(17.3) RBCs
1/41
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
42 Terms
List the Composition of Formed Elements
RBCs
WBCs
Platelets
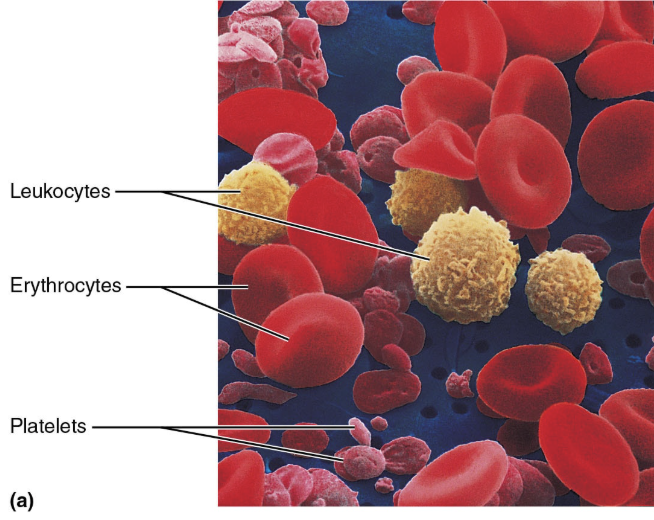
Describe the Formed Elements
Only WBCs are complete cells
Most formed elements survive in bloodstream “only few days”
Most blood cells originate in bone marrow and do not divide
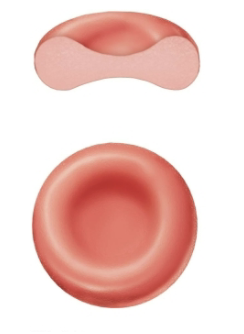
Describe the Structure of Erythrocytes
Small-diameter (7.5 um) cells that contribute to gas transport
Filled with hemoglobin (Hb) for gas transport
What is a hematocrit?
A hematocrit is the percentage of erythrocytes in a whole blood sample
45% of whole blood (Hct)
How to calculate Hematocrit
HCT (%) = (RBCs/Whole Blood) x 100
40–54% for men and 36–48% for women
Explain how RBCs an superb example of Complementarity of Structure and Function
Three features make for efficient gas transport:
Biconcave shape → offers huge surface area relative to volume for gas exchange
Hemoglobin → makes up 97% of cell volume (not counting water), the molecule that binds to and transport respiratory gases
RBCs have no mitochondria → ATP production is anaerobic, so they do not consume O2 they transport
