CPR1 - Exam 2 practice questions
1/118
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
119 Terms
A patient had acute viral infection that caused severe alveolar damage. Following recovery, the alveolar cells are replenished by which of the following?
Type II alveolar cells
As part of a research project, you develop a monoclonal antibody that identifies club cells in paraffin-embedded sections. immunohistochemical assays using your antibody confirm that these are found at which of the following anatomical locations?
Terminal bronchioles
Which of the following cells secrete surfactant in the indicated structure?
Club cells
An autopsy finding in a 80-year-old male who dies of left heart failure showed fluid and heart failure cells in the alveoli. In a normal lung, which of the following components prevents interstitial fluid leakage into the alveoli?
Tight functions
A 45-year-old smoker presents with recurrent respiratory infections. Which innate immune component is most likely impaired, leading to reduced pathogen clearance?
Alveolar macrophages
Which component of the adaptive immune system is primarily responsible for long-term immunity in the lungs?
Memory T cells
A patient with a viral lung infection shows increased production of cytokines and chemokines by airway epithelial cells. What is their primary role in this context?
Recruit inflammatory cells to the site of infection
What is the primary mechanical defense provided by ciliated epithelial cells?
Mucociliary clearance
A patient with cystic fibrosis has impaired mucociliary clearance due to thickened mucus secretions in the airways. Which consequence is most likely?
Increased susceptibility to bacterial infections
Which mechanism allows secretory IgA (sIgA) to prevent bacterial adherence in the respiratory tract?
Blocking adhesins on bacterial surfaces
Patients who do not make IgA (selective IgA deficiency) are at increased risk for which condition?
Recurrent respiratory infections
Which T-helper cell subset is predominantly involved in asthma pathogenesis?
TH2
In chronic obstructive pulmonary disease (COPD), which T-helper cell response contributes most significantly to neutrophilic inflammation?
TH17
A 35-year-old patient with severe asthma shows elevated levels of IL-5 in their sputum. What is the primary effect of this cytokine in asthma pathogenesis?
Eosinophil recruitment and activation
A patient experiences wheezing and shortness of breath shortly after exposure to cat dander. Which type of hypersensitivity reaction is most likely occurring?
Type I (immediate)
Which cell type is primarily responsible for the initial sensitization phase in allergic asthma?
Dendritic cells
Club cells possess exocrine secretory function. What type of malignancy is expected to arise from these cells?
Adenocarcinoma
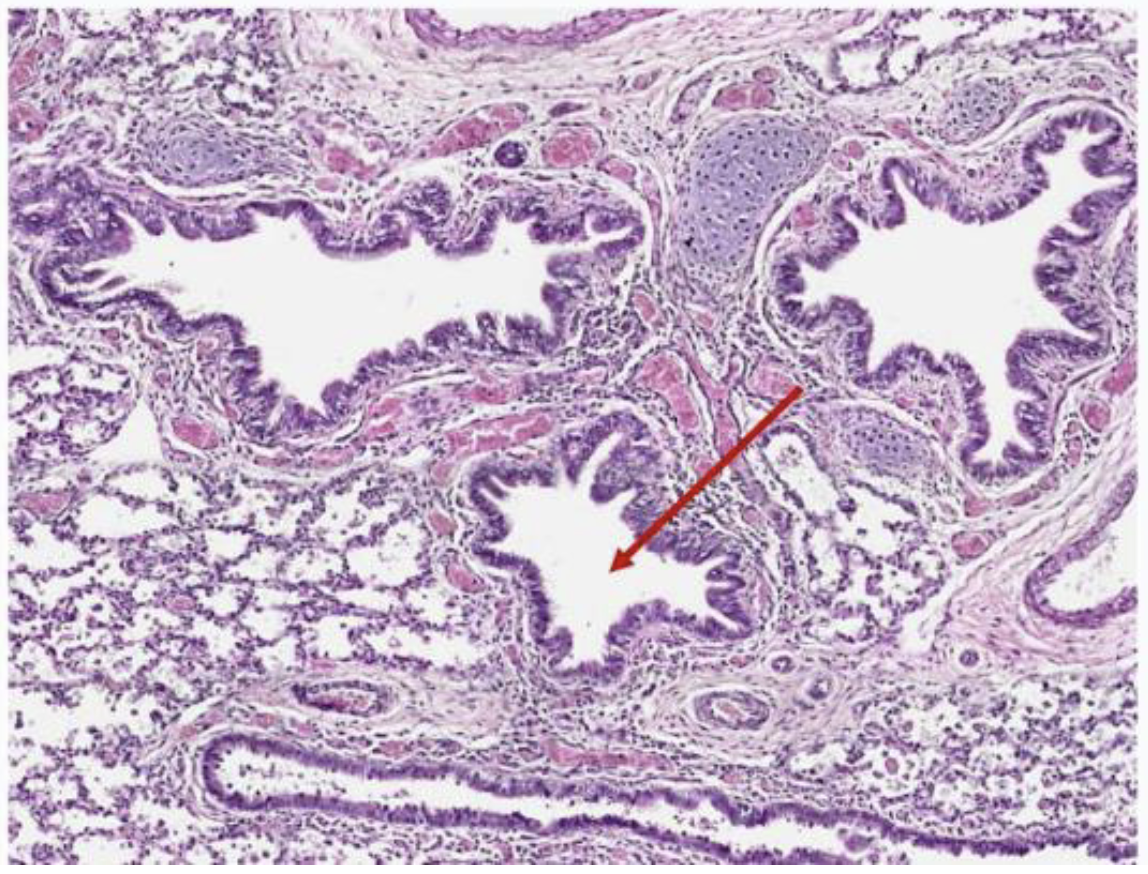
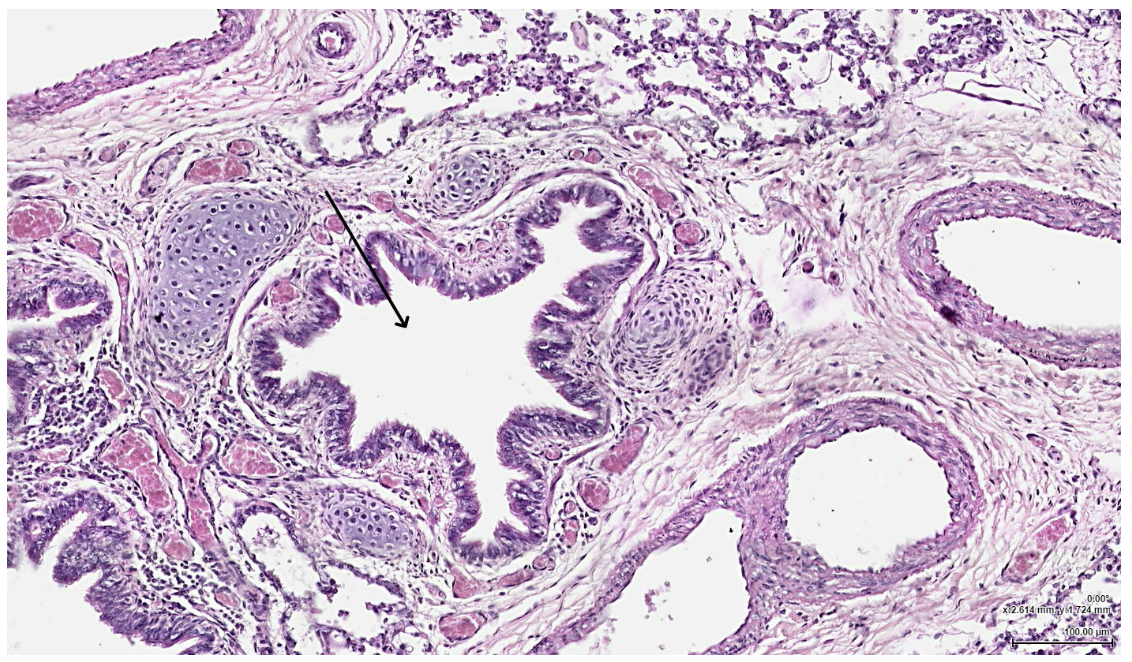
In the attached EM, the cell indicated by the arrow is most likely which of the following?
