Epilepsy treatments
1/35
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
36 Terms
What is epilepsy?
A neurological disorder characterised by recurrent seizures due to aberrant high frequency neuronal discharge in the brain.
What causes epilepsy?
-Brain damage (stroke, infection..)
-Hereditary
How can we scan for epilepsy?
EEG
PET scan
How does PET scan work and what does it visualise?
Identifies structural abnormalities that can underly root of seizures and the scan works by detecting gamma rays as a result of a clash of positrons emitted by a radioisotope tracer with electrons in the body.
18-fluoro-2-deoxyglucose: Provides info on brain glucose metabolism
11C-flumazenil: Provides information on GABA-A receptor density
There are two types of epileptic sezures…
-generalised (whole brain)
-focal (part of the brain)
Partial (focal) seizures can spread to form secondary generalised seizures
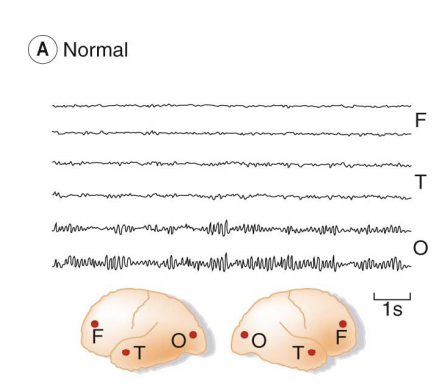
Normal brain activity EEG
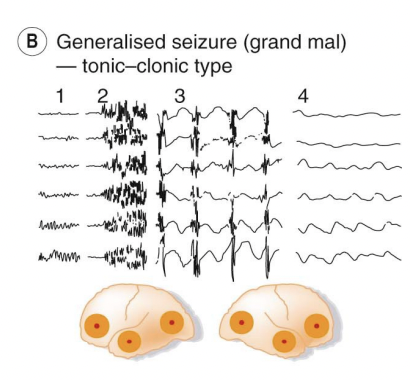
Generalised tonic clonic seizure EEG
Split into 4 phases:
1 – normal activity,
2 – onset of the tonic phase with extensive activity (seen physically by contraction of the whole musculature, respiration ceases, defecation/micturition/salivation, face turns blue),
3 – clonic phase with intermittent discharges (a series of violent, synchronous jerks that die out over a few minutes)
4 – post-convulsive coma with minimal activity in 2 all regions (unconsciousness, followed by waking of patient in a confused and often ill feeling state)
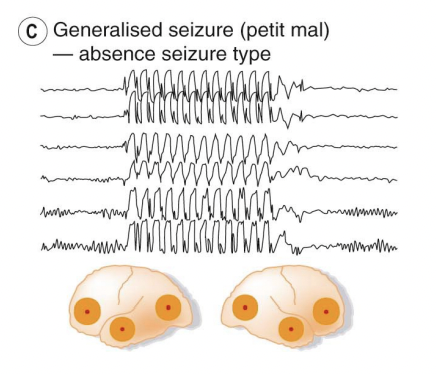
Generalised absence seizure EEG
Activity is altered across all brain regions, patient ceases physically activity, e.g. halts mid-sentence when speaking, recovery occurs with no aftereffects.
The rhythmicity in EEG recording is likely due to oscillatory feedback between cortex and thalamus, which is dependent upon T-type CaVs.
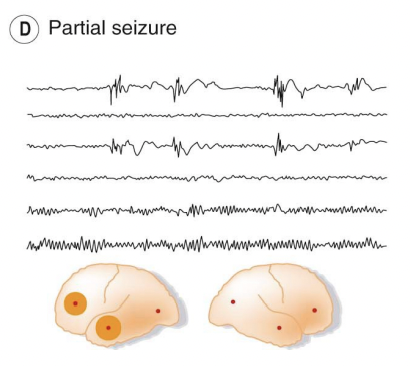
Partial (focal) seizure EEG
Only activity in the 1st and 3rd lines of the recording is changed with synchronous abnormal discharges in the left frontal and temporal regions.