Flexible proteins → allow the cell to bend, twist, and cup, but which will return it to its normal shape
RBCs Function
Erythrocytes are completely dedicated to their job of transporting respiratory gases (oxygen and carbon dioxide)
O2 loading in lungs → Produces oxyhemoglobin (ruby red)
O2 unloading in tissues → Produces deoxyhemoglobin, or reduced hemoglobin (dark red)
CO2 loading in tissues → 20% of CO2 in blood binds to Hb, producing carbaminohemoglobin
What is the name of the protein found in erythrocytes that transports respiratory gases and provides the red color?
Hemoglobin
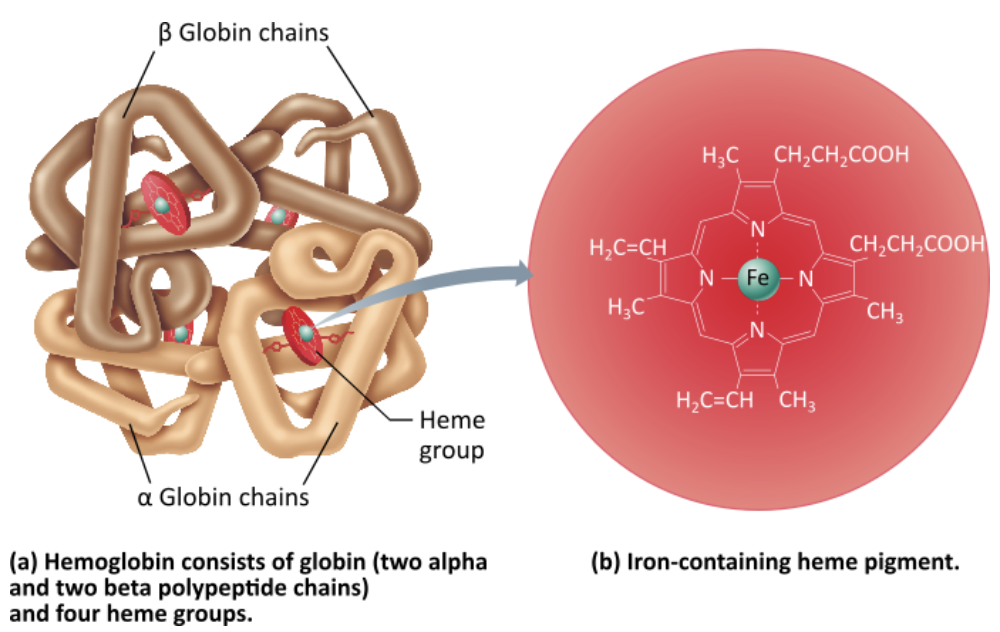
Describe the structure and function of Hemoglobin
LOCATION
An iron-containing protein located within red blood cells
STRUCTURE
Consists of globin (two alpha and two beta polypeptide chains) and four heme groups
Iron-containing heme-pigment
FUNCTION
Hemoglobin molecule can transport four molecules of oxygen because each iron atom can combine reversibly with one molecule of oxygen
Each RBC contain 250 million Hb molecules
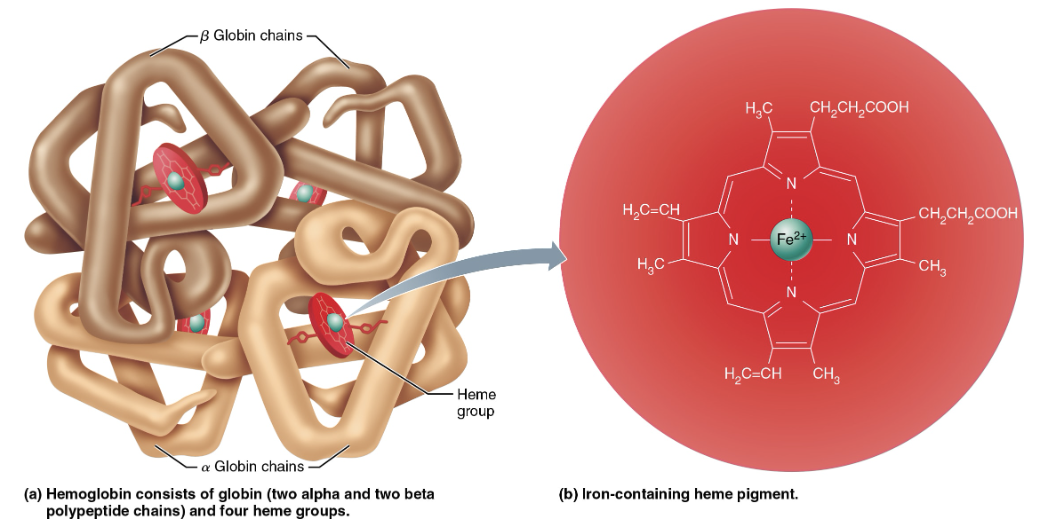
