Preventing & Caring for Exertional Heat Stroke
1/47
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
48 Terms
Essential Emergency Equipment
Automated External Defibrillator (AED)
Glucometer
Rectal thermometer
150 gallon tub for cold water immersion
Unlimited supply of ice and water
Easy up tent
Cell phone
Expendable first aid supplies
Documented and rehearsed emergency action plan
Wet bulb globe temperature (WGBT) device
Prevention: Prescreen Athletes to assess for history of heat illness of presence of risk factors of heat illness
Level of evidence: C
History of EHI
Inadequate heat acclimatization
Low fitness level
Overweight or obese
Inadequate hydration
Poor sleep hygiene
Fever
Stomach illness
Highly motivated / ultra-competitive
Pre-pubescent
Prevention: #2
Strength of Recommendation: B
Allow athletes to acclimate to the heat over the course of 7-14 days by gradually increasing intensity and duration of exercise
Day 1-5: no more than 1 practice per day, no more than 3 hours per day (total), 1 hour max walk through is allowed but then need 3 hour recovery period before practice
Days 1-2 Equipment: helmet only
Days 3-5 Equipment: helmet and shoulder pads -> contact with blocking sleds and dummies
Day 6 Equipment: ALL equipment allowed -> 100% live contact
Days 6-14: double day practices are allowed, followed by a single practice day, 2 practices -> rest day -> 2 practices, 2 practice -> can’t exceed 3 hours (in one practice, cant exceed 5 hours total), 3 hour recovery in cool environment between
Prevention: #3
Strength of Recommendation: B
Ensure fluids are available and easily accessible before, during, and after practice. Encourage Rehydration
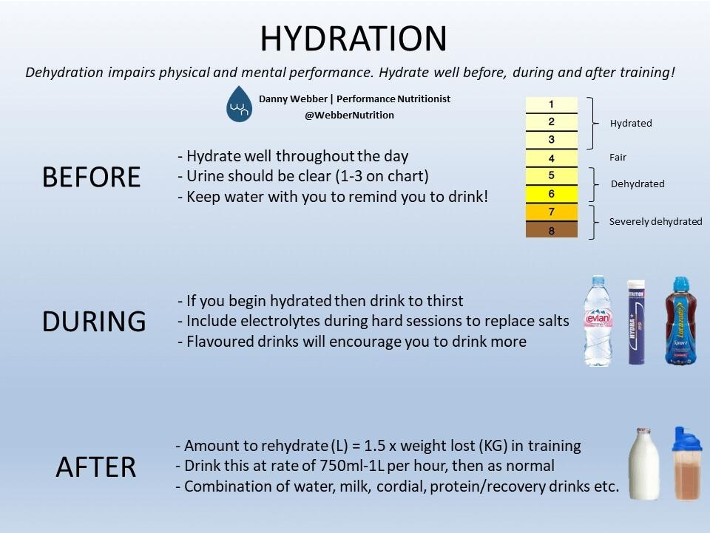
Prevention: Proper hydration
Begin hydrated:
2-3 hrs prior to activity 17-20 fl oz
20 min prior 7-10 fl oz
40 min to restore plasma volume/electrolytes
During Activity
7-10 0z every 10-12 minutes
Prevention: Post activity rehydration
Rehydration should occur within 2 hrs post exercise to assure optimal rehydration. Post exercise rehydration should be 150% of body mass loss during exercise.
