Pharmacology - Bacterial Disease and Antibiotics
1/168
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
169 Terms
Bacteremia
bacteria in the blood stream
Sepsis
bacteremia with toxins causing systemic symptoms/signs
What is this referring to
Gram stain – Gram + (purple) or Gram – (pink) based on membrane constituents
Oxygen requirements – aerobic or anaerobic
Shape
Coccus (pl-cocci) - spherical
Bacillus (pl-bacilli) – rod-like
Spirochete (pl- “-s”) – spiral
Environment – intracellular or extracellular
Atypical
Different classifications of bacteria (prokaryotes)
What cell envelop components are found in both gram-positive and gram-negative bacteria
cytoplasmic membrane and cell wall
What bacteria (gram pos or neg) have a thicker cell wall and outer membrane
gram negative
What maintains bacterial shape and protects it from osmotic lysis if it is placed in a hypotonic medium
Cell wall
________ are more active against rapidly dividing bacteria than they are against bacteria in the resting or stationary phase
Drugs that inhibit cell wall synthesis
What reduces the effectiveness of cell wall inhibitors
concurrent administration of bacteriostatic antibiotics that slow the growth of bacteria
What is – hair-like projections on the bacterial surface
Adhere to cells
Invade tissue
Adhere to other bacteria
Pili (aka fimbria)
What is —- rotary, whip-like extension
Mobility
Adhesion
Flagella
What proteins which aid in breeching the cell’s defenses
Enzymes
What – protect the bacteria from immune system
capsule
What – dormant and highly resistant (unaffected by heat,
Spores
What has a – slimy matrix secreted by bacteria to protect from immune system
Biofilm
What poisons cells
Toxins
What is this referring to
Part of the cell wall of Gram-bacteria which may be released during growth or antibiotic treatment
Good news – at low levels, helps stimulate immune reaction
Bad news – at high levels, cause release of cytokines and activate clotting cascade
Endotoxin
What is produced inside bacteria and secreted
The bad news is there is no good news.
May damage cell walls
Or enter cells and change their function
Examples:
Botulinum toxin
Coagulases
Exfoliative
Enterotoxins
Exotoxin
What is this referring to
Enzymes – such as proteases which digest plasma proteins
Capsules – prevent phagocytosis
Horizontal gene transfer- bug to bug
Bacteriophages –viruses
Plasmids – nonchromosome DNA that move between bacteria by conjugation (fusion with pili)
Biofilm – organized extracellular slime of matrix and bacteria+fungi
Implanted devices, teeth, epithelium
Mechanisms of evasion
What is this referring to
Enzymatic inactivation or modification of drug
Decreased drug uptake or accumulation
Altered or lack of target receptor site
Circumvention of drug action sequences
major mechanism of bacterial antimicrobial resistance
What is this referring
Beta-lactamase hydrolysis of beta-lactam ring
Modification of aminoglycosides by acetylating, adenylating, or phosphorylating enzymes
Enzymatic inactivation or modification of drug
What is this referring to
Lack of outer membrane permeability (intrinsic or acquired)
Faulty or lacking antibiotic uptake and transport systems
Antibiotic efflux system (e.g. tetracycline resistance)
Decreased drug uptake or accumulation
What is this referring to
Altered PBP’s (beta-lactam resistance)
Altered ribosomal target (aminoglycoside, macrolides, etc.)
Altered enzymatic target (sulfa, trimethoprim, rifampin, quinolones)
Altered or lack of target receptor site
What is this referring to
Hyperproduction of drug targets or competitive substrates (Bactrim resistance)
Circumvention of drug action sequences
What is it called when the antibiotic exerts its killing effect as long as the concentration remains above the mic
Ex: beta-lactams and vancomycin
Interval dependent killing (time dependent killing)
What is the antibiotic continues to exert its killing effect after the concentration has fallen below the bacteria’s mic (post antibiotic effect). The higher the peak, the greater the killing effect
Ex: Aminoglycosides and fluoroquinolones
Concentration dependent killing
Nonpathogenic microorganisms adapted to grow on body surfaces of the host, forming part of the normal flora
Body surfaces
Skin (staph epidermidis, diptheroids)
Mucous membranes (e. coli, klebsiella)
Function
Digestive aids
Prevents excessive overgrowth of dangerous bacteria
Synthesis of essential metabolites
Commensals
Microorganisms that do not usually produce disease in healthy individuals, but are involved in human infections when the host’a immune system is weakened or compromised
Transient visitors of the throat
Strep pneumoniae, Group a strep, neisseria meningitidis, hemophilus influenzae, klebsiella pneumoniae
Normal residents of the GI tract
Escherichia coli, klebsiella pneumoniae, citrobacter fruendii, etc.
