CMM MUSCULAR CONTRACTIONS
1/109
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
110 Terms
How does the size of a motor unit affect muscle control?
Smaller motor units allow for finer control of movements, while larger motor units result in less precise control.
What are the connective tissue layers associated with muscle fibers?
Endomysium | Individual muscle fibers | “Endo” = Inside/Innermost |
Perimysium | Bundles (fascicles) | “Peri” = Around/Perimeter |
Epimysium | Entire muscle | “Epi” = Outer layer, like “epidermis |
What is the function of the endomysium?
The endomysium surrounds individual muscle fibers and provides structural support.
What is the role of the perimysium?
The perimysium surrounds bundles of muscle fibers called fascicles.
What does the epimysium do?
The epimysium is a protective layer that surrounds the entire muscle tissue.
What are the two main types of muscle fibers?
The two main types of muscle fibers are striated (skeletal and cardiac) and non-striated (smooth).
What is the significance of striated muscle fibers?
Striated muscle fibers have contractile proteins arranged in parallel bundles, allowing for uniform contraction.
What is the structure of skeletal muscle fibers?
Skeletal muscle fibers are long, multinucleated, and span from tendon to tendon.
What are myofilaments?
Myofilaments are contractile proteins within muscle fibers, primarily actin (thin filament) and myosin (thick filament).
What is the role of the sarcolemma?
The sarcolemma is the plasma membrane surrounding a muscle fiber.
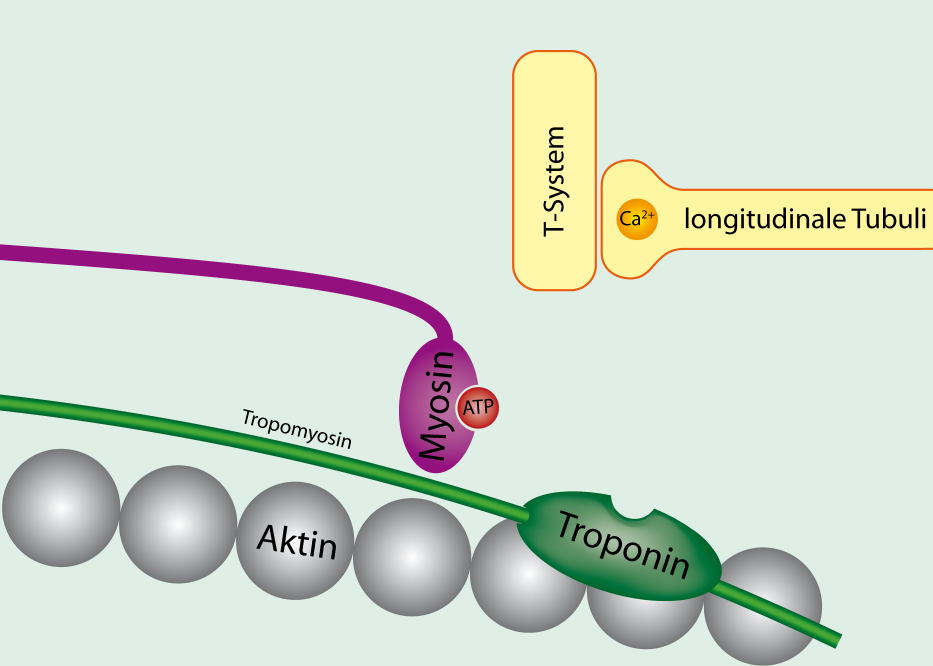
What are T-tubules?
T-tubules are invaginations of the sarcolemma that help transmit action potentials into the muscle fiber.
What is the function of the sarcoplasmic reticulum?
The sarcoplasmic reticulum stores calcium ions and releases them during muscle contraction.
What is a sarcomere?
A sarcomere is the functional unit of muscle fibers, responsible for muscle contraction.
What is the sliding filament theory?
The sliding filament theory explains muscle contraction as the interaction between actin and myosin filaments, causing them to slide past each other.
What initiates muscle contraction?
Muscle contraction is initiated by the release of calcium ions from the sarcoplasmic reticulum in response to an action potential.
What is the role of titin in muscle fibers?
Titin is a spring-like protein that helps stabilize the structure of myosin and contributes to muscle elasticity.
What happens during muscle contraction?
During contraction, the sarcomere shortens as actin and myosin filaments slide over each other.
What is the difference between skeletal and smooth muscle?
Skeletal muscle is striated and under voluntary control, while smooth muscle is non-striated and involuntary.
How do muscle fibers contribute to strength?