What is the complete hemoglobin molecule composed of?
Four globin polypeptides (2 alpha chains, 2 beta chains)
Four heme groups
Four Fe2+ ions
O2 vs CO2 binding to Hemogolbin
O₂→ binds to the heme group in hemoglobin (Hb)
4 oxygen molecules can be transported by one Hb molecule
CO₂ → binds to the amino groups on the hemoglobin protein chains
4 carbon dixoide molecules can be transported by one Hb molecule
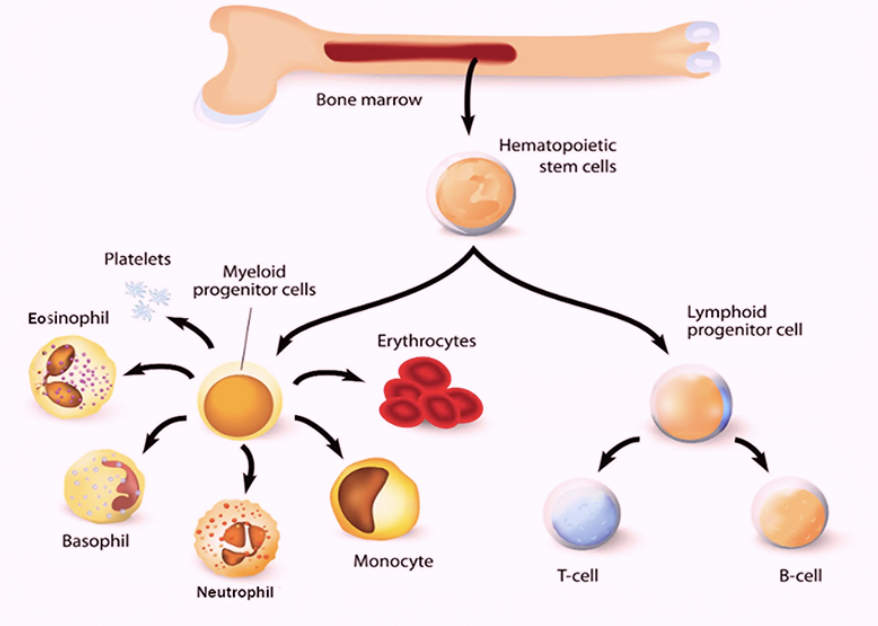
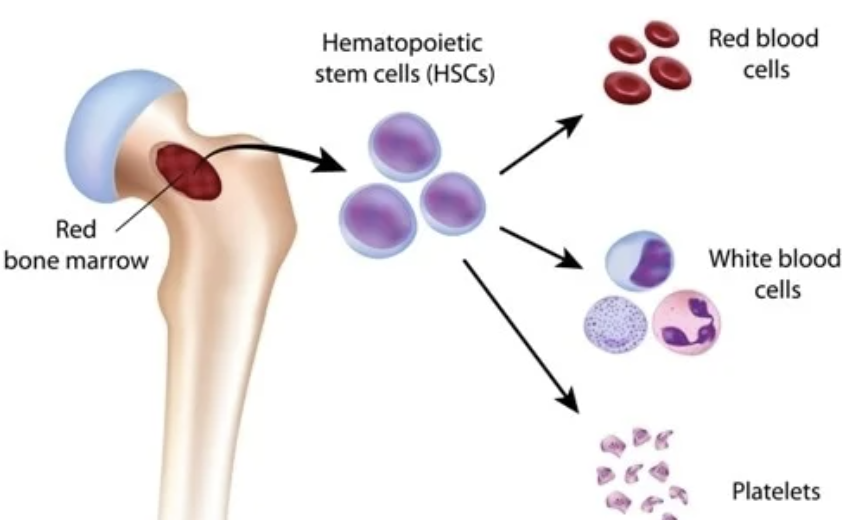
RBCs Production
Hematopoiesis → formation of all blood cells
Occur in red bone marrow
In adult, found in axial skeleton, girdles, and proximal epiphyses of humerus and femur
Hematopoietic stem cells (hemocytoblasts)
Stem cell that gives rise to all formed elements
Hormones and growth factors push cell toward specific pathway of blood cell development
Committed cells cannot change
Explain how Erythropoiesis occurs
Hematopoietic stem cells (hemocytoblasts) → Stem cell that gives rise to all formed elements
Hormones and growth factors push cell toward specific pathway of blood cell development
Committed cells cannot change
Erythropoietin (EPO) → Hormone that stimulates formation of RBCS
