cardiac muscle contraction and contractility
1/32
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
33 Terms
three types of muscle
skeletal, cardiac, smooth
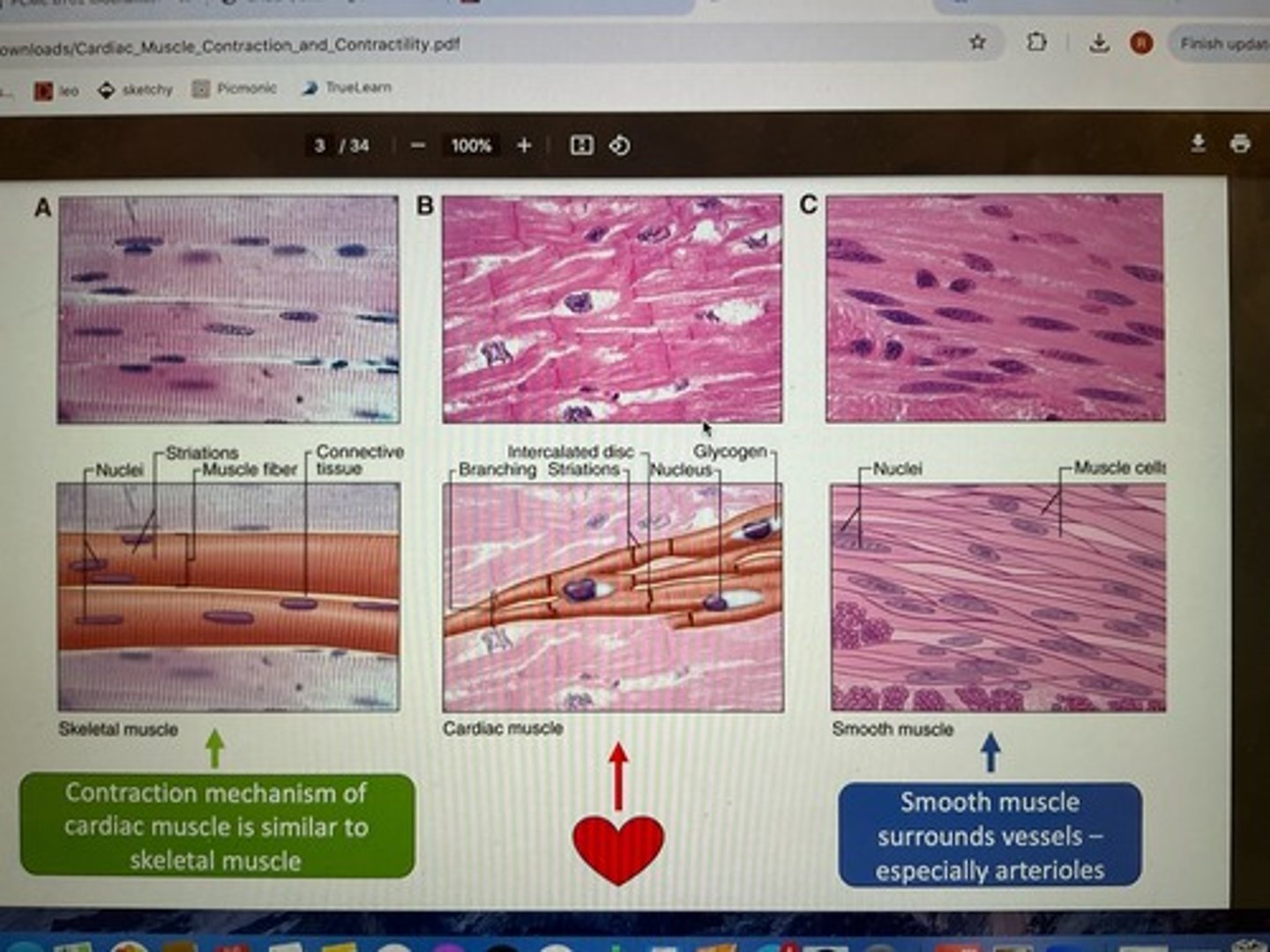
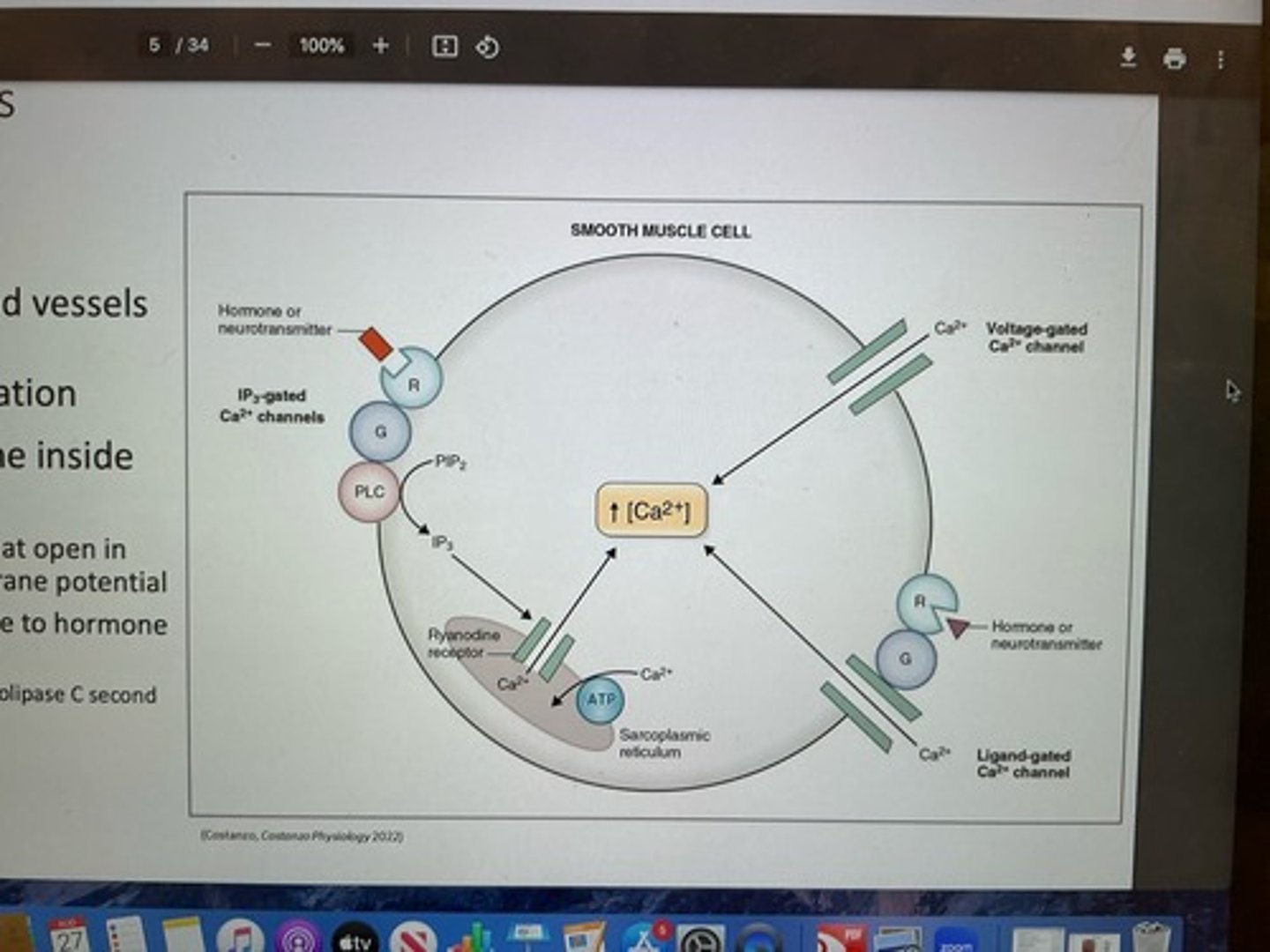
smooth muscle
-regulates vessel diameter
-surrounds vessels (arterioles) and facilitate vasoconstriction and vasodilation
-Ca++ made available to inside of cell: VG Ca++ channels that open in response to changes in membrane potential and channels that open in response to hormone or neurotransmitter (IP3-gated (phospholipids C second messenger system) and ligand-gated Ca++ channels)
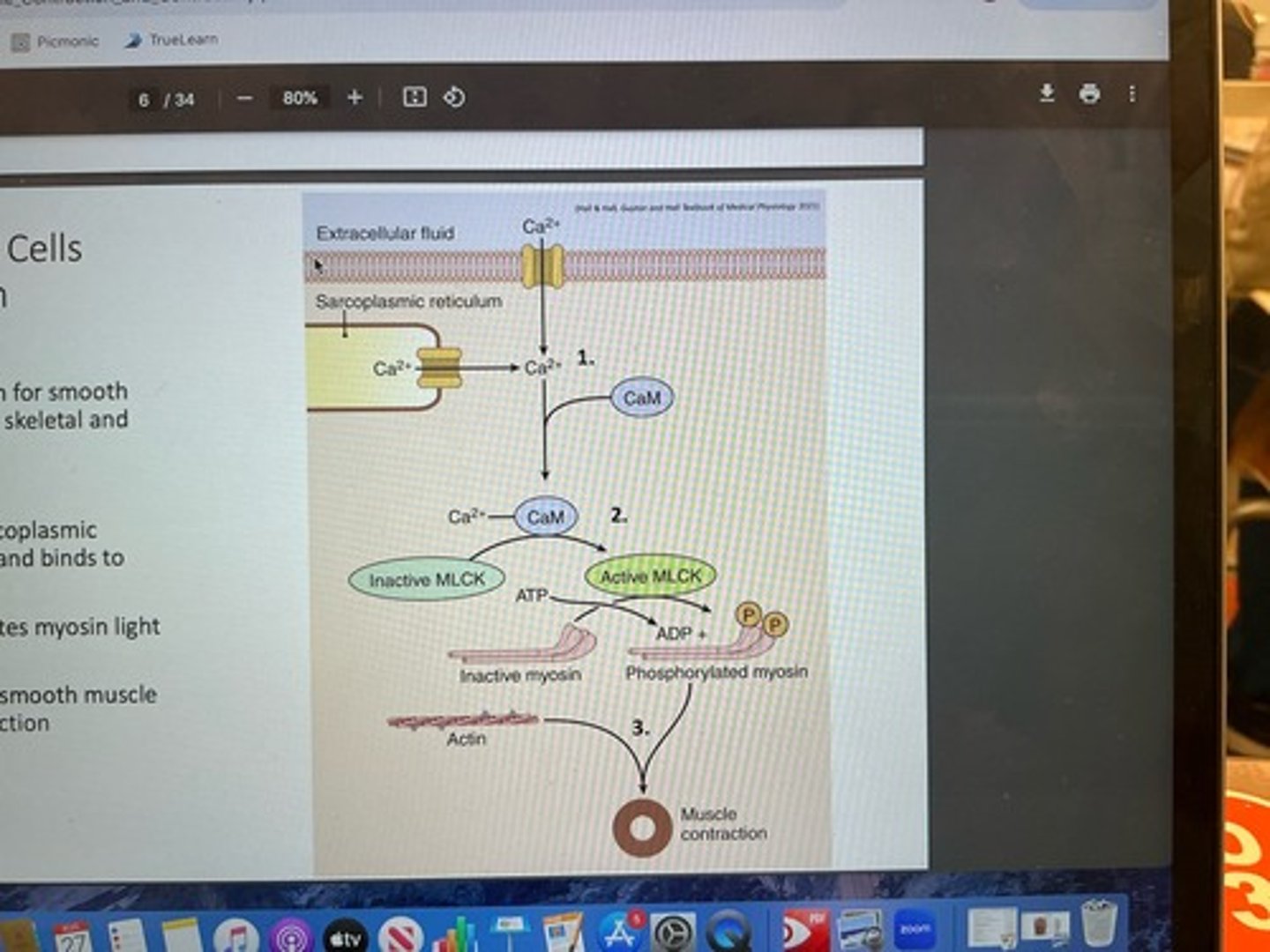
contraction mechanism for smooth muscle
1. Ca++ enters from sarcoplasmic reticulum or from ECF and binds to calmodulin (CaM)
2. Ca++ + calmodulin activates myosin light chain kinase (MLCK)
3. MLCK activation activation causes smooth muscle contraction —> vasoconstriction
muscle cell —> muscle fiber