Muscle fibers bundle together into fascicles, which bundle into larger muscle tissues, increasing strength.
IMPORTANT. ATP AND MYOSIS
IMPORTANT

What is the significance of multinucleation in skeletal muscle fibers?
Multinucleation allows for greater control of protein synthesis and muscle repair.
What is the primary function of actin and myosin in muscle contraction?
Actin and myosin interact to produce the force necessary for muscle contraction.
What is the difference between striated and non-striated muscles?
Striated muscles have a banded appearance due to organized myofilaments, while non-striated muscles do not.
What is the role of the neuromuscular junction?
The neuromuscular junction is the site where a motor neuron communicates with a muscle fiber to initiate contraction.
What does the thick red filament represent in muscle contraction?
Myosin
What does the blue thinner filament represent in muscle contraction?
Actin
What is the role of Titan in muscle contraction?
Titan holds the end of the myosin in place for contraction.
What is the function of dystrophin in muscle tissue?
Dystrophin acts as a shock absorber.
What is the role of nebulin in muscle contraction?
Nebulin acts as a contraction regulator and a structural backbone for actin.
What is excitation-contraction coupling?
The link between the electrical signal (action potential) and the physical contraction of muscles.
What is the function of T tubules in muscle cells?
T tubules transmit the action potential into the muscle cell.
What is the role of the sarcoplasmic reticulum?
The sarcoplasmic reticulum stores calcium ions necessary for muscle contraction.
What triggers the release of calcium from the sarcoplasmic reticulum?
The binding of calcium to ryanodine receptors after the action potential stimulates calcium channels. Calcium regulates ryanodine receptors → calcium release from stores
STIMULES RELEASE OF CLACIUM
What is calcium-induced calcium release?
Calcium entering the cell stimulates the release of more calcium from the sarcoplasmic reticulum.
What happens when calcium binds to troponin?
Troponin changes shape, causing tropomyosin to move and expose the actin active sites.
What is the role of ATP in muscle contraction?
ATP binds to the myosin head, activating it for binding to actin.
What occurs when ATP is broken down on the myosin head?
Energy is released, allowing the myosin head to cock back and prepare for contraction.
What is a crossbridge in muscle contraction?
The binding of actin and myosin that allows muscle contraction to occur.
What is the significance of troponin C?
How it works
Low Ca²⁺ (muscle relaxed):
Troponin keeps tropomyosin blocking the myosin-binding sites on actin → no contractionHigh Ca²⁺ (muscle stimulated):
Ca²⁺ binds to troponin C (TnC) → troponin changes shape → tropomyosin moves → myosin binds actin → contraction
Troponin C is the specific troponin that binds calcium to initiate muscle contraction.
TnT | Binds to Tropomyosin and anchors the troponin complex to the actin filament | T for Tropomyosin |
TnI | Inhibits actin-myosin binding by blocking binding sites on actin
| I for Inhibits |
TnC | Binds Calcium ions → triggers conformational change → exposes binding sites Calcium binds to troponin C, causing a conformational change that moves tropomyosin | C for Calciu m |
How does the myosin head change when activated?
Step | ATP/ADP State | Energy State | Myosin Action | Description |
|---|---|---|---|---|
1. ATP binds | ATP bound | Low energy | Myosin head detaches from actin | ATP binding reduces myosin’s affinity for actin, causing detachment. |
2. ATP hydrolysis | ADP + Pi | High energy | Myosin head cocks forward | ATP hydrolysis energizes the myosin head into a “cocked” position. |
3. Cross-bridge forms | ADP + Pi | High energy | Myosin binds to exposed actin site | Myosin binds to actin, forming a cross-bridge. |
4. Power stroke | ADP + Pi released | Low energy | Myosin head pivots and pulls actin | The release of ADP and Pi triggers the power stroke that moves actin. |
5. New ATP binds | ATP bound | Low energy | Myosin detaches, cycle resets | A new ATP binds, causing myosin to release actin and restart the cycle. |
What is the role of tropomyosin in muscle contraction?
Tropomyosin covers the actin active sites, preventing binding until calcium binds to troponin.
What happens to the muscle fibers during contraction?
The muscle fibers shorten as actin and myosin slide past each other.
What is the function of the sarcolemma?
The sarcolemma is the cell membrane of muscle fibers that conducts action potentials.
What initiates the action potential in muscle contraction?
A stimulus, such as the desire to move, triggers the action potential.
What is the role of calcium in muscle contraction?
Calcium binds to troponin, allowing actin and myosin to interact and contract.