Opportunists
Microorganisms that can produce disease or tissue damage by their mere presence regardless of the condition of the host
Staphylococcus aureus
Salmonella typhi, S. enteriditis
Treponema pallidum
Mycobacterium tuberculosis
Shigella
True pathogens
What does this refer to
Determine the site of infection
Evaluate host characteristics (age, immunocompromise, comorbidities)
Determine most likely causative bacteria
General antibiotic principles for diagnosis
What is this referring to
Prophylactic
Empiric
Definitive
General antibiotic principles for treatment
Prophylactic
prevention
Empiric
best educated guess, based on clinical presentation and probable organism
Definitive
targeted, based on cultures and sensitivities
What is this referring to
Susceptible
Intermediate
Resistant
MIC – Minimum inhibitory concentration (concentration that inhibits visible bacterial growth @ 24 hr.)
MBC (Minimum bactericidal concentration)
concentration that results in 1,000-fold reduction in bacterial density @ 224 hr
Bioavailability
difference between IV and PO routes
What prevents growth of bacteria (remain in stationary phase and doesn’t replicate)
Usually by inhibiting protein synthesis (sulphonamides, TCN, macrolides)
Require the host’s immune system to clear the infection
Bacteriostatic
What actively kills bacteria
Primarily act on the cell wall (beta-lactams) or cell membrane (daptomycin)
Necessary in severe (endocarditis), life-threatening (sepsis), or hard to cure infections (osteomyelitis)
Bactericidal
Almost all Abx potentiate (increase the power) of ________ (a vitamin K antagonist anticoagulant) by inhibiting vitamin K producing intestinal flora
Warfarin
What bind cations (Mg, Ca) in the gut (antibiotic interactions)
Flouroquinolones
What interaction can lower efficacy of oral contraceptives
antibiotics (interaction)
What causes allergic reactions
Rashes, hives
Hypersensitivity reactions
Adverse drug reactions
Abx are most common drugs to cause life-threatening immune-mediated reactions
To prevent antibiotic reactions, one must avoid ______
drugs in the same class (PCN and beta-lactams)
What is this referring to
Gram + aerobe
Most virulent of the staph species
Produce penicillinases (beta-lactamases)—MSSA
May still use penicillinase stable beta-lactams: methicillin or cephalosporins
MRSA alters the penicillin binding protein (or omits it from chromosomal coding
Beta-lactams will not work
Must use antibiotics with a different mechanism of action (ie vancomycin)
Disease associated with skin and soft tissue infections (abscesses), pneumonia (mostly hospital acquired)
Staphylococcus aureus
What is the following
Furunculosis (“boils”)
Pyogenic suppurative lesion
Infection of the hair follicle or seat gland
Stye
Carbuncles
Bullous impetigo
Paronychia
Deep tissue infections
Osteomyelitis
Bacterial pneumonia
endocarditis
Staphylococcal infections
What is the following
Ritter’s disease (scalded skin syndrome)
Toxic shock syndrome
Staphylococcal food poisoning
Diseases caused by staphylococcal toxins
What is this referring to
—”incomplete hemolysis”
Strep pneumoniae: usually ”diplococcus” – has polysaccharide capsules
Strep viridans: grows in chains; usually commensal
Doesn’t usually cause infection but if it does mouth and nasopharynx usually involved
Alpha hemolysis
What is this referring to
—”complete hemolysis”
Strep pyogenes
Strep agalactiae
Beta hemolysis
What is this referring to “non-hemolytic”
Gamma hemolysis
What are grown on sheep’s blood agar producing three patterns of hemolysis around the colonies
Streptococci (brown groups)
What is this referring to
Most common pathogens
Viruses
Strep pyogenes (15%) or other hemolytic strep
Arcanobacterium hemolyticum
Neisseria gonorrhea
Chlamydia pneumoniae
Epstein-barr virus
Pharyngitis (streptococcal diseases)
What is this referring to
Upper respiratory infections
Sinusitis
Otitis media
Impetigo
Strep is most common cause
May see staph aureus as a secondary invader
Erysipelas
Wound and burn infections
Scarlet fever
Immunologic sequellae
Rheumatic fever
