input direct from thalamus (and from somatic association cortex)
Premotor
The premotor areas are those that project onto the motor cortex but are also have routes to the motor nuclei
They go and put motor cortical synergies into the sequence needed for a specific movement.
The premotor cortex processes sensory inputs for cueing movement phases
especially visual and auditory,
the dorsal visual stream goes to the dorsal half on the cortex to tell it where the object is (spatial recognition)
the ventral visual stream goes to the ventral half to tell the cortex what something is
There is also broca’s area for sequencing language elements for speech or writing-typing
Sensorimotor Cues
Can be lots of different environmental cues
Sensory association areas recognize the cues and forward the signal to the frontal lobe
Premotor cortex selects appropriate response synergies in motor cortex
Visuomotor Response
A coordinated sets of activities and cues that want to initiate the synergies the premotor cortex selects.
Preparation of motor cortex
Premotor neurons set up the motor cortex by facilitating appropriate synergies → send a warning cue then a go cue
The premotor neurons not active during performance because they are preparing the motor cortex
Supplementary Motor Area
Located on the medial wall of hemisphere
Needed for a somatotopic representation of body, but less detail than motor cortex
Controls bilateral coordination of limbs when different motions done on each side
Processes internal ‘volitional’ signals that drive movements
voluntary signals
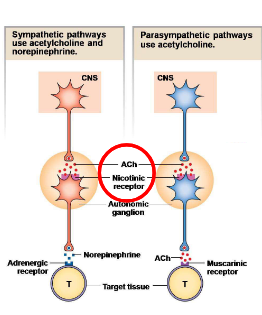
Neurons of the ANS
divided into its preganglionic and postganglionic components
The preganglionic neuron cell bodies of both the parasympathetic and sympathetic portions are in either the brainstem or spinal cord.
The preganglionic neurons project axons onto the postganglionic neurons.
The postganglionic neurons are in the autonomic ganglia between the CNS and target tissue
Autonomic ganglia allows for communication between the two ganglionic neuron types.
The post ganglionic neuron axons project onto target tissues.
This arrangement allows for one preganglionic neuron to synapse onto multiple postganglionic neurons
Called divergence
Preganglionic neuron in BS or SC → Postganglionic neuron in Autonomic ganglia → Target tissue
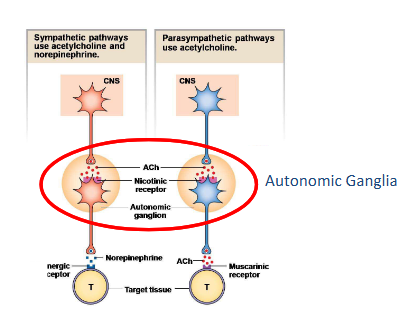
Communication between preganglionic and post ganglionic neurons of ANS
Preganglionic neuron in BS or SC → Secretes acetylcholine → binds to nicotinic receptors on the postganglionic neurons in the autonomic ganglia → postganglionic neurons in the sympathetic system secrete norepinephrine onto adrenergic receptors on the target tissue. Postganglionic neurons in the parasympathetic system secrete Ach onto muscarinic receptors on the target tissue.
Sympathetic autonomic communication
The preganglionic neurons are located in the thoracolumbar spinal cord.
Their nerve fibers/efferents/axons begin in the intermedio-lateral thoracic cord and synapse onto the autonomic ganglia parallel spinal cord.
Very short because they have to stay around the spinal cord
The autonomic ganglia are arranged in a sympathetic chain parallel to the spinal cord.
The preganglionic neurons secrete acetylcholine to the nicotinic receptors of the postganglionic neurons in the autonomic ganglia.
The postganglionic neurons are long as they have to go from the spinal cord to the target tissues.
The postganglionic neurons secrete norepinephrine to the adrenergic receptors of the target tissue.
Sympathetic activities
Fight-or-flight response
Prepare for emergency, stress, and exercise
Increase heart rate and blood pressure
Mobilize energy stores
Pupillary dilation
Diffuse effect due to its widespread and interconnected innervations
Decrease gastrointestinal and urinary functions
Releases epinephrine
Adrenal medulla
Activation of the sympathetic system signals release of epinephrine from the adrenal medulla.
Preganglionic neurons in SC → Postganglionic neurons in adrenal medulla → have no axons to project onto target cells → instead secrete epinephrine
These axon-less cells are called chromaffin.
Prolonged response since hormonal.
Parasympathetic autonomic communication
The preganglionic neurons are located in the sacral spinal cord or the brain stem.
Their nerve fibers/efferents/axons start in the multiple cranial motor nuclei and the intermedio-lateral part of the sacral cord and synapse onto the autonomic ganglia embedded in the target tissue.
Are very long because they have to go from the brainstem or spinal cord all the way to the target tissue.
The preganglionic neurons secrete acetylcholine to the nicotinic receptors of the postganglionic neurons in the autonomic ganglia.
The postganglionic neuron has short nerve fibers as they are already at the target tissue.
