Psych 3501 Exam 3: Sleep and Circadian Medicine
1/33
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
34 Terms
Sleep continuity: sleep metric
Sleep duration: total amount of time from sleep onset to sleep offset
Sleep onset latency (SOL): amount of time to fall asleep
Wake after sleep onset (WASO): amount of time spent awake from sleep onset to sleep offset
Sleep quality: subjective perception of quality of sleep
Sleep efficiency: sleep duration/time in bed (%)
Healthy: 85%-90% or higher
Sleep stages
Non-rapid eye movement (NREM)
3 stages: stage 1, 2, 3
Progress from lighter to deeper sleep
Rapid eye movement (REM)
Characterized by rapid eye movements, muscle paralysis, and mixed frequency EEG activity
- Prevent us from acting out on our dreams
- EEG activity: similar to an awake brain
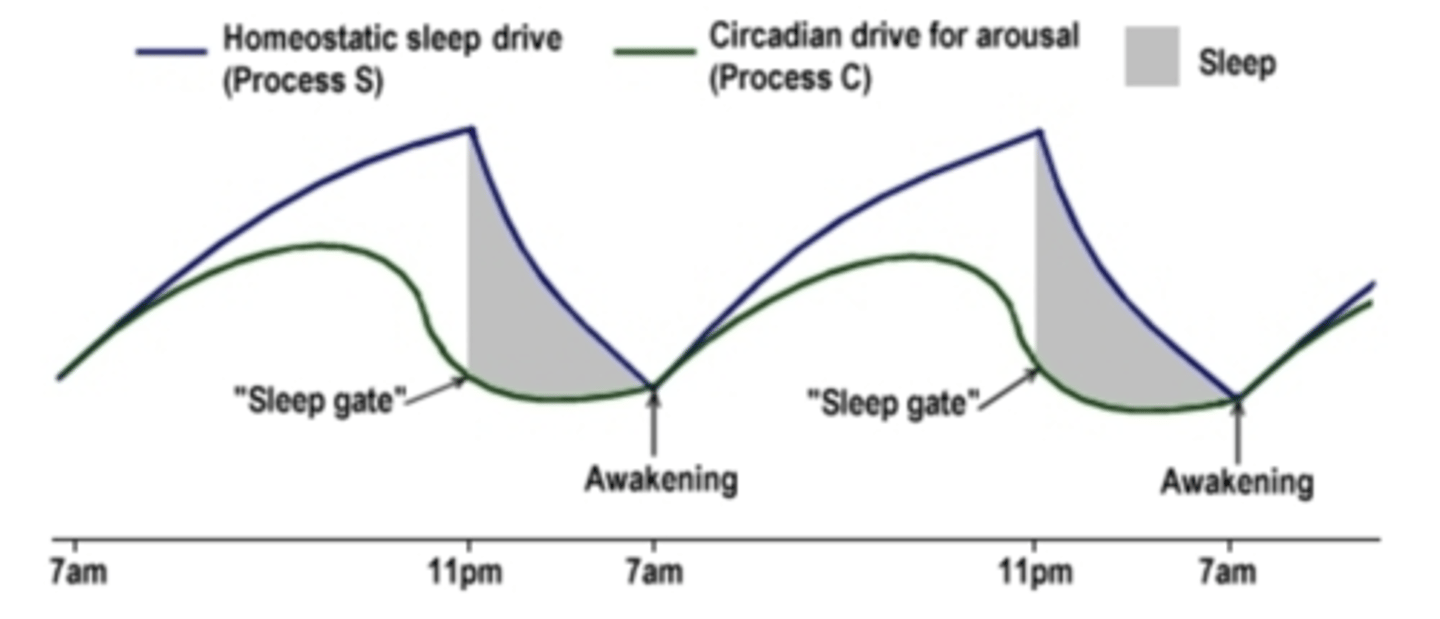
Two process model of sleep regulation
The homeostatic sleep drive
As you stay awake, the drive accumulates
The accumulating pressure for sleep drives for sleepiness
During sleep, the pressure decreases
The circadian drive for arousal
24-hour clock in our body, one of the output is circadian wakefulness
Sending the highest alerting signals during mid-day, dropping off at biological night
Most likely to fall asleep when pressure for sleep is high and circadian alerting signal is low
Most likely to wake up when pressure for sleep is low and circadian alerting signal goes up
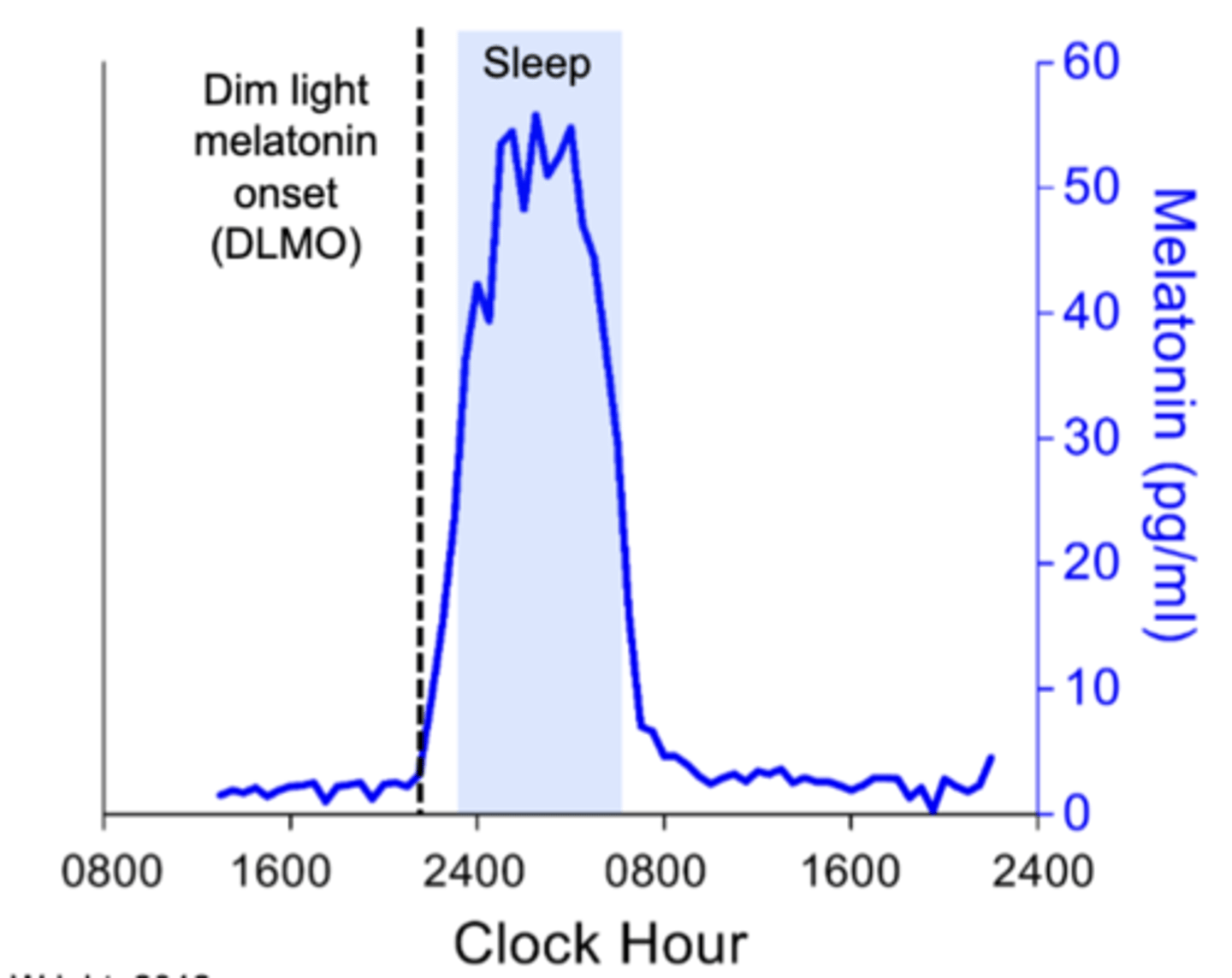
Circadian rhythms