Basal cell
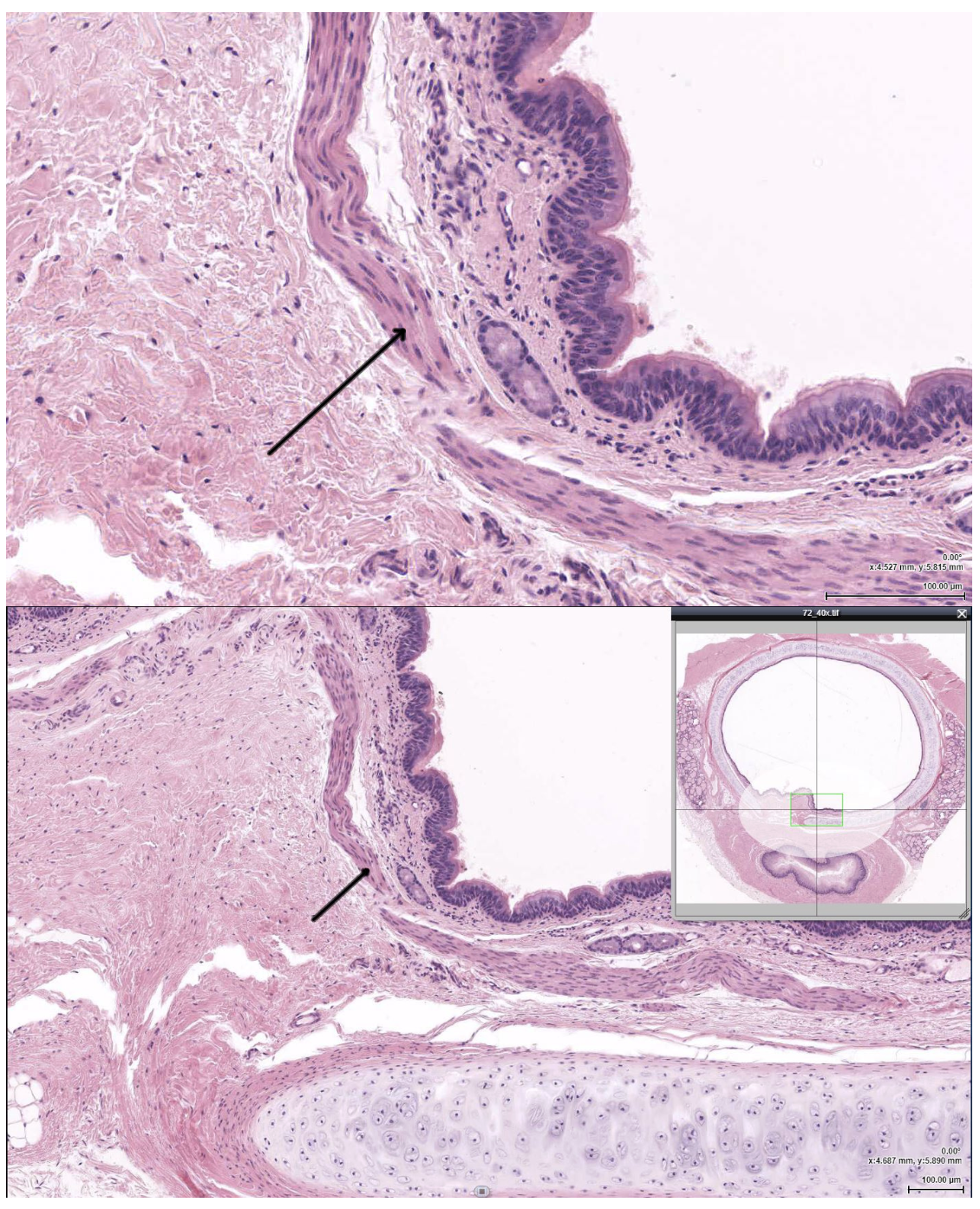
The structure indicated by the arrow is most likely which of the following?
Trachealis muscle
The tissue indicated by the arrow would most likely be found in which other location?
Trachea
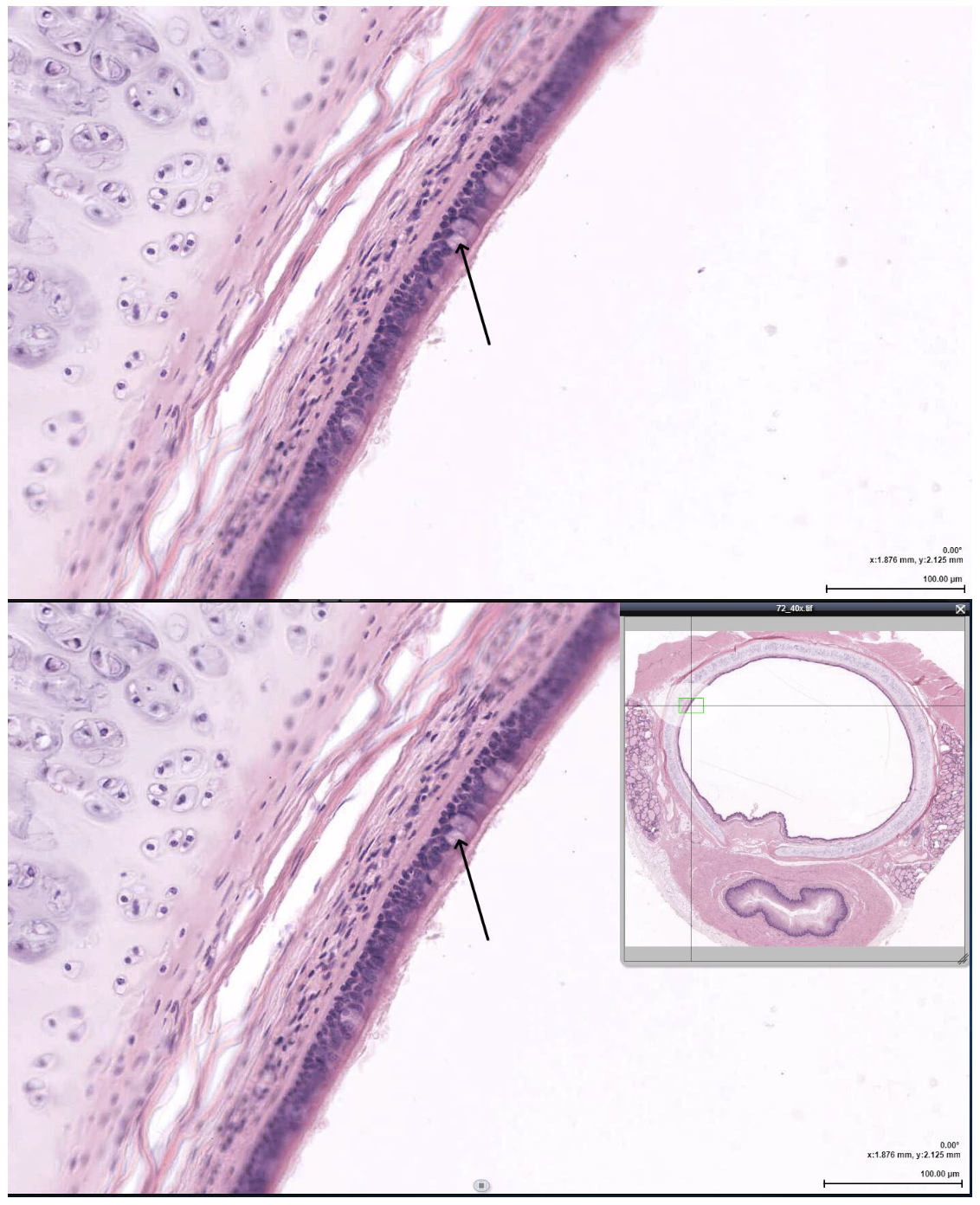
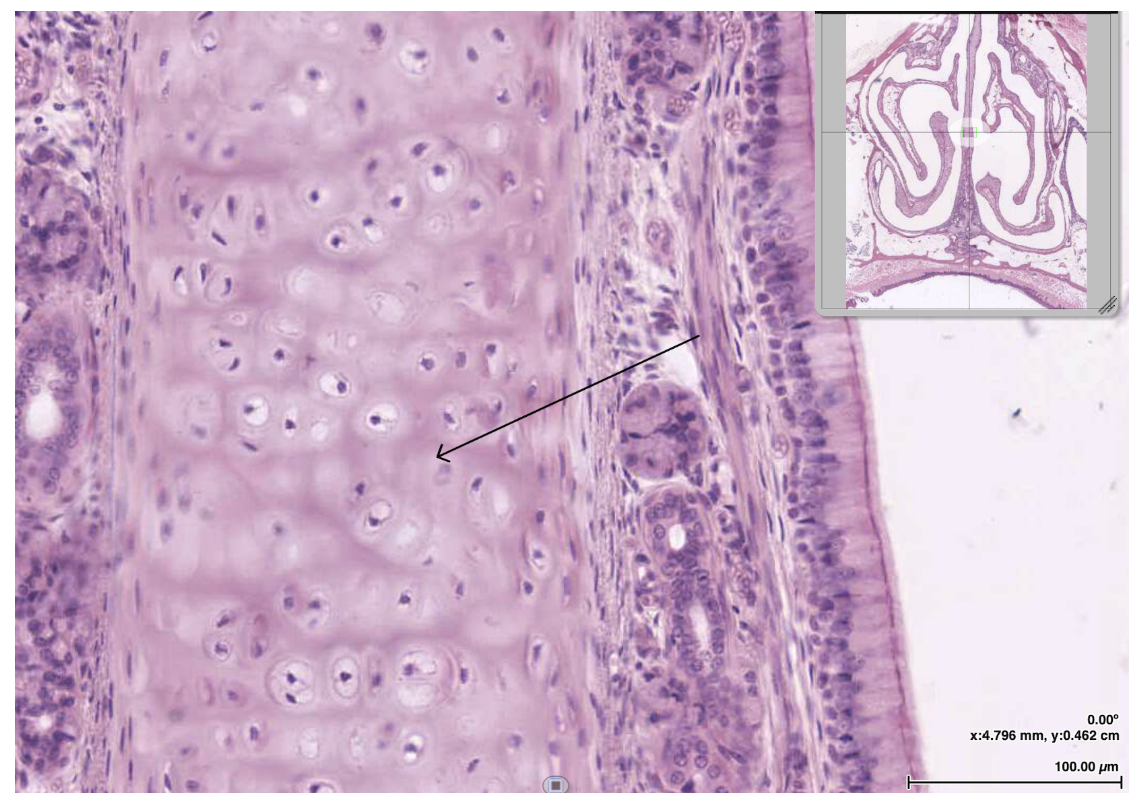
The cell indicated by the arrow would LEAST likely be found in which of the following?
