Embryo 10 - Respiratory System
1/60
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No study sessions yet.
61 Terms
What germ layers contribute to development of the respiratory system?
Ectoderm, mesoderm, and endoderm.
What does splanchnic mesoderm form in the respiratory tract?
Cartilage and smooth muscle of the trachea and bronchi.
What does paraxial mesoderm form in the respiratory tract?
somitomeres
What do somitomeres form in the respiratory system?
Skeletal muscles of the larynx.
What structures are derived from endoderm in the airway?
Epithelial lining and glands.
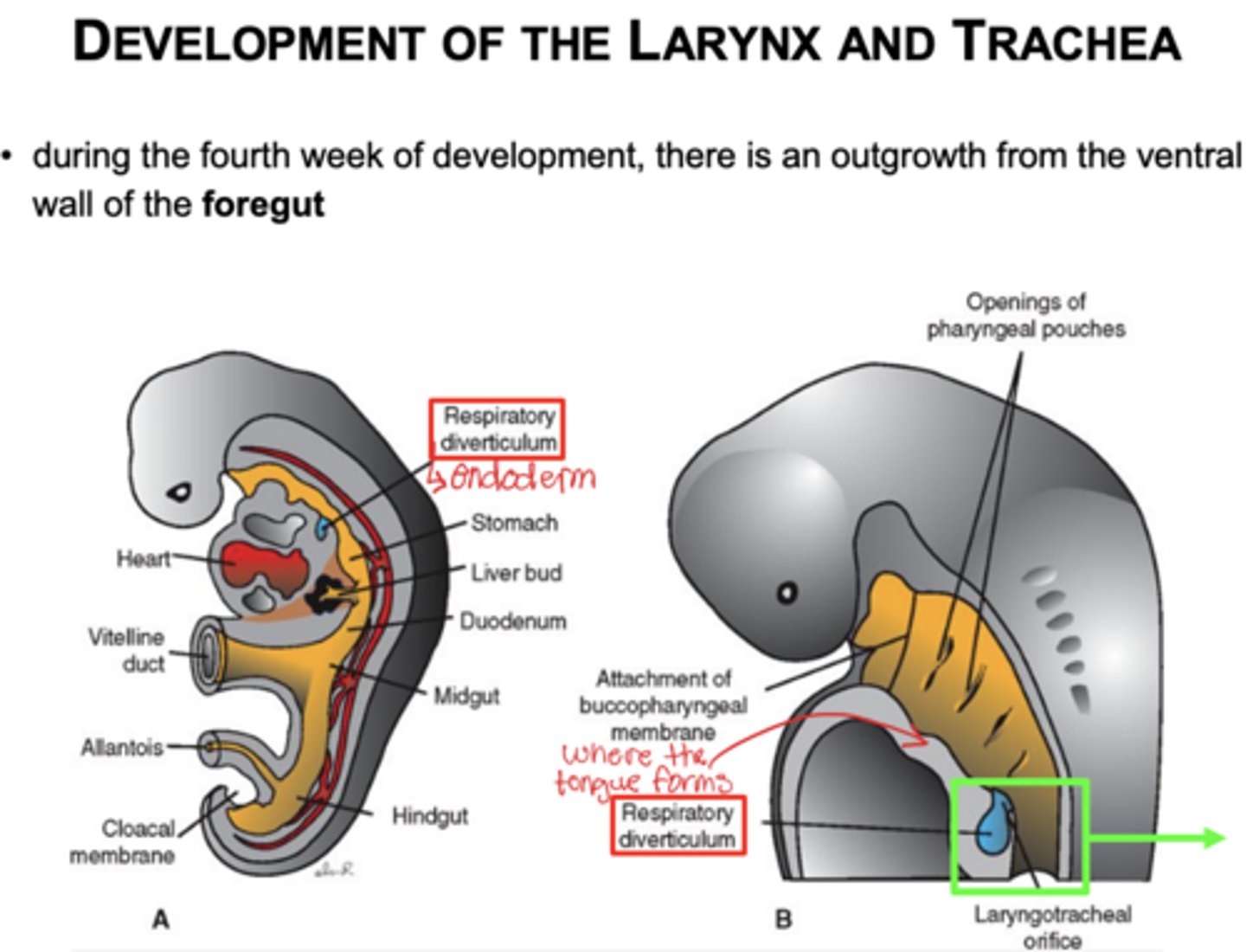
What is the respiratory diverticulum?
lung bud its a dome-shaped structure that appears on the ventral wall of the foregut and will develop into the lungs.
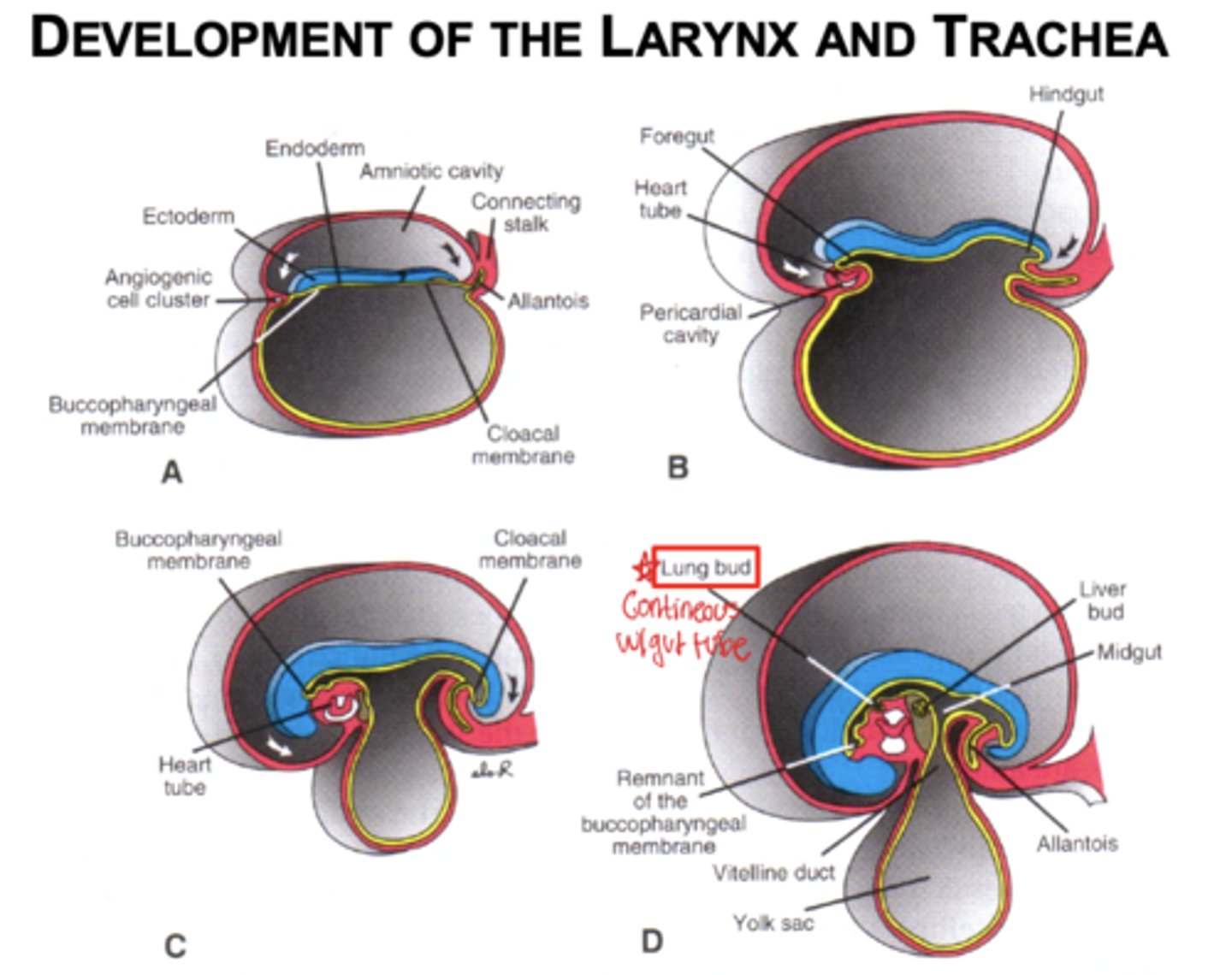
When does the respiratory system begin forming?
Week 4 there is an outgrowth from the ventral wall of the foregut
What separates the lung buds from the foregut?