The effects of a partial (focal) seizure depend upon the brain region affected, these are often due to lesions in the brain and are more common with age.
What is a rare form of seizures?
Status epilepticus in which seizure activity is uninterrupted and emergency medical treatment is required (Benzodiazepines midazolam/diazepam/lorazepam (facilitates GABAA), used in status epilepticus where rapid onset of action is desirable, but sedative effect, alongside the tolerance/dependence limits their utility for long-term maintenance.
What was found when studying familial forms of epilepsy?
Genetic variations identified, some due to single mutations, but others being due to numerous mutations.
The mutations often occur in genes encoding ion channels involved in neuronal excitability, e.g. NaVs and GABA receptors, and epileptogenesis occurs if the balance between excitatory and inhibitory neurotransmission is disrupted, i.e. increased excitatory or decreased inhibitory neurotransmission.
What is a paroxysomal depolarising shift?
At the site of epileptic origin, the resting membrane potential of neurones is suddenly observed to depolarise by ~30mV (paroxysmal depolarising shift, PDS – see panel A, right) generating a string of action potentials.
Suggesting that PDS may result from prolonged activity of glutamate and indeed, repetitive seizure activity can lead to neuronal death, possibly through excitotoxicity.
Percentage effects of antiepileptics?
~75% of patients find that antiepileptics control their epilepsy, but ~10% of patients still have monthly seizures, i.e. severely disruptive effect upon their lives.
What are the considerations for treating epilepsy?
-Reducing neuronal excitability and neurotransmitter release.
-Due to continuous medication, often for many years, minimising side effects is highly desirable, but often difficult because the main mechanisms of action involve enhancing GABA function, or inhibiting CaV/NaV function, which would all be expected to produce significant side effects (sedation and fatigue being common).
-Presence of teratogenic and neurodevelopmental side effects has been a challenge, with guidelines in place restricting the use of anti-epileptic medications such as sodium valproate, topiramate and phenytoin.
-Folic acid is recommended for all women on antiepileptic medications who are planning pregnancy, to reduce the risk of neural tube defects.
-Issues may be complicated further by the effect of antiepileptic drugs on hepatic enzymes which metabolise oral contraceptives.
What are targets of antepileptics?
-NaV Blockers
-Synaptic vesicles
-CaV modulation
-Pre-synaptic CaV channels
-Enhanced GABAergic function
NaV Blockers
SCaLLP
Sodium Valproate
Carbamazepine
Lamotrigine
Lacosamide
Phenytoin
Lamotrigine
first or second choice monotherapy for the treatment of tonic-clonic, focal (partial) and absence seizures
Side effect: hypersensitivity reaction-Stephen-Johnson syndrome
Sodium Valproate
Use limited by teratogenic side effects
Also inhibits T-type CaV channels and is a weak inhibitor of GABA transaminase.
Valproate is recommended as a monotherapy for the 5 treatment of tonic-clonic or absence seizures and as an add on therapy for the treatment of focal (partial) seizures.
Side effect: weight gain
Lacosamide
Enhances slow inactivation ( involves structural rearrangement during sustained depolarisation, i.e. as in PDS) so fewer NaVs are available for activation.
Recommended as a further monotherapy for the treatment of focal (partial) seizures and as an add on therapy for the treatment of tonic-clonic seizures.
Side effect: mood and behavioural changes
Carbamazepine
Recommended as a further monotherapy for the treatment of focal (partial) seizures. Carbamazepine induces hepatic enzymes (CYP450), which can affect the metabolism of other drugs including anti-epilepsy medications and oral contraceptives
Side effect: hypersensitivity reaction-Stephen-Johnson syndrome + liver failure (rare) + leukopenia (rare)
Phenytoin
Historically important but current recommendation as an add on treatment for focal seizures due to unusual pharmacokinetic properties: 80-90% bound to plasma albumin, which is affected by other drugs and also greater hepatic clearance. Recommended as an add on therapy for the treatment of focal (partial) seizures.