Terminal bronchiole
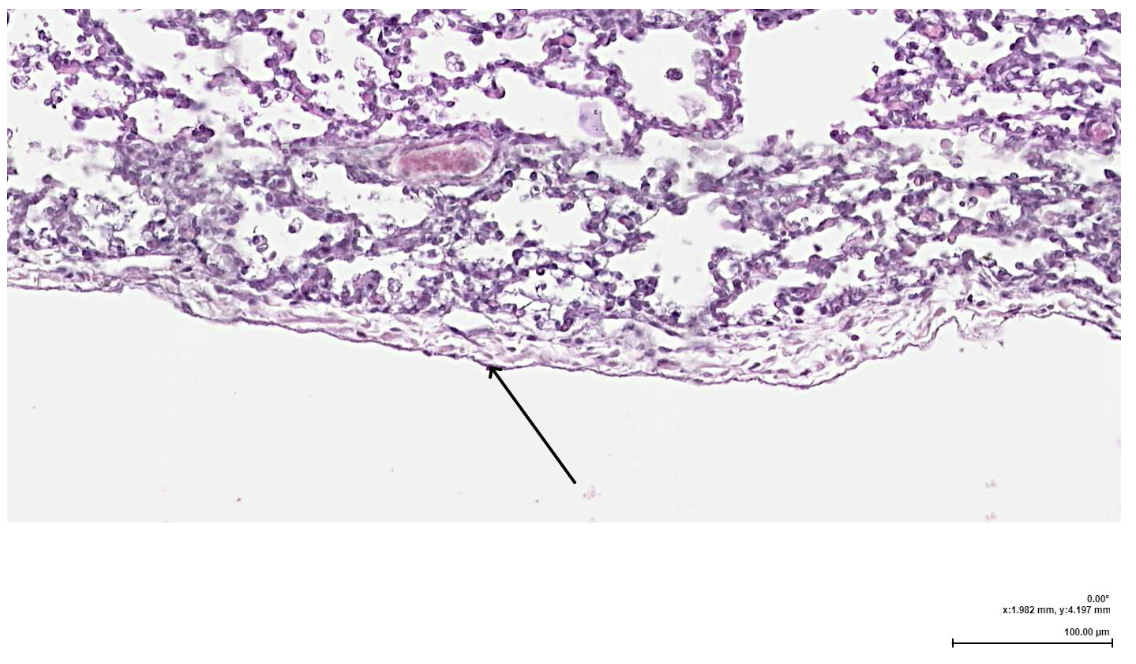
The layer indicated by the arrow is primarily composed of which of the following?
Fibroelastic CT
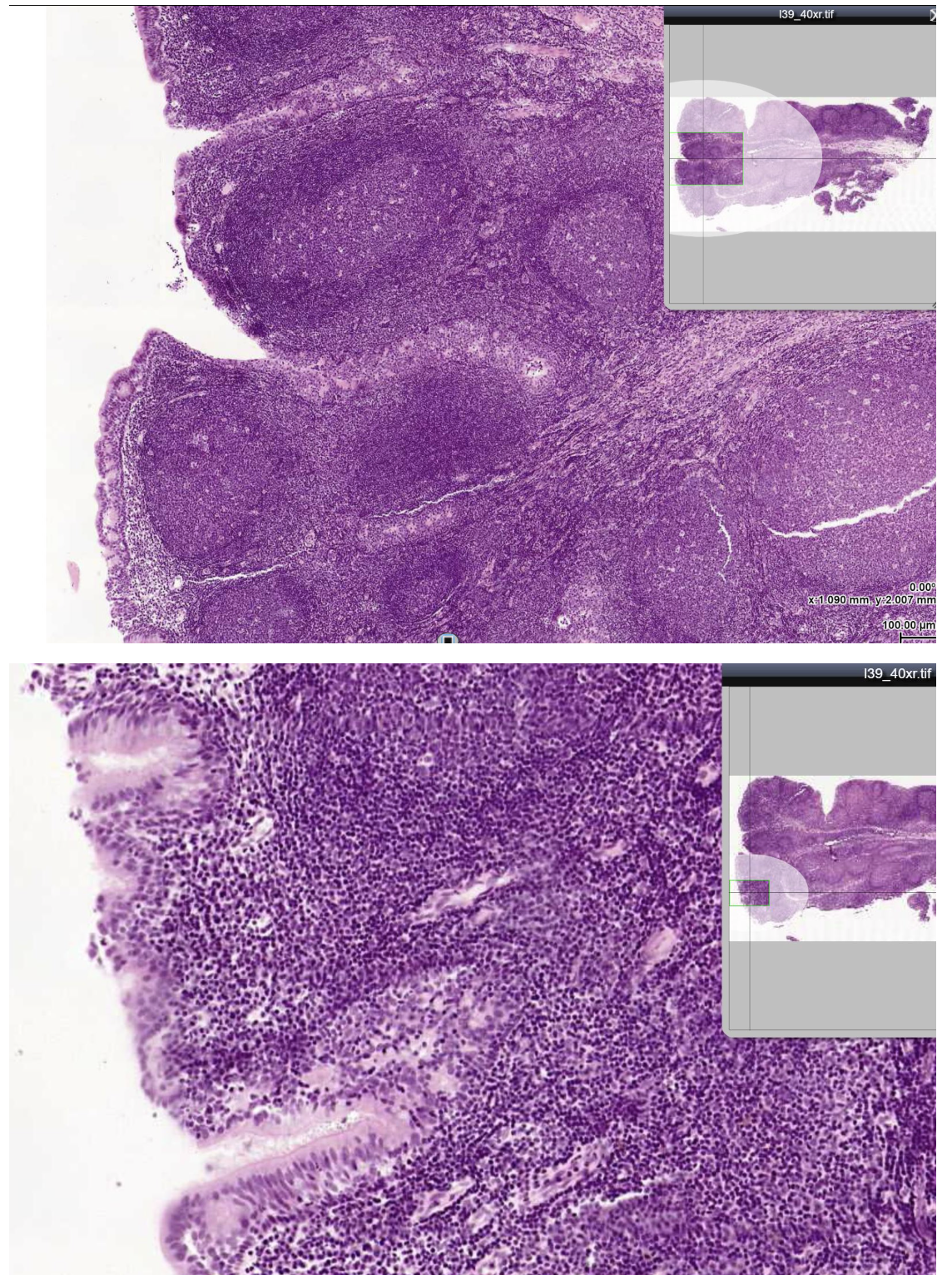
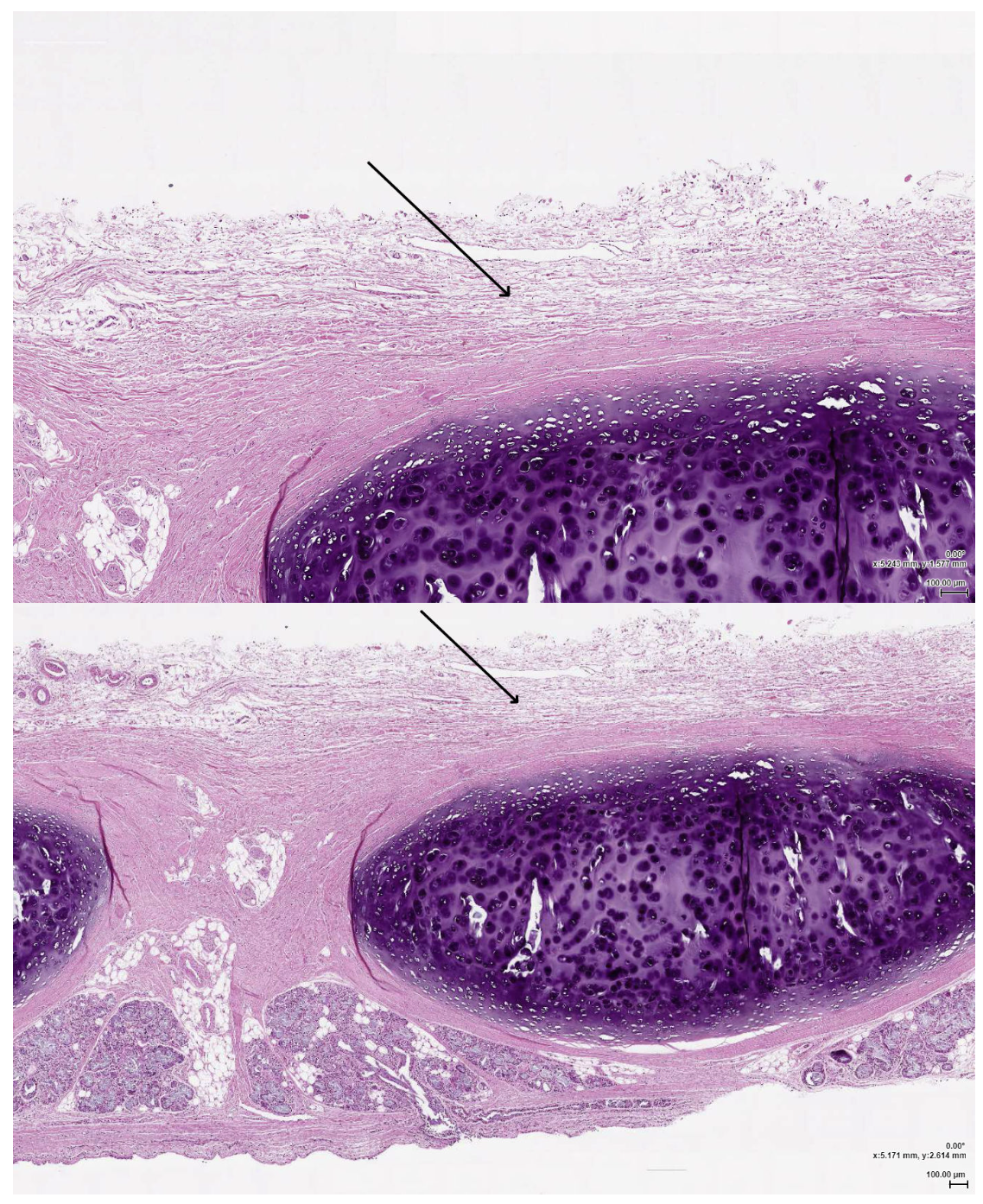
The tissue shown in the linked image is best described by which of the following?