Esophagotracheal ridges (side to side separation from the foregut)
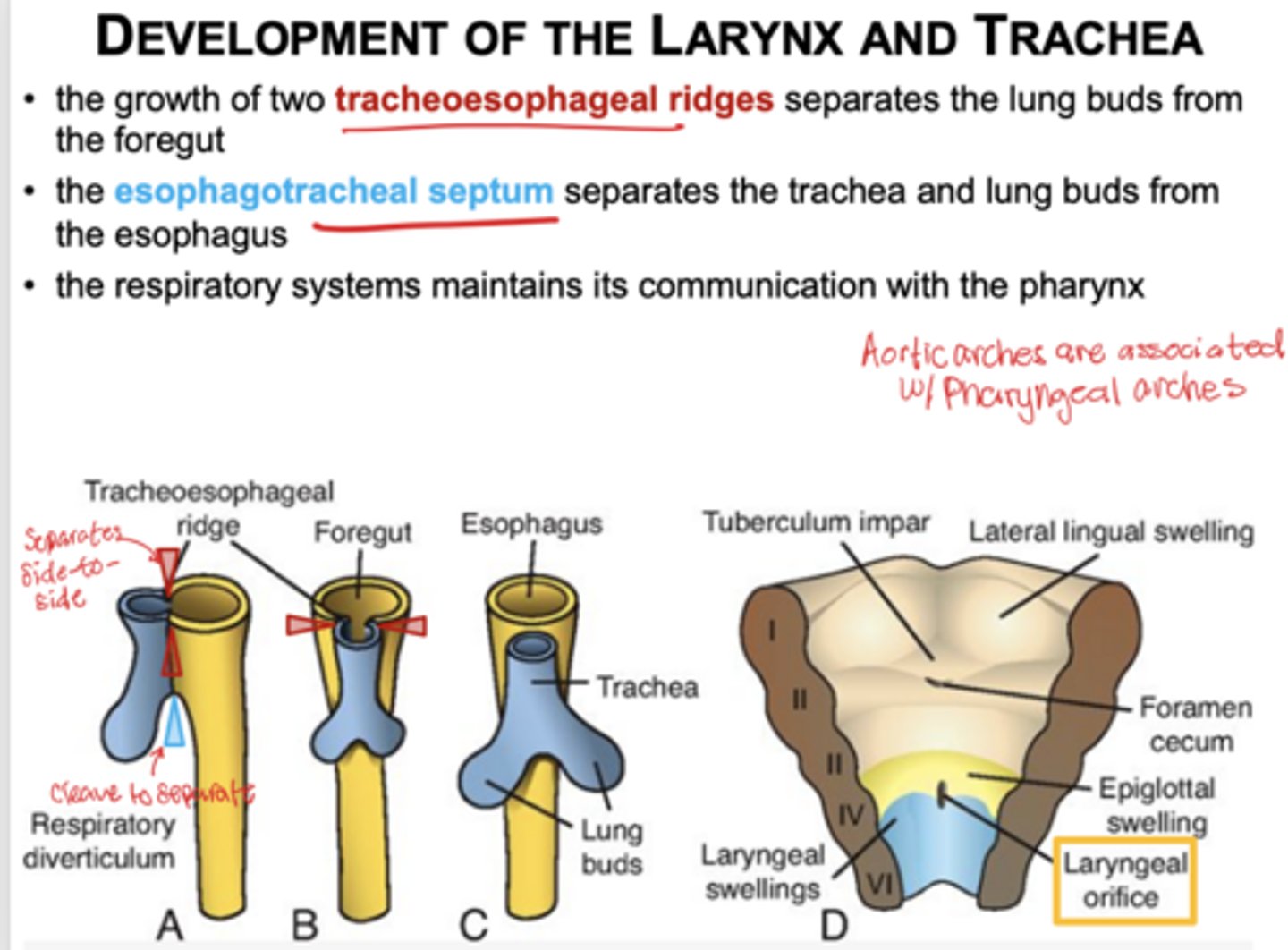
What structure divides the trachea from the esophagus?
Esophagotracheal septum (cleaves to separate) divides into dorsal portion the esophagus and a ventral portion the trachea
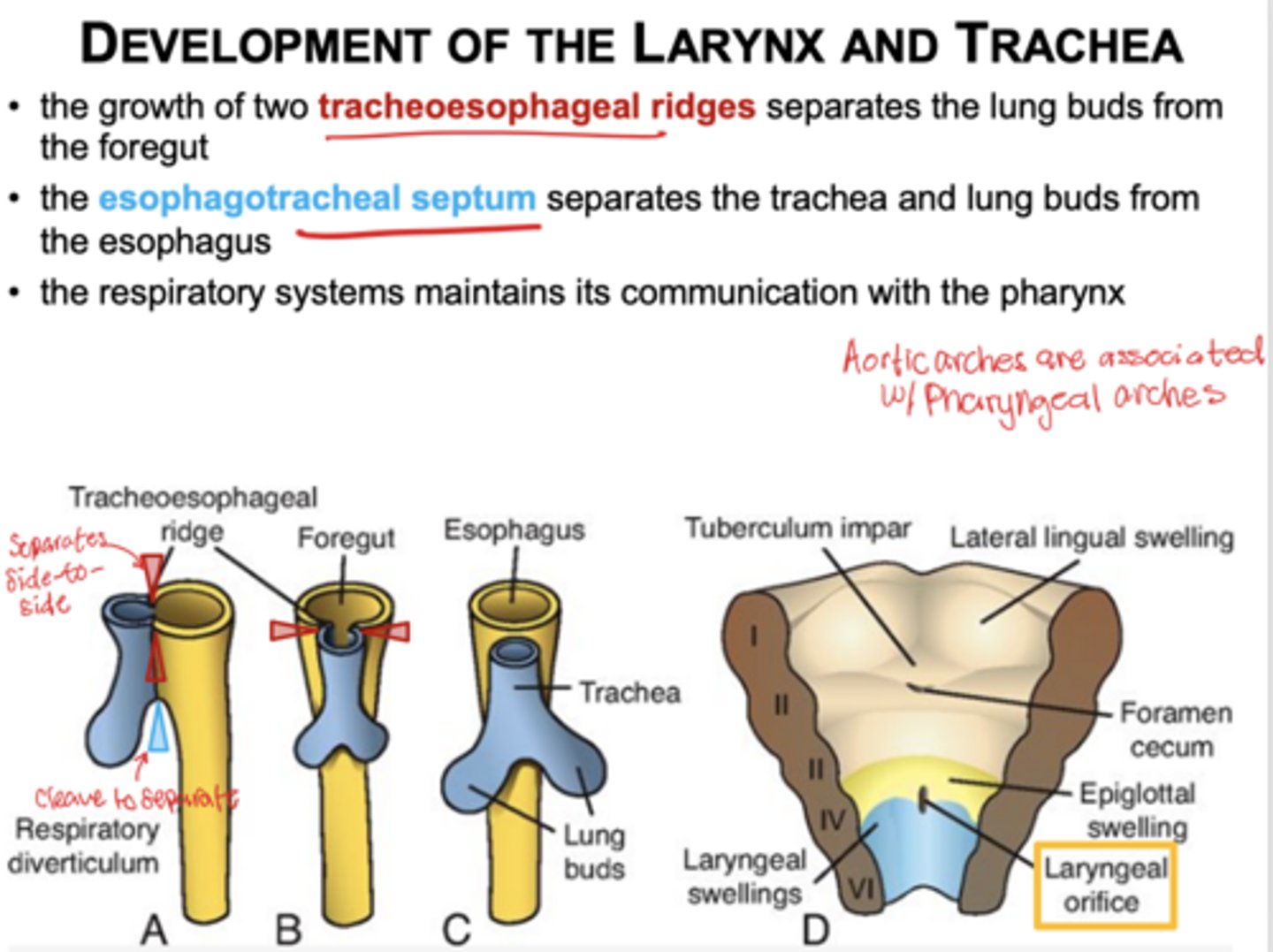
Does the respiratory tract stay connected to the gut tube?
Yes, through the pharynx.
What is the embryologic origin of laryngeal epithelium?
Endoderm.
What cells form laryngeal cartilages?
Neural crest cells.
What causes changes in the laryngeal orifice shape?
Growth of laryngeal cartilages.
Which pharyngeal arch forms the cricothyroid muscle?
4th arch.
What nerve innervates the cricothyroid muscle?
External laryngeal from superior laryngeal nerve (branch of vagus)
Which arch forms the remaining laryngeal muscles?
6th arch.
What nerve innervates most laryngeal muscles?
Recurrent laryngeal nerve branch of vagus
Which arches contribute to epiglottis formation?
3rd and 4th arches.
Which arches form the remaining laryngeal cartilages?
4th and 6th arches.
What do laryngeal ventricles separate?
True and false vocal folds.
Explain how the pleura of the lungs develop?
Pleuroperitoneal and pleuropericardial folds separate the pericardiperitoneal canals from the periotoneal and pericardial cavities.
The remaining spaces form the pleural cavities. Mesoderm coverinng the outside lung becomes visceral pleura and somatic mesoderm covering the body wall from the inside becomes parietal pleura.
