Cardiovascular System
5.0(1)
Card Sorting
1/63
Earn XP
Description and Tags
Last updated 4:23 PM on 12/6/22
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
64 Terms
1
New cards
functions of the cardiovascular system
1) transport: supplies nutrients (food, oxygen, etc) to the body and removes waste (CO2) from body tissues
2) regulation and homeostasis: hormonal highway and plays important role in temperature regulation
3) protection: vessels protect against excessive blood loss (clotting); white blood cells serve immune functions
2) regulation and homeostasis: hormonal highway and plays important role in temperature regulation
3) protection: vessels protect against excessive blood loss (clotting); white blood cells serve immune functions
2
New cards
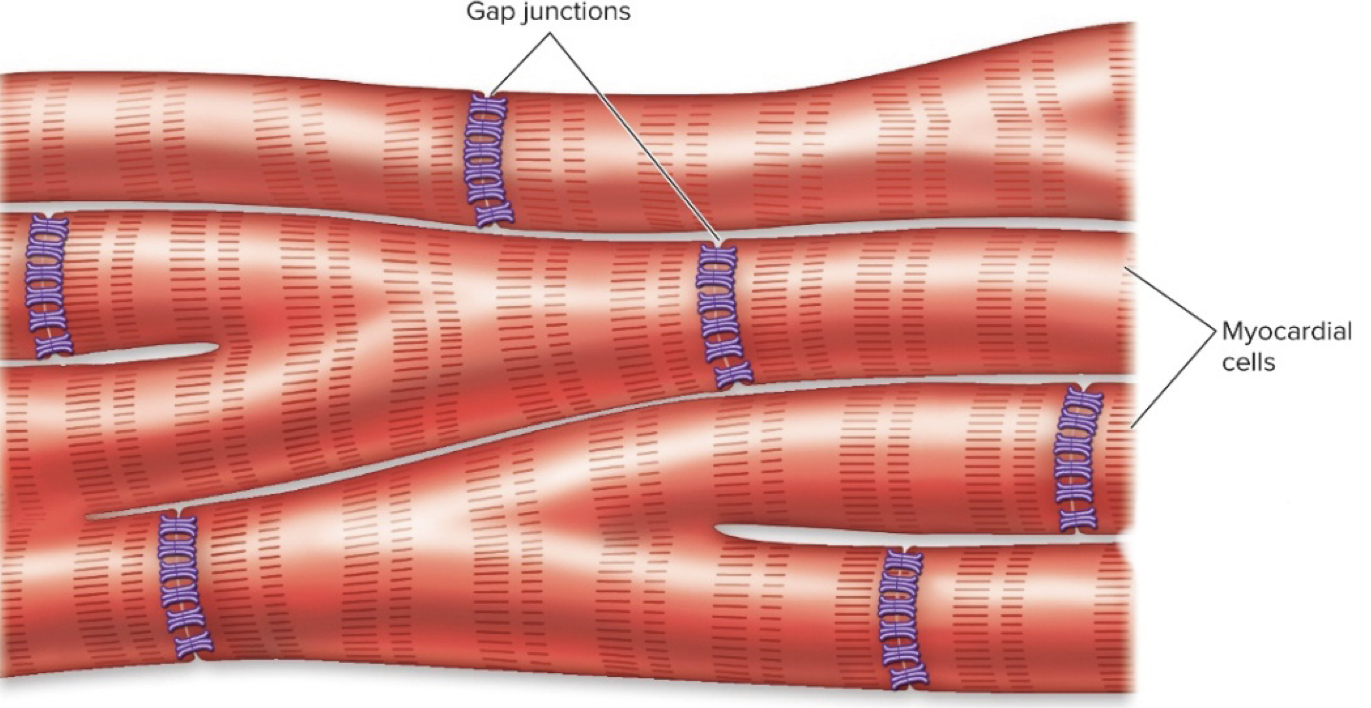
myocardial cells
- striated heart muscle cells that contract in a sliding filament mechanism
- use actin-myosin filaments in sarcomeres
-connected by intercalated discs/gap junctions, therefore cells are electrically connected by flow of charged atoms (ions)
- use actin-myosin filaments in sarcomeres
-connected by intercalated discs/gap junctions, therefore cells are electrically connected by flow of charged atoms (ions)
3
New cards
intercalated discs
- allow cells to be continuously stimulated
- cells are all tightly connected, therefore ions can flow between cells causing depolarization --> muscle cells to contract around the same time
- the load is always the same (same amount of blood in your ventricles each time)
- cells are all tightly connected, therefore ions can flow between cells causing depolarization --> muscle cells to contract around the same time
- the load is always the same (same amount of blood in your ventricles each time)
4
New cards
myocardium
- mass of myocardial cells
- functions as a single functional unit: myocardium contracts to its FULL EXTENT each time
- when one cell gets a signal to contract, it spreads to all cells through gap junctions
- functions as a single functional unit: myocardium contracts to its FULL EXTENT each time
- when one cell gets a signal to contract, it spreads to all cells through gap junctions
5
New cards
skeletal muscle stimulation vs myocardium
- in skeletal we would usually have one neuron stimulate few muscle cells in its motor unit (wouldn't stimulate entire muscle)
- the entire heart muscle is stimulated bc all connected to each other through intercalated discs and gap junctions
- the entire heart muscle is stimulated bc all connected to each other through intercalated discs and gap junctions
6
New cards
gap junctions
- pores that allow for direct ion flow; cell to cell communication
- fluid-filled channels through plasma membrane of adjacent cells that permit conduction of impulses from one cell to the next; connections btwn cytoplasm
- dont have to wait for NT- can send action potential straight to adjacent cell via ions
- ALLOW HEART MUSCLE CELLS TO CONTRACT AS A UNIT