Acute glomerulonephritis
Cellulitis
Necrotizing fasciitis
Pneumococcal meningitis
Streptococcal diseases
What is this referring to
Gram +
E. faecalis***
E. faceium***
Normal inhabitants of GI tract
Able to survive harsh conditions
Typically very resistant
Vancomycin resistant enterococcus (VRE)
Must usually treat synergistically
Opportunistic organisms capable of causing UTI’s wound infections, endocarditis
Enterococcus
What is this referring to
Cannot thrive in the presence of oxygen
Do not contain enzymes to defend against oxygen—peroxidase, catalase, superoxide dismutase
Anaerobes
What is this referring to
Anaerobe that produces toxins that cause other effects; spore forming
C. botulinum
C. tetani
C. perfringens
C. difficile***
Clostridia
What is this referring to
Aka “gram negative rods”, aerobes
Large, diverse group of gram negative rods found in nature and as part of the normal flora of man and animals
Opportunistic pathogens but some are specifically pathogenic (e. coli)
E.coli is the most prominent of this group followed by klebsiella and proteus
True pathogens include: salmonella, shigella, e. coli, yersinia
Enteric bacilli (Enterobacteriaceae)
What is this referring to
Normal flora
Gram negative aerobe
Most common cause of urinary tract infections
Causes opportunistic infections
Diarrheagenic
Caution: septic shock (lipopolysaccharide)
E. coli
What is this referring to
Gram negative aerobes
Virulence
Endotoxin
Flagella
Urease production
Resistance
Some beta lactamase production
Disease
UTI’s – cystitis and pyelonephritis
urolithiasis
Proteus mirabilis
What is this referring to
Multiple antibiotic resistance mechanisms—extremely challenging to treat
Harbored in moist environments—hot tubs, swimming pools
Common secondary infection with cystic fibrosis
Diseases
Pneumonia
Burn wound infections—typically cause a black/green discoloration
Endocarditis
Otitis externa
Osteomyelitis
UTI’s—cystitis and pyelonephritis
Pseudomonas aeruginosa
What is this referring to
A type bacterial resistance due to the production of an enzyme or chemical capable of destroying most beta-lactam antibiotics
Typically seen in gram negative microbes
Often due to exposure to broad spectrum antibiotics (those covering lots of gram negative organisms)
Bacteria which produce ESBL’s are part of the multi-drug resistant organisms (MDRO’s)
Common exhibitors of ESBL:
E.coli
Pseudomonas aeruginosa
Proteus mirabilis
Klebsiella pneumonia
Also known to be producers of Carbapenemases (KPC)
Can be extremely resistant microbes
Extended Spectrum Beta-Lactamase (ESBL)
What is this referring to
Beta-Lactams
Penicillins
Cephalosporins
Carbapenems
Vancomycin
Cell Wall Inhibitors (antibiotics)
What is this referring to
Tetracyclines
Fluoroquinolones
Macrolides
Aminoglycosides
Folate Inhibitors
Protein Synthesis Inhibitors (Antibiotics)
What binds to a group of bacterial enzymes, the PBPs (PCN binding proteins)
inhibit cross-linking of peptidoglycan
Each bacterial species has a set of unique PBPs to which particular β-lactam antibiotics bind with varying affinities
B-Lactam Drugs
What is are responsible for the assembly, maintenance, and regulation of the peptidoglycan portion of the bacterial cell wall
Creates a lattice meshwork that provides structure and stability to the microbe
Penicillin Binding Proteins (PBPs)
What includes penicillin G and penicillin V
Narrow-spectrum penicillins
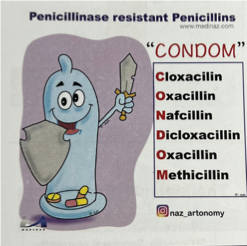
What includes oxacillin, cloxacillin, dicloxacillin, & nafcillin
Good treatment option for Methicillin-Sensitive Staph Aureus (MSSA)
Rarely used unless confirmation of MSSA for step down therapy
Penicillinase-resistant penicillins
What includes amoxicillin, ampicillin, piperacillin, and ticarcillin
Amoxicillin and Ampicillin are often used for gram positive infections and mild gram-negative infections
Piperacillin and Ticarcillin have activity against Pseudomonas
Extended-spectrum penicillins
What are adverse effects of B-Lactam Drugs
Penicillins are a common cause of drug-induced hypersensitivity reactions.