Space between = pleural cavity
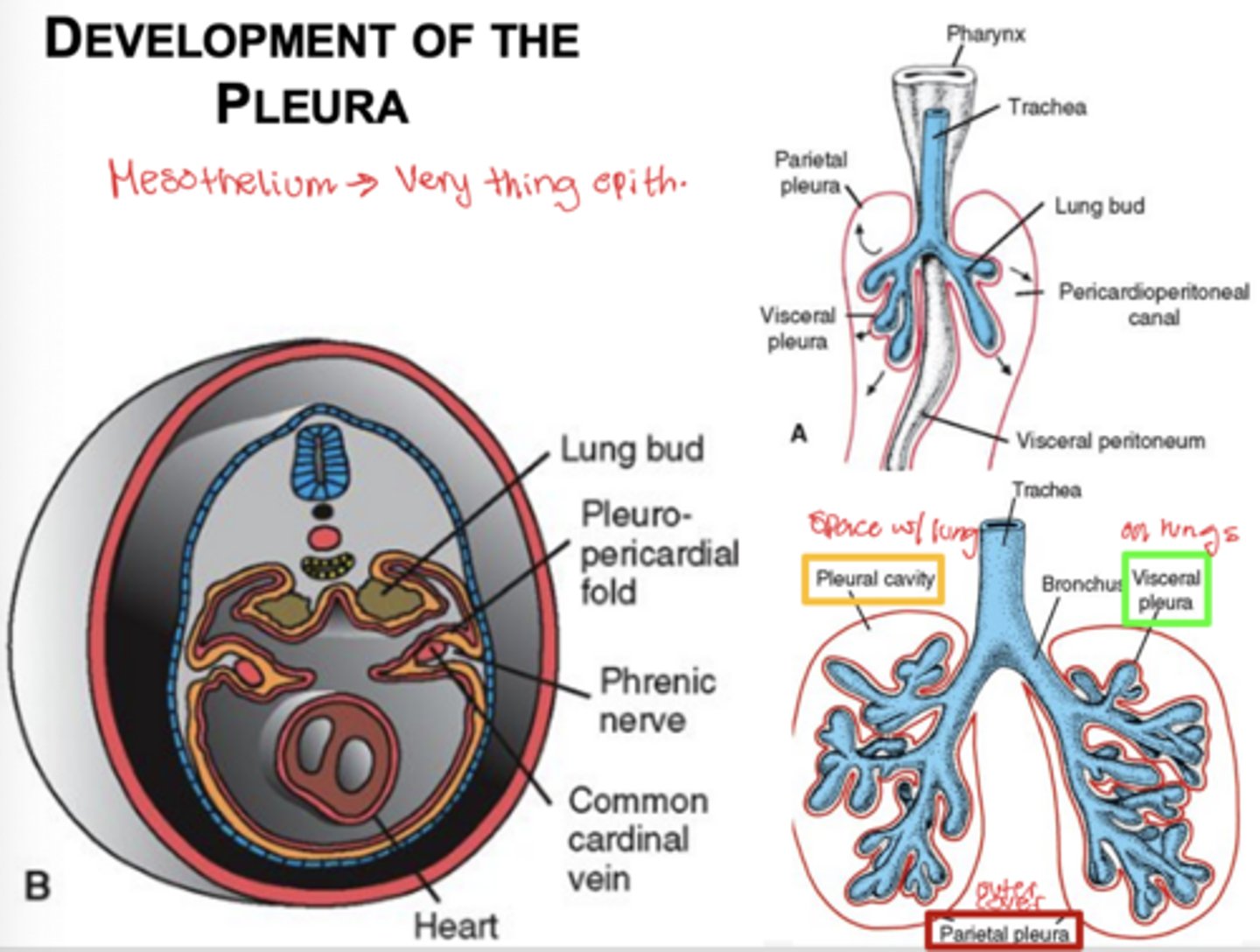
What is mesothelium and where is it found?
simple squamous epithelium that forms the serous membranes of body cavities (very thin epithelium)
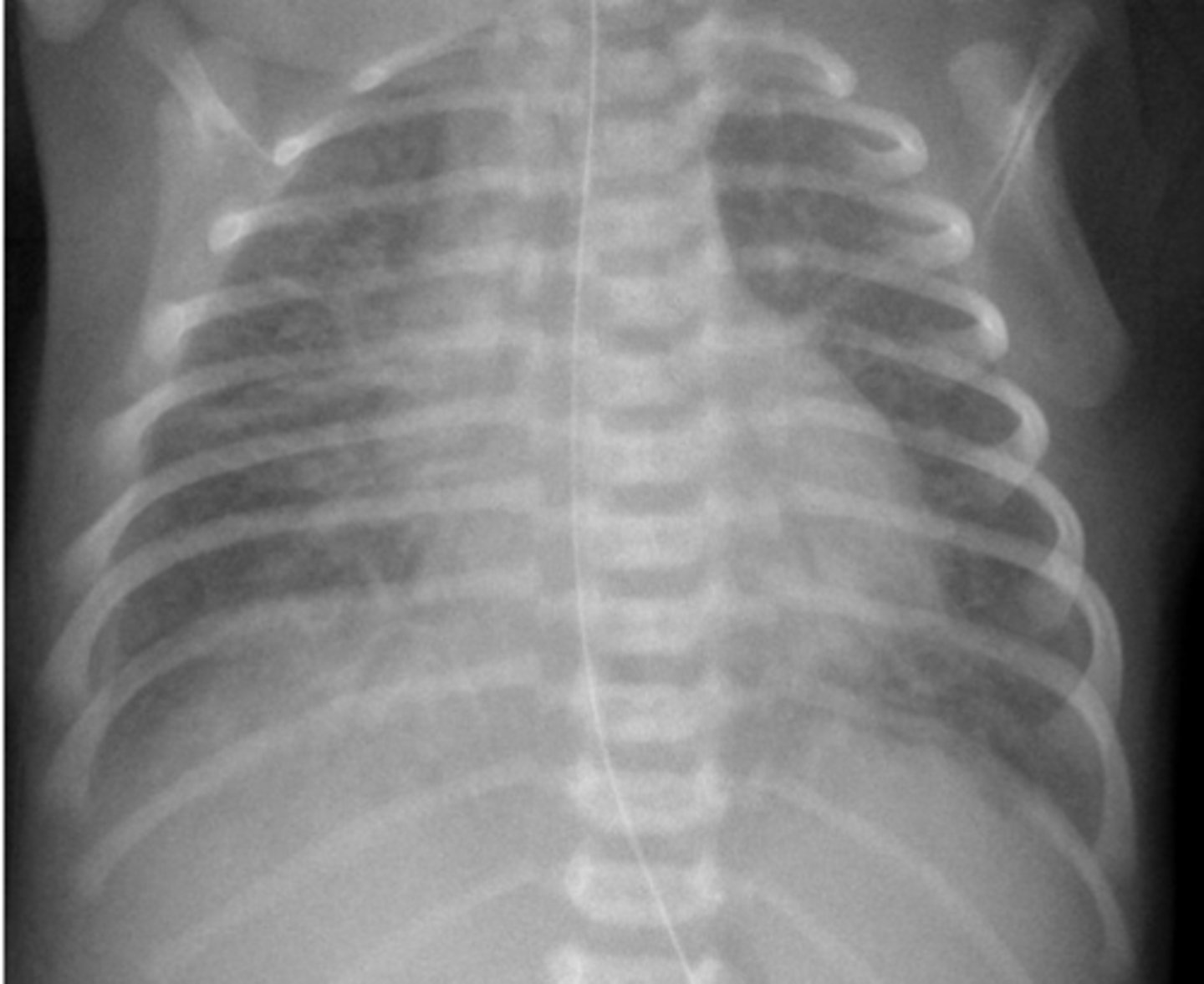
What is meconium aspiration? How does it appear on CTs?