Describe 24-hour rhythms and multiple processes that keep us in sync with the light/dark cycle
Allow us to anticipate changes in our environment rather than respond passively
the circadian rhythm of melatonin: Low during daytime, have a peak over night
To measure circadian rhythm: measure the time we see the steep rise of melatonin levels
Cognitive Behavior Therapy for Insomnia (CBTI)
Behavioral treatment designed to treat chronic insomnia (unable to fall asleep, stay asleep, wake up too early)
Behavioral model of insomnia
Y-axis: insomnia severity
Threshold: when insomnia symptoms become clinically significant
Premorbid: no insomnia symptoms
Acute: meaningful insomnia symptoms
Early: engage in perpetuating factors
Chronic: precipitating factor goes away, perpetuating behaviors maintaining the insomnia in the long-run
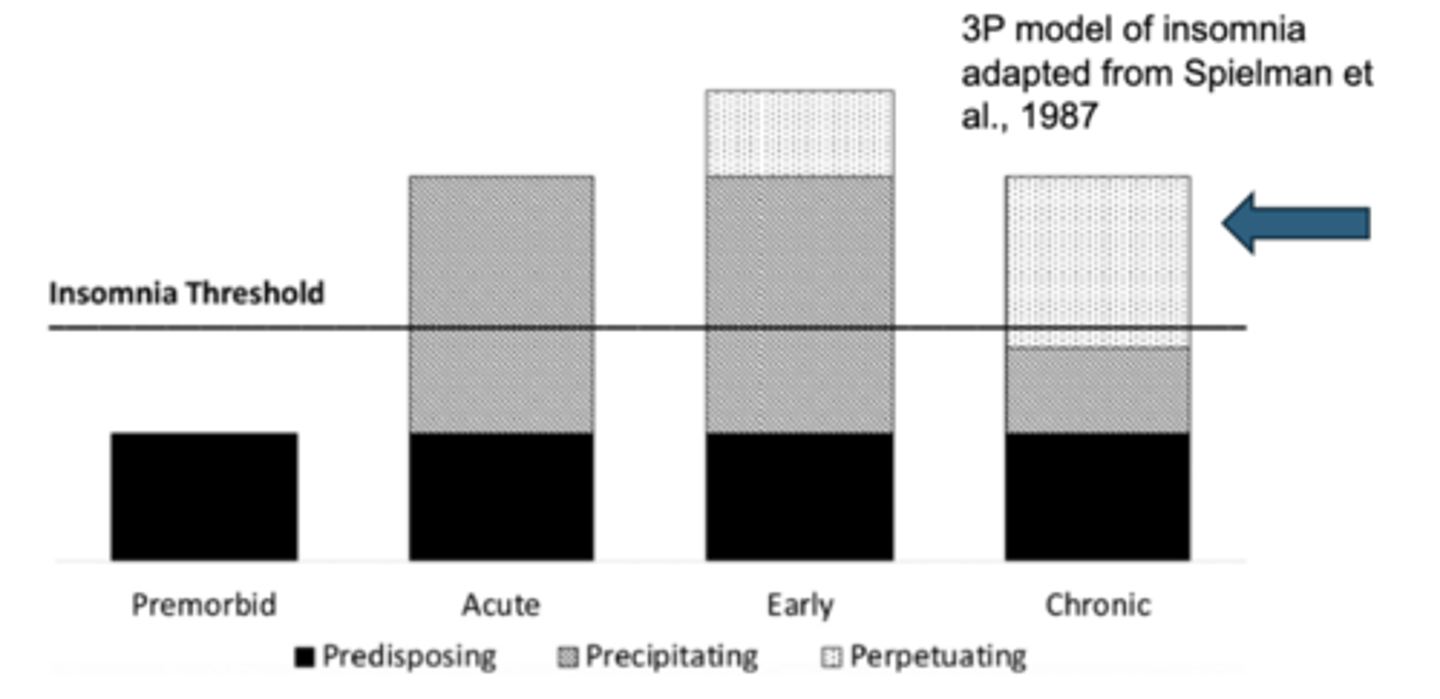
3P model of insomnia
Predisposing: risk factors, things make you more vulnerable to insomnia but don’t cause insomnia on their own
- Genetic risk, medical conditions, mental disorders
Precipitating: stressor in the short-run
- Stressful life event (positive or negative)
- Most people experience in their lives
Perpetuating: behaviors that maintain insomnia over time
- Try to compensate for the sleep loss or to get more sleep
- Spending excessive time awake in bed, going to bed earlier, doing things in bed other than sleep or sex (try to catch sleep)
The problem with perpetuating factors
Mismatch between time in bed and sleep duration