It shrinks after childhood
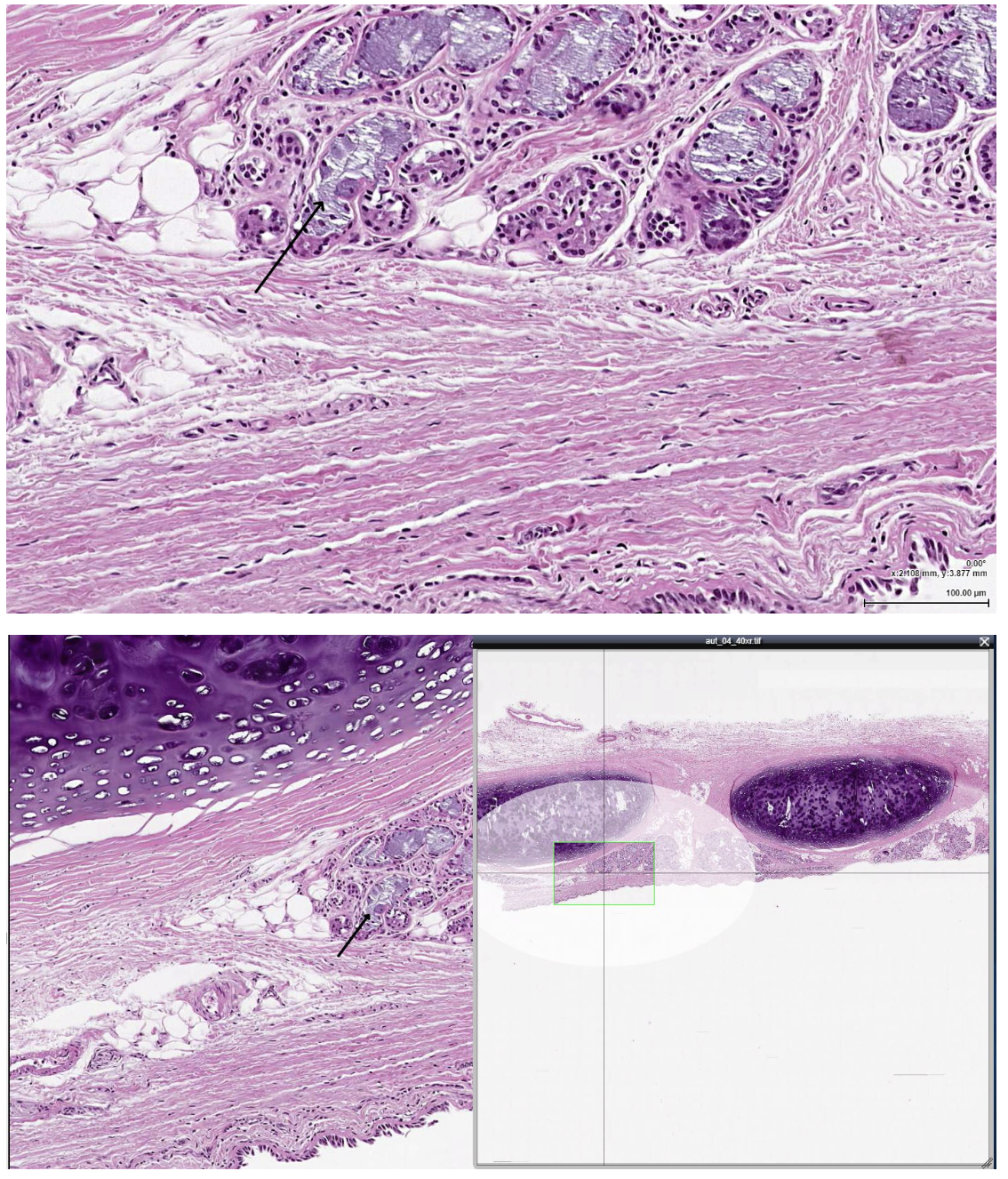
The structure indicated by the arrow is most likely which of the following?
Seromucous gland in submucosa
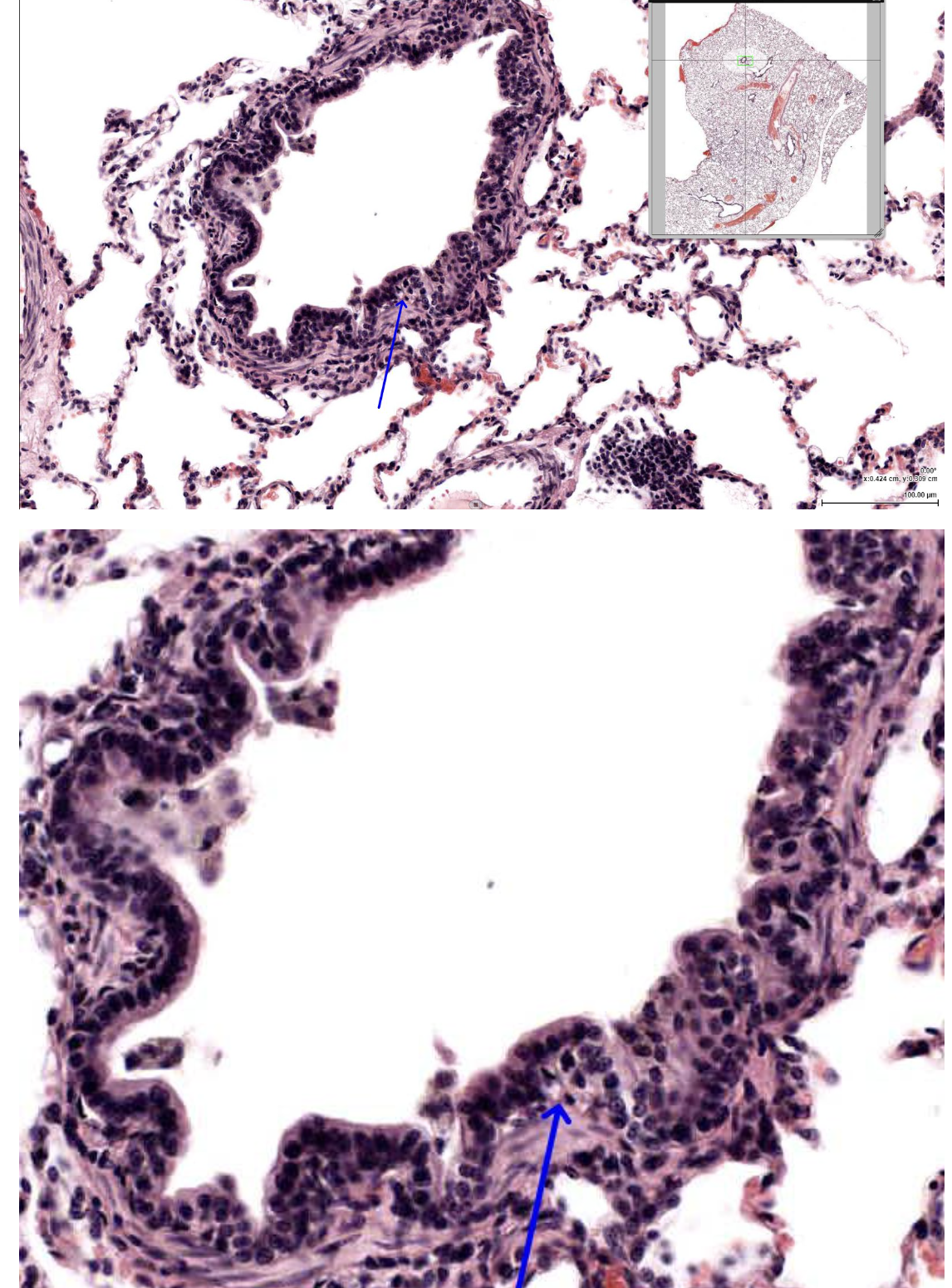
The layer indicated by the arrow is most likely which of the following?