Always small amount of EPO in blood to maintain basal rate
Released by kidneys (some from liver) in response to hypoxia
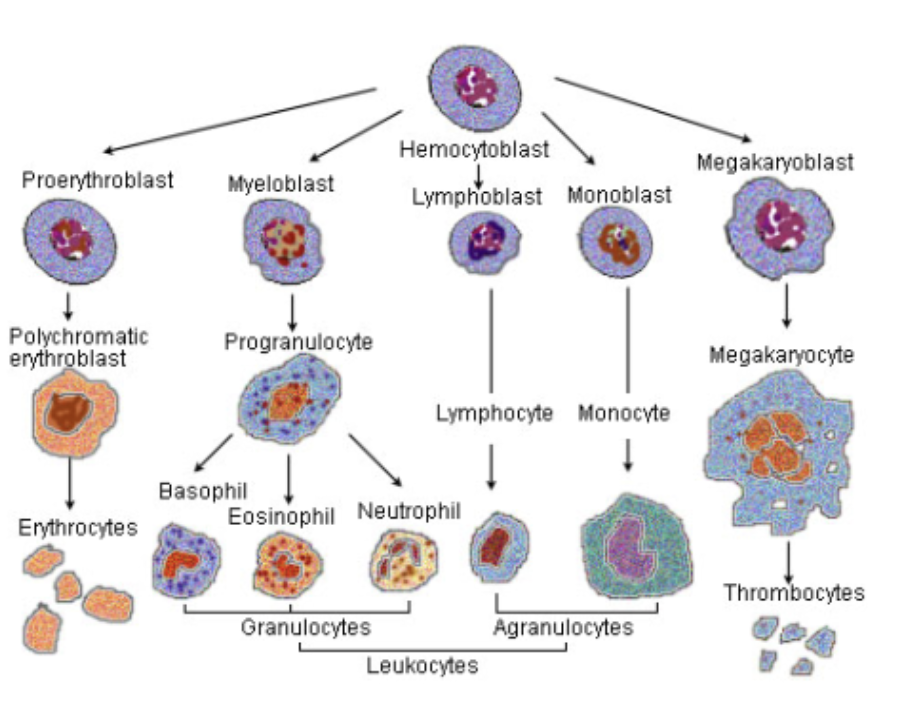
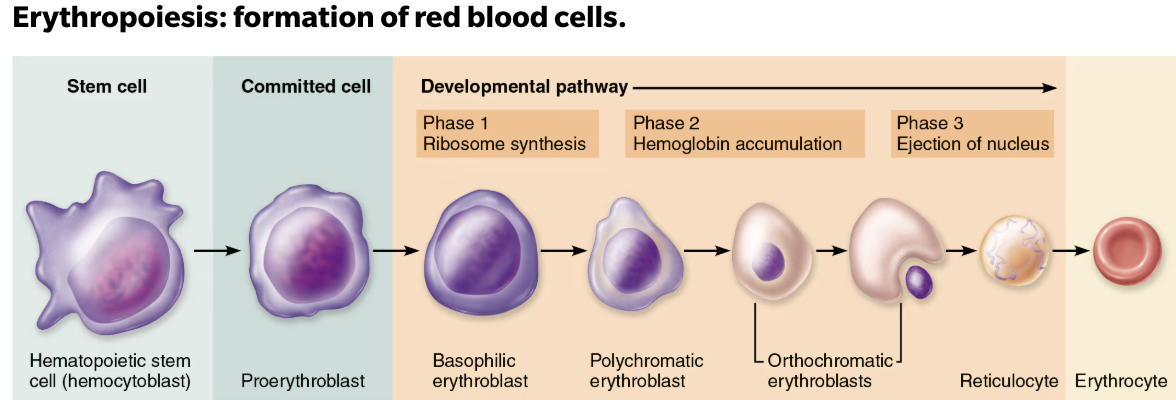
Stages of Erythropoiesis
Erythropoiesis → process of formation of RBS that takes about 15 days
Hematopoietic stem cell
Bone marrow cell that gives rise to all the formed elements of blood; hemocytoblas
Myeloid stem cell
A stem cell that gives rise to erythrocytes, platelets, and a few types of leukocytes
Proerythroblast
A committed cell that gives rise to a basophilic erythroblast in the process of erythropoiesis
Basophilic erythroblasts
A cell in the developmental pathway of erythropoiesis that contains large numbers of ribosomes and transforms into a polychromatic erythroblast
Polychromatic erythroblasts
A cell in the developmental pathway of erythropoiesis that synthesizes hemoglobin, accumulates iron, and transforms into an orthochromatic erythroblast.
Orthochromatic erythroblasts
A cell in the developmental pathway of erythropoiesis that ejects most of its organelles and loses its nucleus as it becomes a reticulocyte.