- fluid-filled channels through plasma membrane of adjacent cells that permit conduction of impulses from one cell to the next; connections btwn cytoplasm
- dont have to wait for NT- can send action potential straight to adjacent cell via ions
- ALLOW HEART MUSCLE CELLS TO CONTRACT AS A UNIT
7
New cards
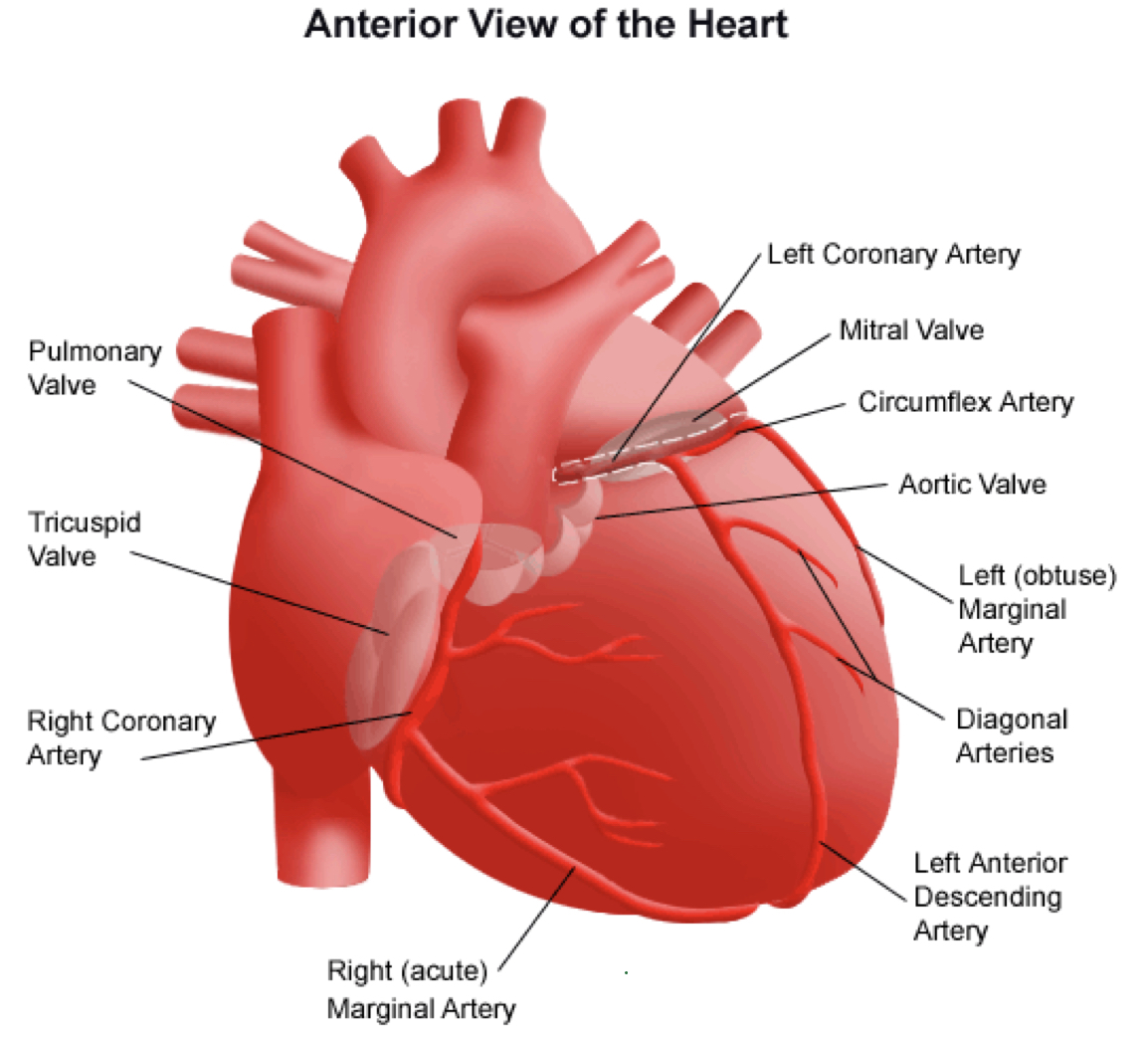
heart basic structure
- arteries that carry blood AWAY from the heart
- veins that carry blood TO the heart
- 2 atria that receive venous blood (blood enters the heart)
- 2 ventricles that eject blood into arteries (blood leaves the heart); right ventricle pumps deoxygenated blood through the pulmonary artery--> lungs and the left ventricle pumps oxygenated blood through the aorta--> rest of the body
- veins that carry blood TO the heart
- 2 atria that receive venous blood (blood enters the heart)
- 2 ventricles that eject blood into arteries (blood leaves the heart); right ventricle pumps deoxygenated blood through the pulmonary artery--> lungs and the left ventricle pumps oxygenated blood through the aorta--> rest of the body
8
New cards
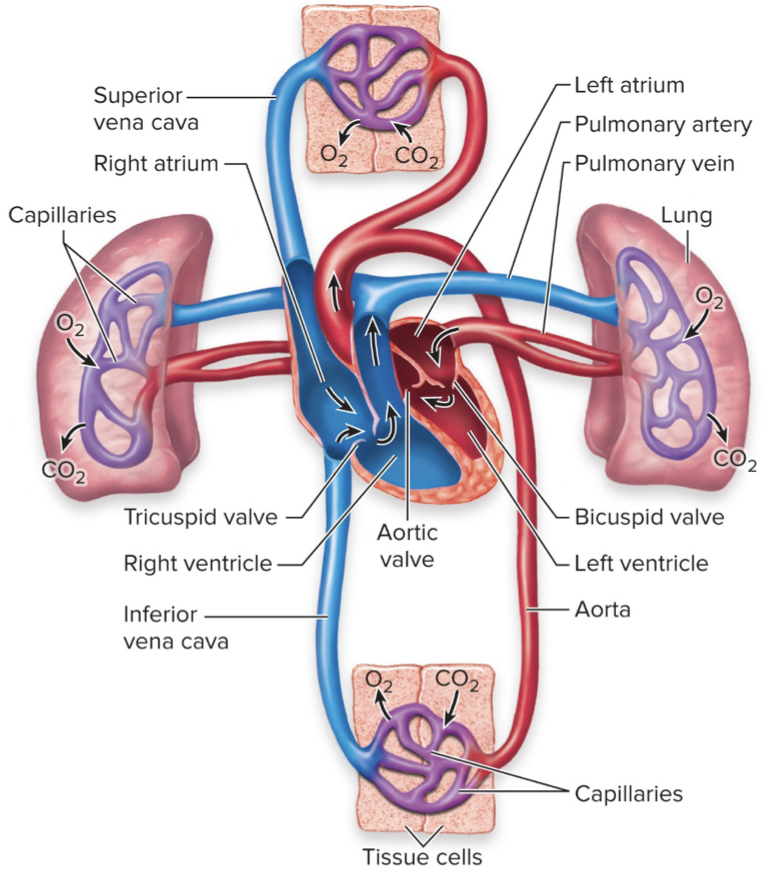
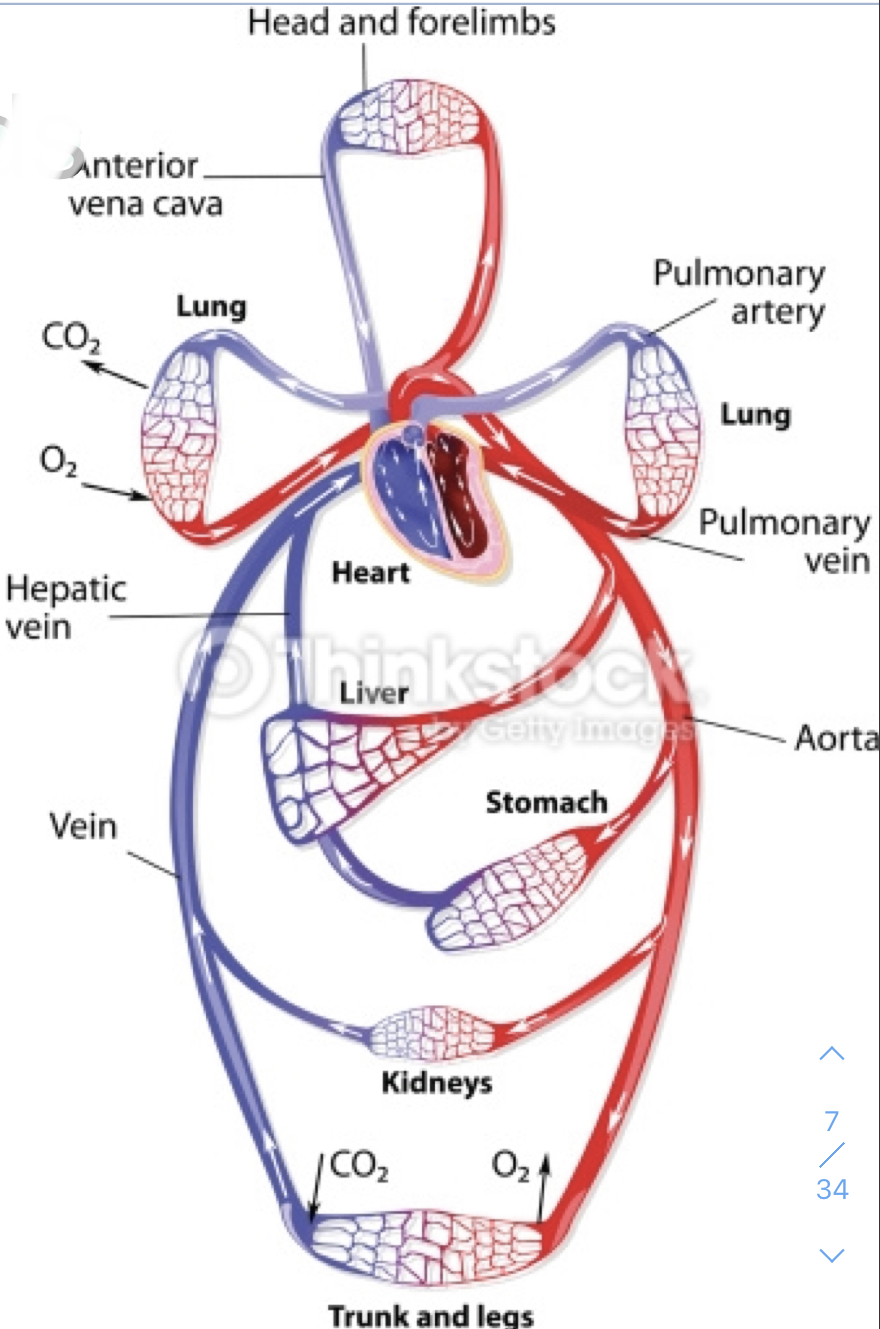
pulmonary circulation
- circulation of blood between heart and lungs
- deoxygenated blood pumps TO LUNGS via pulmonary ARTERIES
- oxygenated blood RETURNS TO HEART via pulmonary VEINS
- deoxygenated blood pumps TO LUNGS via pulmonary ARTERIES
- oxygenated blood RETURNS TO HEART via pulmonary VEINS
9
New cards
systemic circulation
- circulation between the heart and body tissues
- oxygenated blood pumps TO BODY via AORTA
- deoxygenated blood RETURNS TO HEART via superior and inferior VENA CAVAE
- oxygenated blood pumps TO BODY via AORTA
- deoxygenated blood RETURNS TO HEART via superior and inferior VENA CAVAE
10
New cards
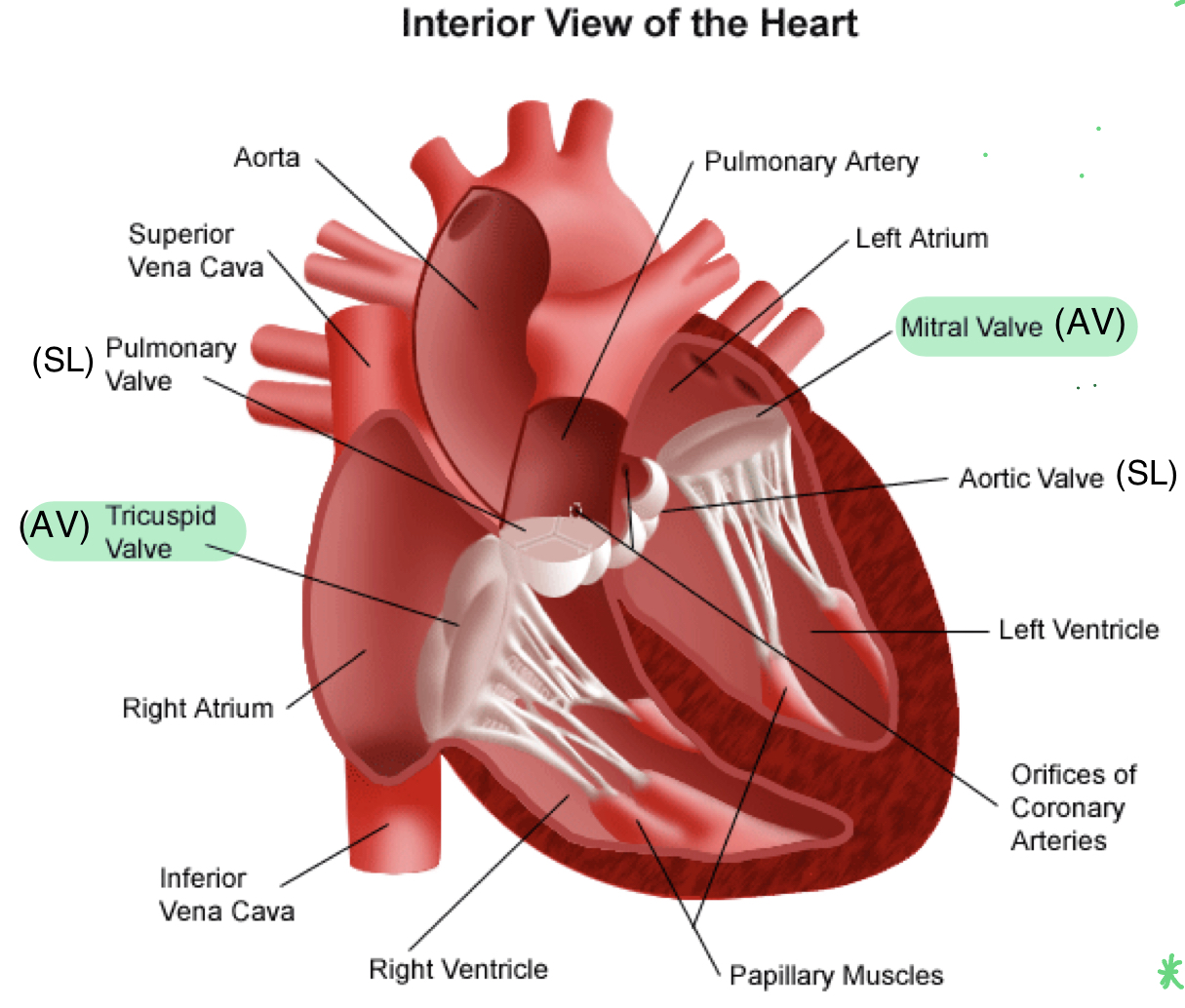
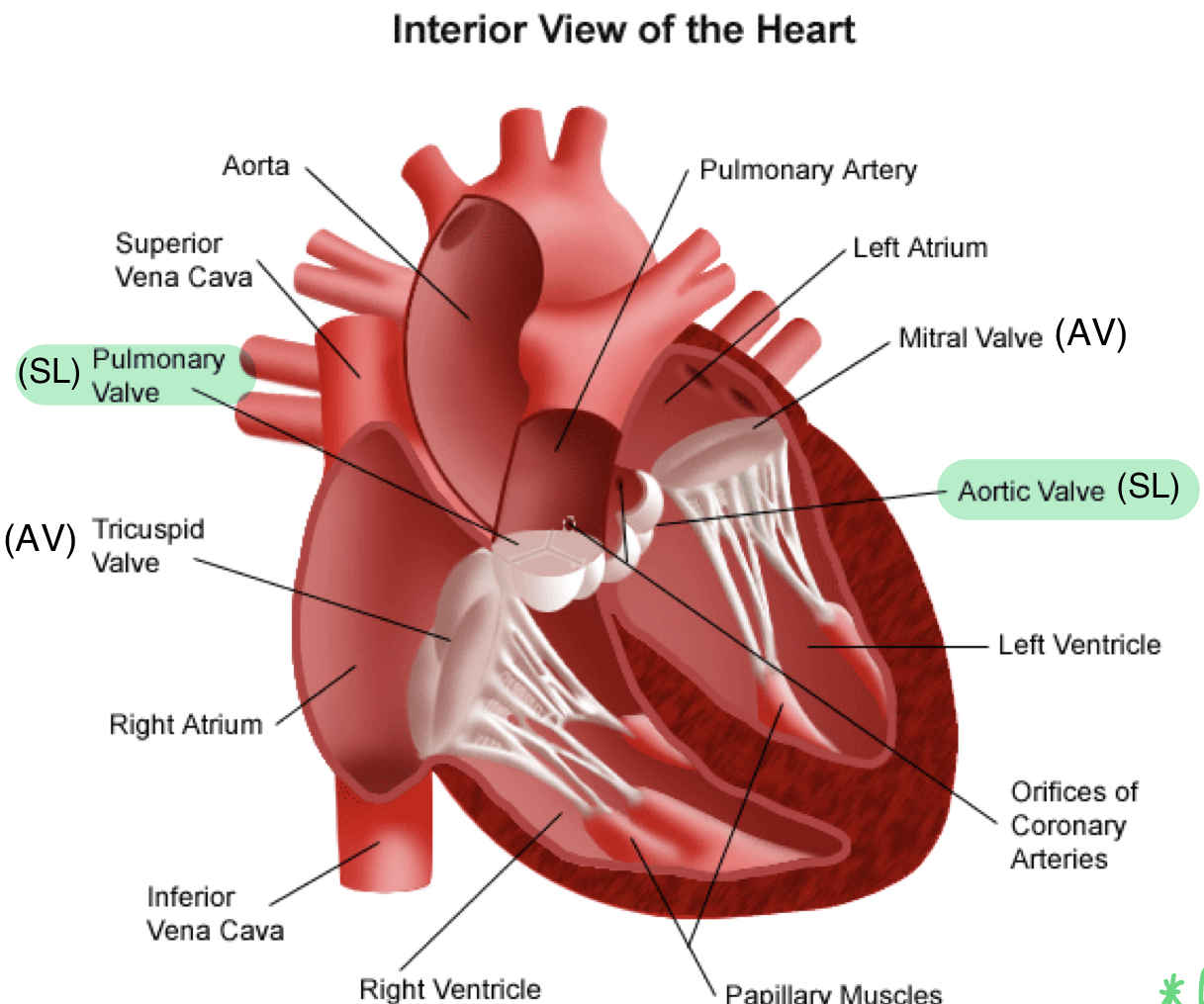
two atria-ventricular (AV) valves
- one-way valves between atria and ventricles
- tricuspid valve (between right atria and right ventricle) and mitral/bicuspid valve (between left atria and left ventricle)
- make "LUB" sound when close (both close at the same time)
- tricuspid valve (between right atria and right ventricle) and mitral/bicuspid valve (between left atria and left ventricle)
- make "LUB" sound when close (both close at the same time)
11
New cards
two semi-lunar (SL) valves
- one-way valves at the base of major arteries
pulmonary valve (between right ventricle and pulmonary artery) and aortic valve (between left ventricle and aorta)
- make "DUB" sound when closing
pulmonary valve (between right ventricle and pulmonary artery) and aortic valve (between left ventricle and aorta)
- make "DUB" sound when closing
12
New cards
function of valves
- allow blood to flow in one direction; prevent back flow and mixing
13
New cards
myocardial septum
- separates the left and right ventricles
- prevents mixing of oxygenated and deoxygenated blood
- prevents mixing of oxygenated and deoxygenated blood
14
New cards
what could happen if someone has a hole in their heart?