True penicillin allergy occurs in only 7% to 23% of patients who give a history of penicillin allergy.
Hypersensitivity reactions occur when penicillin is degraded to penicilloic acid and other compounds that combine with body proteins to form antigens that elicit antibody formation
What is this referring to
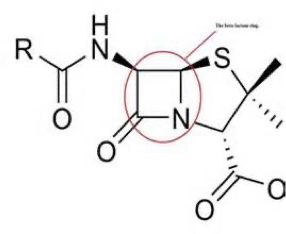
Penicillin (beta lactam ring plus a thiazolidine ring)
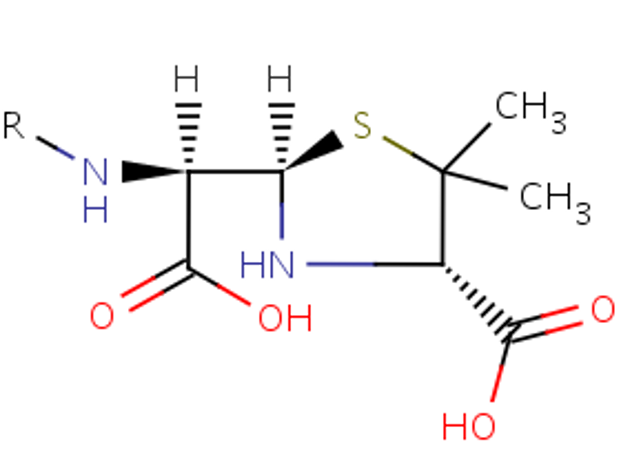
What is this referring to
Penicilloic Acid
What is likely to cause cause a maculopapular skin rash with certain viral infections, such as mononucleosis (mediated by sensitized lymphocytes). Its incidence in ______-treated patients with mononucleosis is over 90%
Ampicillin
An immediate hypersensitivity reaction, which is a type of reaction mediated by Ig E, can lead to urticaria (hives) or anaphylactic shock. Other types of hypersensitivity reactions can lead to serum sickness, interstitial nephritis, hepatitis, and various skin rashes.
B-Lactam Drugs Adverse Effects
What can be confirmed by the use of commercial preparations of ____ antigens.
These preparations contain the major or minor antigenic determinants of penicillin that are formed in the body during ______ degradation.
Injected intradermally and cause erythema at the injection site in allergic persons.
Should be administered by personnel who are prepared to provide treatment for anaphylactic shock in the event that the patient develops a severe hypersensitivity reaction
Penicillin allergy
What is this referring to
Except for hypersensitivity reactions, the _______ are remarkably nontoxic to the human body and produce very few other adverse effects.
________ can disturb the normal flora of the gut and produce diarrhea and superinfections with _______-resistant organisms, such as staphylococci and Clostridium difficile.
Penicillin
Penicillin in association with C. difficile superinfections can cause
Pseudomembranous collitis
What is this referring to
has little IF ANY antimicrobial effects itself but is used on beta-lactamase producing microbes to tie up enzymes (serve as surrogate substrates)
Is the only oral B-Lactamase inhibitor
Effective on H. influenza, N. gonorrheae, E. coli, Salmonella, Shigella, Staphylococcus, Klebsiella, Bacteroides fragilis, and Legionella.