Pre exercise wt (kg) - post exercise wt (kg) x 1.5 = Fluid needs for replacement per ACSM guidelines
For every 1 kg (2.2 lb) loss, additional 1 L of fluid needed
Fluid Replacement After Exercise | |
BM loss | Fluid Needed |
0.5 kg (1.1 lbs) | 0.5 L |
1 kg (2.2 lbs) | 1 L |
1.5 kg (3.3 lbs) | 1.5 L |
2 kg (4.4 lbs) | 2 L |
2.5 kg (5.5 lbs) | 2.5 L |
3 kg (6.6lbs) | 3 L |
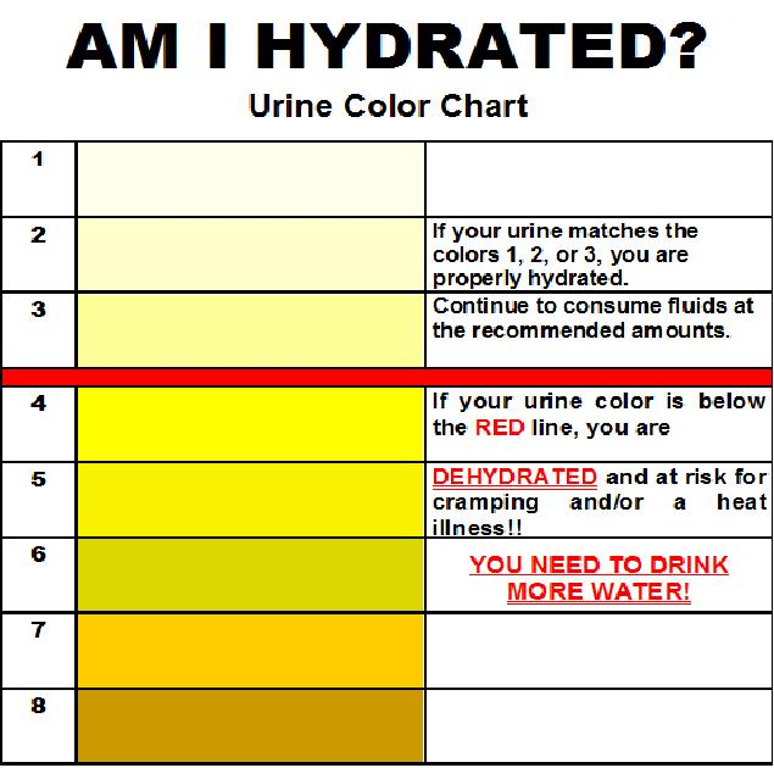
Prevention: Clinical hydration measurments
Urine specific gravity - ration between density of urine and density of water
Euhydration < or equal to 1.020
Dehydration > or equal to 1.020
Measurement
Urine reagent strip - cheap, not as sensitive in hypo-hydrated state
Refractometer - preferred
Clinical Hydration measurements (Body Mass & Urine color)
Body mass
50-70% of body is water
May lose 5% in one session
Pre/post exercise
Urine Color
Normal: light yellow
Severe: brownish green
Activity Modification (Prevention: #4)
Adjust practice times, sessions, and equipment according to environmental conditions and fitness level
Strength of recommendation: C
WBGT Index
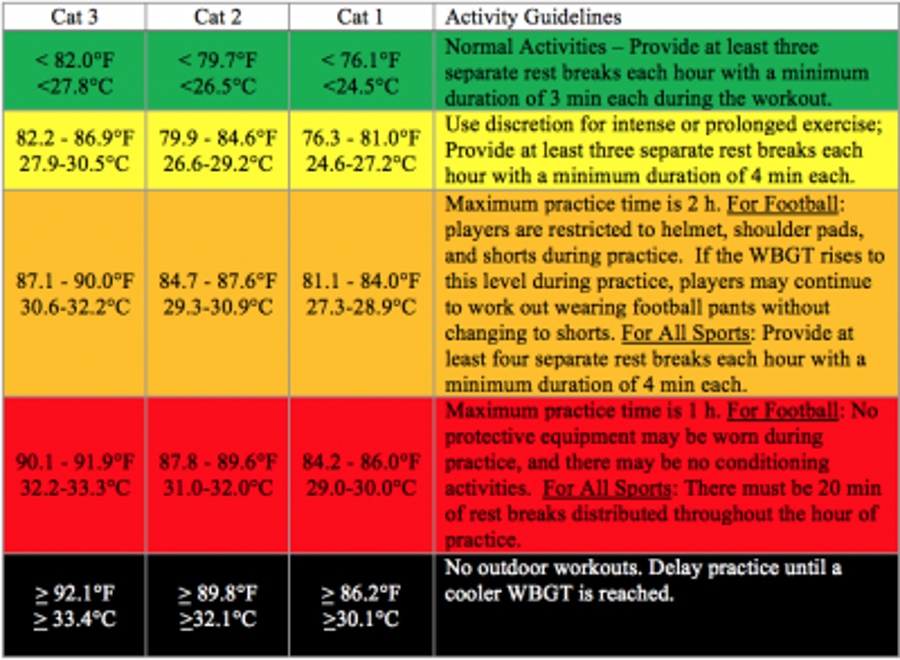
WBGT (overview)
Utilizes ambient temperature, relative humidity, wind, and solar radiation from the sun to get a composite value that can be used when monitoring environmental conditions during exercise in the heat.
