Pediatric Dermatology: Rash and Fever + Other Rashes
1/19
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
20 Terms
high fever, resolves, rash, herpesvirus 6, young, 7-13
Roseola Infantum: Background
-Characterized by 3-5 days of _____ ______ that ________ and is followed by a _____
-Etiology → human ___________ _ is the most common cause. Can also be caused by coxsackievirus, adenovirus, and parainfluenza virus type 1
-Epidemiology → ______ children, 90% of cases occur < 2 years old, peak incidence between __-__ months, and can occur at any time of year
fever, >, macular, neck, face, 1-2, lymphadenopathy, cough, vomiting
Roseola Infantum: Symptoms
-High _____ for 3-5 days (often _ 103 F)
-Rash after fever resolves
Blanching, ________ or maculopapular rash that is rose-pink
Starts on _____ and trunk and spreads to the ____ and extremities
Lasts __-__ days on average
-Cervical, postauricular, and/or occipital ________________ (very common)
-Cold symptoms like _____ and rhinorrhea are possible, as are ________/diarrhea

benign, supportive
Roseola Infantum: Diagnosis and Treatment
-Diagnosis → clinical
-Treatment → ______, self limiting disease. Provide _______ therapy like fluids and rest.
parvovirus B19, school, RBC, erythroid, benign, aplastic, anemia
Erythema Infectiosum: Background
-Etiology → human _____________ ___
-Epidemiology → ______ aged children
-Pathogenesis → affinity for ___ progenitor cells. Replicates in _______ stem cells → cell death → erythroid aplasia and anemia
-Healthy children → _______ viral exanthem
-Children with shortened erythrocyte life span → could lead to transient ________ crisis
-Immunocompromised children → could lead to severe ________
fever, malar rash, 2-5, symmetric, reticulated, 1-4
Erythema Infectiosum: Symptoms
-Prodromal period (low grade ______, malaise, headache, and myalgias)
-Erythematous _____ _____ “slapped cheek” that appears __-__ days after prodromal period
-Erythematous __________, maculopapular, truncal rash described as lacy and _____________
Presents __-__ days after malar rash
Lasts on average 11 days
Can wax and wane

clinical, antibodies, without, transfusions, pregnant, hydrops
Erythema Infectiosum: Diagnosis and Treatment
-Diagnosis
_________ (classic presentation in immunocompetent children)
Atypical presentation or significant risk factors calls for Parvovirus B12 IgM and IgG __________ test and CBC
-Treatment
Typically resolves __________ complications
Supportive care
____________ if aplastic crisis or severe anemia
-Keep away from _________ women due to risk of fetal anemia and _______ fetalis
Coxsackievirus, 5, GI
Hand Foot Mouth Disease: Background
-Etiology → _____________ or enterovirus
-Epidemiology
Infants and children (<_ y/o most common)
Can occur in older children and adults (rare)
Shed through respiratory and __ tract
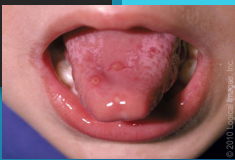
fever, tongue, mucosa, ulcers, red, hand, feet, macular
Hand Food Mouth Disease: Symptoms
-Low grade _____ (< 101), not always present
-Oral lesions (painful)
_______ and buccal ________ are the most common locations
Erythematous macules → vesicles → _______ with greyish-yellow base and ____ rim
-Skin lesions
_____ and ______ are most common. Can also see on buttocks, upper thighs, and arms
______, maculopapular, vesicular, or mix
clinical, self limiting, hydration
Hand Foot Mouth Disease: Diagnosis and Treatment
-Diagnosis → _______
If necessary, throat/stool/vesicle culture or PCR can be performed
-Treatment → mild and ____ _________
Supportive care (__________, pain relief)
Paramyxovirus, 8-12, conjunctivitis, koplik, fever, rash, hairline, downward
Measles: Background
-Etiology → ________________
-Phases
(1) Incubation → __-___ days from exposure to onset of symptoms
(2) Prodromal → cough, coryza, _____________, ______ spots
(3) Exanthematous → high _____ (104-105), macular ____ beginning on head/_________ and progresses _________ over 24 hours
(4) Recovery
-Koplik spots → small, bluish white lesions with a red halo that appear inside the mouth, typically on the inner lining of the cheeks opposite the molars