long, cylindrical, multinucleate
muscle cell plasma membrane —> sarcolemma
-specialized "dips" into cell called transverse tubules or t-tubules
- t-tubules allow action potential to run adjacent to specialization of sarcoplasmic reticulum known as terminal cisteranae
ER —> sarcoplasmic reticulum (Ca++ storage)
-terminal cistern are are specialized regions of SR that run adjacent to T-tubules of sarcolemma
-when AP occurs, it travels down t-tubules and opens channels with terminal cisternae to allow Ca++ to flood into cell
intercalated discs
-connects cardiac muscle fibers
contain: desmosomes (mechanical binding) and gap junctions (conduct AP to neighboring cells via movement of ions from fiber to fiber)
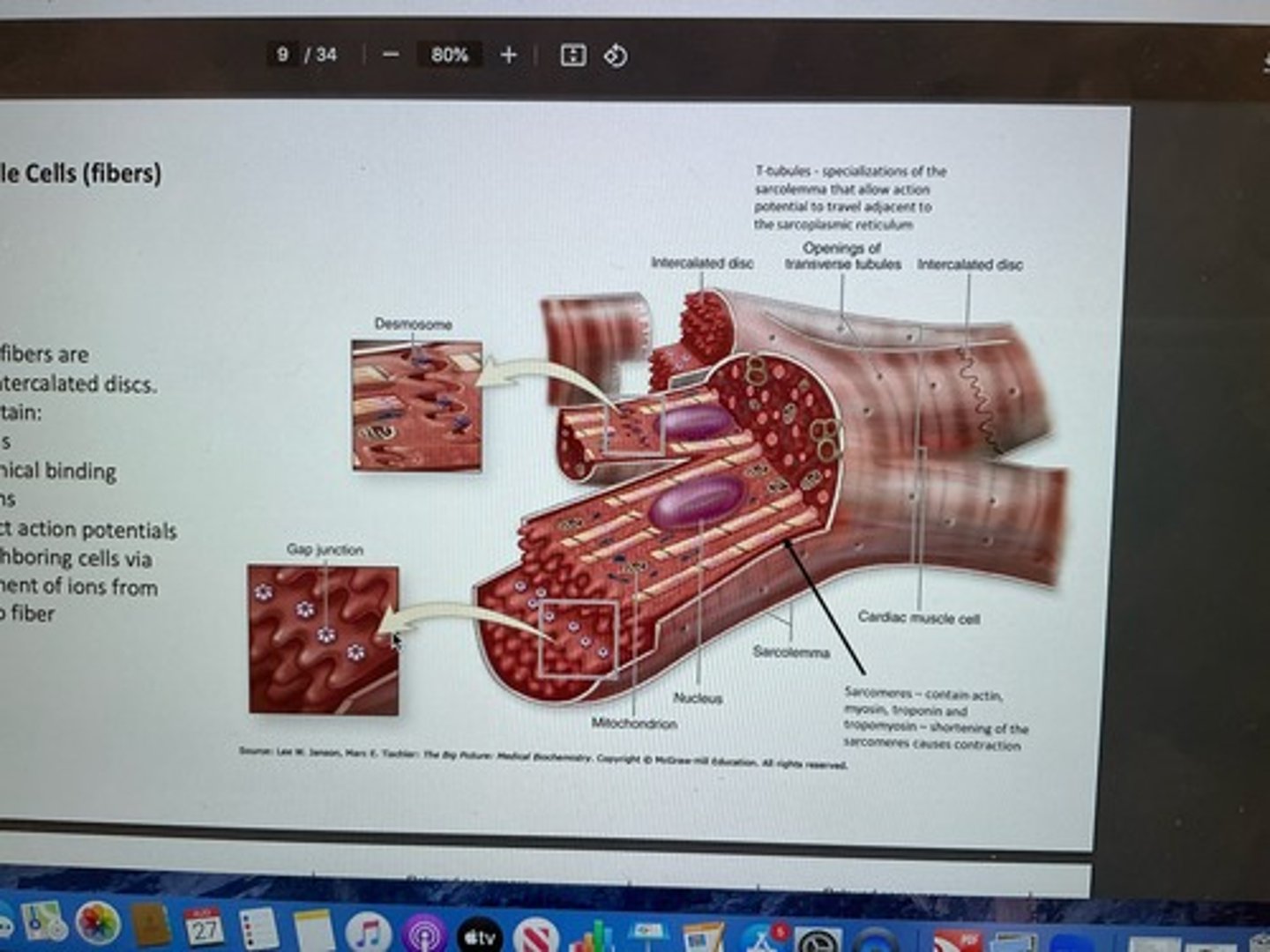
T-tubules
specializations of sarcolemma that allow AP to travel adjacent to SR
sarcomeres
contain actin, myosin, troponin, and tropomyosin
shortening causes contraction
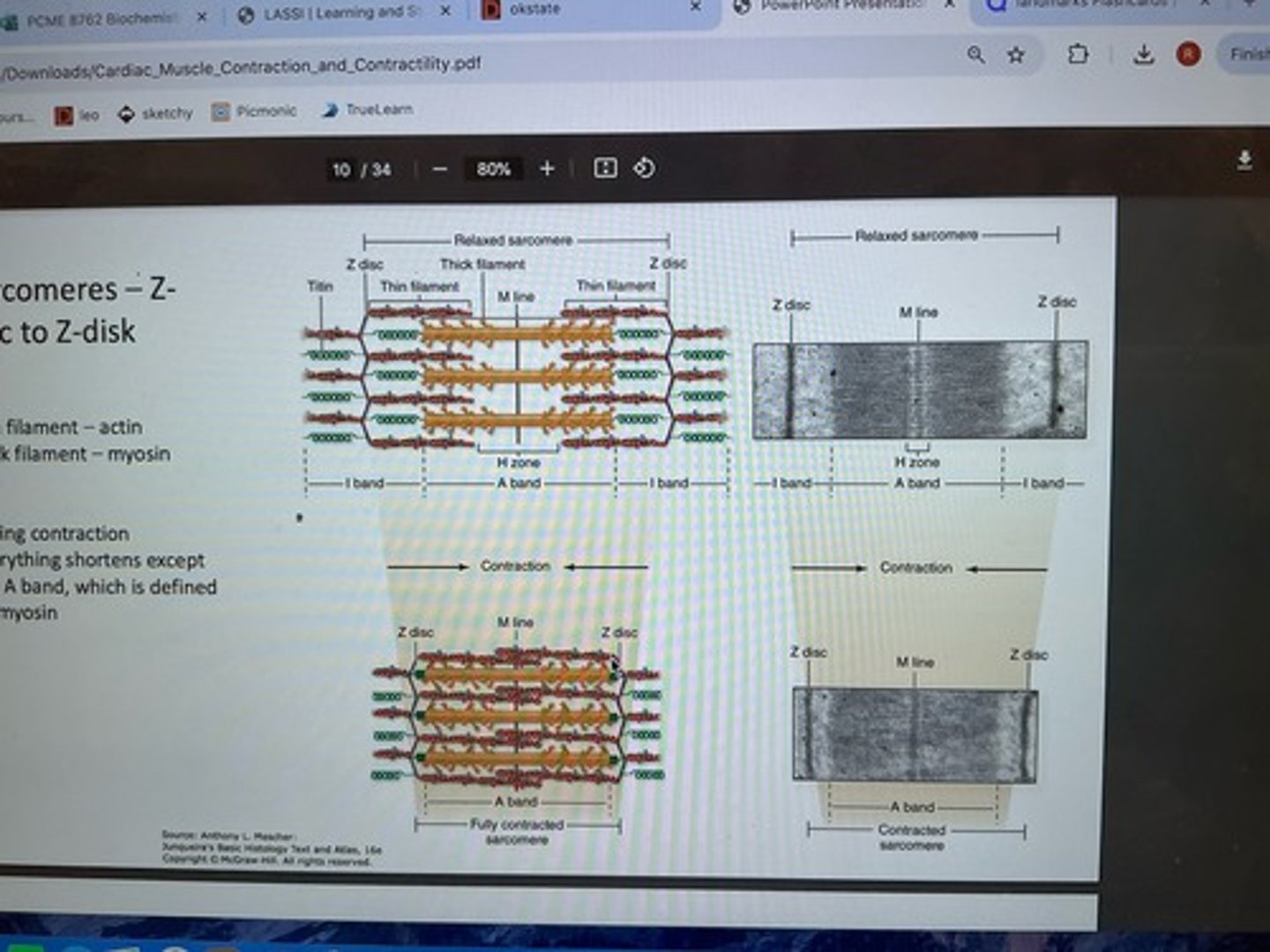