WGBT = 0.7TW+0.2TG+0.1TD
Tw is the wet bulb temperature, which indicates humidity
TG is the globe temperature, which indicated radiant heat
TD is the ambient air (dry) temperature
Nutrition
Electrolyte consumption
Lightly salty food
Watery foods - fruits
Avoid caffeine & alcohol
Sleep guidelines
Encourage 6-8 hrs of sleep each night in a cool environment
Sleep deprivation has negative impact on acclimation to heat
Recognition Heat Stroke : Types
Classic
Under heat wave conditions/illness of unfit-sick
Exertional
illness of young and fit
Severe hyperpyrexia (>104 degrees F)
1 F = 7% metabolic increase
Recognition HS: Key Points
Core body temperature >104-105 degrees F
Measured via rectal probe or gastrointestinal temp immediately following collapse
(Strength of recommendation: B)
CNS dysfunction
Mental status change
Dizziness
Collapse
Irritability
Irrational Behavior
Confusion
(Strength of recommendation: B)
Recognition HS : S/SX
Disorientation
Staggering
Seizures
LOC - most will have lucid interval first
Coma
Hot, dry or wet skin
Dehydration
Tachycardia (100-120 bpm)
Hypotension
Hyperventilation (shallow & rapid)
Vomiting
Diarrhea
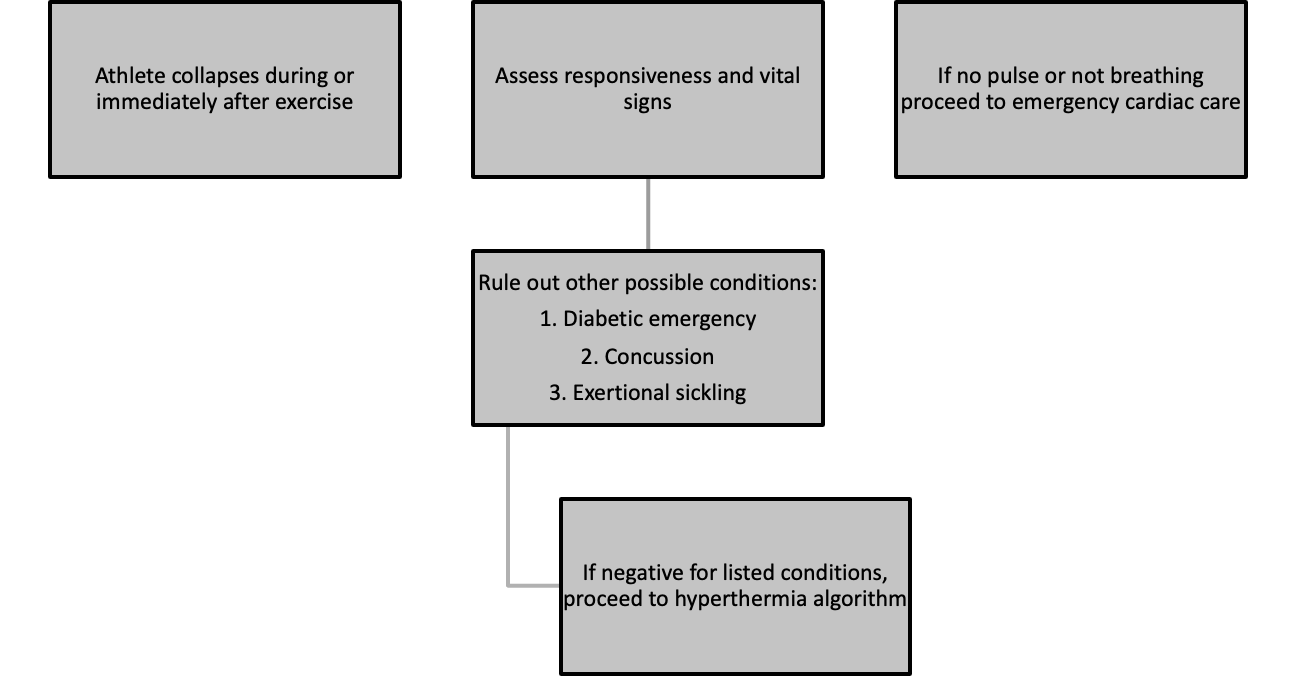
ALL emergency assessments begin the same
Measuring Core Body Temperature
Rectal temperature is the GOLD standard
Other measurements are shown to be inaccurate and unreliable in heat stress patients
Oral gets worse as a predictor as they get hotter
No correlation between rectal temp and oral temp, axillary temp, tympanic temp or temporal temp
No correction factor
Rectal Temp
Assessing rectal temperature
flexible thermistor
Inserted 10 cm past anal sphincter (lift up buttocks)
Put tape at 12 cm mark to hold on to
Danger zone - 105 degrees >
5-7 minute window within 30 minutes of collapse to get patient below 105 degrees F
Athlete should be cooled to 102 degrees within first 30 minutes after collapse
Taking a Rectal Temperature
1.Place patient in a side-lying position with top knee bent
2.Place towel over hips
3.Wash/sanitize hands, don gloves
4.Lower pants/underwear to below the gluteal fold
5.Prepare the thermometer (have correct thermometer, clean instrument with alcohol)
6.Apply thermometer sleeve and lubricant
7.Lift top buttock to visualize rectum
8.Insert thermometer into the rectum 1.5 inches (3.5 cm)
9.If using a thermistor thermometer, insert flexible probe 4-6 inches (10-15 cm) past the anal sphincter into the rectum
10. Wait for digital reading
11. Remove the thermometer; dispose of the sleeve; clean the thermometer with alcohol
12. If using a thermistor thermometer, the measuring aspect may remain in the patient’s rectum until cooling temperature of 102°F has been reached
Why do people die? HS
No care: no AT present
Inappropriate care: failure to assess core temperature accurately and therefore make wrong treatment decision
Inadequate cooling methods: cold water immersion is gold standard
Ambulance delay: COOL first, TRANSPORT second
Complications due to delayed treatment of EHS
Survival without complications
cooling 0-30 min following collapse
Long term complications
30+ min following collapse
Permanent complications
Death