- blood can mix, therefore deoxygenated blood can be transported out of the heart with oxygenated blood to body tissues instead of to the lungs
- tissues may not get enough oxygen and must wait until deoxygenated blood circulates all the way back to the heart
- tissues may not get enough oxygen and must wait until deoxygenated blood circulates all the way back to the heart
15
New cards
flow of blood
1) deoxygenated blood from body tissues enters the right atrium via the superior and inferior vena cavae
2) blood flows through the tricuspid (AV) valve into the right ventricle
3) blood is pumped out of the pulmonary (SL) valve and to the lungs via the pulmonary arteries
4) blood is oxygenated in the lungs and returns to the heart in the left atria via pulmonary veins
5) flows through mitral/bicuspid (AV) valve and into the left ventricle
6) blood is pumped through the aortic (SL) valve out the aorta to body tissues
2) blood flows through the tricuspid (AV) valve into the right ventricle
3) blood is pumped out of the pulmonary (SL) valve and to the lungs via the pulmonary arteries
4) blood is oxygenated in the lungs and returns to the heart in the left atria via pulmonary veins
5) flows through mitral/bicuspid (AV) valve and into the left ventricle
6) blood is pumped through the aortic (SL) valve out the aorta to body tissues
16
New cards
closing of AV valves
- get pulled closed by papillary muscles
- get depolarization signal from ventricles and contract--> pulls AV valves shut
- make a "LUB" sound when close
- systole: when ventricles contract (blood is about to be pushed out of ventricles through contraction so AV valves pulled to shut and SL valves are forced open by pressure)
- get depolarization signal from ventricles and contract--> pulls AV valves shut
- make a "LUB" sound when close
- systole: when ventricles contract (blood is about to be pushed out of ventricles through contraction so AV valves pulled to shut and SL valves are forced open by pressure)
17
New cards
closing of SL valves
- snap shut when "cups" fill with blood
- make "DUB" sound when closing
- diastole: when ventricles relax
- SL snap shut to prevent blood from leaking back into ventricles ( AV valves will be open again to allow blood to fill the ventricles bc no longer contracting)
- make "DUB" sound when closing
- diastole: when ventricles relax
- SL snap shut to prevent blood from leaking back into ventricles ( AV valves will be open again to allow blood to fill the ventricles bc no longer contracting)
18
New cards
blood pressure
- systolic/diastolic
- blood pressure during VENTRICLE CONTRACTION over blood pressure when VENTRICLE RELAXED or dilating
- blood pressure during VENTRICLE CONTRACTION over blood pressure when VENTRICLE RELAXED or dilating
19
New cards
where is blood pressure highest and why?
- left ventricle
- must contract to pump blood far throughout the body
- must contract to pump blood far throughout the body
20
New cards
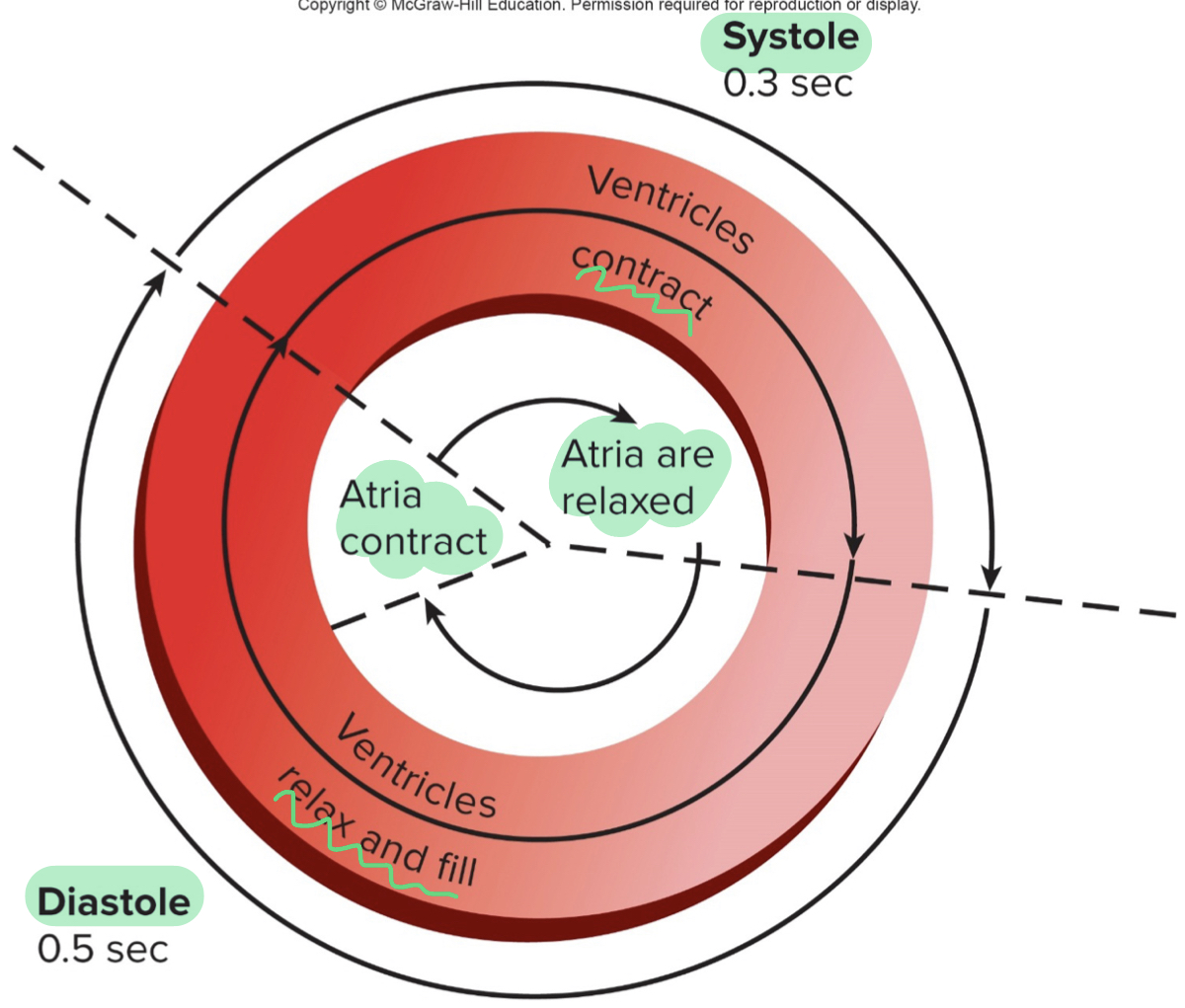
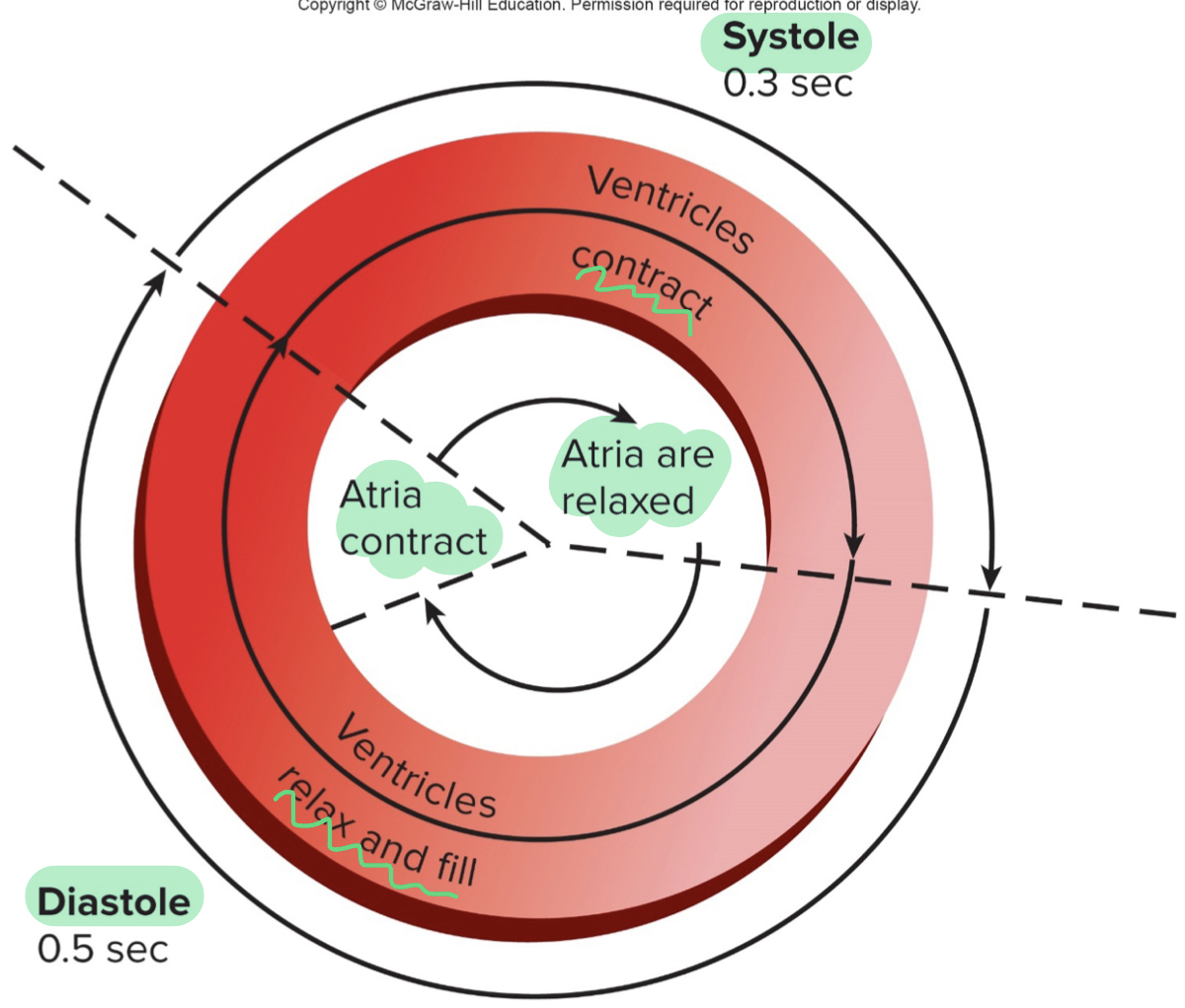
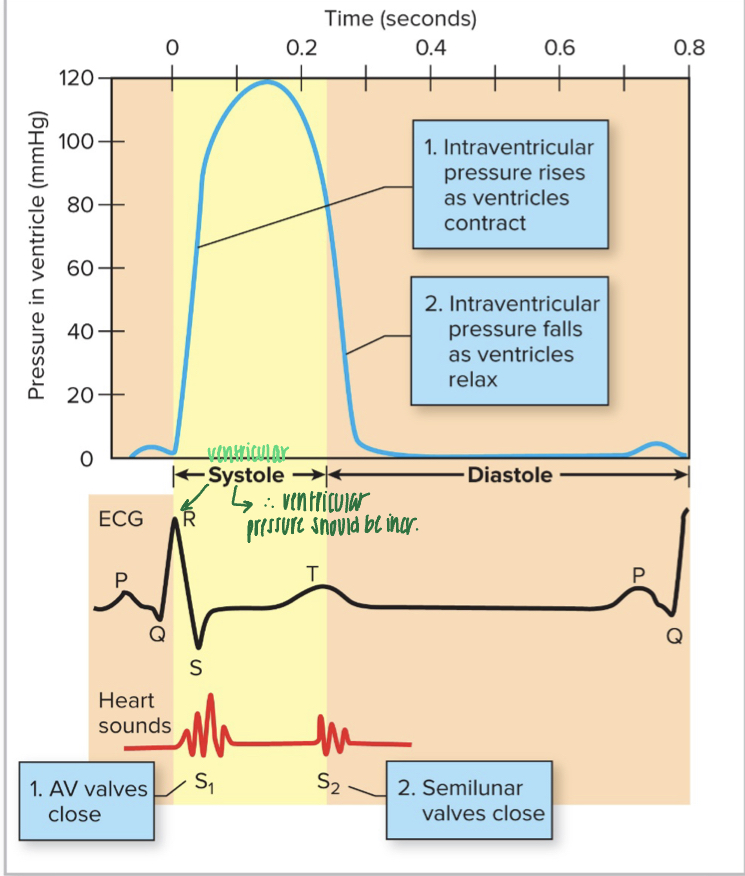
systole
- ventricle contraction (ventricles contract at the same time)
- AV valves shut and SL valves forced open
- short time; takes less time to contract and pump blood out than to fill
- AV valves shut and SL valves forced open
- short time; takes less time to contract and pump blood out than to fill
21
New cards
diastole
- relaxation and filling of ventricles
- SL valves shut an AV valves open
- longer time; takes longer for ventricles to fill