sarcomeres: Z-disc to Z-disc
thin filament: actin
thick filament: myosin
during contraction, everything shortens except A band (defined by myosin)
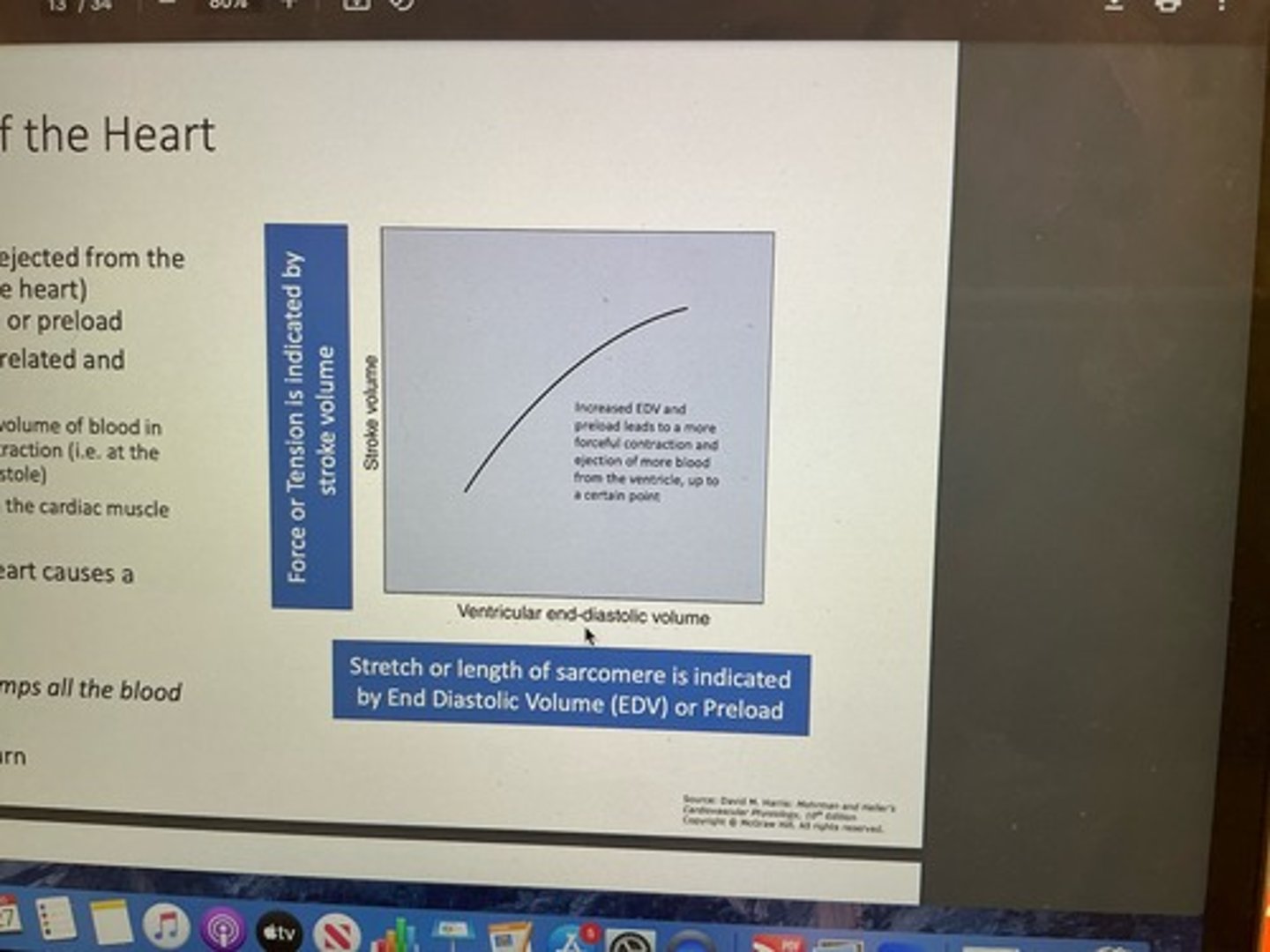
frank starling relationship
based on length-tension relationship, as end-diastolic volume increases, heart responds with increased force of contraction
length - tension relationship in cardiac muscle
force of contraction in cardiac muscle is dependent on sarcomere length
-optimal length: provides "just right amount" of overlap between actin and myosin to generate max force
-sarcomere length too short: actin is already pulled toward M-line, nowhere left to go
-sarcomere length too long: extending sarcomere has very little actin and myosin overlap
frank starling law of the heart
stroke volume (amount of blood ejected from ventricle during contraction of heart)
-EDV and preload closely related and sometimes interchanged (EDV: volume of blood in ventricle right before contraction; preload: degree of stretch in cardiac muscle)