Treatment: key points
1.Cold-water immersion until core body temperature is ≤102°F
–Strength of recommendation A
2.Monitor other vitals
–Strength of recommendation B
3.After body temperature is ≤102°F transport to the hospital and monitor blood work for elevated enzyme levels
–Strength of recommendation B
4.Return to play should involve a gradual introduction and consequent combination of exercise, heat, and protective equipment under the supervision of a medical professional (pending normal blood work and physician clearance).
–Strength of recommendation C
Cooling methods for EHS
Aggressive cooling in cold water immersion bath within 10 minutes of collapse
takes 90 minutes to cool with peripheral methods
Water temp should be around 40F
stir water w/ paddle to avoid developing a thermopane
Use sheet under arms to support patient in case LOC
Keep flexible thermistor inserted during bath to monitor temp
Remove when reach 102F
Cold saline IV is second best tool but not available until in ER
Cooling Rates
Cool 4x faster in water than in air
Decrease 1F every 3 minutes average over 12 minutes
Cooling during 1st 6 min is slower than faster in next 6 mins
Normal thermic patient will increase temp during first 20 mins
EHS patient will decrease temp
Normal thermic patient will shiver and have vasoconstriction
EHS patient - hypothalamus overrides and causes little vasoconstriction and no shivering documented
Cardiovascular shock only a concern in delayed care situations or passive heat stroke in the elderly
IF no rectal thermometer
•Have a documented emergency action plan
•Know the KEY signs/symptoms
–Elevated core temperature
–CNS changes
•Remove from the heat
•Remove equipment and sweaty clothing
•Cool down entire body
–Iced towels rotated every 3-5 minutes
–Cold water immersion 15 minutes
• Take caution as patient will likely lose consciousness
• Call EMS
-Be aware that EMS is not currently trained in assessing rectal temperature nor do that have rapid cooling methods
Comparison of common non-trauma causes of on-filed collapse
SCT Sickling | Cardiac | Heat Stroke |
Weakness > pain | No cramping | Fuzzy thinking |
Slumps to ground | Falls suddenly | Bizarre behavior |
Can talk at first | Unconscious | Incoherent |
Muscles “normal” | Limp or seizing | Can become unconscious |
Temp < 103 | Temp irrelevant | Temp >104 |
Can occur early | No warning | Usually occurs late |
Return to Play
Asymptomatic
Achieve and maintain full hydration
Physician clearance
normal lab tests
Resolution of any underlying conditions
ID predisposing factors
Gradual return = re-acclimatization
Thermoregulation 101
Core Body temp
S = M ± R ± K ± Cv – E
S = amount of stored heat
M = metabolic heat production
R = heat gained or lost by radiation
K = heat gained or lost by conduction
Cv = heat gained or lost by convection
E = heat gained or lost by evaporation
Thermoregulation: definitions
Radiation – energy is transferred to or from an object or body via electromagnetic radiation from higher to lower energy surfaces (we absorb radiant heat from the sun)
Conduction – heat transfers from warmer to cooler objects through direct physical contact (ice bags)