What happens to the muscle when the action potential ceases?
Calcium is reabsorbed, and the muscle relaxes as actin and myosin detach.
What initiates the process of muscle contraction?
A stimulus, such as the desire to move, which triggers nervous stimulation.
What happens after the myosin head is activated?
It forms a crossbridge with actin, pulls the actin filament inward, leading to muscle contraction.
What is the significance of the crossbridge in muscle contraction?
The crossbridge allows the myosin head to pull actin filaments, resulting in the shortening of the muscle.
What are the components of a sarcomere?
Z discs, M line, A band, I band, and H zone.
What does the A band represent in a sarcomere?
The A band represents the overlap between actin and myosin filaments.
What is the function of the I band in a sarcomere?
The I band contains only actin filaments and is where the muscle appears lighter.
What is the H zone in a sarcomere?
The H zone contains only myosin filaments and is lighter than the A band.
What is the M line in a sarcomere?
The M line is the center of the sarcomere where myosin filaments are anchored.
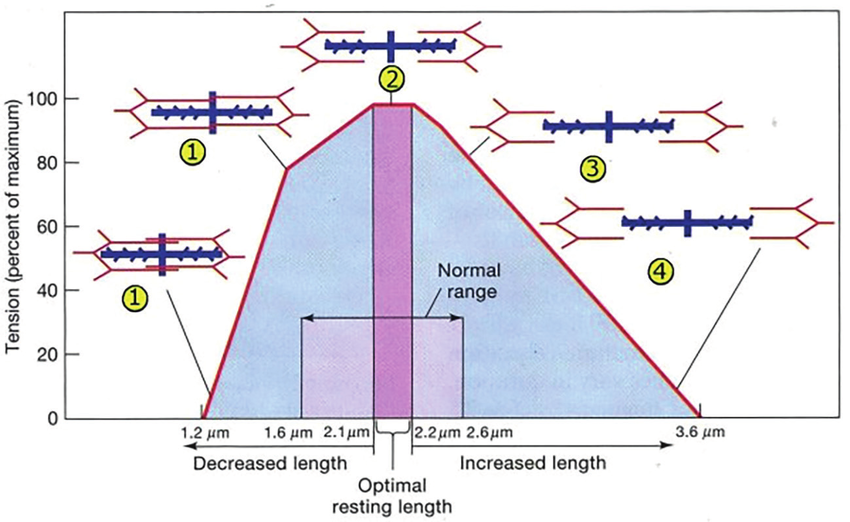
What is the optimal overlap of actin and myosin for muscle contraction?
A balance where there is enough overlap to form crossbridges without excessive overlap that limits contraction distance.
What is the first source of ATP used during muscle contraction?
The ATP that is already present in the muscle cells.
What happens when the initial ATP supply is depleted?
Creatine phosphate is used to regenerate ATP for continued muscle contraction.
What is the final source of ATP during muscle contraction?
ATP generated through oxidative phosphorylation.
What is the role of the T-tubules in muscle contraction?
They help transmit the action potential deep into the muscle fiber, triggering calcium release.
What is the process of calcium-induced calcium release?
Calcium entering the muscle cell triggers the release of more calcium from the sarcoplasmic reticulum.
What occurs during the cocking of the myosin head?
The myosin head is reactivated and prepared for the next power stroke.
What is the significance of the Z disc in a sarcomere?
The Z disc marks the boundary of each sarcomere and anchors the actin filaments.
How does the muscle shorten during contraction?
All parts of the sarcomere shorten as actin filaments are pulled toward the midline.
What happens if there is too much overlap between actin and myosin?
It limits the distance the muscle can contract, reducing efficiency.
What happens if there is too little overlap between actin and myosin?
It results in insufficient crossbridge formation, leading to weaker contractions.
What is the relationship between crossbridges and muscle contraction strength?
More crossbridges formed lead to stronger muscle contractions.
What is the effect of muscle contraction on the sarcomere structure?
Contraction results in the shortening of the sarcomere as actin filaments are pulled inward.
What is the role of the sarcoplasmic reticulum in muscle contraction?
It stores calcium ions and releases them during muscle activation.
What triggers the opening of voltage-gated calcium channels?
An action potential traveling down the T-tubules.
What is the primary source of ATP for muscle contraction?
ATP is primarily sourced from oxidative phosphorylation.
What are the three sources of ATP mentioned for muscle contraction?
Existing ATP, 2. ADP from creatine phosphate, 3. ATP from oxidative phosphorylation.
Which region of the sarcomere has an overlap of both myosin and actin filaments?
The A band.