The postganglionic neuron releases acetylcholine to the muscarinic receptors of the target tissue
Parasympathetic activity
Quiet, relaxed states
Active in “rest and digest”
Increase gastrointestinal activities
Decrease heart rate and blood pressure
Duel innervation
Organs in the body have both sympathetic and parasympathetic activity → the two branches have opposing effects.
Both are active at rest but parasympathetic dominates
Primary function is to regulate organs to maintain homeostasis.
Sympathetic: cardiac output increased, skin vasoconstriction, sweating, piloerection, blood diverted from gut and skin to muscle
Parasympathetic: digestion promoted, cardiac output reduced, slow breathing, urination
Complementary, not antagonistic.
Targets of autonomic neurons
smooth muscles, cardiac muscles, glands.
The synapse between the post ganglionic autonomic neurons with its target cells = neuroeffector junction
Not neuron to neuron
The postganglionic neurons don’t have an axon terminal, they have Varicosities
These are axon swellings that contain the neurotransmitters.
Released in response to an action potential.
Sympathetic pathway:
Action potential to varicosity → voltage gated ca channels open → ca influx triggers NE release → NE binds to an adrenergic receptor on the target tissue → target tissue response. NE can reuptake or recycle → metabolized by MAO
Autonomic reflexes
produced by the autonomic efferent networks but can be modulated
Act as a negative feedback loop
Want to maintain homeostasis
Pupillary Light Reflex
Baroreflex
Pupillary Light Reflex
in pretectal area of midbrain
Uses ON and OFF afferents to luminance and darkness detectors.
Too bright → On afferents detect luminance → parasympathetic reflex activated via 3rd cranial nerve → ciliary ganglion → circular iris muscles → constrict pupil
Too dark → off afferent detect darkness→ sympathetic reflex via thoracic cord → sympathetic chain to radial muscles → dilate
Baroreflex
When BP or HR too high:
NTS receives input from the baroreceptors → NTS sends information to the caudal VLM → caudal half inhibits the rostral half that is responsible for blood pressure→ reduces blood pressure or heart rate
Low BP:
Want to turn on the rostral VLM thru less activation of the caudal half.
Autonomic Control Centers
The ANS works with endocrine and behavioural system to maintain
homeostasis
The autonomic reflexes are integrated in the brain (thalamus, hypothalamus, and brainstem) → these centers regulate heart rate, blood pressure, etc to maintain homeostasis.
the Brainstem Autonomic Centers (hypothalamus, pons, medulla) use the feedback of the sensory system to regulate other functions.
The brainstem itself contains control centers Cardiovascular center, and respiratory pattern generator in lateral medulla/pons
Relays the information it receives to muscles and glands.
Also uses the PAG, the center for autonomic behavioural programs
PAG
The PAG found in midbrain and functions as the coordinator of
autonomic behaviours
Has columns for behaviour patterns.
Ex. fight: PAG projects to cardiovascular center to increase BP and also the respiratory center to increase breathing rate and causes release of serotonin to activate motor neurons and also inhibits pain
Works with the hypothalamus and acts through the hypothalamus and the reticular formation.
Reticular Activating Systems
Works through a diffuse modulatory system that causes a global shift in the CNS so everything everywhere on
Cholinergic: determines level of attention, and sleep-wake cycle; mainly ascending (ACh)
Serotonergic: for stressful situations; influences mood, sleep-wake cycle (Serotonin)
Adrenergic: for stressful situations, vigilance (Norepinephrine NE)
Dopaminergic: reward center (Dopamine)
Histaminergic: sleep wake control, supports the waking state (Histamine)
Skeletal muscles
Only muscle type that is under conscious voluntary control.
Needs to be activated by the somatic nervous system.
Activation of the skeletal muscles by the central nervous system needs to happen through motor neurons.
The motor neuron and its fibers together are called a motor unit.
The motor neurons and the skeletal muscles synapse and communicate with each other at the Neuro-Muscular Junction (NMJ)
The contractile filaments of the skeletal muscles are called sarcomeres
Made of actin and myosin
Organized in an overlapping arrangement called striated.
Skeletal muscles have the best sarcoplasmic reticulum of all muscle types
An intracellular organelle that stores calcium
Skeletal muscle fibers
Made of myofibrils.
Thin filaments made of actin
Has a binding site for myosin
Myosin binding site is covered by tropomyosin when there is no calcium/muscle is relaxed.
When there is calcium or muscle is contracting, the Ca binds to a troponin complex → movement of tropomyosin → myosin binding site exposed → myosin can bind → muscle can contract
Thick filaments made of myosin → has lots of crossbridge → can connect actin and do muscular contractions.
Myosin head has the actin binding site and an ATP binding site for energy
Goes from tendon to tendon
its plasma membrane is called the sarcolemma
Invagination of the sarcolemma into the muscle fiber is called the T tubule system → allows for spread of AP into the muscle fiber
During a muscle contraction, the sarcomere shortens but the filament lengths dont change.
Muscle fiber types
Slow twitch oxidative fibers
Contract slowly
Have lots of mitochondria
Depend on oxidative metabolism → Small force but low fatigue
Innervated by small diameter motor neurons
Fast twitch glycolytic fibers
Fast twitch time
Lots of tension
Low mitochondria → depend on glycolytic metabolism → Fatigue fast due to lactic acid accumulation
Innervated by large diameter motor neurons.