Does not inhibits beta-lactamases from Enterobacter, Serratia, Morganella, Citrobacter, Pseudomonas, & Acinetobacter.
Clavulanic acid/Clavulanate
What B-Lactamase Inhibitor is used with ampicillin (Unasyn)
parenteral
Sulbactam
What B-Lactamase Inhibitor is used with piperacillin (Zosyn) and ticarcillin (Timentin)
parenteral
Tazobactam
What is this referring to
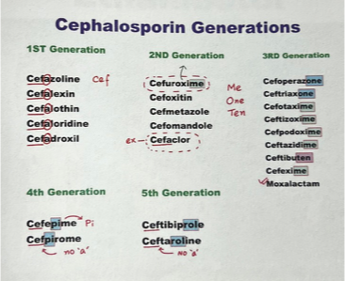
One of the largest and most widely used groups of antibiotics; four generations ; semisynthetic drugs
First-generations are primarily active against gram-positive cocci and a few gram-negative bacilli.
Subsequent generations have increased activity against gram-negative bacilli and less activity against some species of gram-positive cocci.
Cephalosporins (B-Lactam Drugs)
What have good activity against most streptococci and methicillin-sensitive staphylococci; also a few gram-negative enteric bacilli, including E. coli and Klebsiella pneumoniae
What has similar activity against gram-positive cocci with increased activity against gram-negative bacilli.
Second-generation cephalosporins (Ceclor, Cefzil, Ceftin)
What has a greater activity against a wider range of gram-negative organisms, including enteric gram-negative bacilli (Enterobacteriaceae), H. influenzae, and M. catarrhalis
Third-generation cephalosporins (Rocephin, Vantin)
What is active against many gram-negative bacilli, including Citrobacter freundii and Enterobacter cloacae, that are resistant to other cephalosporins
Cefepime (Maxipime) has been called a fourth-generation cephalosporin
What generation of cephalosporins is used for UTI, mild skin or soft tissue infections, otitis media, upper and lower respiratory tract infections
1st generation cepahlosporins
What generation of cephalosporins is used for Sinusitis, otitis media, lower respiratory tract infections
2nd generation cephalosporins
What generation of cephalosporins is used for Meningitis, febrile neutropenia, community acquired pneumonia
3rd generation cephalosporins
What generation of cephalosporins is used for Meningitis, febrile neutropenia, pneumonia, nosocomial infections
4th generation cephalosporins
What generation of cephalosporins is used for resistant infections
5th generation
What generation of cephalosporins does this belong to
Cefadroxil (Duracef) - oral
Cefazolin (Ancef)**- IV
Cephalexin (Keflex)**- oral
Cephapirin – IV
Cephradine - oral
1st generation cepahlosporins
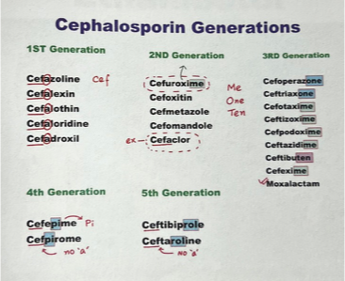
What generation of cephalosporins does this belong to
Cefaclor (Ceclor)**- oral
Cefamandole (Mandol)- IV
Cefotetan (Cefotan)- IV
Cefoxitin (Mefoxin)- IV
Cefprozil (Cefzil)- oral
Cefuroxime (Ceftin)**- oral, IV
Cefmetazole - IV
2nd generation cepahlosporins
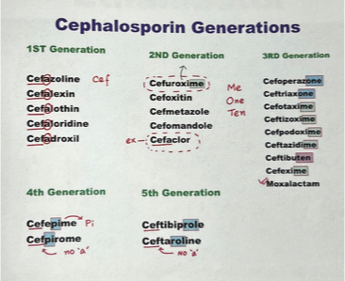
What generation of cephalosporins does this belong to
Cefdinir (Omnicef)**- oral
Cefditoren (Spectracef)**-oral