What protein does calcium bind to in muscle contraction?
Troponin.
What is the role of troponin in muscle contraction?
Troponin binds calcium, allowing tropomyosin to move and expose the myosin binding site on actin.
How does cardiac muscle contraction differ from skeletal muscle contraction?
Cardiac muscle contraction is involuntary and initiated by pacemaker cells, while skeletal muscle contraction is voluntary and initiated by nervous impulses.
What are intercalated discs and their function in cardiac muscle?
Intercalated discs connect cardiac muscle cells and facilitate the spread of action potentials between cells.
What initiates the action potential in cardiac muscle cells?
Pacemaker cells generate the impulse that initiates the action potential.
What is the significance of calcium in cardiac muscle contraction?
Calcium is released from the sarcoplasmic reticulum and also enters the cell through intercalated discs, stimulating further calcium release and contraction.
What happens to cardiac muscle cells during a myocardial infarction?
Cells die due to lack of oxygen, leading to the release of troponin into the bloodstream.
What is the main source of calcium for contraction in skeletal muscle?
The sarcoplasmic reticulum.
How does calcium enter cardiac muscle cells?
Calcium can diffuse directly into the cell through intercalated discs and is also released from the sarcoplasmic reticulum.
What is the consequence of lactic acid buildup in cardiac muscle cells?
It leads to anaerobic respiration and cell death, which can release troponin into the bloodstream.
What is the role of the SAN and AVN nodes in cardiac muscle?
They act as pacemakers, generating impulses that regulate heart contractions.
What is the difference between aerobic and anaerobic respiration in cardiac muscle?
Aerobic respiration requires oxygen, while anaerobic respiration occurs when oxygen is insufficient, leading to lactic acid buildup.
What is the function of tropomyosin in muscle contraction?
Tropomyosin blocks the myosin binding sites on actin until calcium binds to troponin.
What mechanism allows for the contraction of cardiac muscle cells?
Calcium release triggers contraction through a cascade effect initiated by pacemaker cells.
What is the significance of the A band in muscle contraction?
The A band is where myosin and actin filaments overlap, crucial for muscle contraction.
What happens to the calcium levels during muscle contraction?
Calcium levels rise, binding to troponin and allowing muscle contraction to occur.
How do cardiac muscle cells communicate with each other?
Through intercalated discs that allow the passage of ions and action potentials.
What is the primary energy source for cardiac muscle contraction?
Primarily from aerobic respiration, utilizing oxygen.
What is the function of the T-tubules in muscle cells?
They facilitate the transmission of action potentials into the muscle fiber, triggering calcium release.
What is the relationship between troponin and tropomyosin in muscle contraction?
Troponin binds calcium, causing tropomyosin to move and expose binding sites on actin for myosin.
What role does troponin play in muscle contraction?
Troponin binds calcium, allowing the actin active site to be exposed for muscle contraction.
Toilet Part / Action | Muscle Component / Event | Function / Analogy Explanation |
|---|---|---|
Toilet handle | Depolarization of the muscle cell membrane (action potential) | The electrical signal (like flushing) triggers the whole process. |
Cable from handle to valve | DHPR (Dihydropyridine Receptor) on the T-tubule membrane | Acts as the “sensor” for the voltage change — detects the electrical signal. |
Valve on the tank | RYR-1 (Ryanodine Receptor) on the sarcoplasmic reticulum (SR) | The “release valve” — opens to let Ca²⁺ flow out of the SR. |
Water in the tank | Calcium (Ca²⁺) stored in the SR | The stored supply, waiting to be released. |
Water flowing into the bowl | Cytoplasmic Ca²⁺ increase | Ca²⁺ floods into the cytoplasm to start contraction. |
Water draining away / refilling tank | Ca²⁺ reuptake into SR by SERCA pumps | The calcium is pumped back into the SR to end contraction (resetting for the next “flush”). |
analogy
What happens if troponin is not present?
Without troponin, calcium cannot bind, preventing the exposure of the actin active site and leading to limited or no muscle contraction.
What are the three types of troponin?
Troponin C, Troponin I, and Troponin T.
What is the function of Troponin C?
Troponin C binds calcium, which is essential for exposing the actin active site.
What is the role of Troponin I?
Troponin I helps stop muscle contraction in the heart when it is at rest and is specific to cardiac muscle cells.
How can elevated troponin levels indicate a heart problem?
Elevated Troponin I levels specifically indicate a cardiac issue, such as a heart attack.
What is the function of Troponin T?
Troponin T attaches muscle fibers together and allows the heart to contract properly.