Reticulocyte
Young erythrocyte, still contains a bit of reticulum
Erythrocyte
Causes and Effect of too few RBCs
Hypoxia
Too few RBCs
SYMPTOMS:
Cyanosis
Difficulty breathing
Tachycardia
Unconsciousness
Causes and Effect of too high RBCs
Increased blood viscosity
Too many RBCs
Balance between RBC production and destruction depends on:
Hormonal controls
Erythropoietin (EPO)
Dietary requirements
Nutrients
Two B-complex vitamins
Iron
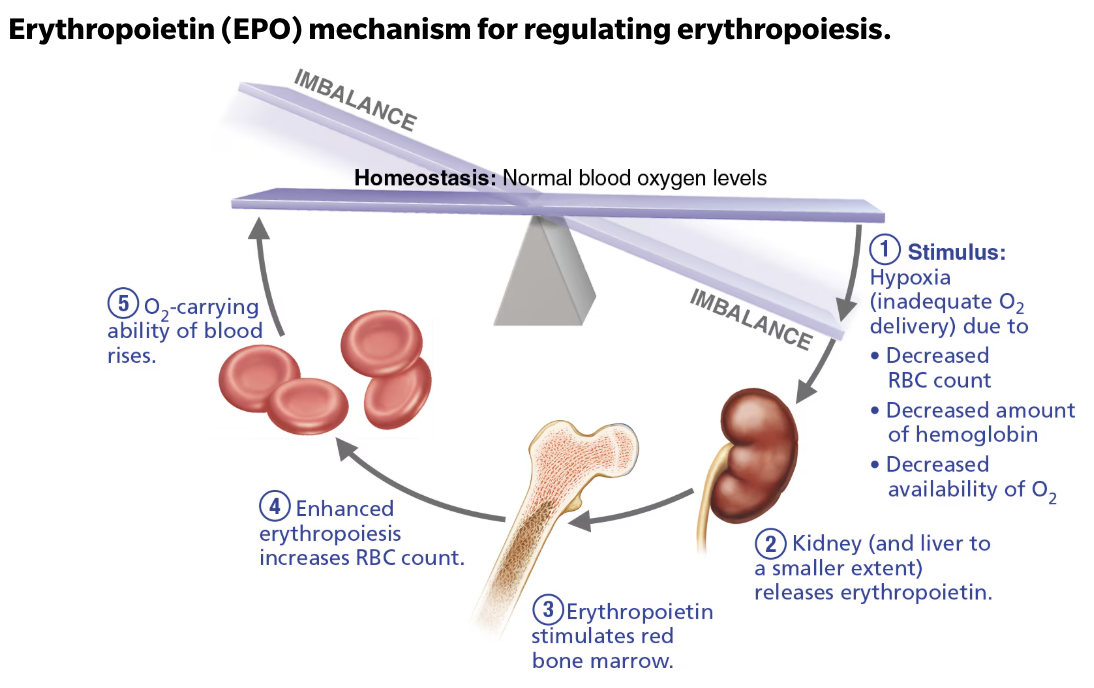
Explain Regulation of Release of RBCs
STIMULATED by Erythropoietin (EPO) in response to
Hypoxia → inadequate O2 delivery due to:
Decreased RBC count
Decreased amount of hemoglobin
Decreased availability of O2
INHIBITED by
Too many erythrocytes
High O2
Role of Erythropoietin (EPO)
Erythropoietin (EPO) → Hormone that stimulates red bone marrow for the formation of RBCS
Always small amount of EPO in blood to maintain basal rate
Released by kidneys (some from liver) in response to hypoxia
EPO causes erythrocytes to mature faster
Testosterone enhances EPO production, resulting in higher RBC count
Erythropoietin (EPO) mechanism for regulating erythropoiesis
STIMULI: Hypoxia (inadequate O2 delivery due to)
Decreased RBC count
Decreased amount of hemoglobin
Decreased availability of O2
Kidney (and liver to a smaller extent) releases Erythropoietin
Erythropoietinstimulates red bone marrowEnhanced erythropoiesis increases RBC count
O2-carring ability of blood rises
Explain Artificial EPO and its Effects
Use of EPO increases hematocrit → which allows athlete to increase stamina and performance
CONSEQUENCE → EPO can increase hematocrit from 45% up to even 65% with dehydration concentrating blood even more
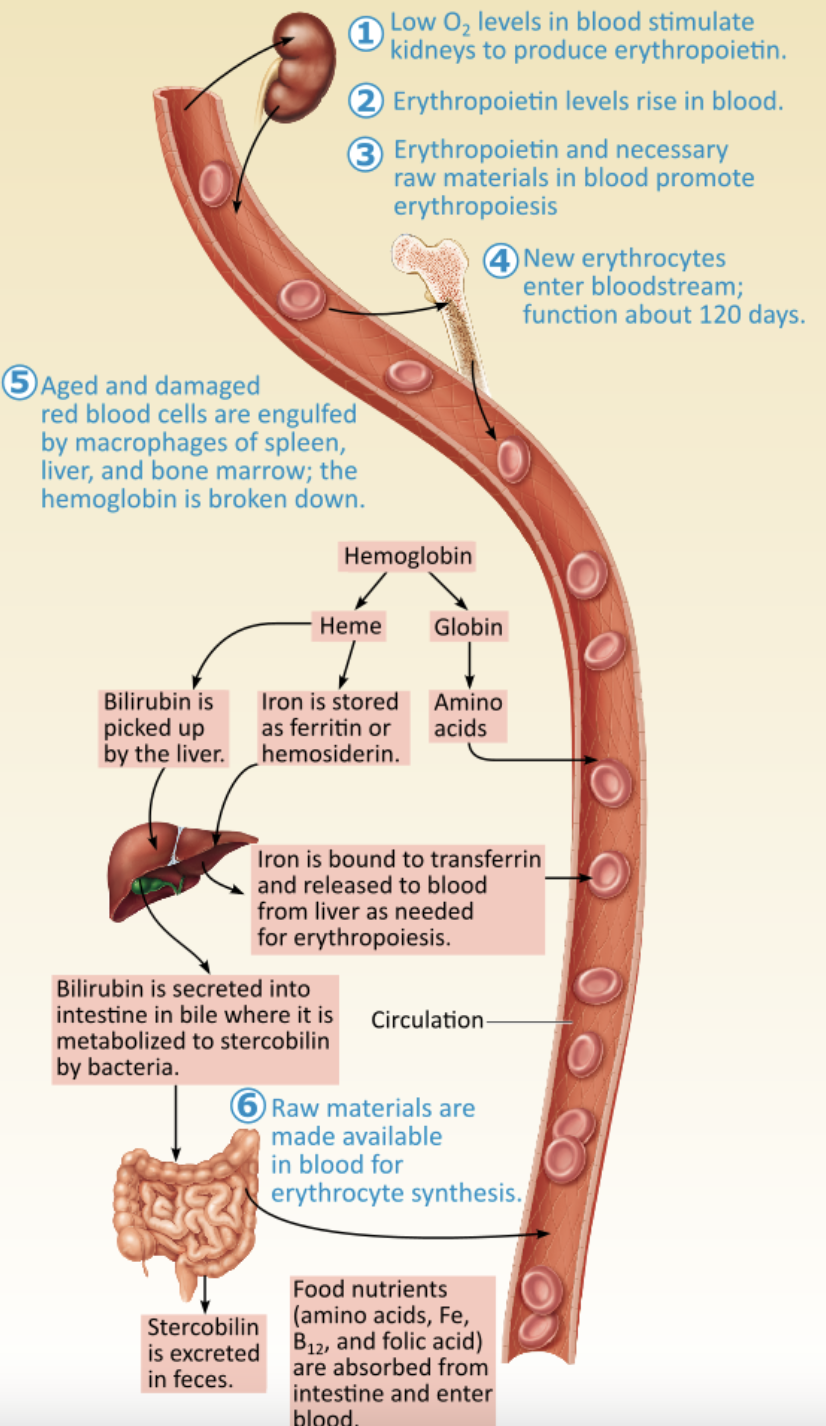
List and Explain Dietary Requirements for Erythropoiesis
Nutrients
Amino acids, lipids, and carbohydrates
Iron