- contraction of the atria occurs in the last 0.1 second of ventricular diastole (little extra push/squeeze for ventricle to contract
- relaxation of the atria occurs during ventricular diastole
- SL valves shut an AV valves open
- longer time; takes longer for ventricles to fill
- contraction of the atria occurs in the last 0.1 second of ventricular diastole (little extra push/squeeze for ventricle to contract
- relaxation of the atria occurs during ventricular diastole
22
New cards
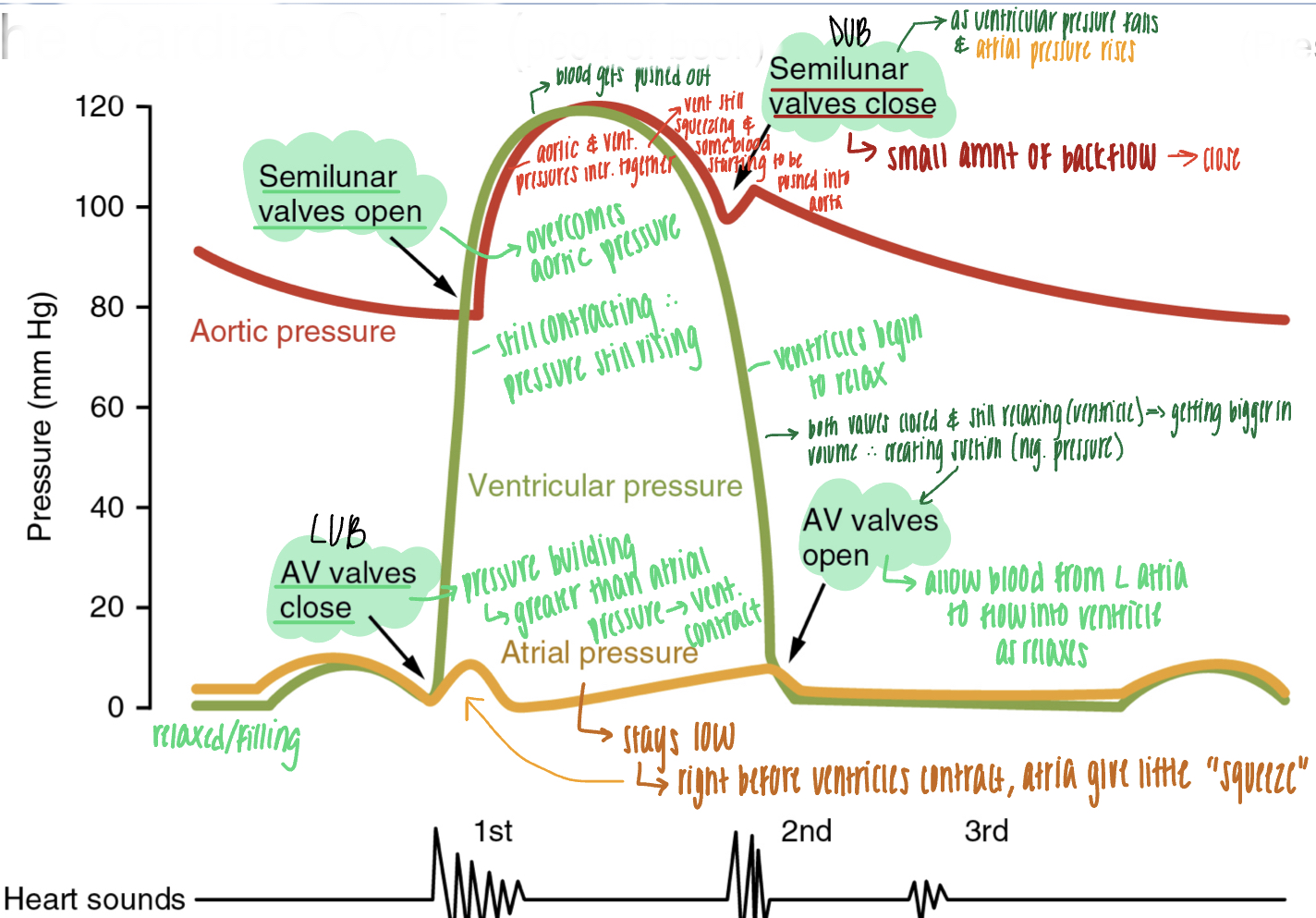
what drives closing of valves
changes in pressure between heart chambers
23
New cards
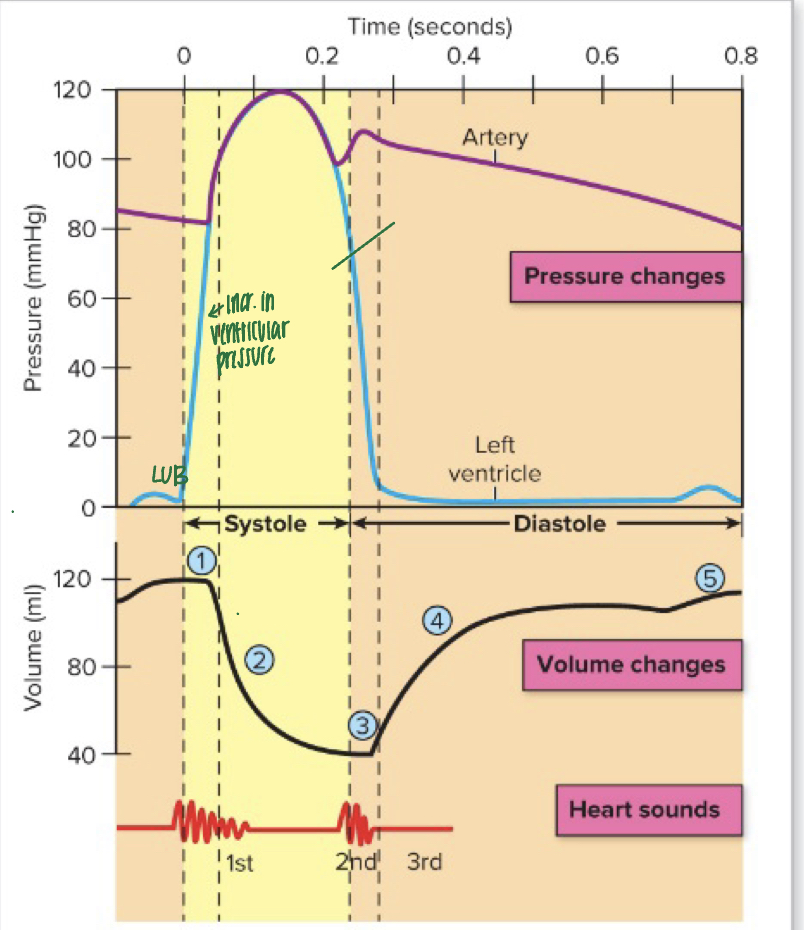
stages of the cardiac cycle
- start in systole
1) isovolumic contraction
2) ejection
3) isovolumic relaxation
4) rapid filling
5) atrial contraction
1) isovolumic contraction
2) ejection
3) isovolumic relaxation
4) rapid filling
5) atrial contraction
24
New cards
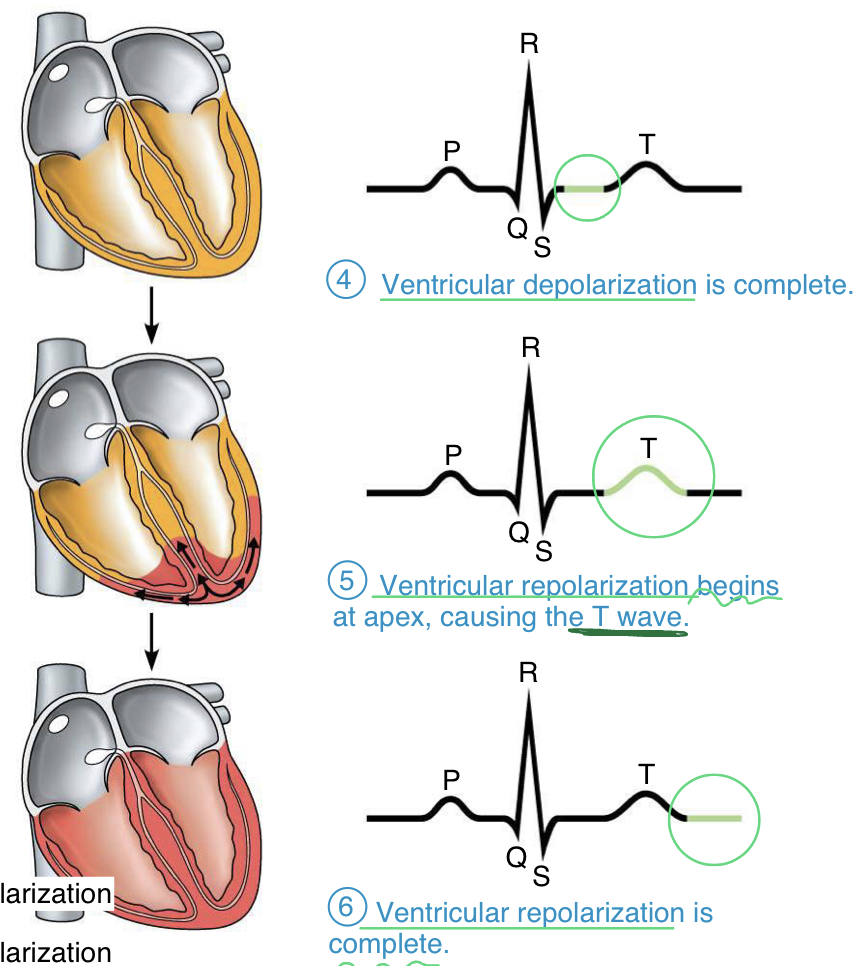
isovolumic contraction
SYSTOLE
- contract, but volume stays the same
- ventricles begin to contract, causing intraventricular pressure to RISE
- AV valves snap SHUT(LUB- and ventricular contraction) --> first sound heard
- ventricles are neither filling with blood nor ejecting blood (SL valves not open yet)
- both valves are shut, which is causing the pressure to rise
- contract, but volume stays the same
- ventricles begin to contract, causing intraventricular pressure to RISE
- AV valves snap SHUT(LUB- and ventricular contraction) --> first sound heard
- ventricles are neither filling with blood nor ejecting blood (SL valves not open yet)
- both valves are shut, which is causing the pressure to rise
25
New cards
ejection
- ventricular pressure is GREATER than aortic pressure, SL valves open and blood is ejected from the ventricles
- pressure in the left ventricle and aorta rises to 120 mmHg (being pumped straight into aorta, therefore aortic pressure also rises)
- stroke volume: amount of blood ejected by ventricle contraction (about 2/3 of total ventricular volume)
- pressure in the left ventricle and aorta rises to 120 mmHg (being pumped straight into aorta, therefore aortic pressure also rises)
- stroke volume: amount of blood ejected by ventricle contraction (about 2/3 of total ventricular volume)
26
New cards
isovolumic relaxation
- shift to diastole
- ventricular pressure decreases (because relaxing) to below that of arteries, this "back flow" causes SL valves to snap SHUT (DUB- and ventricular relaxation) --> second heart sound; blood starting to fill "cups" of SL valve (from back pressure of ventricle relaxing and expanding)--> SL valves to shut)
- pressure in aorta decreases slightly, pressure in left ventricle falls to 0mmHg
- both AV and SL valves are closed until...
- ventricular pressure decreases (because relaxing) to below that of arteries, this "back flow" causes SL valves to snap SHUT (DUB- and ventricular relaxation) --> second heart sound; blood starting to fill "cups" of SL valve (from back pressure of ventricle relaxing and expanding)--> SL valves to shut)
- pressure in aorta decreases slightly, pressure in left ventricle falls to 0mmHg
- both AV and SL valves are closed until...
27
New cards
rapid filling
- ventricular pressure falls below pressure of the atria, causing AV valves to open --> rapid filling of the ventricles with blood from the atria
28
New cards
atrial contraction
- delivers the final amount of blood into the ventricles immediately before the next phase of isovolumic contraction of the ventricles
29
New cards
why is the myocardium thicker over the left ventricle?