Lamina propria of terminal bronchiole
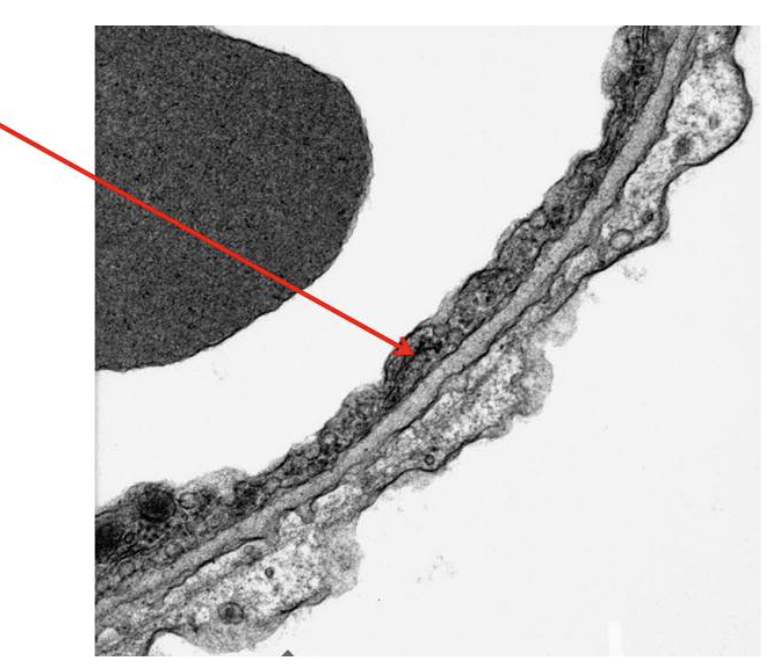
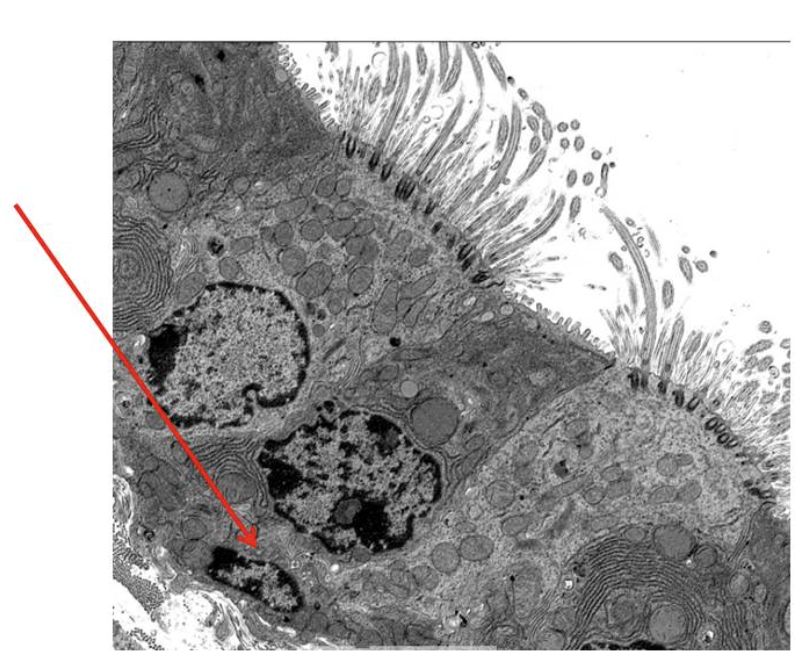
In the attached EM of the blood-air barrier, the structure indicated by the arrow is most likely which of the following?
endothelial cell
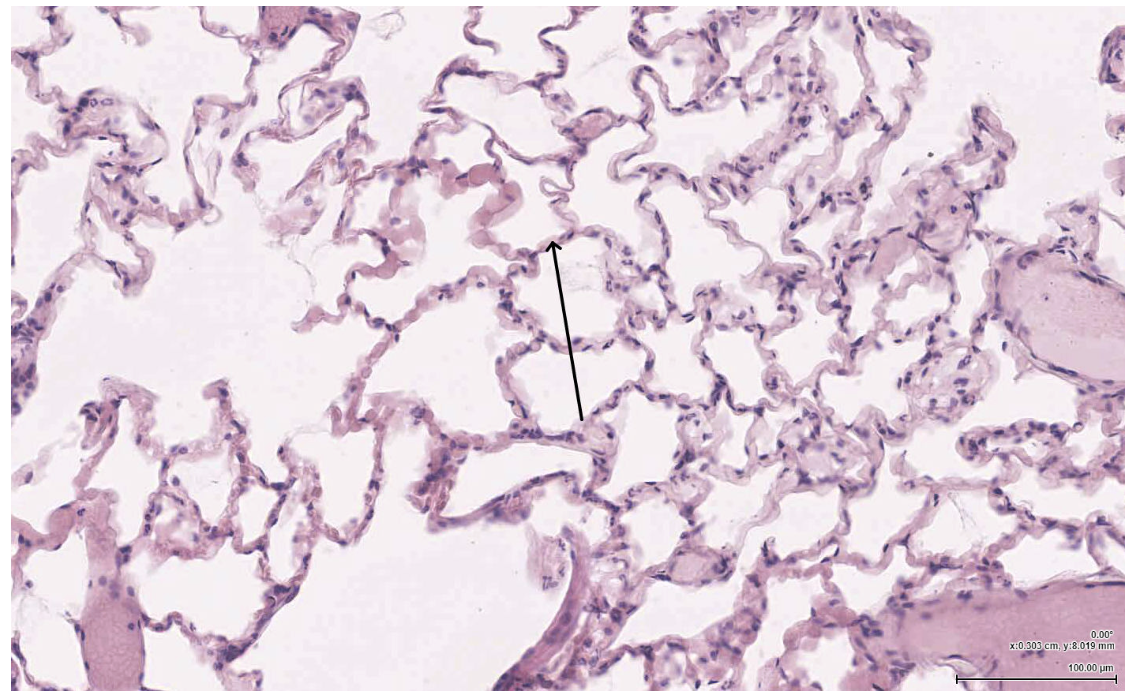
The structure indicated by the arrow most likely contains which of the following:
Elastic fibers
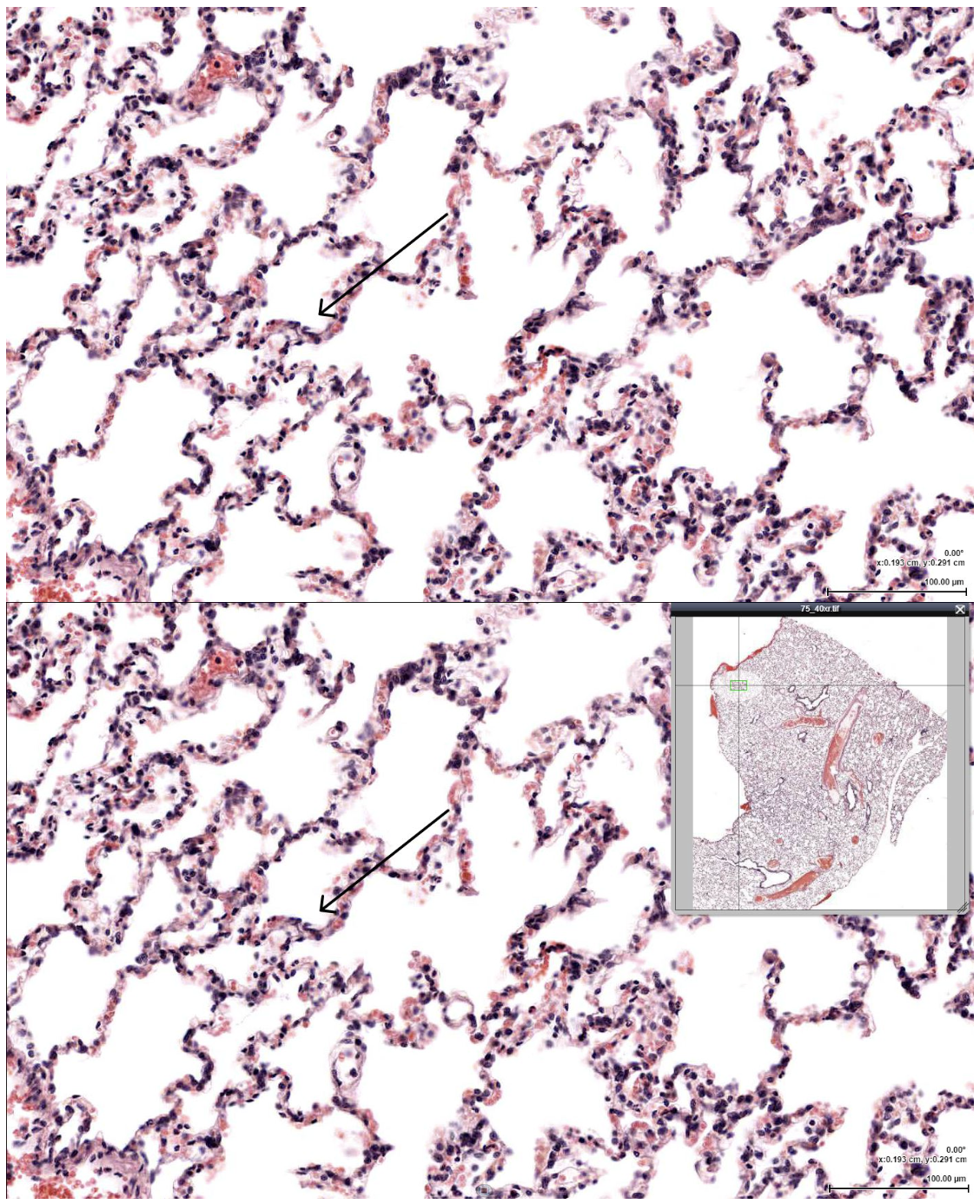
Which of the following cells would be LEAST likely to be found lining the indicated structure?
Clara cell
Right before passing through the indicated structure, where would air most likely travel?
Primary bronchus

The structure indicated by the arrow is most likely which of the following?
Alveolar Sac
The structure indicated by the arrow is most likely composed of which of the following?
Simple squamous epithelium
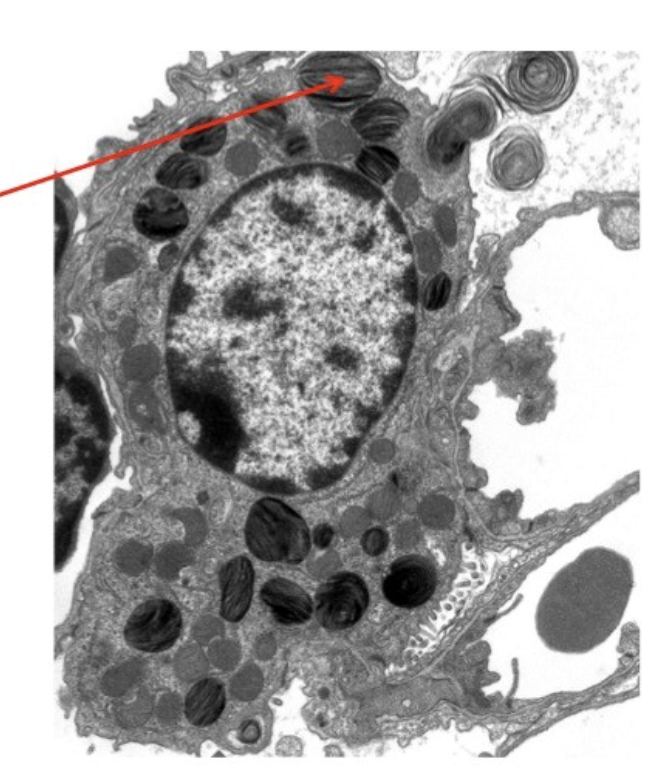
In the attached EM of an alveolus, the structure indicated by the arrow is most likely which of the following?