65% of iron is found in hemoglobin, which rest in liver, spleen, and bone marrow
Free iron ions are toxic so iron is bound with proteins:
Stored in cells as ferritin and hemosiderin
Transported in blood bound to protein transferrin
Two B-complex vitamins
Vitamin B12 and folic acid are necessary for DNA synthesis for rapidly dividing cells such as developing RBCs
Explain RBCs Destruction
Life span 100-120 days
Old RBCs become fragile, and Hb begins to degenerate
Macrophages in spleen engulf and breakdown dying RBCs
Explain RBC breakdown
RBC breakdown → heme, iron, and globin are separated
Hemoglobin
Heme → Molecule, containing iron
Iron removed and recycle, stored as ferritn or hemosiderin
Bilirubin Formation
Globin → Protein component
Broken down into amino acids, which are recycled for the synthesis of new proteins, including new red blood cells
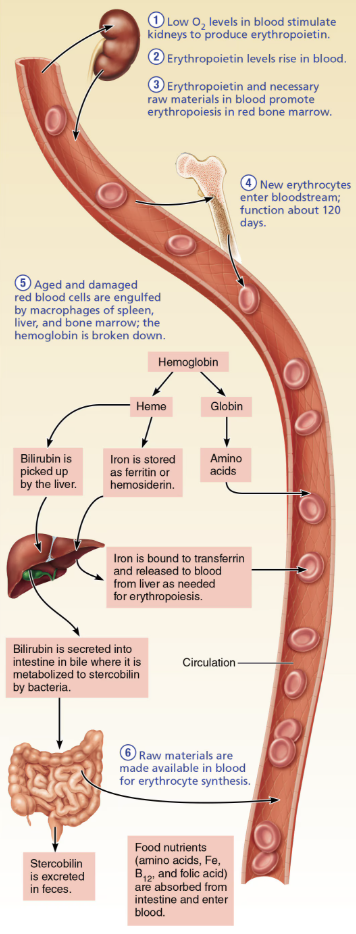
Explain Steps of Bilirubin Formation
Heme group has its iron removed and recycled, while the remainder is converted to bilirubin
Heme group is degraded to
bilirubin(a yellow pigment) that is released to the bloodBinds to albumin for transport
Bilirubin is picked u by the liver
Bilirubin is secreted into intestine in bile where it is metabolized to stercobin by bacteria
Stercoblin is exreted in feces
Explain causes and effects of Jaundice
Hyperbilirubinemia
A yellow discoloration of the body tissue resulting from the accumulation of excess bilirubin
CAUSES
Liver damage
Hemolytic anemia → Too many RBCs destoryed
Classification of Erythrocyte Disorders
Anemia
Polycythemia
Describe Anemia
Blood has abnormally low O2-carrying capacity that is too low to support normal metabolism
Sign of problem rather than disease itself
SYMPTOMS:
Shivering
Difficulty breathing
Lethargy
List the causes of Anemia
Blood loss
Hemorrhagic anemia
Not enough RBCs produced