during infants first breath amniotic(fecal waste) is inhaled and enters the lungs. Baby swallows meconium
smokey appearance on CT
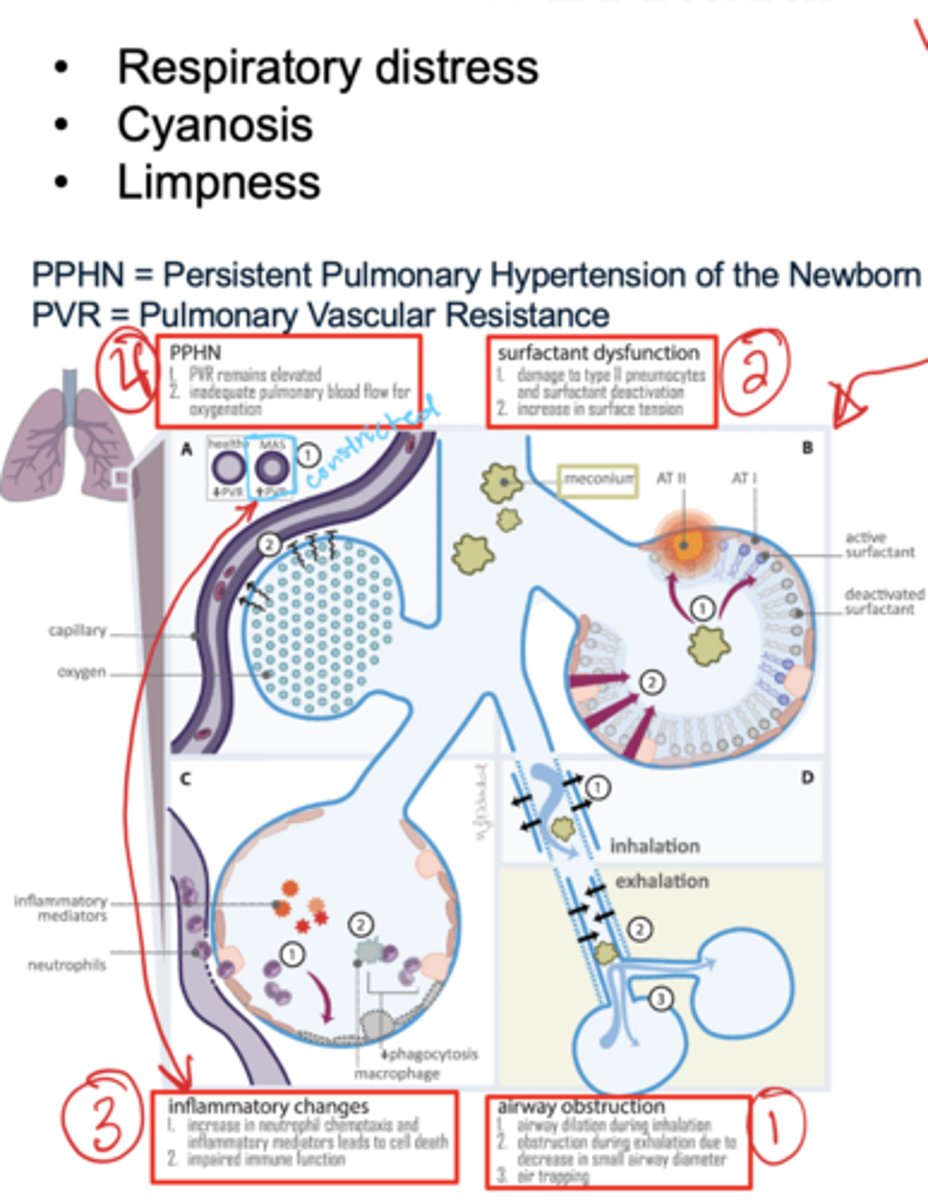
What can result from meconium aspiration?
1. Airway obstruction (respiratory distress)
2. Surfactant dysfunction (damage to type II pneumocytes - increases surface tension) baby appears cyanotic
3. Inflammatory changes (high neutrophil count - causes cell death)
4. Persistent pulmonary hypertension of the newborn
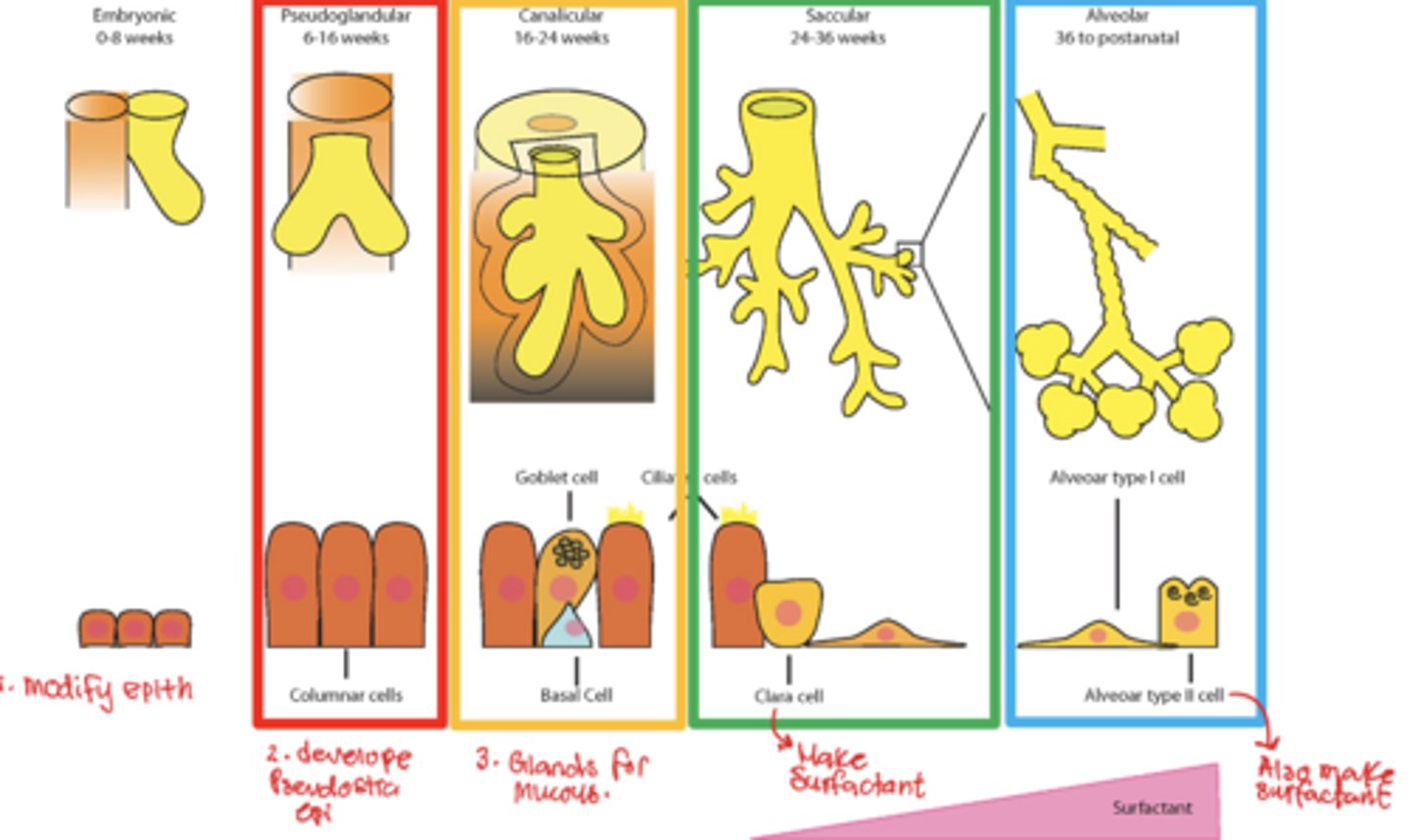
List the 5 stages of lung development?
1. embryonic stage
2. pseudoglandular stage
3. canalicular stage
4. terminal sac stage
5. alveolar stage
What occurs in the embryonic stage of lung development?
Lung buds grow into the intraembryonic coelom and form bronchi.
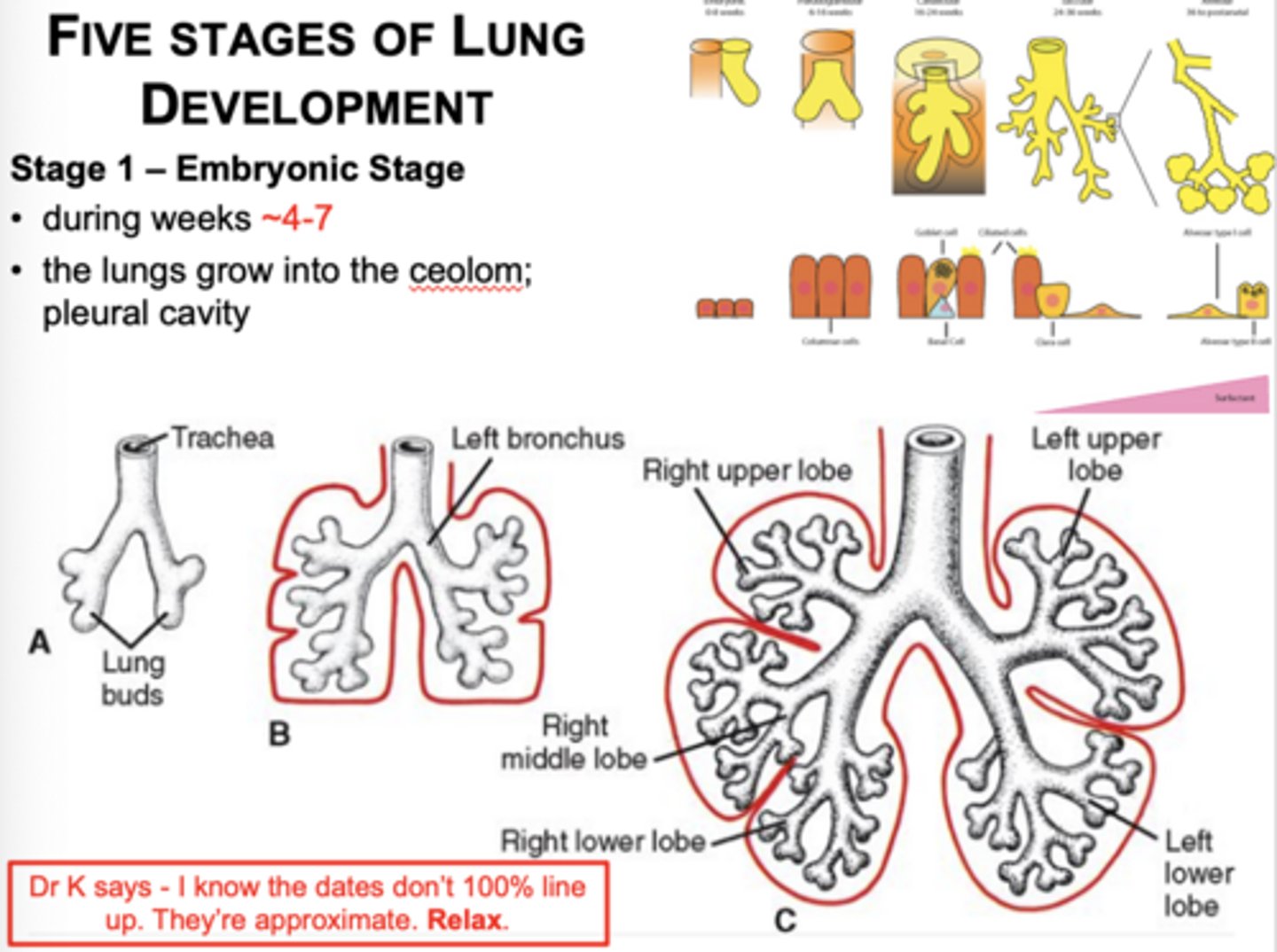
When do right vs left bronchial differences first appear?