Lamellar body
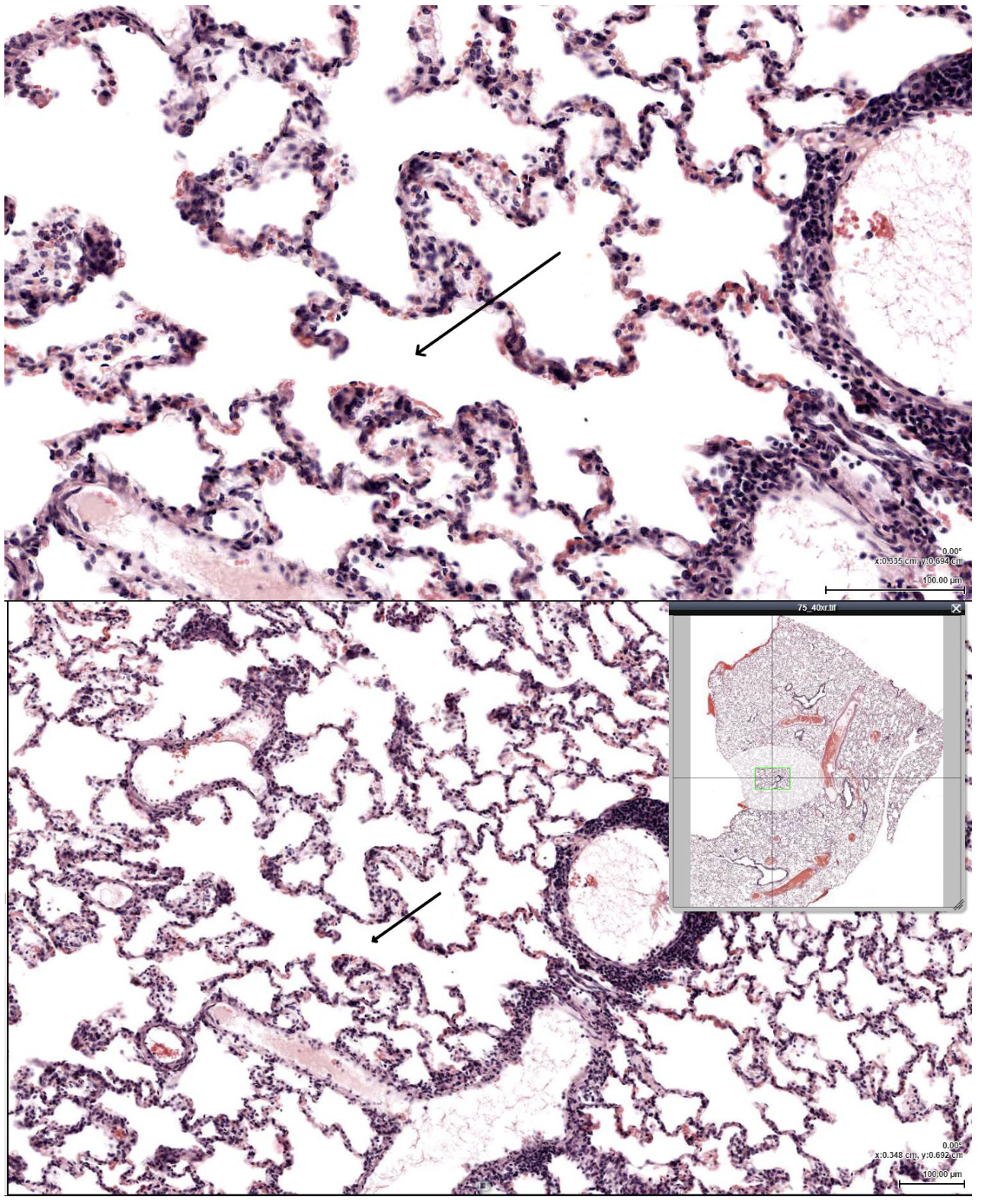
After passing through the indicated structure, where would air most likely travel next?
Alveolar sac
Which of the following components of the airway epithelium act in mucociliary transport to prevent pulmonary infection?
Ciliated epithelial cells
Which of the following molecules is involved in the innate immune defense to prevent infection in the lung?
Surfactant SpA
A 15-year-old female presents to the walk-in clinic with a runny nose, itchy eyes, and a cough. She says the symptoms started a few weeks ago when the flowers started blooming. Which immune mediator is contributing to her symptoms?
IL-4-induced goblet cell hyperplasia
A 62-year-old man with a 40-pack-year smoking history presents with a 3-year history of productive cough that is worst in the mornings and has occurred for at least 4 months each year. He reports frequent winter “chest colds” requiring antibiotics. On exam, he is mildly cyanotic, with diffuse expiratory wheezes and coarse crackles. Spirometry shows an obstructive pattern with decreased FEV1/FVC ratio and minimally reversible airflow limitation after bronchodilator administration. Bronchial biopsy reveals reveals goblet cell hyperplasia, thickened bronchial walls with mucus gland enlargement, and infiltration of neutrophils, macrophages, and CD8+ T cells. Which immune mechanism most directly explains this patient’s recurrent bacterial infections?
Loss of ciliated epithelial cells and mucus hypersecretion impairing mucociliary clearance
A 22-year-old male presents to the hospital with a 6-day history of difficulty breathing and productive cough. History reveals he is a frequent smoker, and further examination indicates remodeling of the lung tissue as a reason for his dyspnea. Which of the following immunological mediators is the primary cause of this patient’s present pathology?
Neutrophil elastase
A 15-year-old male presents to the emergency department with a chief complaint of dyspnea. Upon examination extended inspiration, exhalation and pronounced wheezing are noted. No edema or constriction of throat is observed. History reveals he is allergic to cats and has recently had contact with one at a friend’s house. Bronchoscopy reveals presence of large accumulation of mucus. Bacterial cultures are negative and no viral cytopathology is noted. Which helper T cell response is most directly responsible for the local pathologies observed in this patient and blocking of which immune mediator would most help relieve his symptoms?
TH2 response, IL-13
A student was tracing the bronchial tree from the trachea to the alveoli in order. Which of the following is the first location where the exchange of oxygen and carbon dioxide take place?
Respiratory bronchiole
A pathology resident examined a sample of lung tissue obtained from an abortus. The tissue sample showed varied components of airway and vasculature. The resident claimed that the abortus was over 24 weeks of gestation. The presence of which of the following histological findings most likely support the predicted gestational age of the specimen?
Respiratory bronchiole
A newborn baby chokes throughout her first feeding with the breast milk regurgitating from the infant’s mouth and nose. Noticing the difficulty feeding, a pediatrician tries to pass a catheter into the baby’s stomach and meets resistance. The physician suspects tracheo-esophageal fistula as the underlying condition in this newborn. Which of the following structures normally separates the pharynx from the respiratory bud and likely to have failed in this patient?
Tracheoesophageal septum
Which feature makes inspiration an active process during quiet breathing?
Contraction of respiratory muscles
During quiet inspiration, contraction of the diaphragm primarily results in:
increase in vertical thoracic dimension.
At the end of quiet expiration, intrapleural pressure is normally negative relative to atmospheric pressure because of:
opposing inward lung recoil and outward chest wall recoil.
Transpulmonary pressure is best defined as the difference between:
intrapulmonary pressure and intrapleural pressure.
A healthy adult is breathing at a rate of 12 breaths per minute with a tidal volume of 500 mL. Anatomical dead space is approximately 150 mL. Which value best represents this individual’s alveolar ventilation?
4,200 mL/min
A patient develops localized alveolar hypoventilation, due to mucus plugging in a segment of the lung. Which physiological response best explains how the lung minimizes ventilation–perfusion mismatch in this region?
Pulmonary arteriolar vasoconstriction caused by closure of O2-sensitive K+ channels
The standard PA chest x-ray is taken in full inspiration. Which of the following would be an indication for taking an expiratory image?
Bronchial foreign body
The settings involving windowing are most common in which of the following modalities?
Computed Tomography
A 24-year-old woman with mild persistent asthma reports frequent wheezing during exercise and nighttime symptoms twice per week. She uses her albuterol inhaler multiple times per day and has required 2 urgent care visits in the past month. Her physician prescribes a new inhaled medication to be used twice daily, in addition to an inhaled corticosteroid. Which pharmacologic property best explains why this medication is not appropriate for relief of acute bronchospasm, but is effective for long-term symptom control?
Slower onset of action due to high lipid solubility
A 67-year-old man with a 40-pack-year smoking history presents with chronic cough, exertional dyspnea, and recurrent COPD exacerbations. He is unable to tolerate β2-agonists, due to tremor and palpitations. His pulmonologist prescribes a once-daily inhaled medication that improves lung function and reduces exacerbation frequency by targeting the dominant autonomic input to airway smooth muscle. Which mechanism best explains the therapeutic benefit of this drug?