-additional blood entering heart causes more forceful contraction
IOW cardiac output = venous return
contraction
1. auto rhythmic cells depolarize contractile cells
2. depolarization opens up L-type Ca++ channels (dihydropyridine)
3. Ca++ enters and binds to ryanodine receptors (RYR) located on SR
4. when Ca++ binds RYR receptor in SR, more Ca++ released into ICF and facilitates contraction
relaxation
1. Ca++ again is stored in SR via action of SERCA pump which is Ca++ ATPase
2. Ca++ also leaves to extracellular fluid via Na+/Ca++ exchanger (made possible by Na+/K+ ATPase)
Excitation-contraction coupling
-L-type Ca++ channels on t-tubules also known as dihydropyridine receptors or channels (VG)
-within SR, calsequestrian binds Ca++ for storage
-Phospholamban (PLN) regulates SERCA pump
Phospholamban regulates SERCA pump
-unphosphorylated PLN decreases Ca++ reuptake rate in SR
-phosphorylated PLN increases Ca++ reuptake rate in SR and increases relaxation
Ca++ used for
-before myosin can form crossbridge with actin, tropomyosin must be moved out of binding site on actin
-accomplished when Ca++ binds to troponin (complex moves tropomyosin out of way and myosin can form crossbridge for contraction)
troponin
C- Ca++ binds here
I- inhibits binding of myosin
T- tropomyosin bind site
tests available to measure cardiac-specific: Troponin T (cTNT) and Troponin I (cTNI)
phosphocreatine
source of ATP
-backup
creatine kinase facilitates transfer of phosphate from phosphocreatine to ADP to make ATP (cardiac specific: creatine kinase MB)
cardiac injury
-releases cardiac-specific isoforms of troponin (T and I) into circulation
-releases cardiac-specific isoenzyme creatine kinase (CK-MB)
isoforms or isoenzymes
variant forms of proteins/enzymes that perform similar functions in different physiological environments