the left ventricle needs to be able to produce a greater contraction to transmit blood farther
30
New cards
summary of pressure changes during the cardiac cycle
1) ventricles begin contraction, pressure rises, and AV valves close (LUB); isovolumic contraction
2) pressure builds, SL valves open, and blood is ejected into arteries
3) pressure in ventricles falls; SL valves close (DUB); isovolumic relaxation
4) slight inflection in pressure during isovolumic relaxation
5) pressure in ventricles falls below that of atria and AV valves open --> blood fills ventricles
6) atria give small squeeze/contraction, sending last of blood to ventricles
2) pressure builds, SL valves open, and blood is ejected into arteries
3) pressure in ventricles falls; SL valves close (DUB); isovolumic relaxation
4) slight inflection in pressure during isovolumic relaxation
5) pressure in ventricles falls below that of atria and AV valves open --> blood fills ventricles
6) atria give small squeeze/contraction, sending last of blood to ventricles
31
New cards
automaticity
heart is able to beat on its own; depolarize muscle without need of the nervous system
32
New cards
sinoatrial (SA) node
- "pacemaker" of the heart
- located in the right atrium
- comprised of non-contractile cells (patch of cells) that spontaneously depolarize --> "pacemaker potential" NOT action potential
- repolarize and depolarize constantly
- located in the right atrium
- comprised of non-contractile cells (patch of cells) that spontaneously depolarize --> "pacemaker potential" NOT action potential
- repolarize and depolarize constantly
33
New cards
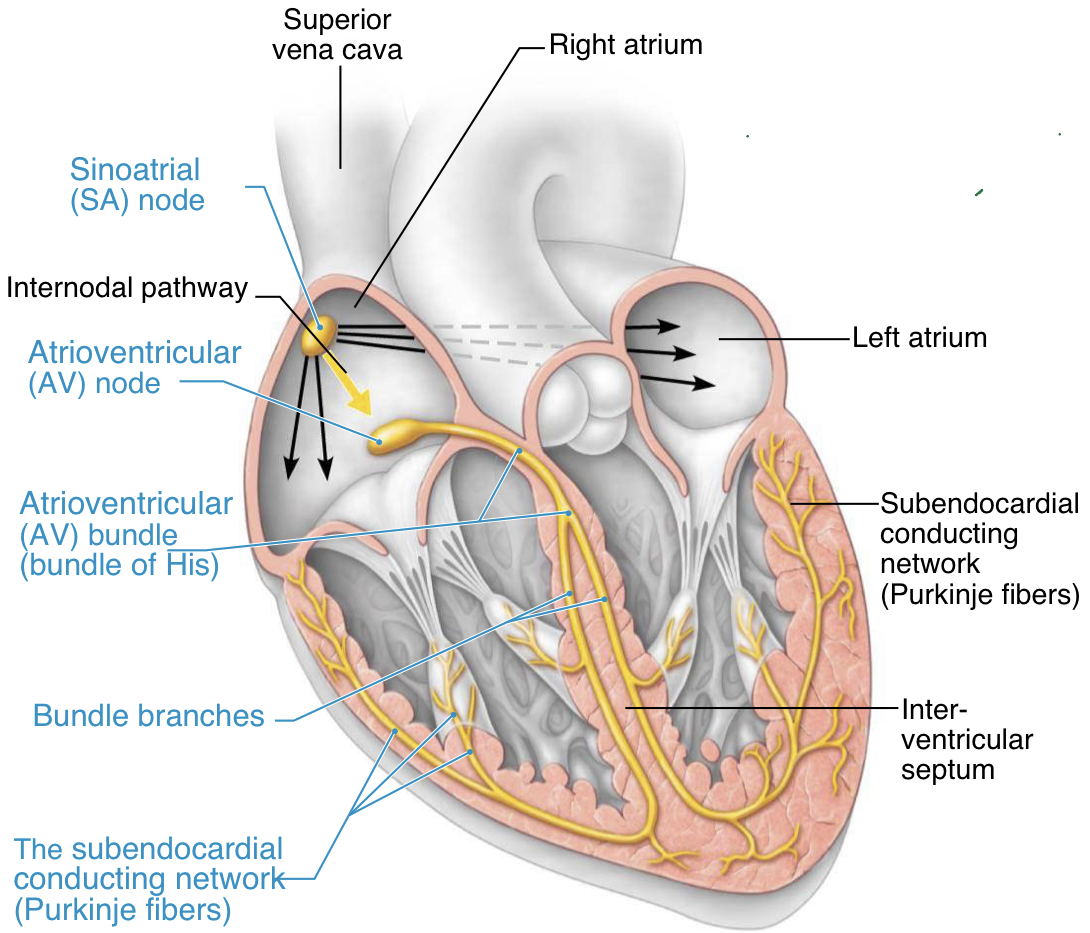
atrioventricular (AV) node and purkinje fibers
- AV node receives depolarization signal from SA node
- act as secondary "pacemakers"- normally suppressed by action potentials from SA node
- AV node can depolarize if it doesnt receive a signal from the SA node, however, it is usually slower and less effective
- depolarization in purkinje fibers --> ventricle contraction
- act as secondary "pacemakers"- normally suppressed by action potentials from SA node
- AV node can depolarize if it doesnt receive a signal from the SA node, however, it is usually slower and less effective
- depolarization in purkinje fibers --> ventricle contraction
34
New cards
conduction system of the heart
1) pacemaker potential originates in the SA node located in the right atria- signal spreads throughout myocardial cells of atrium; electrical depolarization can go through septum--> both atria get depolarization signal--> provide little extra squeeze to push blood into the ventricles
2) fibrous tissue separates the chambers therefore the potential cant spread directly to the ventricle so the signal is passed through AV node
3) pacemaker potential continues through bundle of His, down bundle branches until it reaches purkinje fibers
4) pacemaker potential spreads medial to lateral, causing both ventricles to contract simultaneously
2) fibrous tissue separates the chambers therefore the potential cant spread directly to the ventricle so the signal is passed through AV node
3) pacemaker potential continues through bundle of His, down bundle branches until it reaches purkinje fibers
4) pacemaker potential spreads medial to lateral, causing both ventricles to contract simultaneously
35
New cards
why is there a slight delay of ventricular contraction?
the pacemaker potential/signal has to travel all the way down the fibers
36
New cards
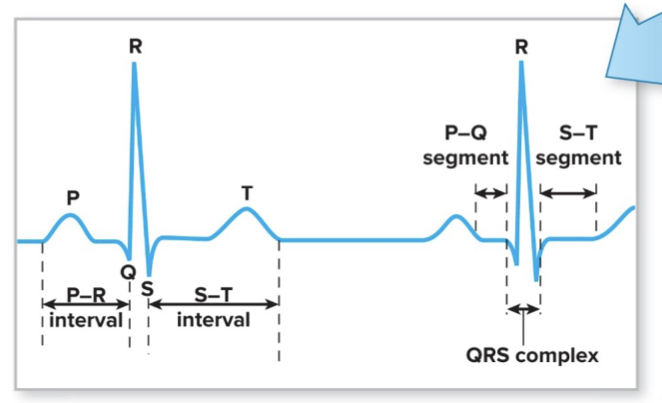
function of an electrocardiogram (ECG/EKG)
-detect changes in voltage current from heart through the skin
- change in electrical charge is conducted through the body, which is why can measure from wrist and ankle
- measurement for depolarization of heart tissue
- change in electrical charge is conducted through the body, which is why can measure from wrist and ankle
- measurement for depolarization of heart tissue
37
New cards
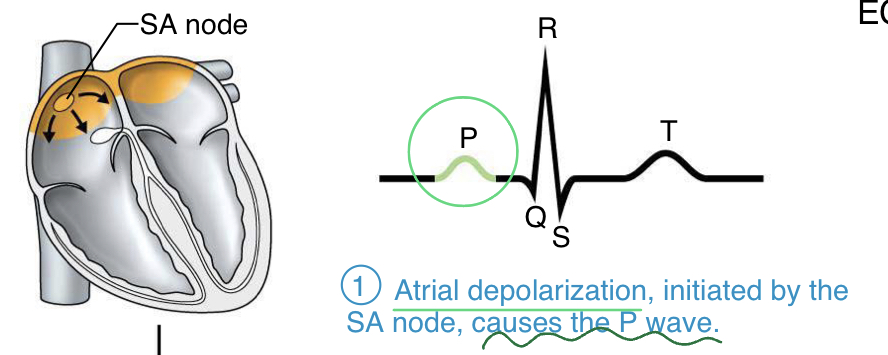
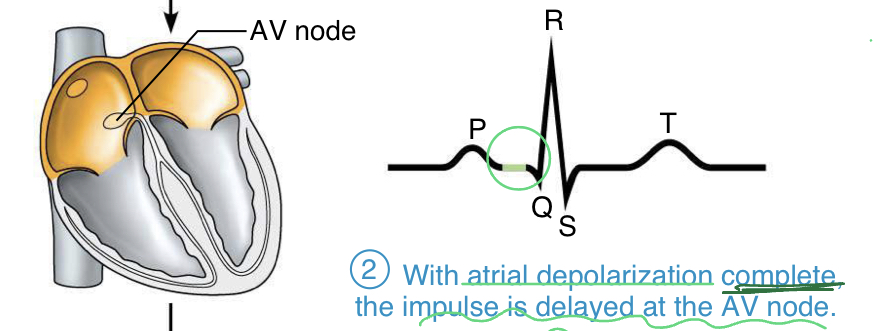
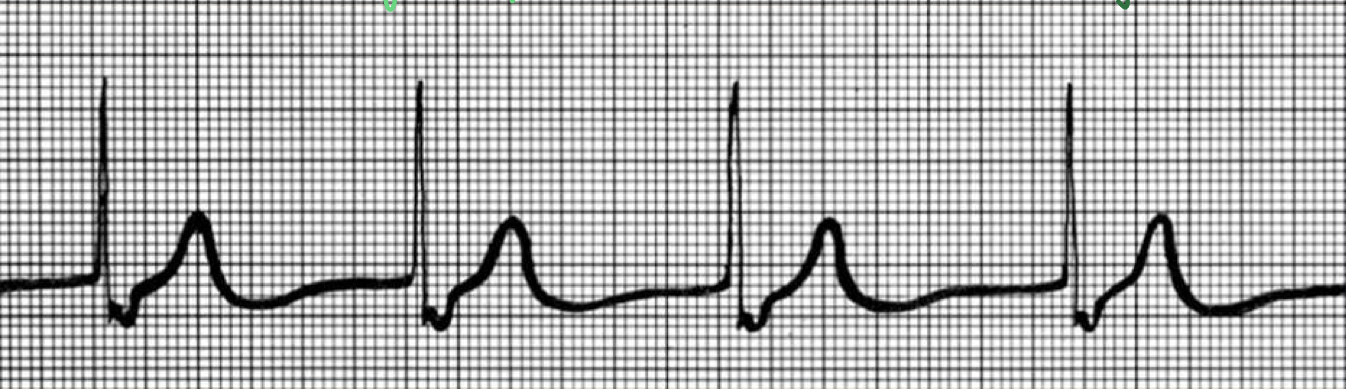
P wave
- depolarization (and small contraction) across the atria
- initiated by the SA node
- initiated by the SA node
38
New cards
period before QRS wave
- with atrial depolarization complete (potential is back to baseline), the impulse is delayed at the AV node, therefore the ventricles have not received the signal yet
39
New cards
QRS wave
- ventricular depolarization
Q: ventricle starts to depolarize
R: reaches a point where half tissue is depolarized; atria repolarize during this time
S: ventricle fully depolarizes (measuring the potential, therefore if the whole tissue is depolarized, its potential is zero)
Q: ventricle starts to depolarize
R: reaches a point where half tissue is depolarized; atria repolarize during this time
S: ventricle fully depolarizes (measuring the potential, therefore if the whole tissue is depolarized, its potential is zero)
40
New cards
T wave
- repolarization of the ventricles (pumping Ca out of the cytoplasm); begins at apex
- back to resting to be able to depolarize again
- back to resting to be able to depolarize again
41
New cards
correlation of ECG with heart sounds
- QRS wave is the depolarization of ventricles- stimulates their contraction: rise in intraventricular pressure causes AV valves to close
- LUB occurs after the QRS wave as the AV valves close
- DUB occurs at the beginning of the T wave as the SL valves close
- LUB occurs after the QRS wave as the AV valves close
- DUB occurs at the beginning of the T wave as the SL valves close
42
New cards
why do the mechanical changes not happen until after electrical stimulation?