Stimulus dyscontrol
Conditioned arousal
3 core components of CBTI
Stimulus control
Sleep restriction
Sleep hygiene
Stimulus control: playing the odds
Odds 1 in 2: sleep/sex
Odds 1 in 6: sleep/sex/read/eat/worry/work
Complex conditioning history: stimulus paired with many responses
Low probability the stimulus will yield a single given response (sleep)
Stimulus control
Aims to limit amount of time spent in bed/bedroom awake
Instructions:
- Go to bed only when sleepy
- Avoid any behavior in the bed or bedroom other than sleep and sexual activity
- Leave the bedroom if awake more than 15 minutes
- Return to bed only when sleepy
Goal: reduce stimulus dyscontrol; create new conditioning history (bed-sleep instead of bed-awake)
Sleep restriction
Limit sleep opportunity to current sleep duration
Sleep prescription
- Set fixed wake time based on patients weekday needs
- Set bedtime based on average sleep duration
Goals
- Reduced mismatch between time in bed and time asleep
- Increase sleep pressure -> more consolidated sleep
Weekly upward titration by 15 minutes if >90% sleep efficiency
Sleep hygiene
good habits related to sleep
Aims to address problematic sleep-related behaviors/environment
Not effective monotherapy
Example sleep hygiene instructions
- Exercise regularly
- Make sure you bedroom is at a comfortable temperature
- Don’t watch the clock
Optional components
Cognitive therapy
Reduce preoccupation with or anxiety about insomnia
Relaxation/mindfulness