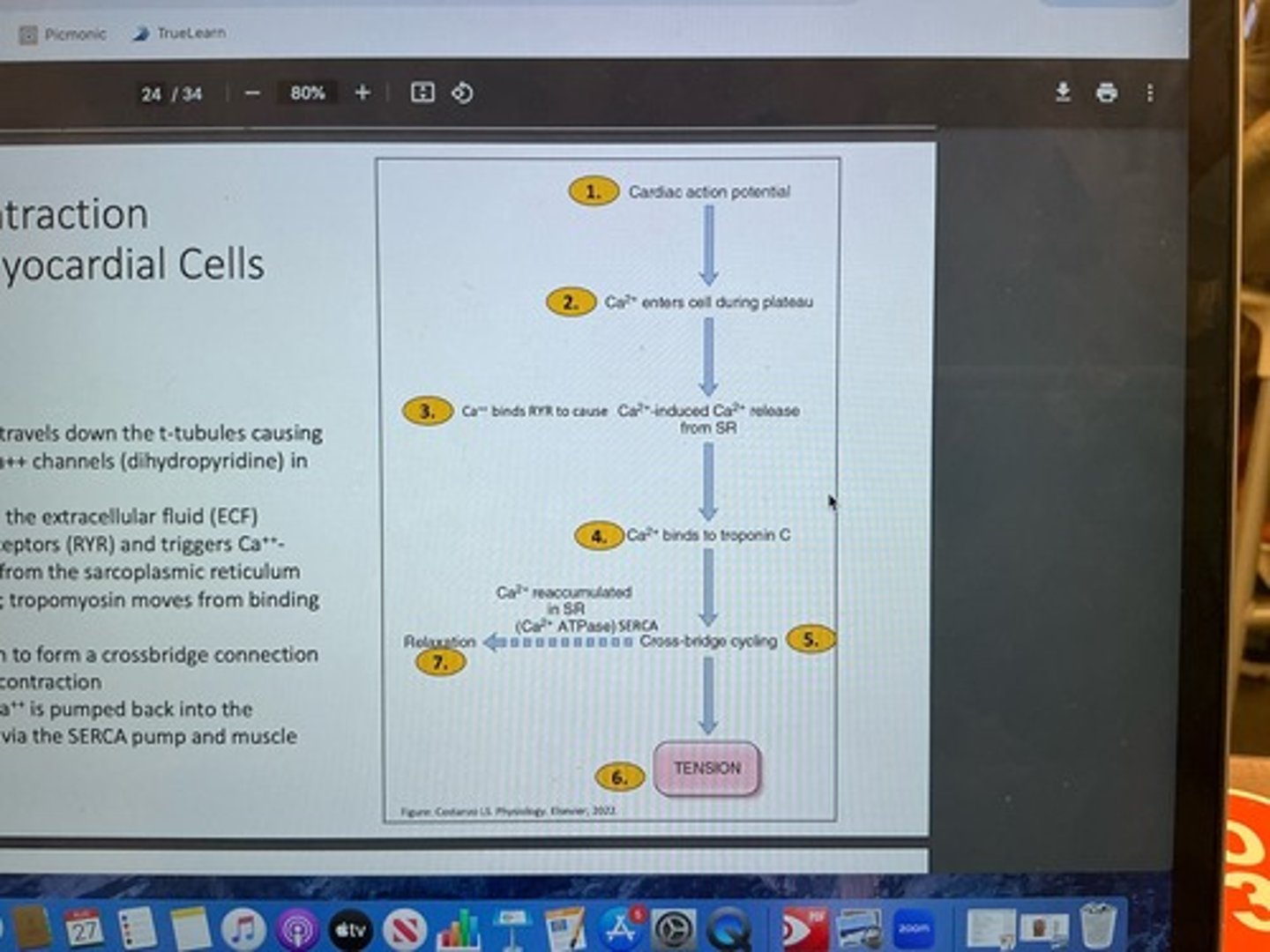
excitation-contraction coupling in myocardial cells summary
1. cardiac AP travels down t-tubules causing depolarization; L-type Ca++ channels in sarcolemma open
2. Ca++ enters cell from ECF
3. Ca++ binds ryanadine receptors (RYR) and triggers Ca++-dependent Ca++ release from SR
4. Ca++ binds to troponin C; tropomyosin moves from binding site
5. myosin can bind to actin to form crossbridge connection
6. power stroke or muscle contraction
7. after contraction, Ca++ is pumped back in to SR via SERCA pump and muscle relaxation occurs
contractility
intrinsic ability of heart to contract at given fiber length - dependent on Ca++ availability
more Ca++ = more cross bridges formed at sarcomeres = more forceful contraction
increased contractility = increased stroke volume
MAP = CO x TPR
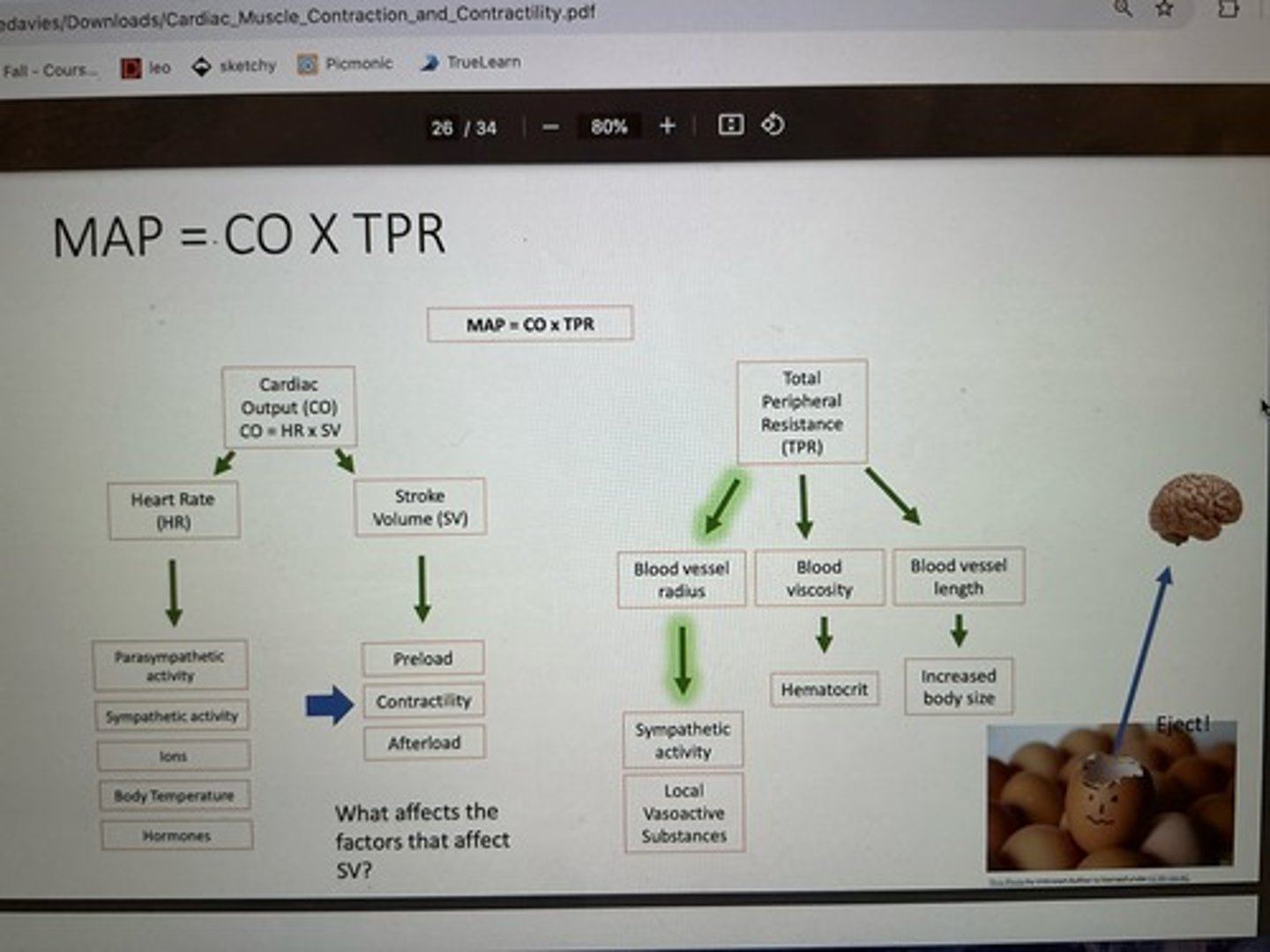
stroke volume
volume of blood ejected from ventricle during systole
3 major affectors: preload, contractility (inotropy), afterload