Convection – heat transfers to or from the body to surrounding moving fluid or air (moving air from a fan, wind, moving water)
Evaporation – heat transfers via the vaporization of sweat and is the most efficient means of heat loss
Sweating
Begins 1-2 sec. after exercise begins
Reaches equilibrium in direct relation to exercise load in 30 mins
Adult sweat output of 1 - 2 liters / hour
Peak of 3 liters / hour
2-3% loss of body weight impairs function
Inter-Association Task Force for Preseason Secondary School Athletics Participants
Initial 14 consecutive days of preseason practice
1 day of complete rest every 6 days
•Need for heat exposure every 4 days
•Smaller rise in core temperature a result of:
–increased stroke volume
–extracellular fluid volume expansion
–diminished sweat [Na+]
–increased sweat volume
Heat Syncope
Typically occurs first 5 days of acclimatization before blood volume expands
Dehydration
Peripheral vasodilation
Postural pooling of blood
Dizziness
Lightheadedness
Fainting
Fatigue
Tunnel vision
Pale or sweaty skin
Decreased pulse rate
normal core body temp <104 F
TX: elevate feet in supine, rehydrate
Heat Exhaustion
Caused by inadequate CV response to circulatory stresses caused by heat
Slow, progressive, Peripheral vascular collapse
Predisposing Factors
young, old, hypertensive
Heavy sweating, vomiting, dehydration, sodium loss, energy depletion
Those at risk : Heat Exhaustion
•Exercising in hot and humid environment (air temp > 33°C, 91.4F)
•Inadequate fluid intake before or during exercise resulting in dehydration
•Inappropriate work to rest ratios with too much work compared to rest breaks
•Body mass index > 27 kg/m
Heat Exhaustion S/SX
•Headache, fatigue
•Dizziness, nausea
•profuse sweating
•Pale, cool, clammy skin
•Rapid, weak pulse
•Rapid shallow respirations
•BP decreased
•Temperature 97-103.9F
•Dehydration
•Lightheadedness
•Syncope
•Anorexia
•Diarrhea, intestinal cramps, urge to defecate
•Decreased urine output
•Persistent cramps
•Chills
Heat Exhaustion : Treatment
•Treatment
–move to cool environment
•Inside, shade, fans, AC
–if temp elevated apply cool towels or sponge
•Keep cooler of towels in ice bath on the field
•Remove wet clothing, helmets/hats, socks, shoes
–monitor vital signs
–give cool fluids if conscious and alert
–Will get better in 5-10 minutes
–No RTP for at least 24 hours
(Gradually increase intensity and volume of exercise)
Hyponatremia
• Core body temp <104F
• Excessive water consumption and/or decreased Na+ intake
• Serum Na+ < 130 mmol/l
• Activity > 4 hrs, rare….
Signs and Symptoms
•. Disoriented, progressive headache, nausea, vomiting, swelling of extremities
• Leading to Cerebral edema, pulmonary edema, death
Prevention
•. Fluid intake with Na+
Sickle Cell trait
Sickle cell trait is the inheritance of one gene for sickle hemoglobin Hb S and one for normal hemoglobin Hb A. During intense or extensive exertion, the sickle hemoglobin can change the shape of red cells from round to quarter-moon, or “sickle.” This change, exertional sickling, can pose a grave risk for some athletes. In the past seven years, exertional sickling has killed nine athletes, ages 12 through 19.