During the embryonic stage (4-7 weeks)
What structures are present in the pseudoglandular stage?
Terminal bronchioles
No, it looks a lot like glands
Is gas exchange possible during the pseudoglandular stage? How does it appear?
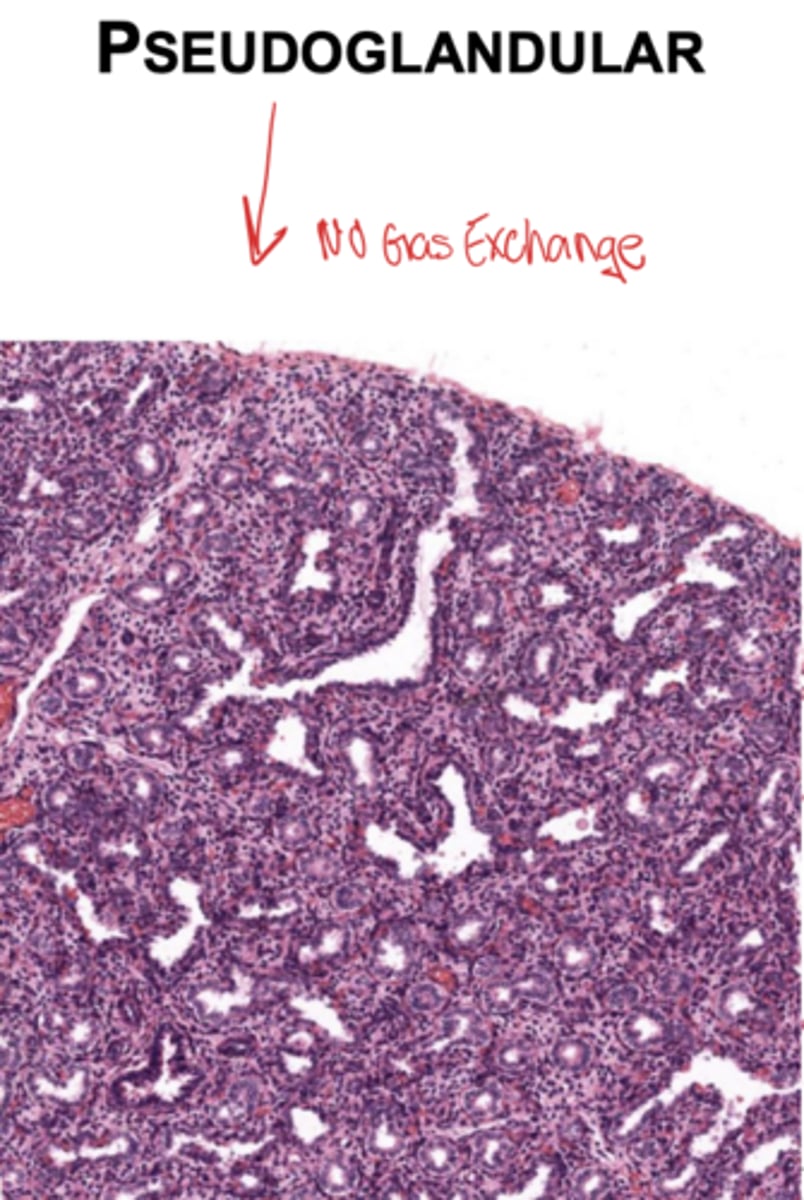
What is the epithelial shape distally during the pseudoglandular stage?
Cuboidal.
What structures appear during the canalicular stage?
Respiratory bronchioles and alveolar ducts.
When does gas exchange first become possible?
Late canalicular stage.
What happens to distal airspaces during the canalicular stage?
They widen while capillary networks form.
What major epithelial change occurs in the terminal sac stage?
Type I alveolar cells form.
When do Type II alveolar cells begin producing surfactant?
Near the beginning of the terminal sac stage.
Why is surfactant important?
Prevents alveolar collapse and allows gas exchange.
What is the alveolar stage?
begins near birth and continues until approx. 8 years of age
When do mature alveoli form?
After birth.
What increases during the alveolar stage?
Number and size of alveoli.
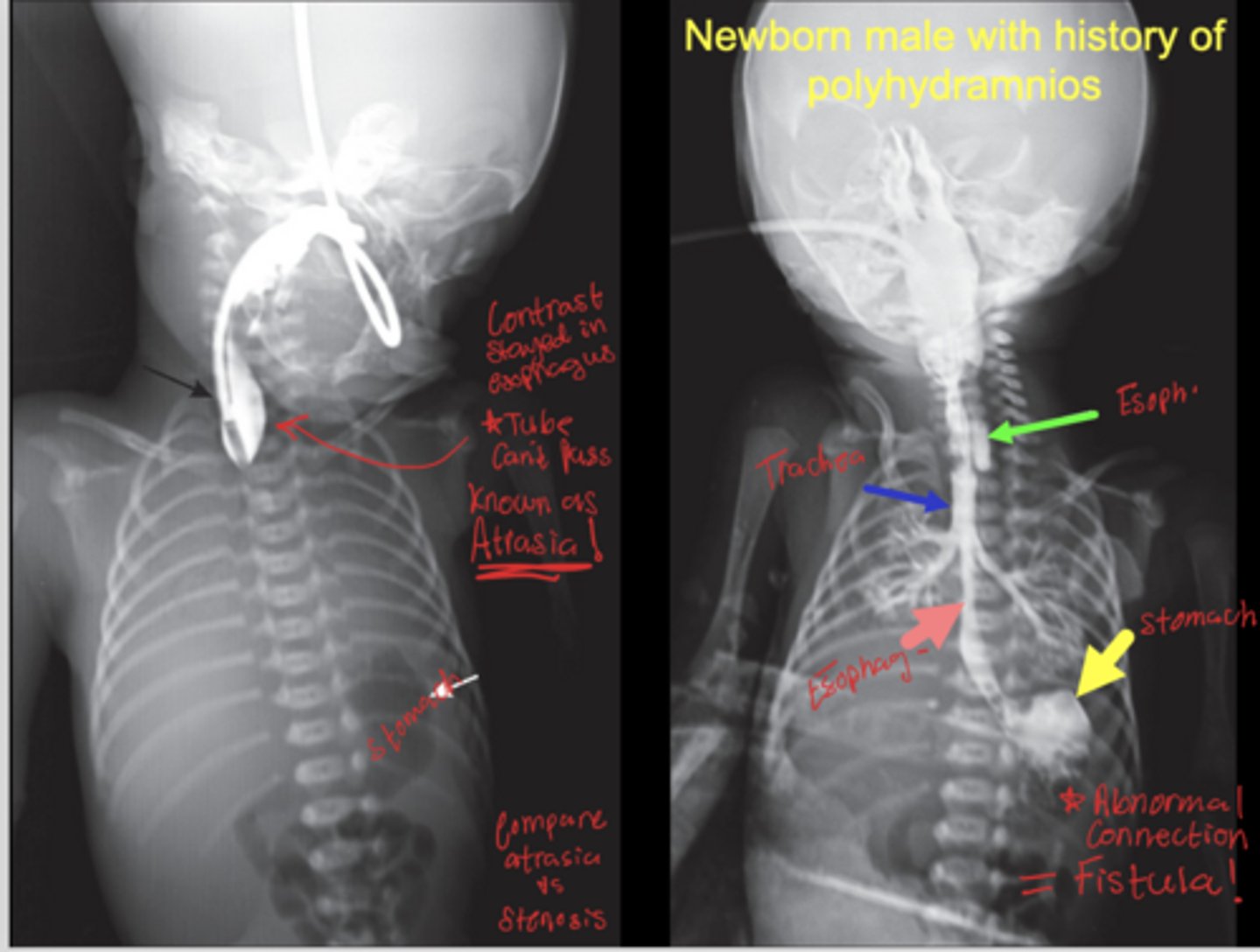
What causes esophageal atresia?
Abnormal partitioning of trachea and esophagus.