Reduce physiological arousal in the pre-sleep period
Light therapy
Reduce circadian phase delay/advance
CBTI efficacy
Recommended as first-line treatment for insomnia by American College of Physicians
Reduces sleep onset latency and wake after sleep onset by ~50%
60-80% have a therapeutic response to treatment
Improvements stable up to 24 months
Small acute increases in sleep duration but ~1hr increase over long-term follow up
CBTI vs. hypnotics: efficacy
Similarly effective in short-term
CBTI treatment responses maintained up to 24 months
- Long-term: more enduring benefits
Gains from medications diminish after medication cessation
- Hypnotics: more side-effects, tolerance problems
CBTI + hypnotics
adults with insomnia randomly assigned to CBTI alone or CBTI + hypnotics
Conclusion: the combined group has a faster response to treatment compared to CBTI alone, but both groups end up in the same place
Light Therapy
Light has multiple effects: circadian and training effects (directs our circadian clock), but also non-circadian regions of the brain (arousal effect), and mood-related areas of the brain (mood-promoting effect independent of the circadian effect)
time of light exposure
The time at which we receive light exposure affects its impact on circadian clock
Bright light in the morning + dim light in the evening: shift circadian clock earlier
Dim light in the morning + bright light in the evening: shift circadian clock later
The same principle used in light therapy: increase in bright light morning exposure
Light therapy delivery options
Historically: delivered through light boxes: high-intensity lighting
10,000 lux = outdoor natural daylight, 30min-1hr each morning after wake up to receive treatment
Limitation: have to sit in front of the box: burdensome
Recent alternative: wearable light therapy glasses
Benefits: less burden, can continue morning routine
Downsides: much dimmer intensity of light compared to the box (400-500 lux, bright indoor lighting)
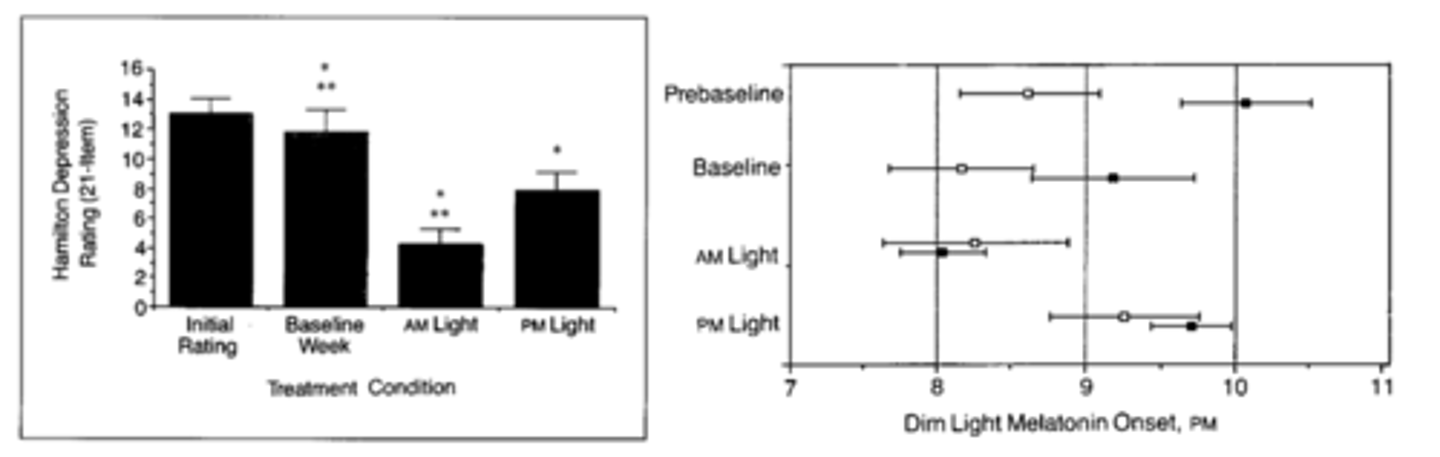
Light therapy in seasonal depression
Compared patients with seasonal depression to healthy controls
Baseline: one week of fixed sleep schedule
Two light therapy conditions: bright light 6-8am or 7-9pm
Measure depression symptoms & circadian rhythm using melatonin onset
Compared to baseline week, depression symptoms decreased in both conditions, largest in morning condition compared to evening condition
Patients with seasonal depression have a significant delay pre baseline
In baseline: an advance just by stabilizing the sleep schedule
Morning light condition: further circadian phase advance
Evening light condition: circadian phase moved later
Conclusion: two effects of lights (circadian + mood impact)
Interpersonal and social rhythm therapy (IPSRT)
Developed for bipolar disorders
What are the intervening mechanisms of stressful life events precipitating mood episodes?
Social time cues: interacting with people, eating, etc.