Iron-deficiency anemia
Too many RBCs being destroyed
Describe the causes and treatment of Acute Hemorrhagic Anemia vs Chronic Hemorrhagic Anemia
Blood loss
Acute Hemorrhagic Anemia
CAUSE → Blood loss is rapid (as might follow a severe stab wound)
TREATMENT → Replacing the lost blood
Chronic Hemorrhagic Anemia
CAUSE → Slight but persistent blood loss (due to hemorrhoids or an undiagnosed bleeding ulcer)
TREATMENT → Once the primary problem is resolved, normal erythropoietic mechanisms replace the lost blood cells

Describe the causes and treatment of Iron-deficiency anemia
Not enough RBCs produced
CAUSE → Not enough RBCs being produced, can be caused by hemorrhagic anemia, but also by low iron intake or impaired absorption
RBCs produced are called microcytes → small and pale because they cannot synthesize their normal complement of hemoglobin
TREATMENT → increase iron intake in diet (for example, red meat, beans, and spinach) or through iron supplements
Describe the causes and treatment of Pernicious anemia
Not enough RBCs produced
CAUSE → Autoimmune disease that destroys stomach mucosa that produces intrinsic factor
Intrinsic factor needed to absorb B12
B12 is needed to help developing RBCs divide
Without B12 developing RBCs enlarge but cannot divide, resulting in large macrocytes
TREATMENT → regular intramuscular injections of vitamin B12 or application of a B12-containing gel to the nasal lining once a week
Microcytes vs Macrocytes
Microcytes:
RBCs produced under Iron-deficiency anemia conditions
Small and pale because they cannot synthesize their normal complement of hemoglobin
Macrocytes:
RBCs produced under Pernicious anemia conditions
Developing RBCs enlarge but cannot divide, resulting in large cells
Describe the causes and treatment of Renal anemia
Not enough RBCs produced
CAUSE → lack of EPO
Often accompanies renal disease