Antagonism of muscarinic receptors that mediate bronchoconstriction
A 63-year-old man with severe COPD continues to experience frequent exacerbations, despite maximal inhaled therapy, including a long-acting β2- agonist, inhaled corticosteroid, and tiotropium. His pulmonologist adds roflumilast to his regimen. Several weeks later, the patient reports mild nausea and weight loss, but fewer exacerbations. The therapeutic effect of roflumilast is most closely related to which shared mechanism with theophylline and β2-agonists?
Increased intracellular cyclic AMP levels in inflammatory cells
A 55-year-old who smokes 1½ pack of cigarettes each day and has a 45-packyear history of tobacco use, presents with cough and shortness of breath intermittently over the past 6 weeks, especially toward the end of his work shifts. He works as a waiter and is on his feet and walking throughout his 4-hour shifts. He reports he has used a coworker’s asthma inhaler a few times and finds it doesn’t seem to do anything. You anticipate he has COPD. Which pattern of pulmonary function testing would support your clinical diagnosis?
FEV1/FVC = Decreased; FVC = Normal; The abnormality does not significantly reverse with bronchodilator
A 24-year-old has had episodes of coughing and chest tightness 3 or 4 times each week for the past month. She was diagnosed with asthma as a child. She is using her short acting beta agonist inhaler with good relief during these episodes. Which choice is most appropriate at this time?
Continue the use of short acting beta agonist inhaler as needed and add a daily low-dose inhaled corticosteroid
A 68-year-old man with a 45–pack-year smoking history presents with progressive exertional dyspnea. Pulmonary function testing shows increased total lung capacity and decreased DLCO. Histologic examination of lung tissue using H&E and elastic fiber staining reveals permanent enlargement of air spaces distal to the terminal bronchioles with destruction of alveolar septa. Which of the following mechanisms is most responsible for these findings?
Protease–antiprotease imbalance leading to elastin degradation
A 62-year-old male presents with chronic productive cough for at least 3 months per year for the past 2 consecutive years. Arterial blood gas analysis shows hypercapnia. Bronchial biopsy stained with H&E demonstrates mucous gland enlargement and increased goblet cells. Which histopathologic finding is most characteristic of this condition?
Increased Reid index greater than 50%
A 42-year-old African American woman presents with progressive dyspnea and dry cough. Chest radiograph shows bilateral hilar lymphadenopathy. Transbronchial lung biopsy stained with H&E reveals well-formed noncaseating granulomas. Which of the following mechanisms best explains the pathogenesis of this disease?
Cell-mediated immune response involving Th1 lymphocytes
A healthy individual at sea level is breathing room air. Which variable has the greatest direct effect on lowering alveolar PO2 according to the alveolar gas equation?
Increased arterial PCO2
A patient presents with hypoxemia that does not improve with supplemental oxygen. Which mechanism of hypoxemia best explains this finding?
Right-to-left shunt
A 65-year-old male with a history of diabetes mellitus and chronic alcohol use presents with a high fever, productive cough with thick, mucoid, blood-tinged sputum ("currant jelly" sputum), and difficulty breathing. A lung biopsy is performed, and histopathology shows extensive alveolar destruction with necrotizing inflammation, fibrinopurulent exudates, and Gram-negative bacilli within the alveoli. Which of the following is the most characteristic histopathologic finding in this case?
Alveolar spaces filled with abundant mucoid capsular material and neutrophilic infiltration
A 62-year-old female has had a chronic cough and increasing dyspnea for 10 years. A chest radiograph performed 1 year ago showed increased lucency of upper lung fields and bilateral flattening of the diaphragmatic leaves. She has had nausea and vague abdominal discomfort for 6 months. Biopsy specimens from an upper gastrointestinal endoscopic study show a chronic nonspecific gastritis with no detectable Helicobacter pylori organisms. During the past month, she has passed red urine on several occasions. Cystoscopic examination shows a 3-cm exophytic mass in the dome of the bladder, and biopsy specimens show a urothelial carcinoma. What is her most likely risk factor for this spectrum of findings?
Cigarette smoking
A patient comes in complaining of a dry cough that has persisted over the past 4 days. He states that the cough is persistent, and he has no other associated symptoms. Which of the following is BEST to recommend for this patient?
Benzonatate
A 22-year-old, previously healthy man, who had immigrated to the US 5 years prior, presented to the ED with a 2-day history of fever and right-sided scrotal swelling. He was in a monogamous relationship with a male partner and had no history of HIV or other sexually transmitted infections. He had immunization records including immunization against measles-mumps-rubella (MMR), but did not specify the number of doses he received. The patient reported that he had a self-limiting episode of bilateral painful neck swelling 7 days before presenting to the ED. He did not report any headache, neck stiffness, abdominal pain, urinary tract symptoms, urethral discharge or rash. However, his partner had also suffered from symptoms of bilateral parotid gland enlargement before the onset of the patient's illness. Physical exam indicates a temperature of 39°C (102.2°F). The oropharynx was normal and there was no swelling of the parotid glands. Testicular exam showed a tender right testis. Which of the following is the most likely diagnosis?
Mumps
A 19-year-old college student presents to the student health clinic with 3 days of nasal congestion, rhinorrhea, sore throat, and sneezing. He is afebrile, and physical examination is unremarkable, aside from mild erythema of the nasal mucosa. He is diagnosed with a viral upper respiratory infection and advised on supportive care. At the cellular level, the virus most commonly responsible for this illness gains entry into respiratory epithelial cells by binding to a host cell surface molecule that normally functions in leukocyte adhesion and migration. Which of the following host receptors is most likely involved in viral entry?
ICAM-1
A neonate was delivered at 30-weeks' gestation (premature) in a hospital. The community in which the hospital resides is currently experiencing the peak incidence of respiratory syncytial virus (RSV) infections. Which of the following agents should this patient receive to prevent RSV infection?
Palivizumab
A 7-year-old boy is brought to the pediatric clinic in early November for his annual influenza vaccination. His medical history is significant for mild persistent asthma controlled with inhaled corticosteroids. His parents ask about the differences between the available influenza vaccines and whether one option avoids injections. The physician explains that one influenza vaccine uses a live attenuated virus that replicates primarily in the cooler temperatures of the nasopharynx, while the other contains inactivated viral particles and is administered systemically. Which of the following best distinguishes the live attenuated influenza vaccine (LAIV) from the inactivated influenza vaccine?
Is administered through nasal inhalation while the inactivated vaccine is injected
A 58-year-old male presents to the emergency department with acute respiratory failure. He started experiencing symptoms of dry cough, rigors, fever of 39°C and headache, 2 days ago, which worsened rapidly to severe shortness of breath. Health history reveals that the patient is diabetic. Travel history is significant for a trip to the middle east to see his ailing mother from which he returned about a week ago. Rapid antigen detection tests for the most common infectious agents are negative. The doctors are suspicious that the patient is suffering from an infection that is caused by a(n):
enveloped RNA virus.
A 13-year-old girl with cystic fibrosis followed up with a physician and has had symptoms of recurrent sinusitis, including headache, facial pain, and chronic nasal drainage. Nasal irrigation, intranasal steroids, and several courses of antibiotics have failed to clear the infection. The most appropriate treatment for this patient would be:
Endoscopic sinus surgery
A physician is caring for an 8-month-old infant in the pediatric intensive care unit. She has been hospitalized for 1 week with respiratory syncytial virus bronchiolitis. In discussions with the mother, she reports that the child has very frequent, large, foul-smelling stools. Physical examination of the child reveals a temperature of 37.0°C, heart rate of 130 beats/min (normal for age), respiratory rate of 35 breaths/min on the ventilator (normal for age), and blood pressure of 80/40 mmHg (normal for age). Her oxygen saturation is 90%, and her most recent arterial blood gas shows a pH of 7.25 (decreaed) and PaCO2 of 70 mmHg (elevated). Her weight is 7 kg, and she appears malnourished, with decreased muscle development. No obvious congenital abnormalities are apparent. Her chest appears hyperinflated; she has no heart murmur; her pulses are equal and strong, and her abdomen is protuberant with normal bowel sounds. Computed tomography scan of her chest was obtained earlier today to evaluate enlarging cystic-appearing lesions on her chest radiograph. The scan revealed cystic lesions and bronchiecatsis. Of the following, the most likely underlying diagnosis in addition to bronchiolitis is:
Cystic fibrosis
A 1-year-old boy presents with a 2-month history of “wet” coughing. He was delivered at term but had delayed passage of meconium due to a meconium ileus. Over the past 3 to 6 months, he has been treated each month for acute otitis media. His parents are concerned that, despite a good appetite, their son has been losing weight and has 4 to 6 loose, foul-smelling stools per day. Of the following, the most appropriate study to confirm the suspected diagnosis is
sweat chloride pilocarpine iontophoresis measurement
A 6-month-old female infant exhibits failure to thrive, loose stools, and recurrent respiratory problems. The infant has had 2 positive sweat chloride test results (> 60 mEq/L). She has 1 full sibling who is healthy. The parents inquire about the recurrence risk to future siblings. What is the estimated likelihood that the parents will have another child with this diagnosis?