Stressful life events disrupt social time cues (context about time), which impact circadian rhythms, and result in disruption in biological rhythms, which in turn precipitate a mood episode
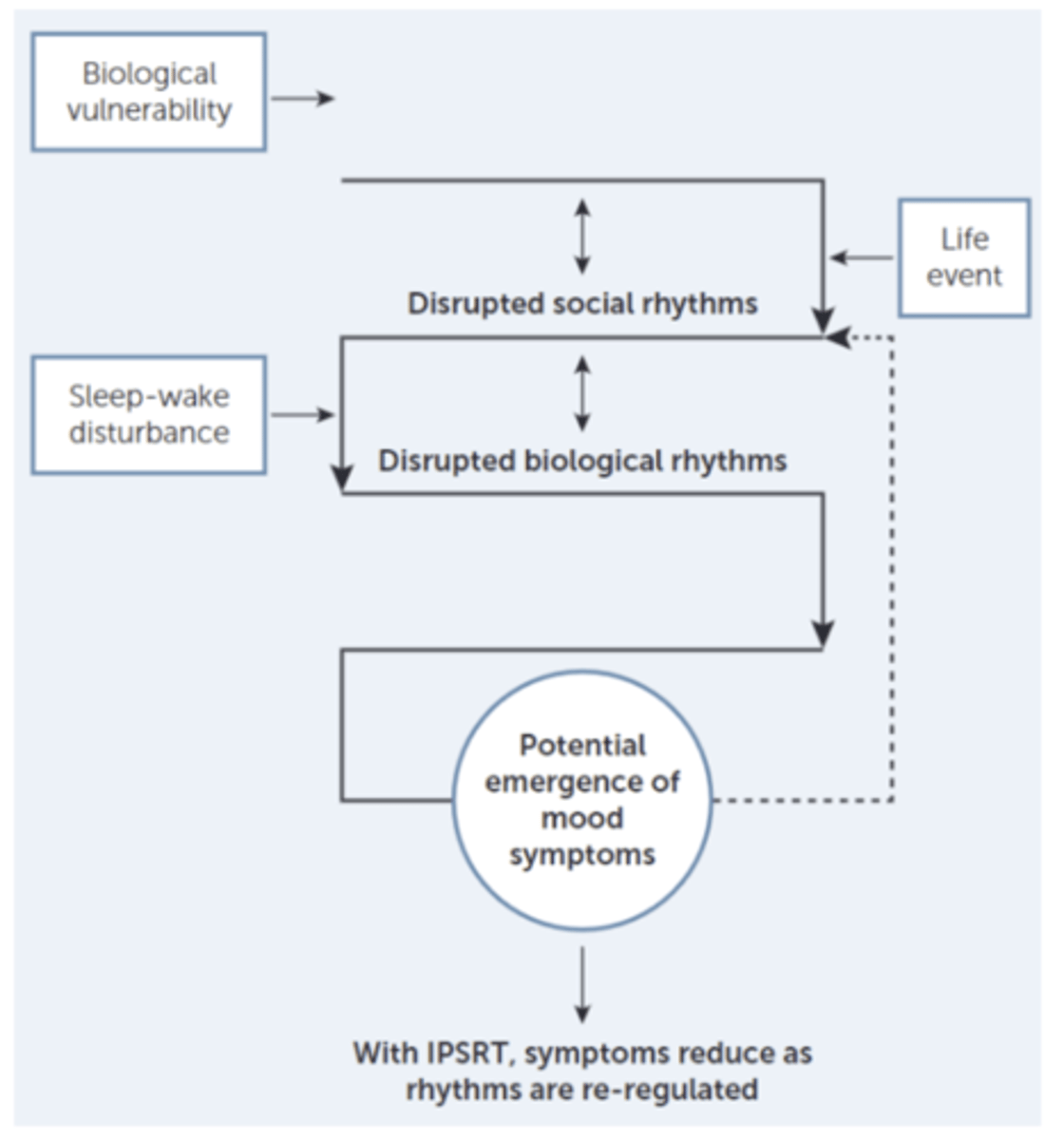
Interpersonal and social rhythm therapy (IPSRT) component
Interpersonal psychotherapy +
Social rhythm therapy: stabilize social time cues, which in turn stabilizes biological rhythms
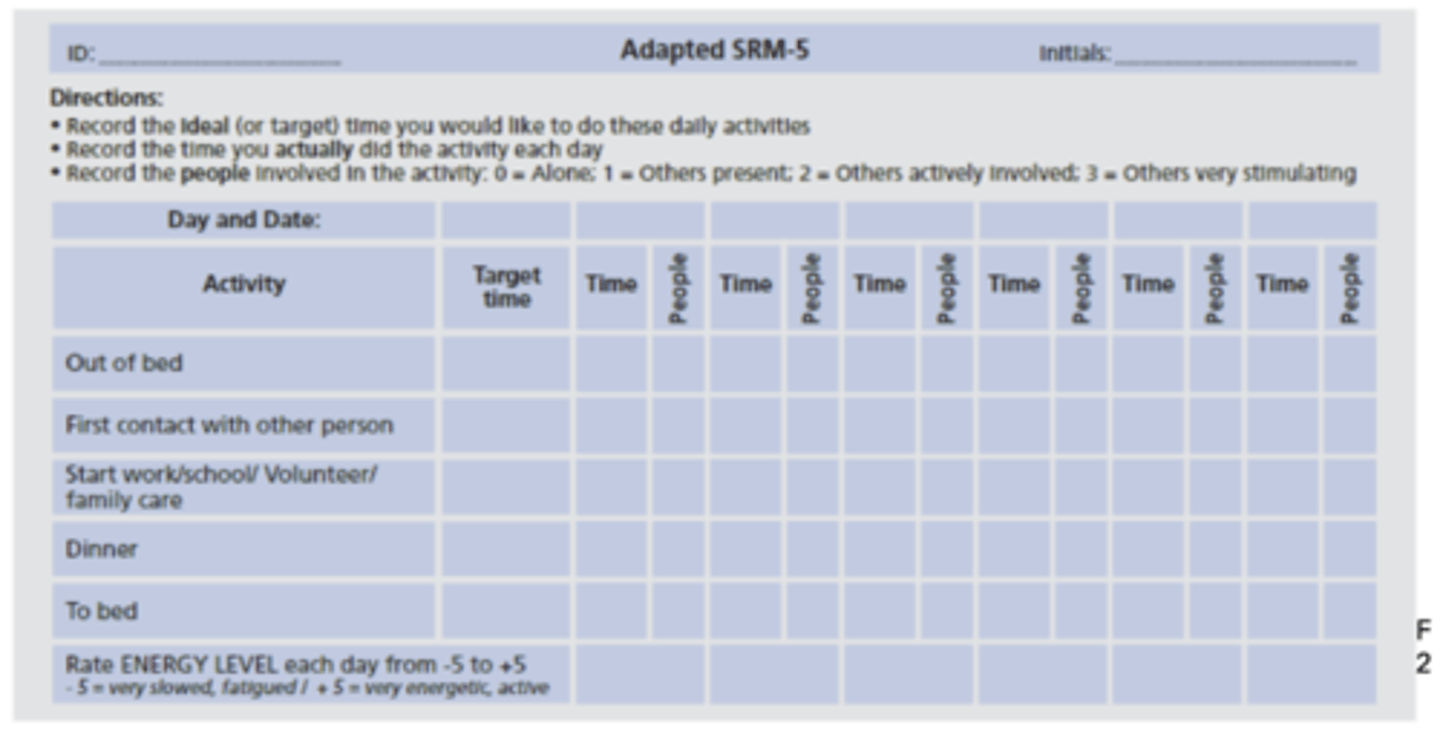
Have clients track their social rhythm through social rhythm measure (SRM-5)
Help them construct a daily schedule to stabilize social time cues
IPSRT Efficacy
Efficacious for improving bipolar disorders
BP vs. TAU
T0: baseline; T1: 3-month into treatment; T2: 3-month follow up
A significant reduction in manic symptoms for IPSRT compared to TAU
Increase the amount of time into the next mood episode
Improved regularity of social rhythms
Association between increase social rhythm regularity & reduced likelihood of mood episode recurrence
The role of sleep and circadian medicine in traditional psychotherapy
Sleep disturbance and mental health