Side effect: hypersensitivity reaction-Stephen-Johnson syndrome + gum hypertrophy + hirsutism + megaloblastic anaemia
Synaptic vesicles
Levetiracetam
Levetiracetam
Binds SV2A, synaptic vesicle protein 2A which is involved in synaptic vesicle docking and hence is thought to lead to reduced transmitter release. Recommended as a first or second choice monotherapy for the treatment of tonic-clonic, focal (partial) and absence seizures
Ethosuximide
Recommended as the first line monotherapy for the treatment of absence seizures.
Side effect: mood and behavioural changes + weight loss
How do we characterise absence seizures?
Absence seizures are characterised by 3 Hz oscillations in the EEG.
Due to oscillations in thalamocortical circuitry caused by: Activation of T-type Ca2+ channels in thalamocortical neurons. They stimulate cortex and reticular thalamic nucleus to activate in bursts.
When T-type Ca2+ channels in thalamocortical neurons inactivate - GABA from the reticular thalamic nucleus inhibits thalamocortical neurons promoting the re-priming of Ttype Ca2+ channels - Thalamocortical neurons become active again - GABA modulating drugs can therefore exacerbate absence seizures.
Pregabalin/Gabapentin
binds to CaV accessory subunit α2δ1, reduces CaV trafficking to the plasma membrane thus reducing Ca2+ influx, recommended as an add on therapy for the treatment of focal (partial) seizures -also effective in treating pain.
Enhanced GABAergic (receptor) function
Clobazam
Phenobarbital
Vigabatrin
Tiagabine
Clobazam
A benzodiazepine (positive allosteric modulator at GABAA) is recommended for use as a first line add on therapy for the treatment of tonic-clonic seizures.
Reported to cause less tolerance and sedation than other benzodiazepines. Need to follow guidance on prescribing medicines associated with dependence or withdrawal symptoms.
Phenobarbital
(barbiturate, positive allosteric modulator at GABAA), is recommended for use as a second line add on therapy for tonic-clonic seizures and add on therapy for focal (partial) seizures.
Risk of respiratory depression in overdose. As above requirement to follow guidance on prescribing medicines associated with dependence or withdrawal symptoms.
Vigabatrin
Irreversibly inhibits GABA transaminase leading to an increase in brain [GABA] and increased GABA release suggesting that vigabatrin increases the releasable pool of GABA.
Short half-life (5-8 hrs), but irreversible action means it can be taken once daily.
Vigabatrin is not a first line treatment, recommended as an add on therapy for focal (partial) seizures may be useful in treating refractory cases.
Side effect: mood and behavioural changes and irreversible visual field defects for long term use
Tiagabine
Inhibits GAT1 leading to increased extracellular [GABA], ~7 hour half-life, used as an add-on therapy for focal (partial) seizures.
GABA enhancers are generally contraindicated for the treatment of absence seizures as they tend to worsen seizure activity.
Why are GABA enhances contraindicated for absence seizures?
GABA enhancers, such as benzodiazepines, work by potentiating the effect of GABA at receptors. These drugs:
Increase the Tonic Inhibition: They likely intensify the very mechanism (enhanced tonic inhibition in the thalamus) that leads to the pathological hyperpolarization and subsequent rhythmic burst firing.
Worsen the SWDs (Spark and wave discharges): By amplifying the inhibition within the critical thalamocortical circuit, they worsen the abnormal oscillatory pattern, thereby exacerbating the seizure activity.
Phenobarbital + tiagabine+ vigabatrin
Perampanel
non-competitive AMPA receptor antagonist recommended as an add on therapy for the treatment of tonic-clonic or focal (partial) seizures.
Topiramate
Bit of everything, NaV, CaV and AMPA receptor block, plus GABAA facilitation, recommended for use as an add on treatment for tonic-clonic or focal (partial) seizures.
Use limited by teratogenic effects.
Zonisamide
blocks NaVs and CaVs, possible enhancement of GABAA function, recommended as an adjunct therapy for the treatment of tonic-clonic seizure or a further monotherapy for the treatment of focal (partial) seizures
Retigabine
Kcnq2 (Kv7.2) channel opener (approved 2011, discontinued 2017) – was approved for the treatment of focal (partial) seizures.