increased end diastolic volume = ________ stretch
increased
increased preload = ______ stretch and ______ contractility = ______ forced
increased, increased, increased
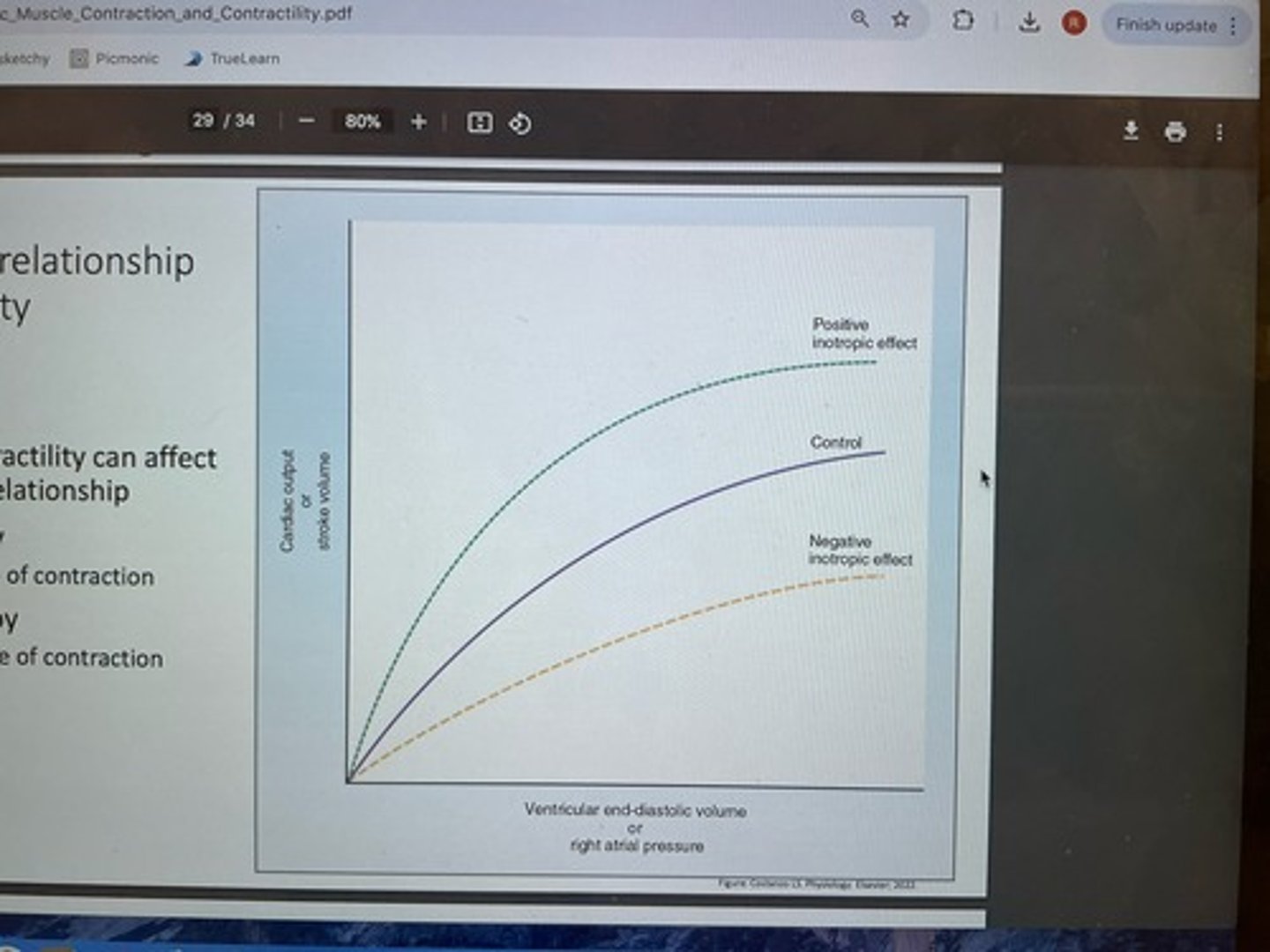
frank-starling relationship and contractility
-changes in contractility can affect frank-starling relationship
-positive inotropy (increased force of contraction)
-negative inotropy (decreased force of contraction)
positive inotropy effects
increased force of contraction - catecholamines (epi and NE) sympathetic
1. bind B1 adrenergic receptors on myocardial contractile cells
2. cAMP second messenger activated resulting in phosphorylation of
- phospholamban (phosphorylation removes regulatory effect on SERCA, SERCA can reuptake Ca++ at faster rate and is more readily available for next contraction)
- Ca++ channels (phosphorylation keeps channels open longer and result and increase in intracellular Ca++)