Kidneys cannot produce enough EPO
TREATMENT → Synthetic EPO
Describe the causes and treatment of Aplastic anemia
Not enough RBCs produced
CAUSE → Destruction or inhibition of bone marrow (drugs, chemicals, radiation or viruses)
Usually cause is unknown
All formed element cell lines are affected → results in anemia and clotting & immunity defects
TREATMENT → short term with transfusion, long term with transplanted stem cells
Describe the causes Hemolytic anemia
Too many RBCs being destroyed
Premature lysis of RBCs
CAUSES:
Incompatible transfusions or infections
Hemoglobin abnormalities → usually genetic disorders resulting in abnormal goblin (Sickle-cell anemia)
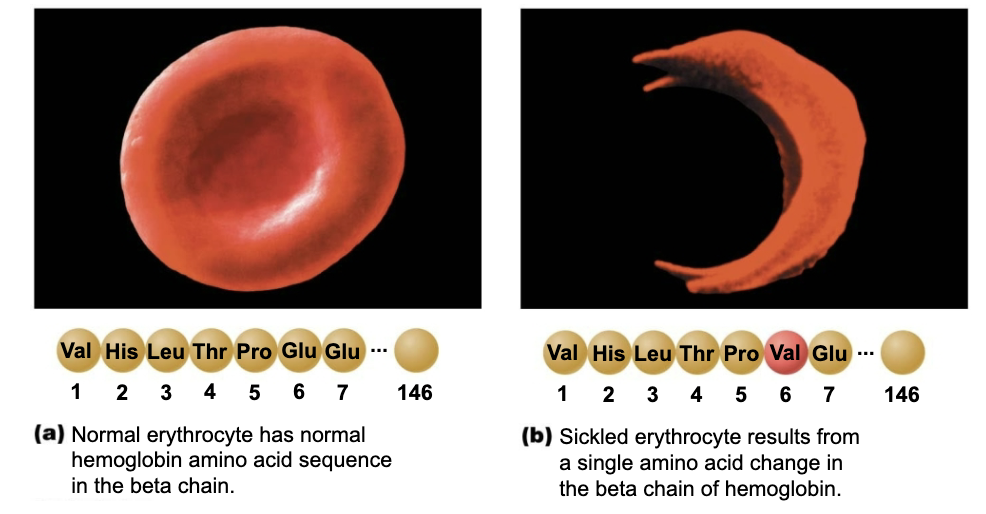
Describe the causes and treatment of Sickle-cell Anemia
Too many RBCs being destroyed
CAUSE → Misshaped RBCs rupture easily and block small vessels
Hemoglobin S (HbS), results from a change in just one of the 146 amino acids in a beta chain of the globin molecule
Results in poor O2 delivery and pain
Prevalent in African-Americans of the African malarial belt and their descendants
Possible benefit → people with sickle cell do not contract malerai
Kills 1 million/year
TREATMENT → acute crisis treated with transfusion
Describe Polycythemia
Abnormal excess of RBC
SYMPTOMS:
Increases blood viscosity → sluggish blood flow
Describe the causes and treatment of Polycythemia vera
CAUSE → Bone marrow cancer leading to excess RBC
Hematocrit may as high as 80%
TREATMENT → therapeutic phlebotomy
Describe the causes Secondary Polycythemia
CAUSE → low O2 levels (high altitude) or increased EPO production
Explain Blood doping
Polycythemia
Athletes remove, store, and reinfuse RBCs before an event to increase O2 levels for stamina
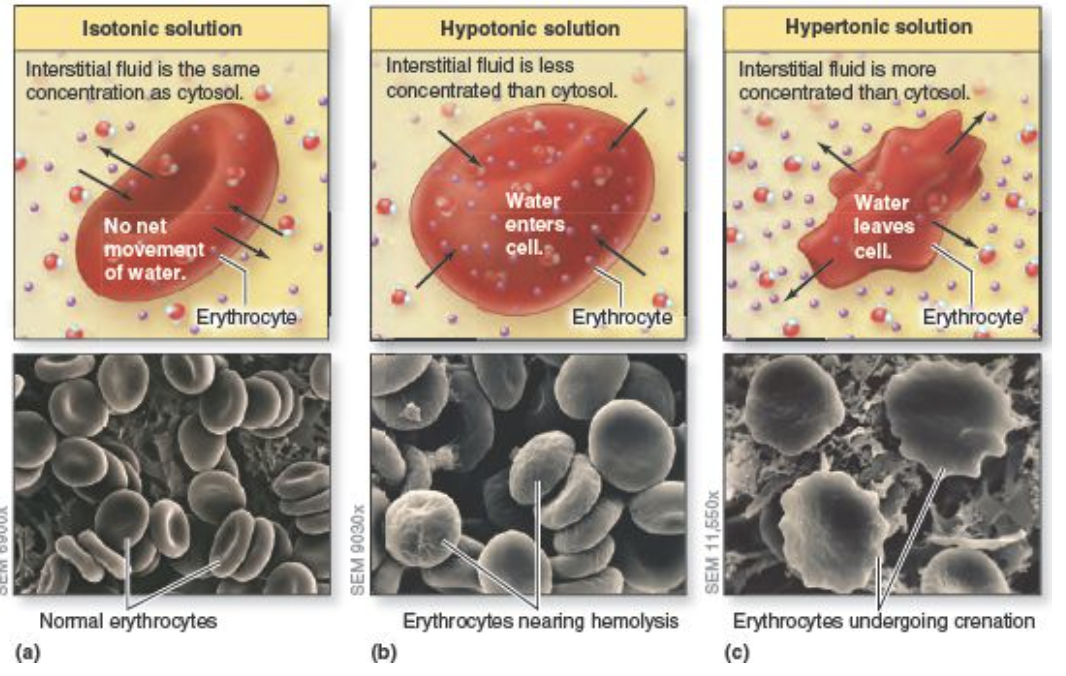
Describe how changing tonicity leads to changes in RBC shape