Fast twitch oxidative glycolytic fibers
In between the two
Motor unit
All the fibers in one unit contract together.
The smoothness and movement of the contractions depends on the number and timing of motor units active.
Small motor units are more easily excited than big ones → contractions begin with the small units
All the fibers in one unit are the same → there are 3 types of fibers → there are 3 types of units
Slow twitch
Fast twitch
In between
Neuro-Muscular Junction (NMJ) properties
Its axon terminals are called terminal bouton and opposite the terminals are the membrane called the motor end plate
Terminal bouton receives the action potential while the motor end plate causes depolarization in the muscle itself.
Communication happens here
In the peripheral tissues and muscles, there is no BBB so there is no protection from toxins.
Nicotinic receptor blockers: Makes it hard to generate an action potential in the muscle fibers.
A poison dart form is called curare.
Can be used as a muscle relaxant.
Blocks reflexes
Exocytosis blocker: No ACh release
Botox does this
Ach-esterase inhibition: ACh not broken down → depolarization continues → paralysis
Skeletal Muscle contraction
Starts with excitation contraction coupling of skeletal muscle
Command sent to motor neurons → action potential started → goes to terminal bouton of NMJ → voltage gated Ca channels open → Ca influx → ACh release is triggered → binds to nicotinic recepotrs at the motor end plate of NMJ → Na and K Channels opened → depolarization of skeletal muscle → action potential started in skeletal muscle → AP travels deep into the muscle through T tubules → DHP receptor changes conformation → Change causes RyR in the sarcoplasmic reticulum to open → Ca release into cytoplasm → Ca binds to troponin → tropomyosin moves from myosin binding site of actin.
Moves on to generation of force
When there is high energy, myosin has a high affinity for actin.
Myosin binds to actin’s binding site → starts a power stroke where it pulls the thin filaments to the center of the muscle → force is generated → ADP is released from myosin → ATP binds to myosin → Myosin hydrolyzes ATP → its head rotates → actin now bound weakly → if no calcium bound anymore, tropomyosin moves back to cover the myosin binding site → contraction ends.
Muscle twitch
A single contraction-relaxation cycle.
3 phases
Latent period
Excitation contraction coupling
Period of contraction
High intracellular Ca
Cross bridge cycle
Period of relaxation
Low intracellular Ca
tension goes down to 0
Summation of force
More action potentials → increased tension through summation
Successive twitches fuse together and the contractile force increases
Eventually, the contractions fuse into one contraction called tetanus
When your muscles fatigue, the tension will rapidly drop
Smooth muscle
Found in the internal organs and blood vessels.
Controlled by the ANS, not voluntary control.
Actin and myosin not organized parallel, diamond shaped instead.
Actin and myosin are longer than in the skeletal muscle → allows them to have a longer range of contraction → Can operate on a range of lengths
Also contracts more slowly
Classified by either location or communication with neighbouring cells.
Single unit or multi unit
Single unit smooth muscle
Found in the intestinal tract and blood vessels
Have spontaneous activity
Contracts when stretched
Can exert tension even without stimulation
Some processes need tension to work even with no stimulation.
Multi unit smooth muscles
Found in airways or arteries
Each fiber acts individually
Heavily innervated and contracts with stimulation only.
Excitation contraction coupling of smooth muscle
Ca is from both the sarcoplasmic reticulum and the ECF → slower contraction.
Slower relaxation time cuz of slower removal of calcium.
Opening of calcium channels → Influx of Ca → More calcium release is triggered → Ca binds to calmodulin → calmodulin activates MLK (a kinase) → phosphorylates myosin → cross bridge cycling can occur
To stop the cycle, phosphatases are also needed on top of the calcium ATPases.
Removes phosphate from myosin
Cardiac muscles
Has contractile and conductile cells.
Conductile cells are responsible for conducting the excitation between atria and ventricles
Certain heart cells can to automaticity
Pacemaker cells
Striated and has a SR like the skeletal muscles
Its gap junctions allow excitation to spread, allowing a synchronous heart beat.
Modulated by ANS
Cardiac muscle AP
During an AP in cardiac muscles, Ca channels and Na channels open
Ca channels open slower and stay open longer → Ca can enter from ECF
The AP lasts as long as contraction and relaxation
C
Cardiac muscle contraction
Recruitment of more cells or frequency doesn’t increase force, but muscle length does.
More blood volume → More contraction force because of more overlap of myosin and actin
Excitation contraction coupling of cardiac muscle
Ca released from ECF and SR
Done by contractile proteins
To relax, Ca needs to be removed by Ca pump
Unlike the rest, there is a Na/Ca membrane exchange that removes Ca from the cytosol.
Digitalis increases force of contractions by inhibiting Na/K ATPase → increased intracellular Na → Na/Ca membrane exchange has decreased Na influx and decreased Ca efflux → Increased intracellular Ca → Increased contraction strength.