IgM, 1-2, PCR, before, supportive, vitamin A, otitis media, 5
Measles: Diagnosis, Treatment, and Complications
-Diagnosis
___ antibodies that appear _-_ days after rash and last for _-_ months
Reverse transcriptase ___ → detects measles RNA up to 5 days ______ symptoms
-Treatment
_________ care (resolves within 7-10 days)
High dose ________ _ in infants
Prevent with MMR vaccine
-Complications
_______ _______ is MC
Pneumonia
Myocarditis
Encephalitis
-High risk individuals are immunocompromised and children < _ y/o
Togavirus, lymphadenopathy, maculopapular, face, body, soft palate, IgM, unborn fetuses
Rubella (German Measles)
-Etiology → __________ family
-Symptoms
Mild prodromal phase (may go unnoticed)
Postauricular, posterior cervical, occipital _____________
Erythematous, _____________ rash that begins on ____ and spread to ____. Lasts about 3 days
Forscheimer spots → rose colored spots on ____ _______
-Diagnosis
___ antibodies (positive 5 days after symptoms onset)
-Treatment
Supportive care
MMR vaccine for prevention
-Complications
Greatest risk to ____ _________ due to congenital rubella syndrome

Varicella zoster, fever, pruritic, trunk, head, extremities, papules, vesicles, crusts, different
Varicella: Background and Symptoms
-Etiology → ________ _______ virus
-Symptoms
Prodromal period (_____, malaise, anorexia)
Rash (_______) → starts on the _____, followed by ____/face then extremities
Small red _________ → nonumbilicated, oval, “teardrop” _________ on erythematous base → ulcerates → _______ → heals
New crop of lesions for 3-4 days (lesions in __________ stages of healing)

PCR, supportive, oral, IV
Varicella (Chickenpox): Diagnosis and Treatment
-Diagnosis → clinical, ____ is the method of choice
-Treatment
Children < 12 y/o → _______ measures (not including neonates)
High risk for complications (immunocompetent) → ____ antiviral
High risk for complications (immunocompromised) → __ antiviral
-Vaccine is available
herald, clearing, thigh, torso, oval, macules, Christmas tree
Pityriasis Rosea
-Etiology → viral
-Epidemiology → peak incidence in adolescence
-Symptoms
______ patch → solitary, 2-5 cm, pink, oval patch with central _________ usually on the trunk or proximal ______
Generalized rash → follows herald patch in 1-2 weeks, occurs on ______ and proximal extremities, 0.5-2 cm _____ to oblong ________ that are red or tan with fine scale
“__________ ______ pattern”
-Treatment → benign, self limited

sebum, Malassezia, scalp, eyebrows, cradle cap, first, 1, thick, crusting
Seborrheic Dermatitis: Background and Infant Presentation
-Common, chronic inflammatory disease accompanied by overproduction of _____
-Pathogenesis
Unknown but thought to be an abnormal inflammatory response to _________ species in sebum rich areas
Common areas affected are _____, _________, eyelids, nasolabial folds, external auditory canal, and posterior auricular folds
-Infants (______ ___)
Begins during ______ month of life
Resolves around _ year
Most often on vertex of scalp
______, greasy/waxy, yellow-white scaling and __________ of scalp
Asymptomatic

dandruff, scaling, oil, ketoconazole, shampoo
Seborrheic Dermatitis: Presentation, Diagnosis, Treatment
-Adolescents (________)
Scalp most often affected
Fine, white, dry ________ of the scalp
May have minor itching
-Diagnosis → clinical
-Treatment
Frequent shampooing can help remove scale
Cradle cap → can apply ____ (mineral or olive), allow to sit for a few minutes then gently brush and shampoo
Adolescents → ____________, selenium sulfate, or salicylic acid _________

pruritic, stress, allergens, early, 5
Eczema/Atopic Dermatitis: Background
-Chronic, _________, relapsing inflammatory skin condition
-Pathogenesis
Genetics, immunologic abnormalities, impaired skin barrier function, and environmental interactions
-Triggers
_____/anxiety, climate, irritants/_________, and sweating
-Epidemiology
Often starts in ______ infancy, most cases before _ y/o
erythematous, ill, scale, allergic, face, extremities, antecubital, neck
Eczema/Atopic Dermatitis: Symptoms
-Symptoms
____________ papules/plaques with ____-defined borders and overlying _____ or hyperkeratosis
Pruritic
May weep
Skin fissures
Excoriations
-Tend to have other _______ diseases like asthma and allergic rhinitis
-Location of Rash
Infants → _____, scalp, extensor surfaces of ___________
Older children → __________ and popliteal fossae, head, ____

hydration, corticosteroid, tacrolimus, triggers
Eczema/Atopic Dermatitis: Treatment
-Skin ____________ → fragrance free ointment or cream, avoid lotions
-Decrease itching/inflammation/flares → ____________ ointment with the lowest potency effective
-Immunomodulating topicals (________) → second line in patients unresponsive to other treatments
-Avoid ________