- need depolarization to happen before can have muscle contract
- have to have ion channels open, voltage changes, release of calcium, etc. --> all takes time, therefore there is a delay between electrical and mechanical
- have to have ion channels open, voltage changes, release of calcium, etc. --> all takes time, therefore there is a delay between electrical and mechanical
43
New cards
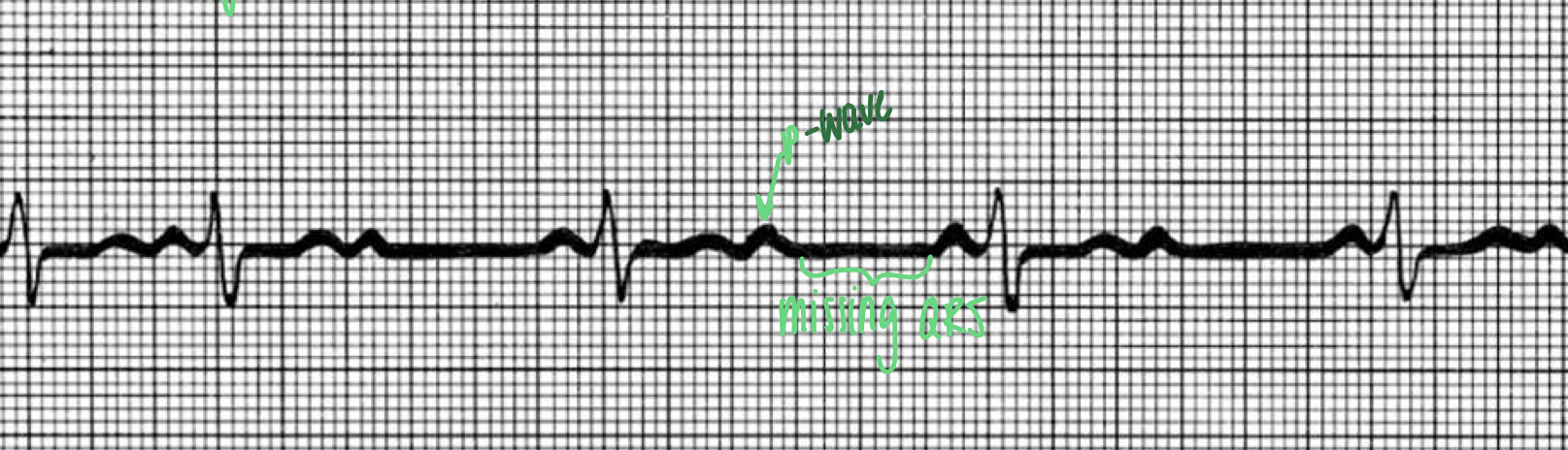
ECG of nonfunctional SA node
- absence of P wave
- "junctional rhythm"
- Av node acting as primary pacemaker
- "junctional rhythm"
- Av node acting as primary pacemaker
44
New cards
ECG when AV node fails to conduct some impulses
- more P waves than QRS waves; missing QRS waves
- "second degree heart block"
- "second degree heart block"
45
New cards
ECG of ventricular fibrilation
- waves all over; no pattern
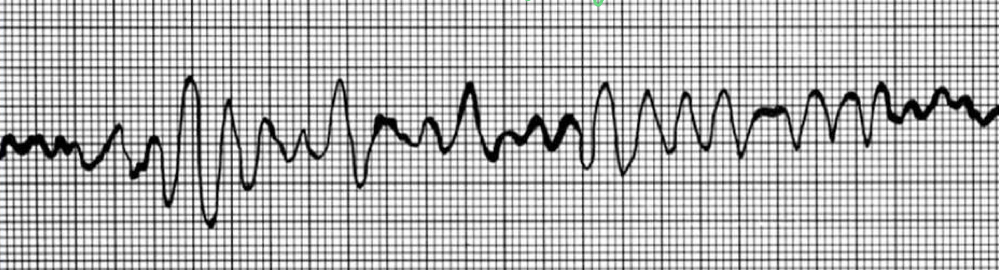
46
New cards
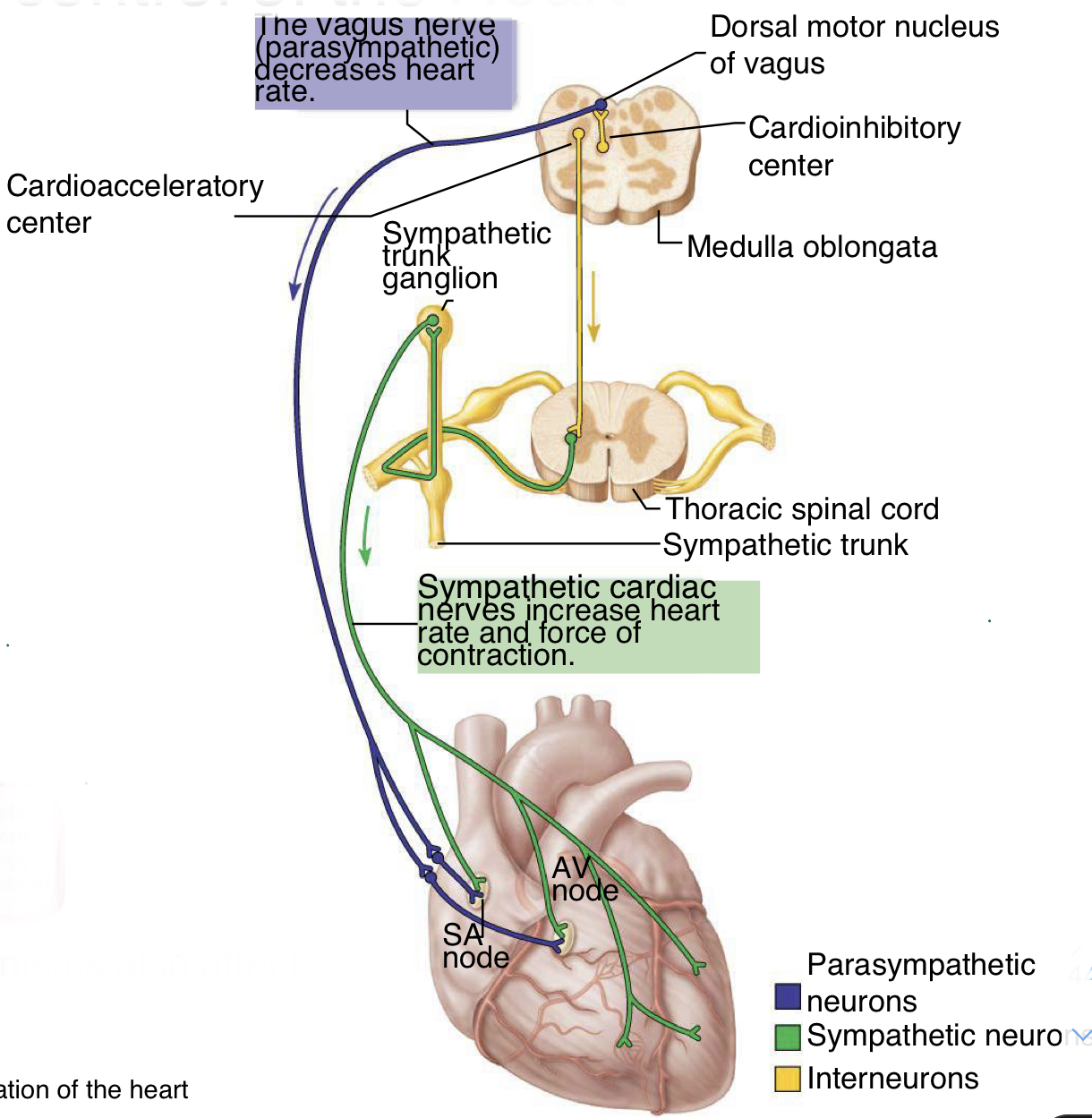
nervous system control of the heart
- can modify heart rate; brain isnt telling your heart to beat but is modifying it based on sensory inputs
- autonomic innervation of the SA node= major means of regulation: sympathetic nervous system stimulate heart to beat faster (innervate at SA node, AV node, atria, and ventricles); vagus nerve/parasympathetic nervous system decrease heart rate (innervate only at SA node and AV node)
- autonomic innervation of the SA node= major means of regulation: sympathetic nervous system stimulate heart to beat faster (innervate at SA node, AV node, atria, and ventricles); vagus nerve/parasympathetic nervous system decrease heart rate (innervate only at SA node and AV node)
47
New cards
effects of autonomic nerve activity of the heart
sympathetic nerve effects (fight or flight):
- at SA node, increased rate of diastolic depolarization (increased cardiac rate)
- at AV node, increased conduction rate
- at atrial muscle, increased strength of contraction
- at ventricular muscle, increase strength of contraction
parasympathetic nerve effects (rest and digest)
- at SA node, decreased rate of diastolic depolarization (decreased cardiac rate)
- at AV node, decreased conduction rate
- at atrial muscle, no significant effect
- at ventricular muscle, no significant effect
- at SA node, increased rate of diastolic depolarization (increased cardiac rate)
- at AV node, increased conduction rate
- at atrial muscle, increased strength of contraction
- at ventricular muscle, increase strength of contraction
parasympathetic nerve effects (rest and digest)
- at SA node, decreased rate of diastolic depolarization (decreased cardiac rate)
- at AV node, decreased conduction rate
- at atrial muscle, no significant effect
- at ventricular muscle, no significant effect
48
New cards
arteries
- transport blood away from the heart
- thick muscle layer
- blood being ejected from heart is under high pressure
- elastic fibers expand when blood pressure rises and recoils when blood pressure falls
- artery--> arteriole--> cappilary
- thick muscle layer
- blood being ejected from heart is under high pressure
- elastic fibers expand when blood pressure rises and recoils when blood pressure falls
- artery--> arteriole--> cappilary
49
New cards
veins
- carry blood to the heart
- thin muscle layer (can expand very large and store blood-capacitance); larger than artery
- contain one way valves to ensure blood returns to heart
- blood flowing through at much lower pressure
- no elasticity needed bc under low pressure
- vein--> venule--> capillary
- thin muscle layer (can expand very large and store blood-capacitance); larger than artery
- contain one way valves to ensure blood returns to heart
- blood flowing through at much lower pressure
- no elasticity needed bc under low pressure
- vein--> venule--> capillary
50
New cards
capillaries
- smallest blood vessel; usually one cell layer thick
- allow gas exchange between blood and interstitial fluid
- allow gas exchange between blood and interstitial fluid
51
New cards
endothelium
- thin layer of epithelium that lines inside of blood vessels; or only layer for capillaries (one layer makes easy for gas exchange to occur)
52
New cards
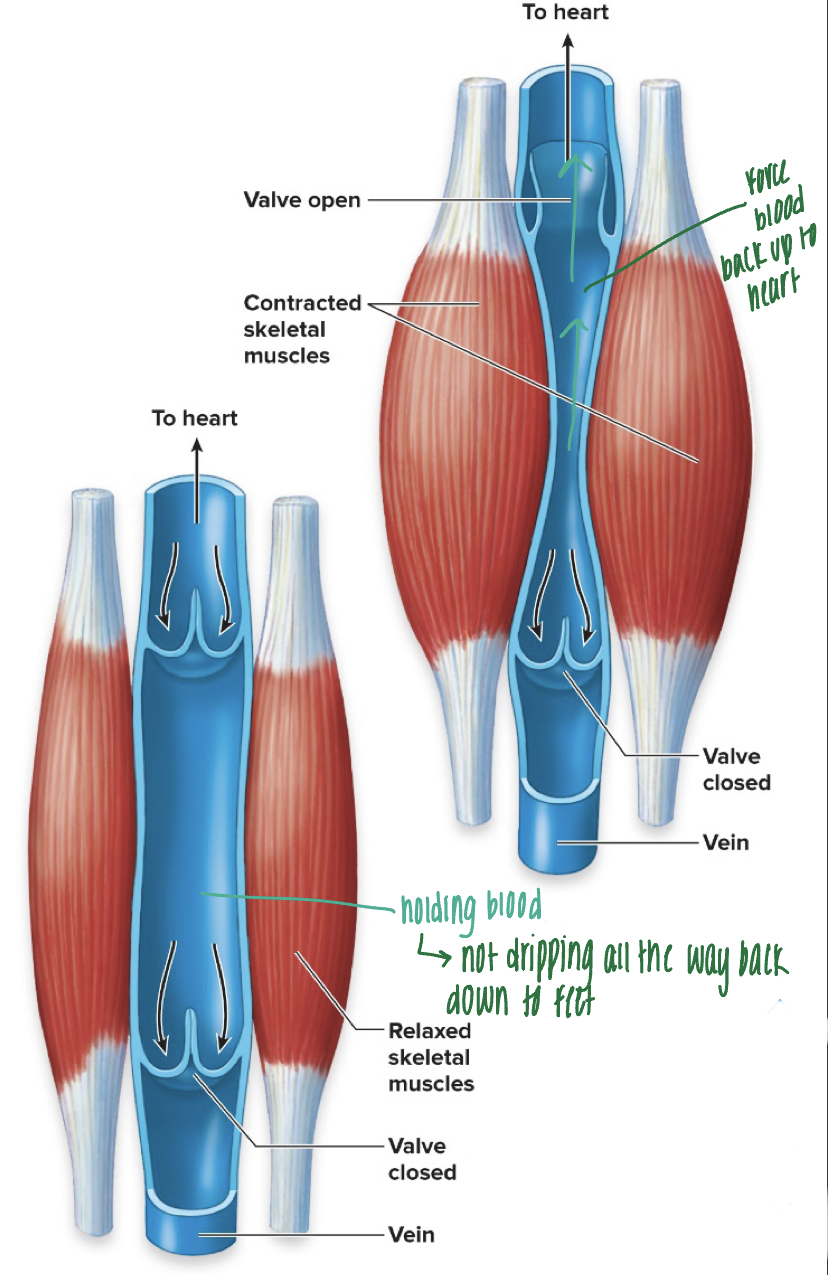
venous valves
- veins contain valves (similar to SL valves) that prevent the flow of blood away from the heart
- veins have large diameter, therefore very low pressure, and need help from skeletal muscles to pump blood back to heart - "skeletal muscle pump" or "venous return"