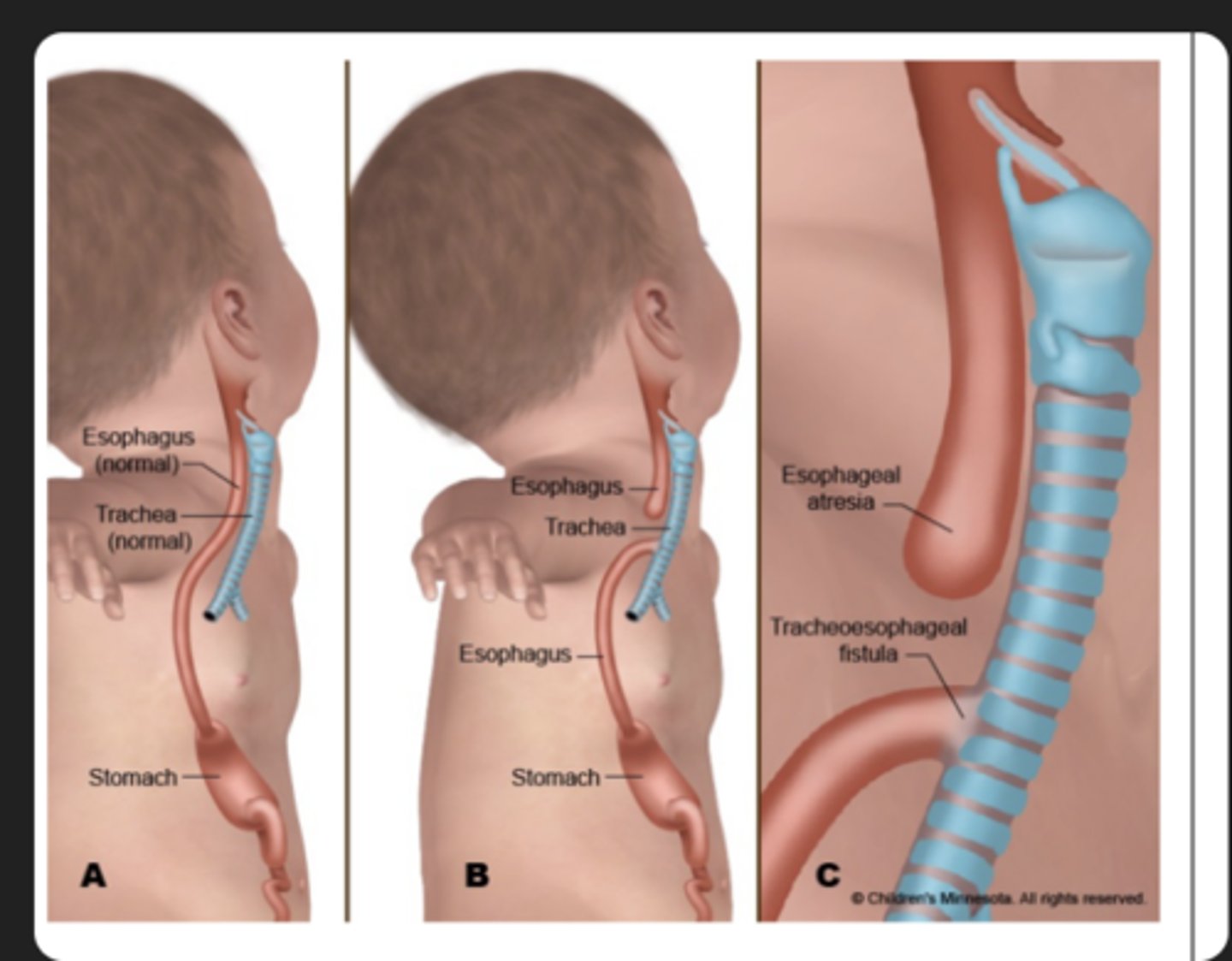
What is the most common fistula pattern?
tracheoesophageal (TE) prox. esophageal pouch with distal fistula to airway
Why does airway obstruction cause polyhydramnios?
The fetus cannot swallow amniotic fluid.
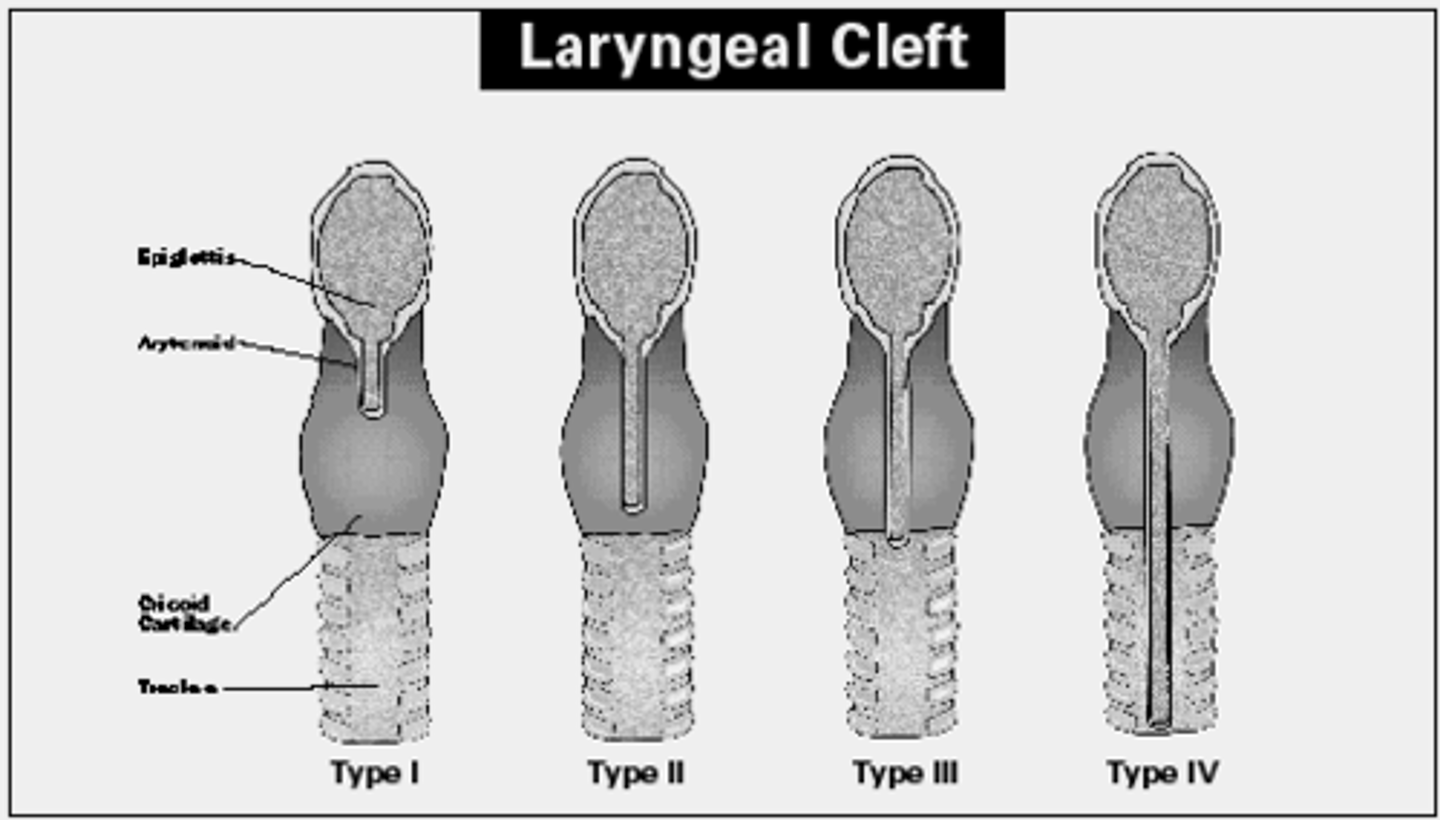
What is a laryngotracheoesophageal cleft?
the larynx/trachea fail to completely separate from the esophagus;
distinguished from fistulas by aphonia
What is a tracheal diverticulum?
Blind pouch projecting from the trachea.