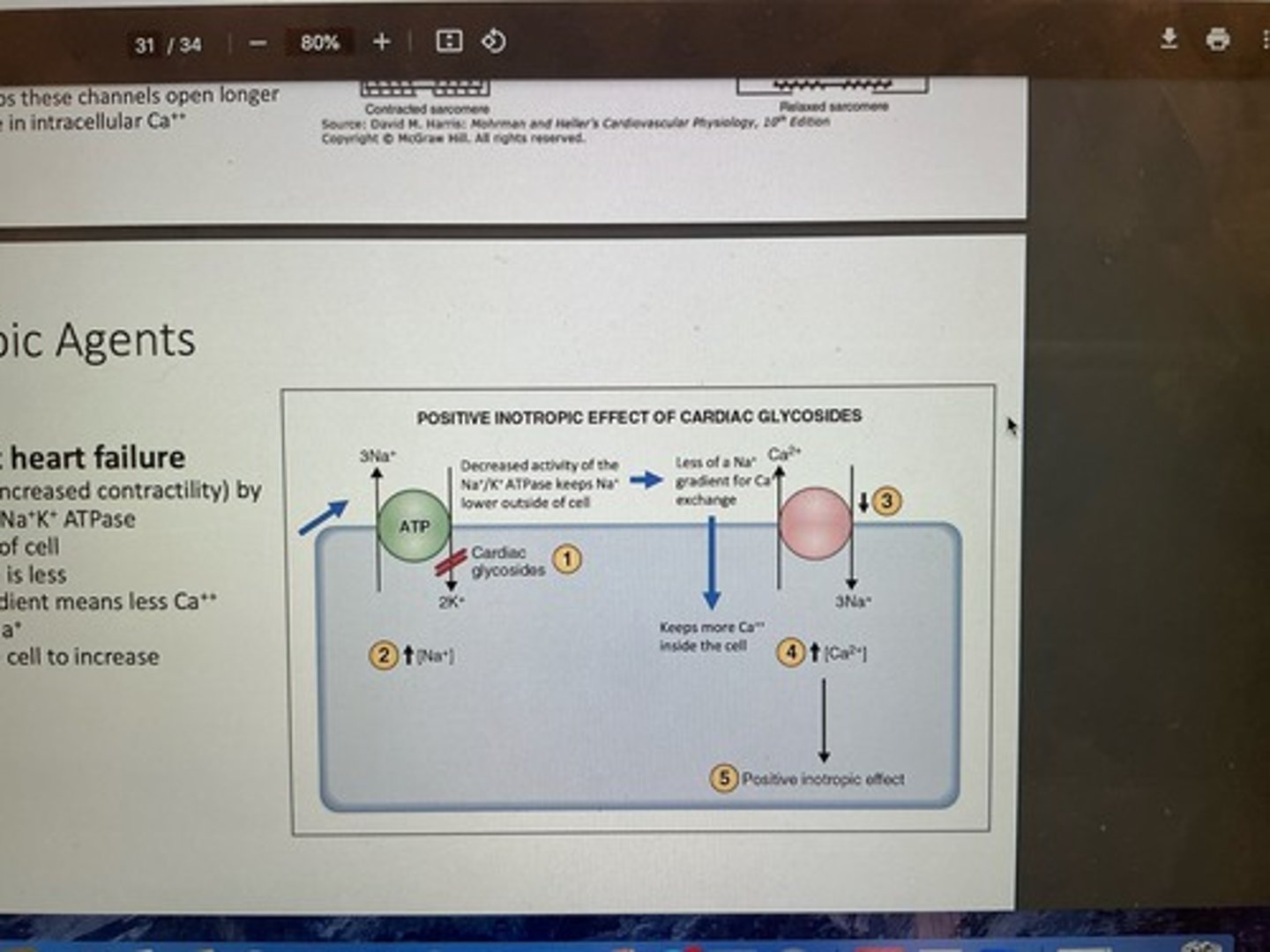
Positive inotropic agents
Glycosides used to treat heart failure
- increase Ca++ availability (increased contractility) by decreasing activity of Na+/K+ ATPase
-keeps Na+ lower outside of cell
-Na+ gradient for diffusion is less
-less Na+ moving down gradient means less Ca++ moving out in exchange for Na+
-more Ca++ remains inside cell to increase contractility
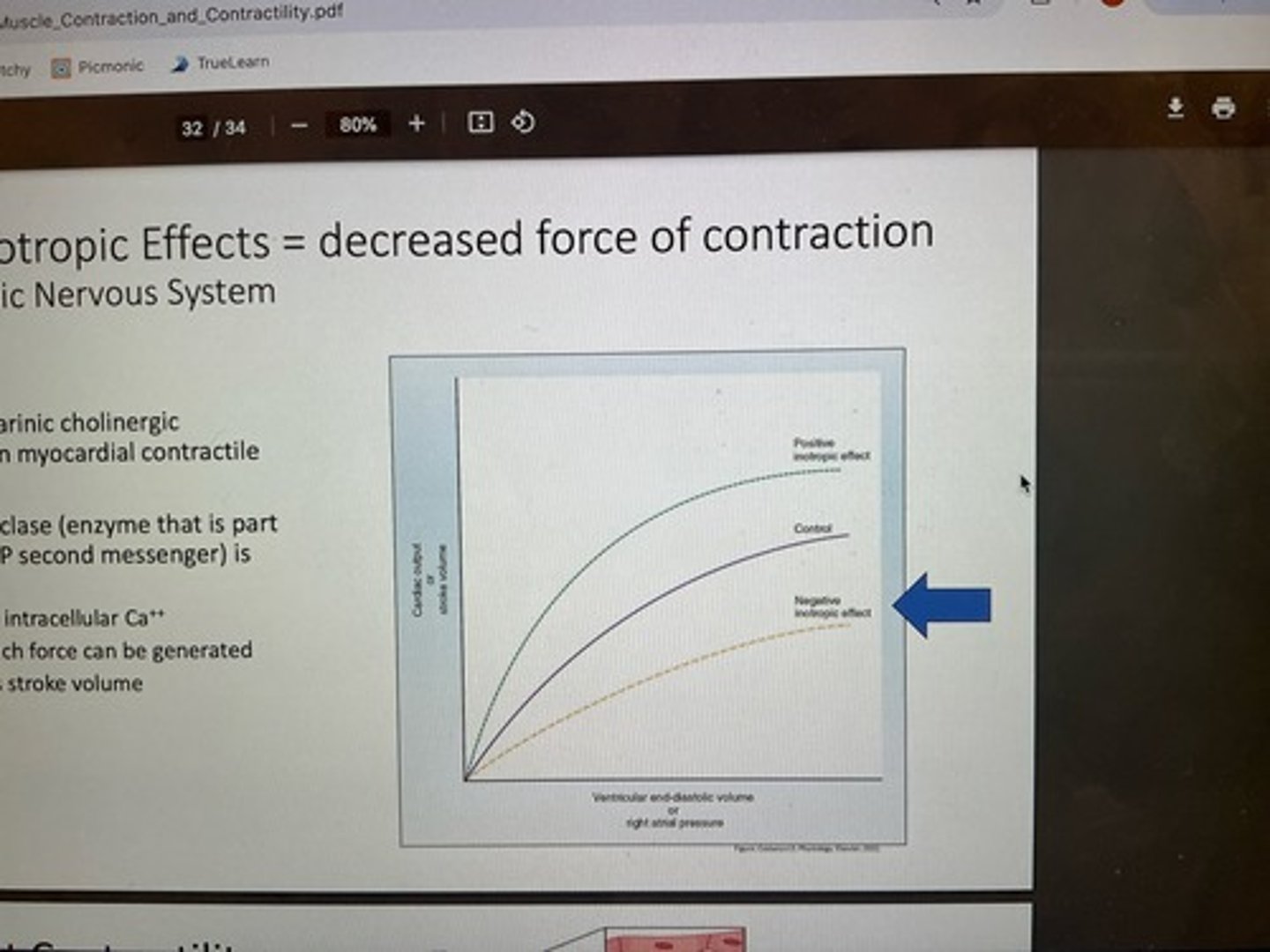
negative inotropic effects
decreased force of contraction (parasympathetic) acetylcholine
1. binds muscarinic cholinergic receptors on myocardial contractile cells
2. adenylyl cycles (enzyme part of cAMP second messenger) inhibited
-decreased intracellular Ca++
-not as much force can be generated
-decreases stroke volume
drugs affect contractility
cardiac glycosides like digoxin
-decreases activity of Na+/K+ pump
-decreases Na+ gradient that exchanges Ca++ and Na+ (keeps more Ca++ inside cell, increases contractility)