- when not using skeletal muscles much, blood accumulates in the veins--> causing them to bulge
- veins have large diameter, therefore very low pressure, and need help from skeletal muscles to pump blood back to heart - "skeletal muscle pump" or "venous return"
- when not using skeletal muscles much, blood accumulates in the veins--> causing them to bulge
53
New cards
capillary beds
- site of exchange of fluid, nutrients, and wastes
- blood flow in capillaries is slow; allows time for exchange of substances between the blood and surrounding tissues
- all over the body
- capillary walls are composed of just one cell layer; simple squamous epithelium (endothelium); allows more rapid exchange of materials to/from tissues
- blood flow in capillaries is slow; allows time for exchange of substances between the blood and surrounding tissues
- all over the body
- capillary walls are composed of just one cell layer; simple squamous epithelium (endothelium); allows more rapid exchange of materials to/from tissues
54
New cards
lymphatic system
- comprised of lymph, lymphatic vessels, and lymphoid organs
- follows circulatory system; lymph vessels are located around blood vessels
- important in transport of immune cells and regulation of fluid balance
- takes up excess tissue fluid and returns it to the blood
- follows circulatory system; lymph vessels are located around blood vessels
- important in transport of immune cells and regulation of fluid balance
- takes up excess tissue fluid and returns it to the blood
55
New cards
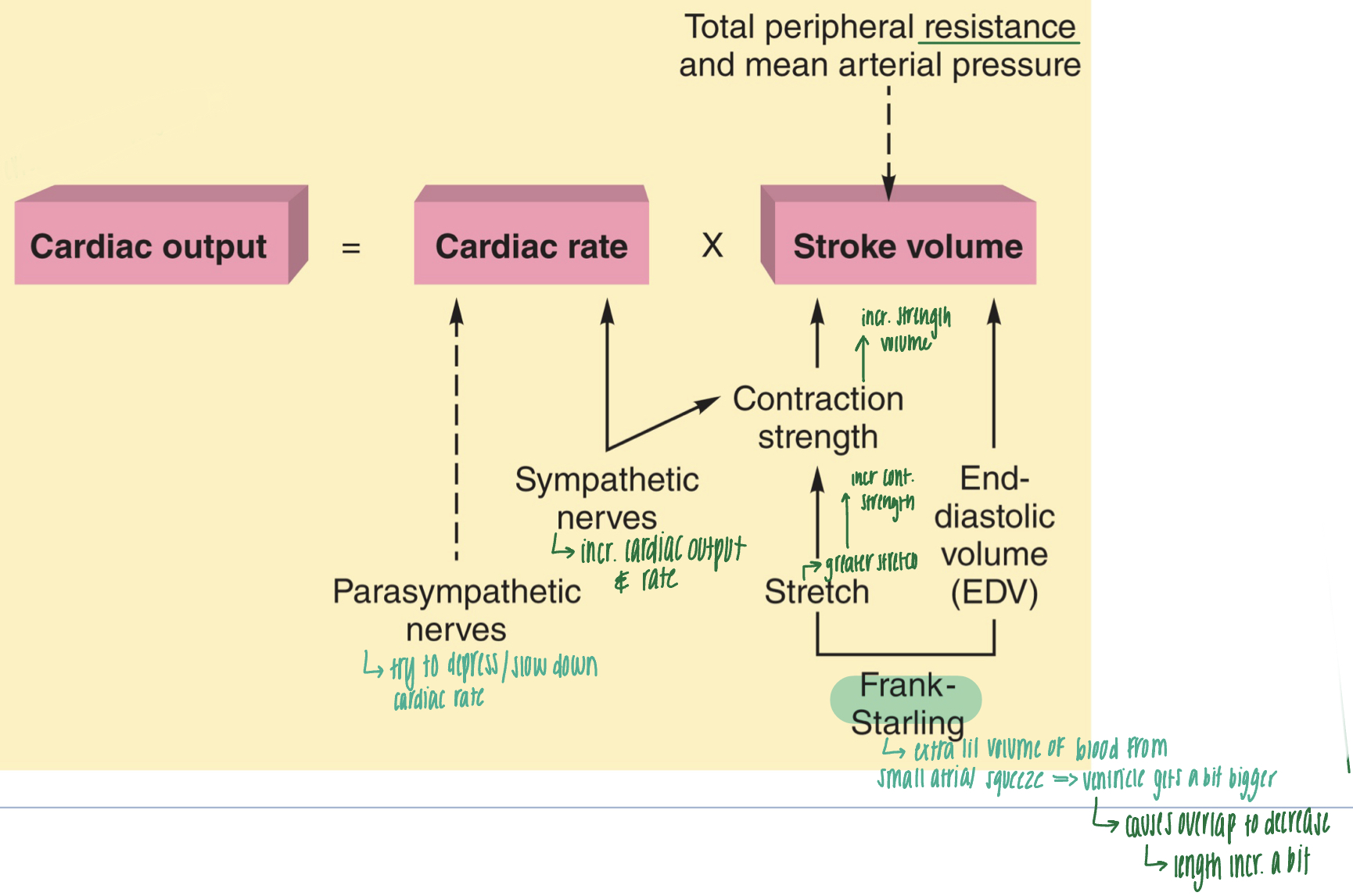
cardiac output
- volume of blood pumped per minute by each ventricle
- cardiac output= cardiac rate x stroke volume
- sympathetic nerves increase cardiac rate--> increase cardiac output
- parasympathetic nerves try to depress/slow down cardiac rate
- end diastolic volume (EDV): volume of blood in ventricle right before it contracts (relaxed; should be full); effects stroke volume
- frank starling: extra lil volume of blood from small atrial squeeze--> ventricle gets bigger and causes overlap to decrease
- stretch: when the ventricle is full, the myocardium stretches. the greater the stretch, the more forceful the contraction (greater stretch--> increase contraction strength--> increase stroke volume--> increase cardiac output)
- total peripheral resistance and mean arterial pressure affect stroke volume
- cardiac output= cardiac rate x stroke volume
- sympathetic nerves increase cardiac rate--> increase cardiac output
- parasympathetic nerves try to depress/slow down cardiac rate
- end diastolic volume (EDV): volume of blood in ventricle right before it contracts (relaxed; should be full); effects stroke volume
- frank starling: extra lil volume of blood from small atrial squeeze--> ventricle gets bigger and causes overlap to decrease
- stretch: when the ventricle is full, the myocardium stretches. the greater the stretch, the more forceful the contraction (greater stretch--> increase contraction strength--> increase stroke volume--> increase cardiac output)
- total peripheral resistance and mean arterial pressure affect stroke volume
56
New cards
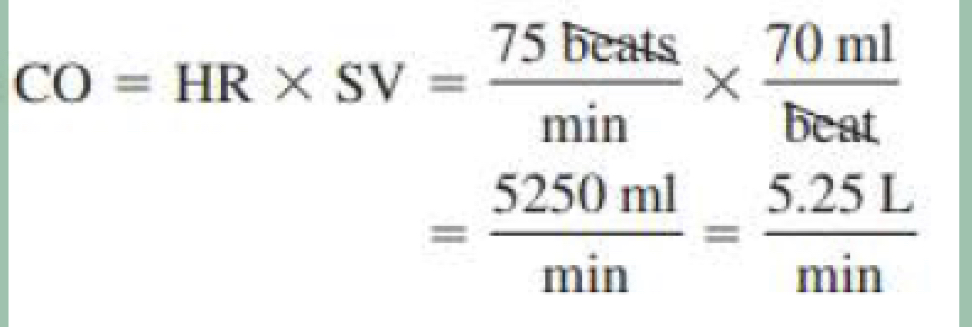
normal cardiac output of person at rest
resting heart rate= 75 beats/min
stroke volume (volume being pushed out) = 70ml/beat
stroke volume (volume being pushed out) = 70ml/beat
57
New cards
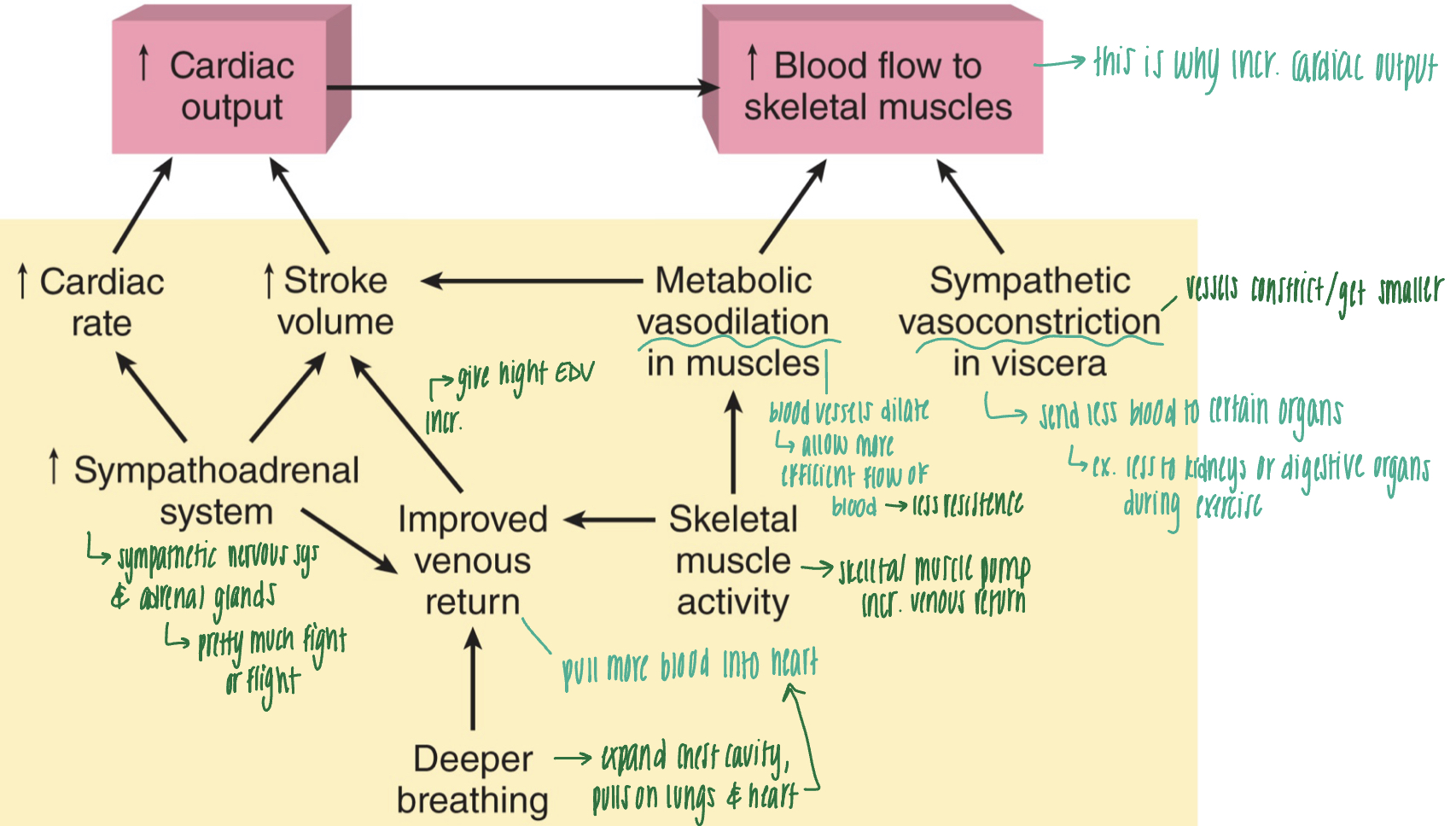
cardiac output during exercise
- deeper breathing: expand chest cavity, which pulls on lungs and heart, pulling more blood into the heart--> improved venous return
- skeletal muscle activity --> skeletal muscle pump increases venous return
- improved venous return increases stroke volume
- increase in sympathoadrenal system (pretty much fight or flight) increases venous return, cardiac rate, and stroke volume --> increased cardiac output
- increase cardiac output to increase blood flow to skeletal muscles
- sympathetic vasoconstriction in viscera: vessels constrict/get smaller so less blood is sent to other organs and more is sent to skeletal muscles
- metabolic vasodilation in muscles: blood vessels dilate, allowing blood to flow more efficiently and with less resistance: increase stroke volume
- skeletal muscle activity --> skeletal muscle pump increases venous return
- improved venous return increases stroke volume
- increase in sympathoadrenal system (pretty much fight or flight) increases venous return, cardiac rate, and stroke volume --> increased cardiac output