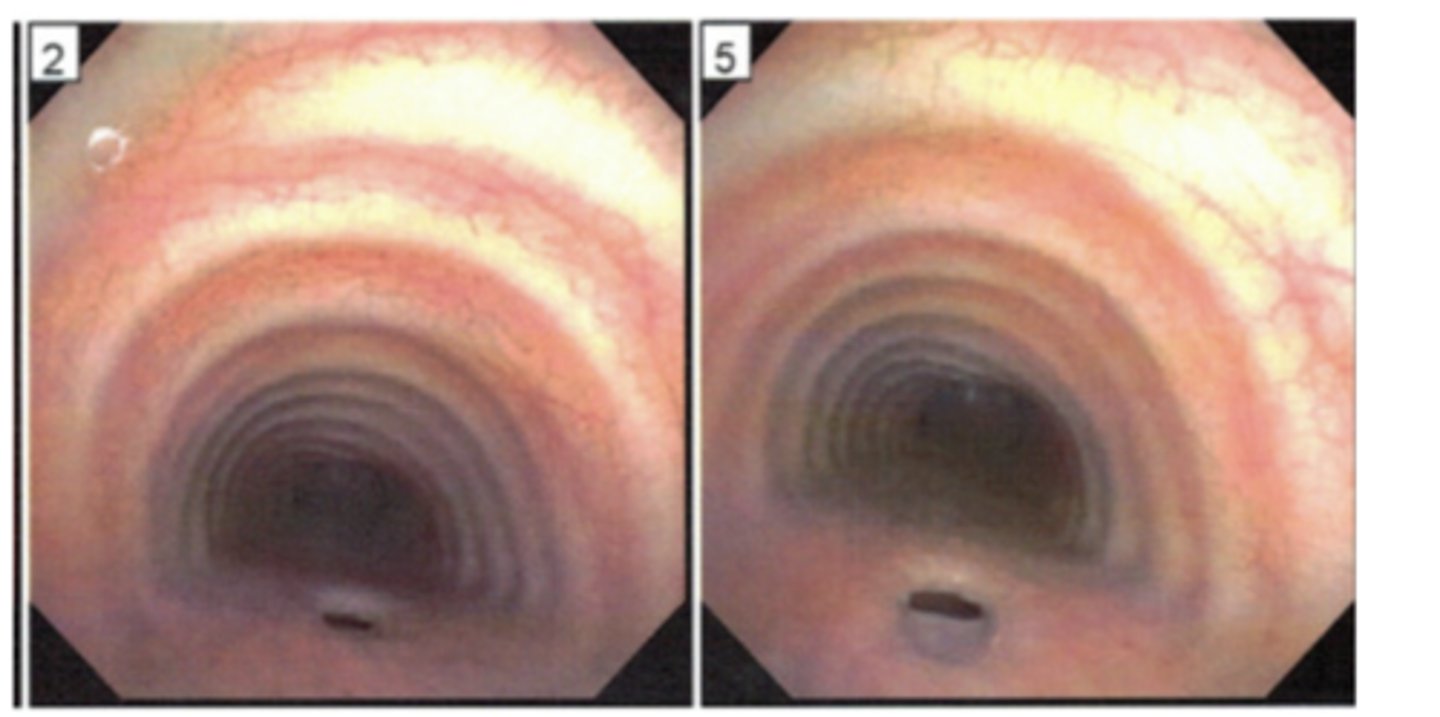
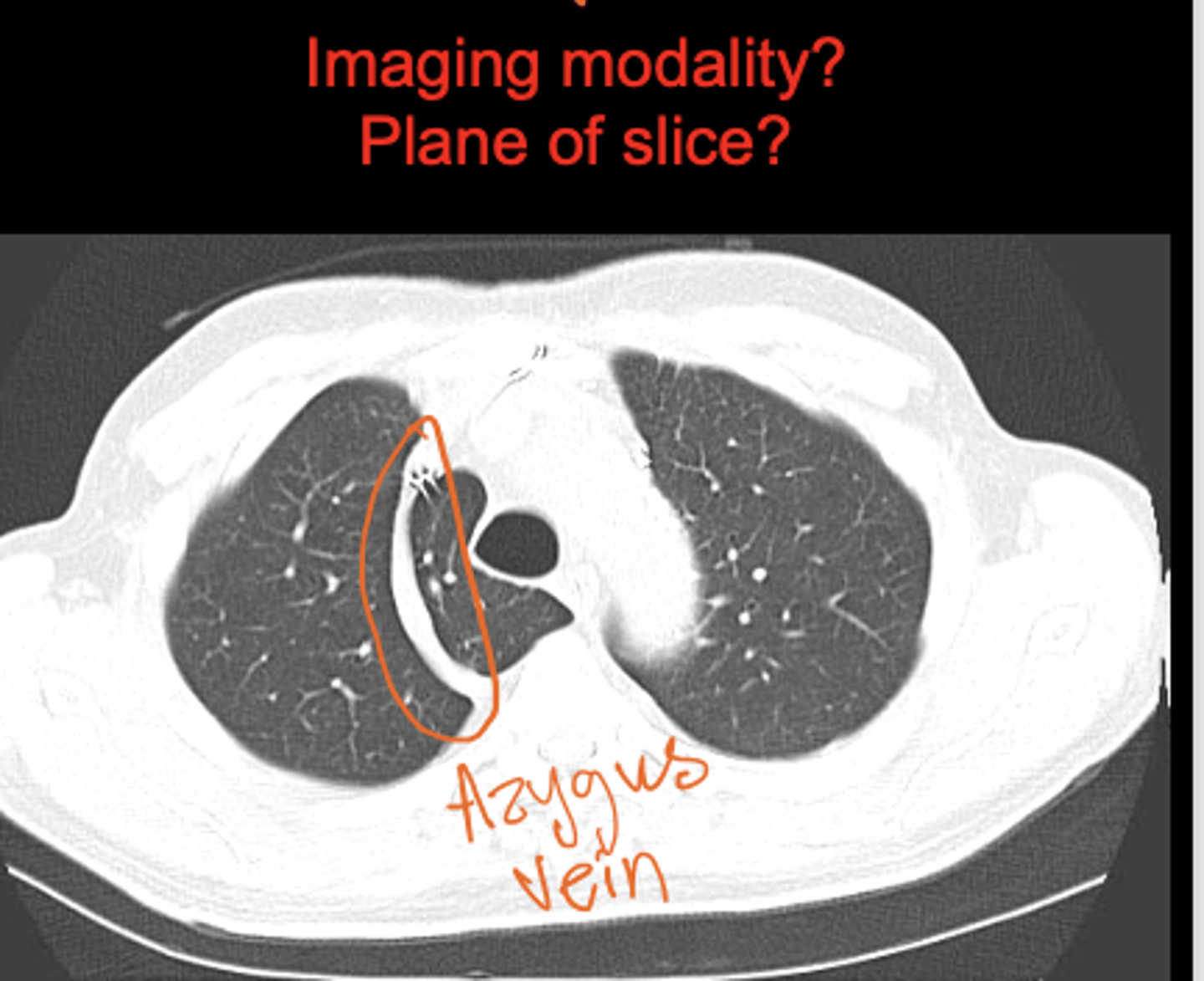
What is an azygos lobe?
A groove formed by the azygos vein at the right lung apex.
CT showing lung window
What causes congenital lung cysts?
Dilation of terminal bronchi.
What results if multiple cysts form?
Honeycomb lung appearance.
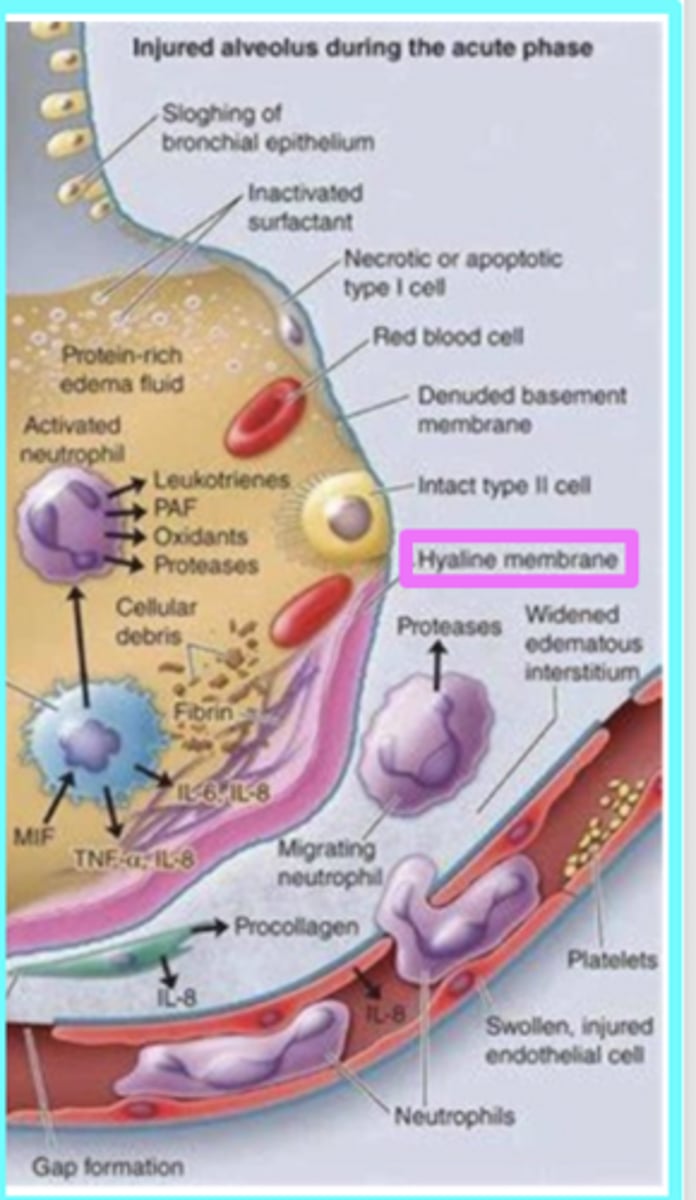
What causes neonatal respiratory distress syndrome?