Across disorders, medium to large effects for decreased sleep continuity, small to medium to decreased sleep depth, small to medium to increased REM pressure compared to healthy controls
Takeaway: broad association between worse sleep and mental health conditions
Delayed sleep timing associated with blunted response to psychotherapy for OCD
Worse sleep reduces treatment responses for psychotherapies
Later sleep timing (suggesting rhythm delay) is associated to lower response to ERP for OCD
Bedtime at baseline: divided into non-delayed and delayed group
delayed: less reduction in symptoms, more non-responders
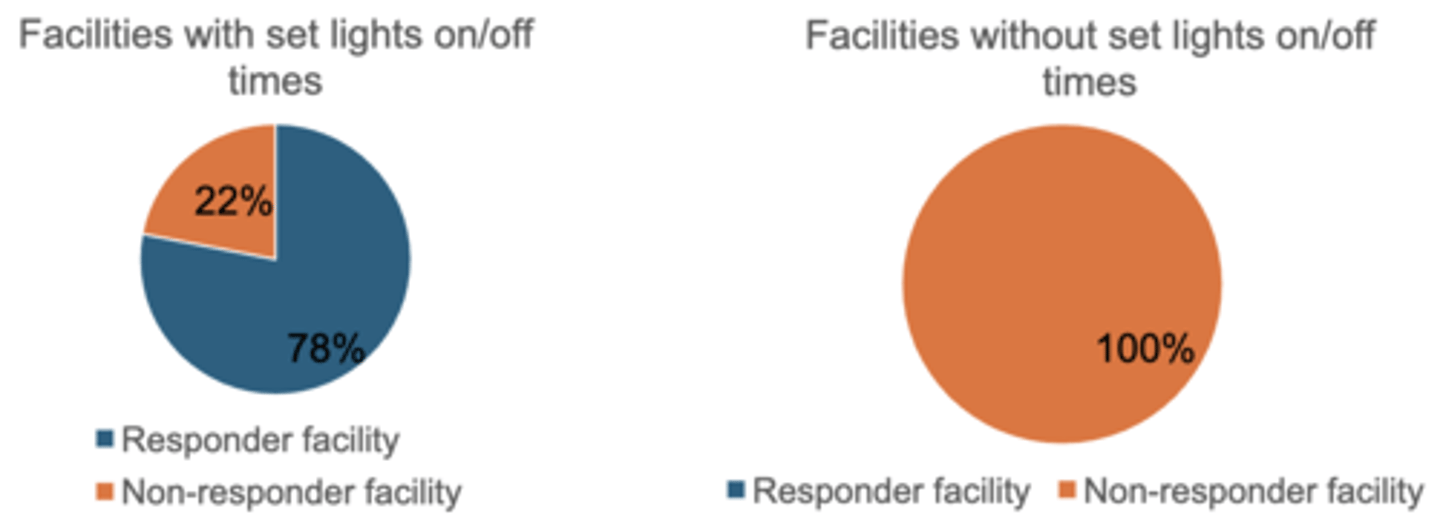
Consistent lighting schedules associated with treatment response in residential OCD treatment facilities
Residential facilities for OCD categorize by the average symptom scores of their patients at discharge
Responder facility: the average patient responds to treatment
Non-responder facility: the average patient doesn't respond to treatment
A fixed lighting schedule can have impact on treatment outcomes
Multiple symptoms of psychopathology decrease following CBTI in adolescents
Adolescents with insomnia treated with CBTI (GT)/CBTI over Internet (IT)/waitlist
Both GT and IT significantly decreased mood symptoms that are maintained after 12-month follow-up
Both GT and IT significantly improvements in sleep efficiency
Only treated for insomnia but have improvement on other symptoms
Depression and anxiety decrease following CBTI in pregnant women
Pregnant women with insomnia treated with digital CBTI or TAU
Depression and anxiety decrease from pre to post insomnia treatment and were maintained after 12-month post-treatment follow-up
Suicide ideation decreases following CBTI
Treated with CBTI or control
CBTI reported lower rate of SI at post-treatment and 1-yr follow-up
CBTI enhances PTSD treatment
Treated with CBTI first and then CPT (treatment for PTSD) or control first + CBT
After CBTI/control & after CPT, CBTI has significantly lower depression and PTSD symptoms
Only targeting sleep has significant positive benefits for individual depression and PTSD symptoms
Adding CBTI onto psychotherapy for PTSD improves treatment outcomes
CBTI prevents incidence of depression
Patients treated with CBTI followed over time
Those who were treated with CBTI were less likely to be depressed in the future compared to control
Can leverage CBTI to prevent new depression onset in the future
Summary