- increase cardiac output to increase blood flow to skeletal muscles
- sympathetic vasoconstriction in viscera: vessels constrict/get smaller so less blood is sent to other organs and more is sent to skeletal muscles
- metabolic vasodilation in muscles: blood vessels dilate, allowing blood to flow more efficiently and with less resistance: increase stroke volume
58
New cards
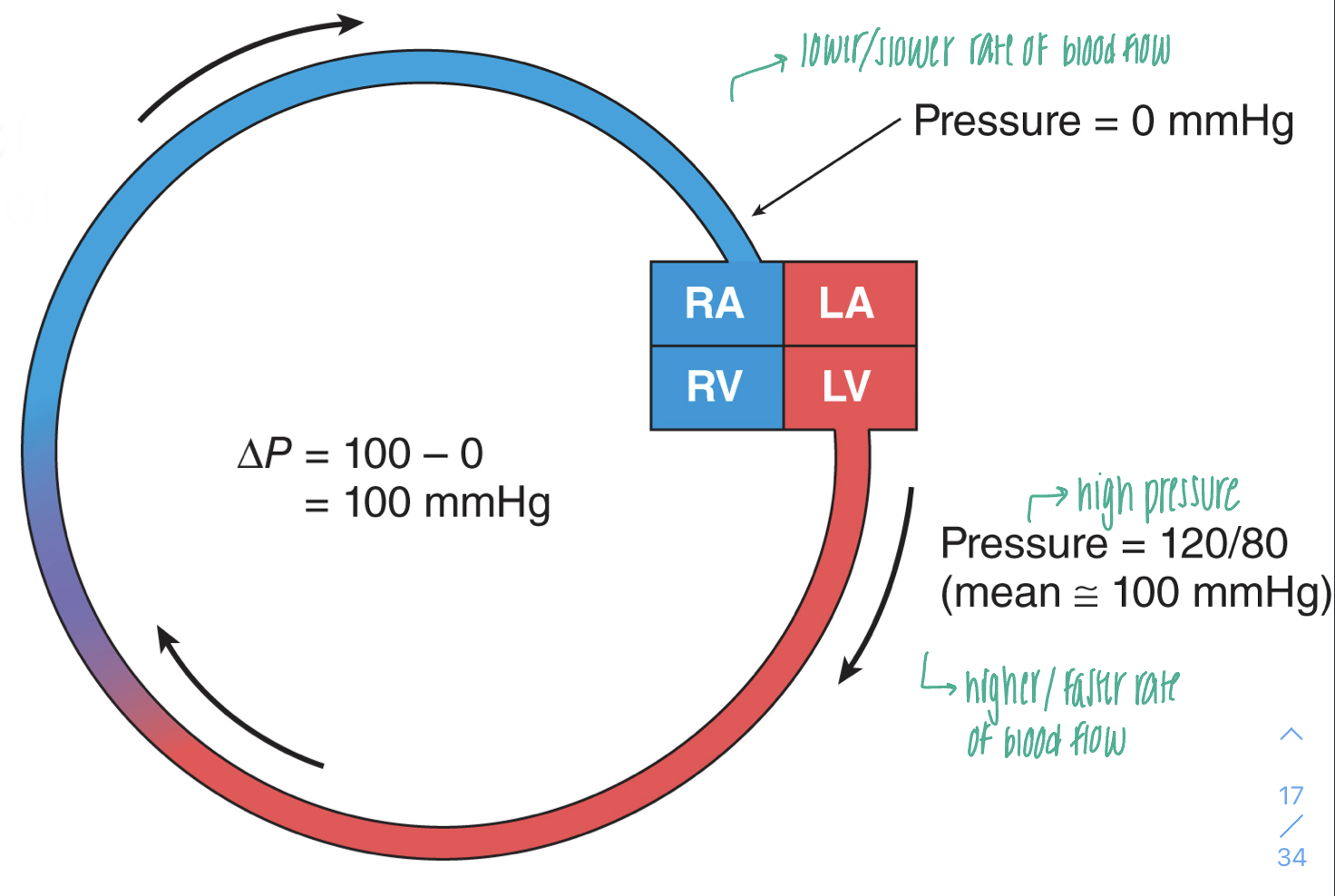
pressure and blood flow
- blood flows from a region of higher pressure (arteries) to a region of lower pressure (veins); pressure gradient pushing blood forward
- the rate of blood flow is proportional to the difference in pressure
- the rate of blood flow is proportional to the difference in pressure
59
New cards
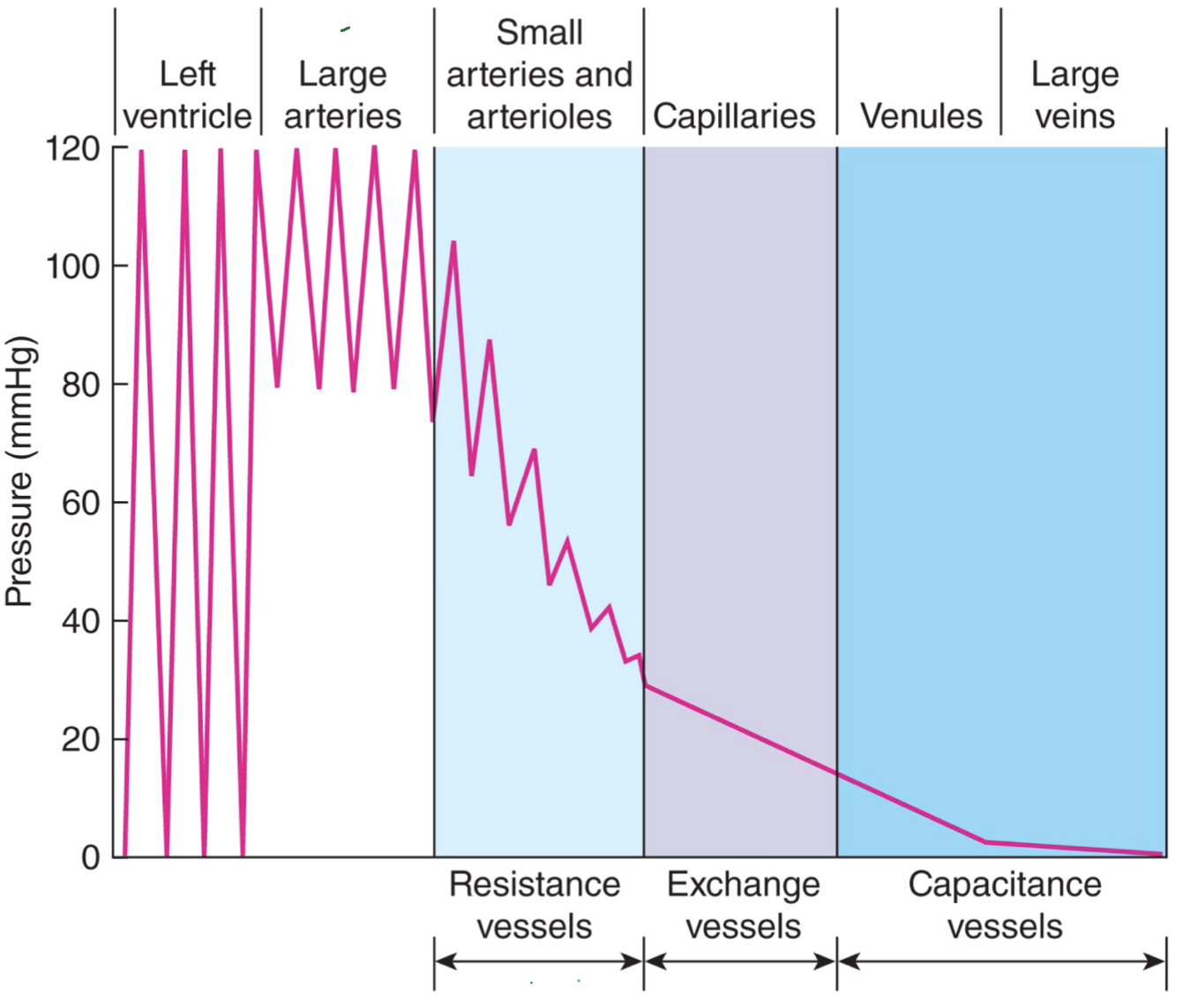
pressure differences in systemic circulation
- left ventricle: high pressure
- large arteries (aorta): still pretty high pressure
- small arteries and arterioles: "resistance vessels"- still seeing higher pressures
- capillaries: "exchange vessels"- still some pressure bc need to be abel to force stuff out
- venules and large veins: "capacitance vessels"- very low or no pressure; store lots of blood
- large arteries (aorta): still pretty high pressure
- small arteries and arterioles: "resistance vessels"- still seeing higher pressures
- capillaries: "exchange vessels"- still some pressure bc need to be abel to force stuff out
- venules and large veins: "capacitance vessels"- very low or no pressure; store lots of blood
60
New cards
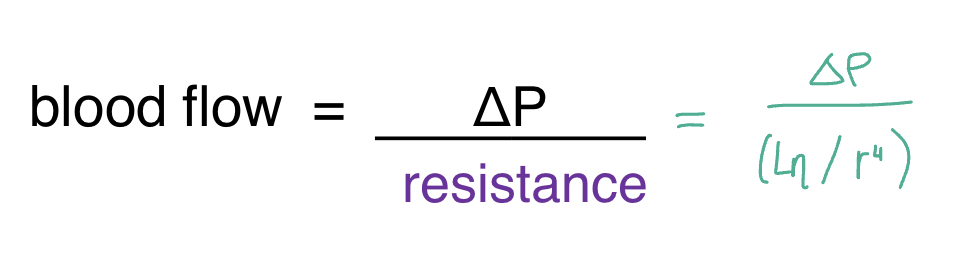
physical laws of describing blood flow
- the rate of blood is inversely proportional to the frictional resistance to blood flow within the vessels: blood flow= (pressure difference/resistance); higher/greater the RESISTANCE, the LOWER the blood flow and the higher/greater the PRESSURE, the GREATER the flow
- resistance = (length of vessel x viscosity)/radius of the blood vessel ^4; larger radius will decrease resistance and increase flow
- double the radius: resistance is 1/16R and blood flow is 16F
- half the radius: resistance is 16R and blood flow is 1/16 F
- resistance = (length of vessel x viscosity)/radius of the blood vessel ^4; larger radius will decrease resistance and increase flow
- double the radius: resistance is 1/16R and blood flow is 16F
- half the radius: resistance is 16R and blood flow is 1/16 F
61
New cards
venous return
- veins have high compliance/capacity: stretch more at a given pressure than arteries bc have thinner walls
- capacitance vessels : 2/3 of total blood volume is in veins
- hold more blood than arteries, but maintain lower pressure
- capacitance vessels : 2/3 of total blood volume is in veins
- hold more blood than arteries, but maintain lower pressure
62
New cards
body water distribution
- osmotic forces control the mvmt of water between interstitial spaces and the capillaries, affecting blood volume
- urine formation and water intake play role in blood volume
- fluid is always circulating in a state of dynamic equilibrium
- urine formation and water intake play role in blood volume
- fluid is always circulating in a state of dynamic equilibrium
63
New cards
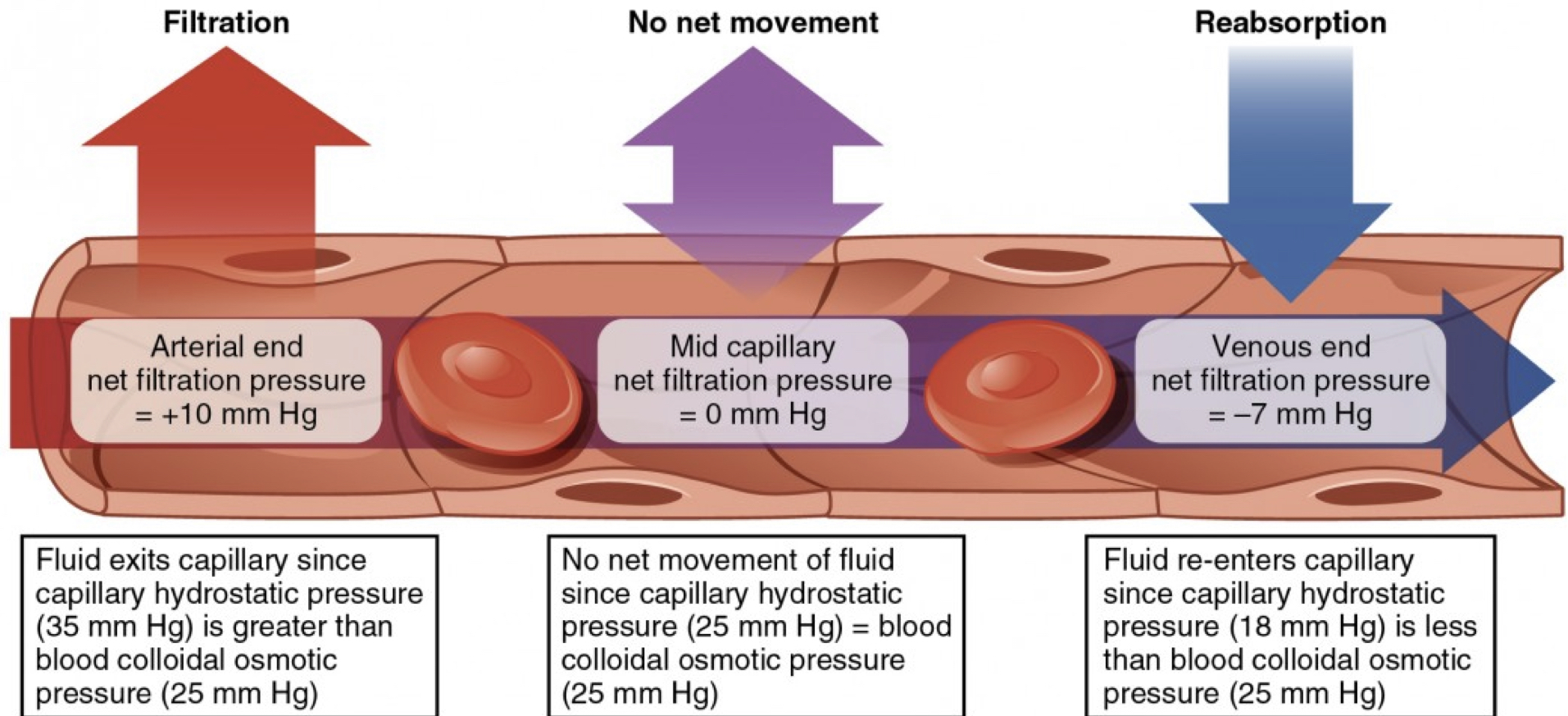
tissue capillary fluid exchange
- net filtration pressure= the hydrostatic pressure of the blood in the capillaries minus the hydrostatic pressure of the fluid outside the capillaries
- arterial end: higher pressure, therefore fluid is forced out (filtration)
- venous end: fluid in tissue at higher pressure and inside capillary is lower pressure, therefore fluid moves in (reabsorption)
- arterial end: higher pressure, therefore fluid is forced out (filtration)
- venous end: fluid in tissue at higher pressure and inside capillary is lower pressure, therefore fluid moves in (reabsorption)
64
New cards
edema
- excessive accumulation of interstitial fluids
- water going out of capillaries/circulatory system and not going back in, therefore filling interstitial space
- may be a result of: high arterial blood pressure, venous obstruction, leakage of plasma proteins into interstitial space, decreased plasma protein concentration
- water going out of capillaries/circulatory system and not going back in, therefore filling interstitial space
- may be a result of: high arterial blood pressure, venous obstruction, leakage of plasma proteins into interstitial space, decreased plasma protein concentration