Insufficient surfactant a
common cause of death to premature infants.
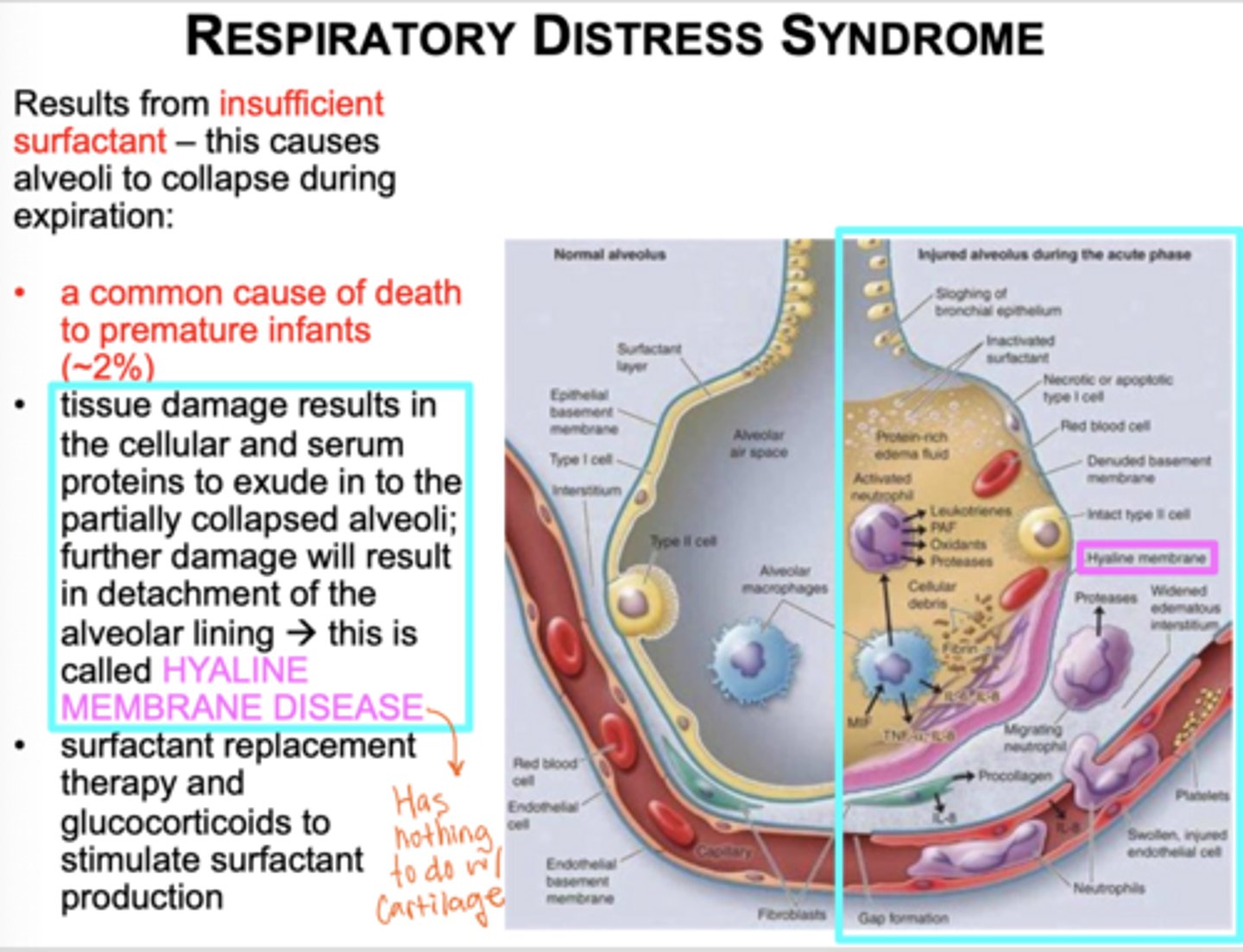
What happens to alveoli in RDS?
They collapse during expiration (commone cause of death to premature infants)
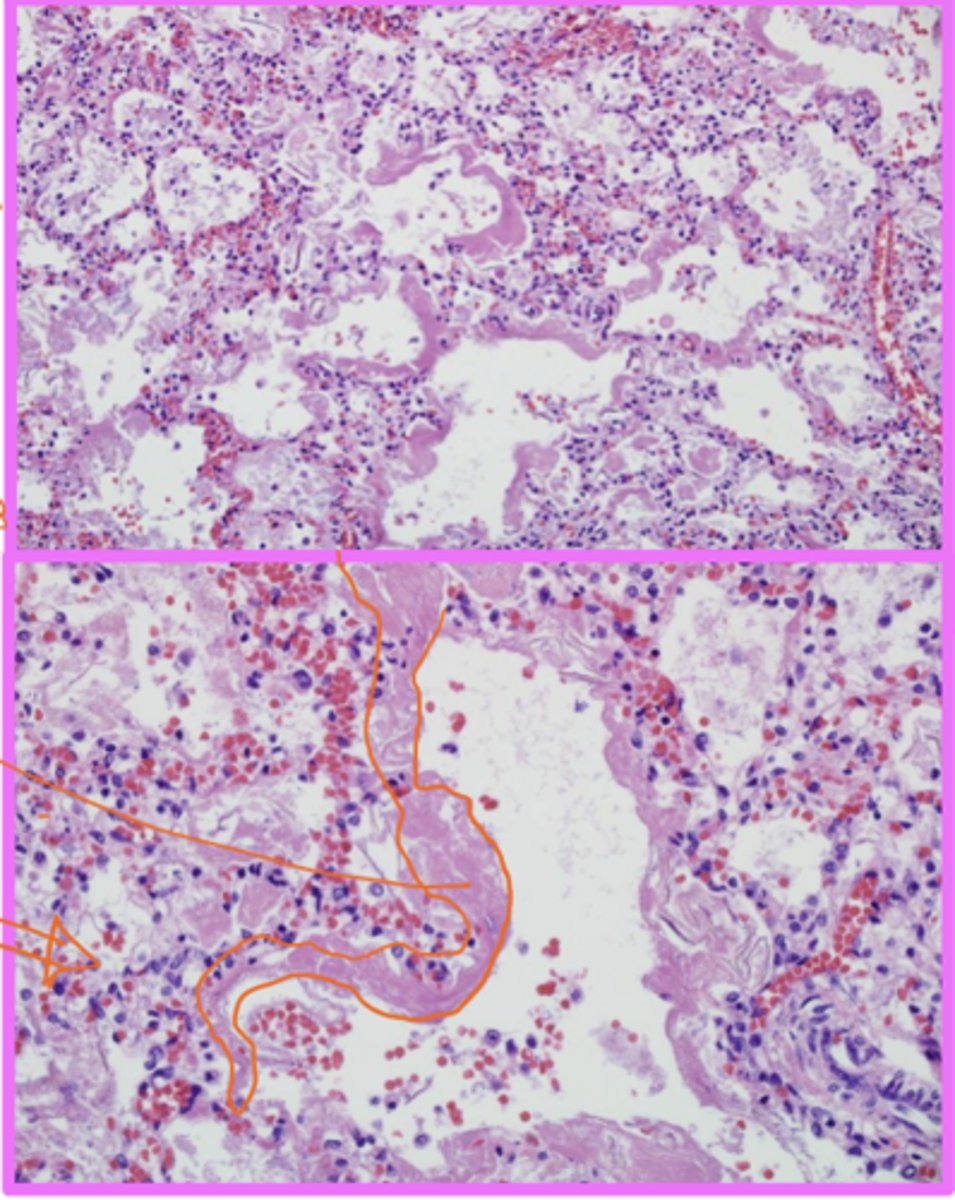
What is hyaline membrane disease?
Tissue damage from RDS results in cellular and serum proteins accumulating in the partially collapsed alveoli
Has nothing to do w/ cartilage
Hylaine membrane disease (outlined in orange - very cellular)
Identify the pathology
What treatments are used for RDS?
Surfactant replacement and glucocorticoids.
What is lung agenesis?
Complete absence of one or both lungs.
What is lung aplasia?
Rudimentary bronchus without lung tissue.
What is lung hypoplasia? What is it associated with?
agenesis, absence of one or both lungs; congenital absence of a lung (EXTREMELY RARE)
Congenital diaphragmatic hernia
What is ectopic lung tissue?
Lobes of lung tissue arising from trachea or esophagus.
What is an accessory lung?
Extra lung tissue supplied by systemic circulation.
What does VACTERL stand for?
V- Vertebral defect (spina bifida)
A- Anal atrasia (imperforate anus)
C- Cardia (dextrocardia)
TE- TrachEsophageal fistula
R- Renal (horse shoe kidney)
L- Limb (polydactyly)
What genetic condition is associated with VACTERL?
Trisomy 18.
What maternal factor is linked to VACTERL?
Maternal diabetes also exposure to contraceptive during the early stages of pregnancy.
How can lungs indicate live birth?
Live-born infant lungs float; stillborn lungs sink.