Cefixime (Suprax)- oral
Cefotaxime (Claforen)- IV
Cefpodoxime (Vantin)- oral
Ceftazidime (Fortaz)**- IV
Ceftizoxime (Cefizox)- IV
Ceftriaxone (Rocephin)- IV
Cefoperazone (Cefobid) – IV
Ceftibuten (Cedax) - oral
3rd generation cepahlosporins
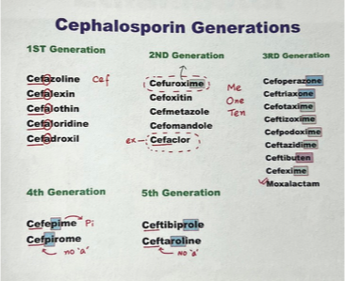
What generation of cephalosporins does this belong to
Cefepime (Maxipime)**, Cefluprenam, cefozopran, cefpirome
Gram-positive: similar activity against Gram + organisms as 1st generation cephs
Gram-negative: have a greater resistance to beta-lactamases than 3rd generation cephs. Many can cross the BBB and are effective in meningitis. Effective against pseudomonas aeruginosa
4th generation cepahlosporins
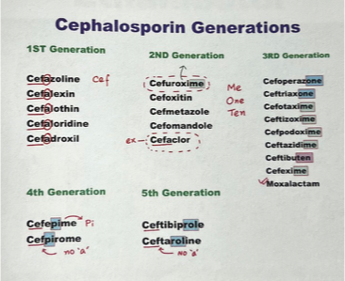
What generation of cephalosporins does this belong to
ceftobiprole (Zeftera)
Advantage is activity against MRSA, pseudomonas and Enterococci
Ceftaroline (Teflaro)
Broad spectrum coverage against gram+ and gram – esp. MRSA & VRSA
5th generation cepahlosporins
What does this refer to
Although can elicit hypersensitivity reactions, the incidence of this is lower than for penicillins.
________ exhibit some cross-sensitivity with penicillins, and about 5% of persons allergic to penicillin will also be allergic to cephalosporins.
Persons who have had a mild hypersensitivity reaction to penicillin usually do not cross-react to a _______; a severe hypersensitivity reaction to penicillin (e.g., an anaphylactic reaction) has a greater risk of cross-reacting and should usually not be given a _________.
Cephalosporins
What does this refer to
Aztreonam (Azactam) is a monocyclic β-lactam (monobactam) antibiotic.
Active against many aerobic gram-negative bacilli, including strains of Enterobacter, Citrobacter, Klebsiella, and Proteus species as well as P. aeruginosa.
IV for very serious infections
Aztreonam can cause hypersensitivity reactions and thrombophlebitis.
Only rarely shows cross-sensitivity with penicillins and cephalosporins, and can usually be used in persons allergic to other β-lactam antibiotics
Monobactam (B-Lactam Drugs)
What does this refer to
________ is a monocyclic β-lactam (monobactam) antibiotic.
________ can cause hypersensitivity reactions and thrombophlebitis.
Aztreonam
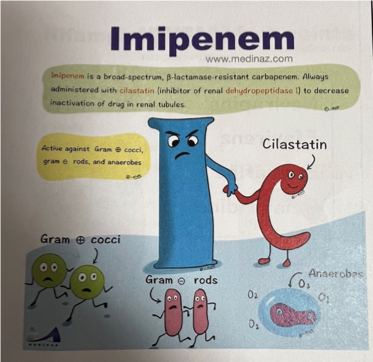
What does this refer to
Bactericidal to a wide range of gram-positive and gram-negatives , including many aerobic and anaerobic gram-negative bacilli
Resistant to most beta-lactamases and are the drugs of choice for infections caused by ESBLs- extended spectrum beta-lactamases
Covers Streptococcus, Staphylococcus, Enterococcus, Listeria, Gram negatives, and anaerobes; All cover Pseudomonas except Ertapenem
Carbapenems
What B-Lactam drugs can cause seizures
Imipenem
What is the Drug of Choice for the treatment for respirator-associated and/or aspiration nosocomial pneumonia in the ICU (DOC for Enterobacter & Serratia)
Meropenem