5 major concerns for athletes with SCT
•Genetic counseling
•Splenic infarction at altitude
•Bleeding in the urine
•Inability to concentrate urine
•Exertional rhabdomyolsis
What happens SCT
• Sickle cells can accumulate in the bloodstream during intense exercise
• Ischemic rhabdomyolysis
– Rapid breakdown of muscles starved of blood
– Blood vessels collapse due to “log jam” of sickled cells
Sickle Cell trait & Exercise : Overview
Each cell has ~ 40% Hgb S and ~ 60% normal Hgb A
Strenuous exertion causes sickling of some cells because of:
Hypoxemia
Hyperthermia (due to increased muscle heat)
Metabolic acidosis
Dehydration of red cells (increases concentration of Hgb S)
Sickle cells log jam and stop blood supply
Ischemic rapid muscle breakdown = explosive rhabdomyolsis
Sickle Cell trait & exercise: definitions
Acute Ischemic rhabdomyolysis: the rapid breakdown of muscle tissue starved of blood
Acute Rhabdomyolysis: a serious and potentially fatal condition involving the breakdown of skeletal muscle fibers resulting in the release of muscle fiber contents into the circulation
Exertional rhabdomyolysis: muscle breakdown triggered by physical activity
Exertional sickling: hemoglobin [red blood cell] sickling due to intense or sustained physical exertion
Hyperthermia: body temperature elevated above the normal range
Hypoxemia: decreased oxygen content of arterial blood
Ischemia: a deficiency of blood flow to tissue
Metabolic acidosis: a condition in which the pH of the blood is too acidic because of the production of certain types of acids
Sickling Collapse
•Typical events leading to a collapse:
– High altitude running
– Sprints or “gassers” that occur early in practice
•Think of the typical practice…”work hard and then kill ‘em at the end.”
– Sickling can occur as quickly as during 2-3 minutes of sprinting
– Typically occurs early in season or during preseason
– Can quickly increase to grave levels
– The harder and faster the athlete runs the earlier and greater the sickling occurs
– Increased likelihood in the heat…why?
Telltale sigs: Heat cramps vs Sickling
•Heat Cramps
– Muscle twinges
– Excruciating pain with cramps
– LOF is different – hobble to a halt with “locked up” muscles
– Writhe and yell in pain with rock hard muscles
•Sickling
– None
– Not as painful
– LOF – slumps to the ground with overall muscle weakness
– Lie fairly still with muscles that look and feel normal
Recommendations for Sickle cell trait Athletes
• Should not be disqualified – modifications and precautions should be in place
– Build up slowly in training progression, longer rest/recovery periods
– Participate in preseason strength and conditioning but exclude from mile runs, serial sprints, etc.
– Cessation of activity with onset of symptoms
– Year-round periodization strength and conditioning program that is athlete/sport specific
– Must have adequate rest/recovery if participating in high speed sprints and/or interval training
• Ambient heat stress, dehydration, asthma, illness, and altitude predispose the athlete with sickle trait to an onset of crisis in physical exertion.
– Adjust work/rest cycles for environmental heat stress
– Emphasize hydration
– Control asthma
– No workout if an athlete with sickle trait is ill
– Watch closely the athlete with sickle cell trait who is new to altitude. Modify training and have supplemental oxygen available for competitions
Sickle Collapse - MEDICAL EMERGENCY
1.Check vital signs.
2.Administer high-flow oxygen, 15 lpm (if available), with a non-rebreather face mask.
3.Cool the athlete, if necessary.
4.If the athlete is obtunded or as vital signs decline, call 911, attach an AED, start an IV, and get the athlete to the hospital fast.
5.Tell the doctors to expect explosive rhabdomyolysis and grave metabolic complications.
6.Proactively prepare by having an Emergency Action Plan and appropriate emergency equipment for all practices and competitions.
Acute Exertional Rhabdomylosis
• Sudden catabolic destruction and degeneration of skeletal muscle (myoglobin and enzyme leakage into vascular system)
• Occurs during intense exercise in heat and humidity resulting in:
– gradual muscle weakness, swelling, pain, dark urine, renal dysfunction
– severe case = sudden collapse, renal failure and death
• Associated with individuals that have sickle cell trait
• Emergent Referral