25%
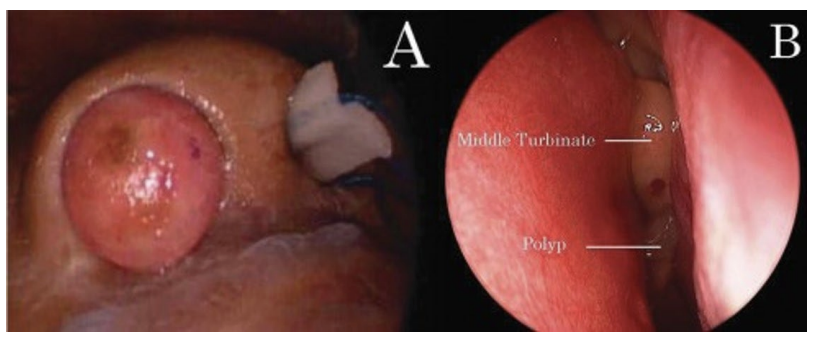
A 6-year-old boy seen in a physician's office has had chronic nasal congestion and noisy breathing for several months. His parent reports mucoid rhinorrhea that is present every day and worsens intermittently. The boy often has difficulty breathing through his nose, especially when sleeping. Past trials of antihistamines or antibiotics have only provided temporary improvement in symptoms. He has no history of serious bacterial infections, pneumonia, or asthma. His growth and development have been appropriate for his age. He eats a regular diet and has normal stool and urine output. On examination of the nasal passages, the attending physican notes glistening, bluish-gray, grape-like masses bilaterally. The remainder of the physical examination findings are unremarkable. The most common cause of this condition in children is best evaluated by performing:
a sweat chloride pilocarpine iontophoresis measurement.
A pediatrician receives a phone call from the state’s newborn screening program regarding a 7-day-old neonate with an elevated trypsinogen. A diagnosis of cystic fibrosis is suspected. The neonate was seen by the pediatrician’s partner 1 day ago. There was no significant family history of diseases in childhood. Vital signs and physical examination were normal. Feeding and growth parameters were normal. Which of the following is the most appropriate next step?
Schedule the neonate for diagnostic testing.
A 15-year-old adolescent girl with cystic fibrosis is seen for chronic dyspnea. She also elicits productive, purulent cough of a persistent, chronic nature. She has poor lung function with forced expiratory volume in 1 second 40% of predicted at last spirometry check. Last computed tomography of the chest performed revealed bilateral bronchiectasis, most notably at the upper lobes bilaterally. On physical examination, chest crackles are appreciated in the upper lobes bilaterally. Mild digital clubbing is appreciated on general exam. Of the following, where would you most likely expect a viscerosomatic reflex on structural examination?
T2 – T7
A 4-year-old boy is admitted to the general medical floor of the local children’s hospital for his third case of pneumonia of the year. He has been known to have at least three severe pulmonary infections each year of his life. The family also reports symptoms that correspond to steatorrhea. Tracking his weight from previous hospitalizations shows that he has lost weight and has “fallen off the growth chart.” A pilocarpine iontophoresis sweat test result is significantly elevated and confirms the suspected diagnosis. Of the following, the MOST likely reason for recurrent episodes of pneumonia in this patient would be
Dried mucus accumulation in the lungs
A 10-month-old girl is admitted to the general medical floor of the local children’s hospital for failure to thrive. The girl has been losing weight despite a typical diet for her age. Prior to this hospitalization, she had been admitted three times since birth for severe, recurrent pneumonia. The parents note that stools for the last several months have been bulky and foul-smelling. Of the following, the test MOST likely to be positive in this patient would be
sweat chloride
A 44-year-old woman with known cystic fibrosis is hospitalized for pneumonia and respiratory distress. Due to moving and being lost to follow-up, she was unable to establish multidisciplinary care. Over the last several months, she has had weight loss and symptoms of fat malabsorption. On respiratory examination, there are crackles in the left lung field, decreased inspiratory and expiratory effort, decreased chest wall expansion, and retractions. Plain chest radiography demonstrates left pulmonary infiltrates. Of the following, the MOST likely organism causing pulmonary infection in this patient is
Pseudomonas aeruginosa
A 5-year-old girl presents with failure to thrive. She has had two or three episodes of pneumonia yearly since birth. Past medical history is significant for a diagnosis of meconium ileus during the neonatal period. A sweat chloride level is significantly elevated at 99 mmol/L, which confirms the suspected diagnosis. Of the following, the MOST likely statement regarding pathology to be true, based on the suspected diagnosis in this patient, is that
lung airways are likely colonized with Staphylococcus aureus
A 5-year-old girl presents with failure to thrive. She has had two or three episodes of pneumonia yearly since birth. Past medical history is significant for a diagnosis of meconium ileus during the neonatal period. A sweat chloride level is significantly elevated at 99 mmol/L, which confirms the suspected diagnosis. Of the following, the MOST likely statement regarding management to be true, based on the suspected diagnosis in this patient, is that
replacement of vitamins A, D, E, and K is necessary
A 12-year-old-female visits an urgent care with an acute onset of breathing difficulty. She has a 7-year history of coughing, wheezing, and repeated attacks of difficulty in breathing. The attacks are particularly common in spring. Physical examination shows that she is afebrile. Her lungs are hyperresonant on percussion. Auscultation reveals loud expiratory wheeze bilaterally. Her chest radiograph shows increased lucency of all lung fields. Which of the following histologic features is most likely to be found in her lung?
Remodeling of airways with smooth muscle hyperplasia
Which of the following parameters decreases most significantly in asthma?
FEV1
A 48-year-old male presents to the ER with complaints of cough and breathlessness. He has gradually increased severity of dyspnea over the past 2 years. He also complains of a 4-kg weight loss over the past 2 years. He has smoked two packs of cigarettes per day for 20 years, but not for the past year. On auscultation, decreased breath sounds are heard bilaterally. A chest radiograph shows bilateral hyperlucent lungs. Pulmonary function tests show that FEV1 is markedly decreased, and the FEV1/FVC ratio is decreased. FEV1/FVC ratio decreases in this patient primarily because of
Decrease in the number of alveoli
Which of the following is most likely to contribute to the pathogenesis of emphysema?
Release of elastase from neutrophils
A patient with emphysema is started on a course of treatment. Three weeks later, he returns with complaints of redness, burning and soreness in his mouth. His symptoms are related to oral candidiasis. Which of the following is the most likely cause of his symptoms?
Fluticasone
Most of the fungi that cause lower respiratory tract infections are considered dimorphic because they grow as ___________ in the infected tissue, but as _________ in the natural environment and laboratory.
yeast; mold
A 62-year-old woman with long-standing rheumatoid arthritis on chronic corticosteroid therapy presents with fever and altered mental status. Blood cultures later grow Candida species. Despite appropriate antifungal therapy, she develops widespread tissue damage. Which host defense mechanism is most critical for controlling fungal infections and limiting tissue injury?
Cell-mediated immunity involving T cells
A 35-year-old female presents with a 3-week history of non-productive cough that has worsened with time, shortness of breath and low-grade fever. Her history is significant for smoking a half-pack of cigarettes/day. She denies any history of pulmonary disease, but confirms her HIV-positive status. Physical examination reveals a temperature of 37.5ºC (99.5ºF), pulse is 100 bpm, respiratory rate is 26 breaths/minute, and oxygen saturation is 89% on room air. Numerous scars are noticeable in her forearm region consistent with "needle tracks”. Her lung examination is notable for decreased breath sounds and rhonchi in all fields. A chest X-ray shows a bilateral interstitial infiltrate. What organism is the most likely cause of her symptoms?
Pneumocystis jirovecii
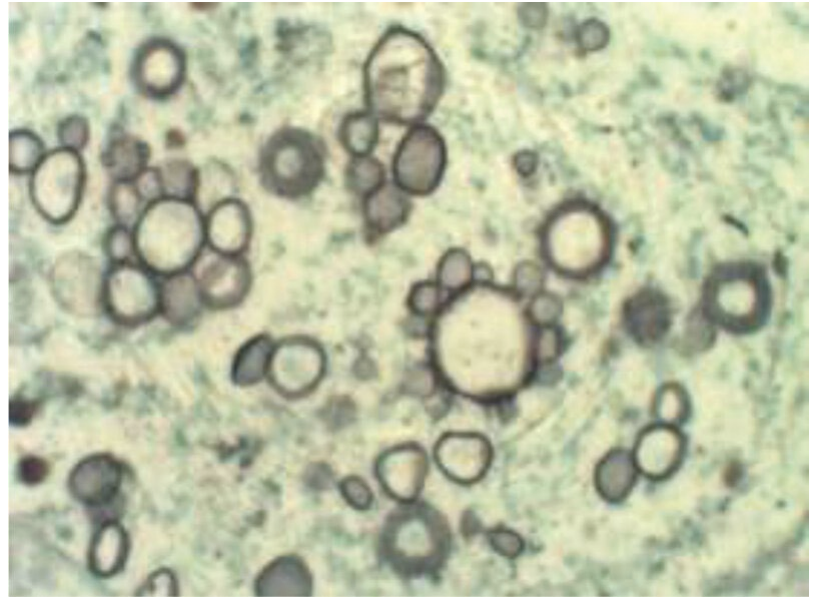
A 42-year-old man originally from rural Brazil presents with chronic cough, weight loss, and painful ulcerative lesions on the oral mucosa. He reports heavy alcohol use and poor nutritional status. Chest imaging shows bilateral pulmonary infiltrates. Biopsy of an oral lesion reveals cells shown in the image. Which of the following organisms is the most likely cause of this patient’s condition?
Paracoccidioides brasiliensis
A 54-year-old man presents to the emergency department with fever, dry cough, headache, and progressive shortness of breath for 4 days. Chest radiograph shows an interstitial pattern He has not been hospitalized recently and has no history of prior antibiotic use. Past medical history is significant for diabetes mellitus (type 2) and COPD. Vital signs reveal tachypnea and hypoxia requiring supplemental oxygen. He is admitted to the medical ward and started on intravenous ceftriaxone monotherapy. Given this patient’s presentation and severity of illness, coverage for which of the following organisms is most significantly missing from this regimen?
Mycoplasma pneumoniae
As you are leaving the supermarket, the cashier tells you that she is worried because her child recently had a positive tuberculin skin test. She had to take him to the health department for skin testing because he had been in contact with her father, who recently was diagnosed with active pulmonary tuberculosis. They told her that the boy’s skin test was positive at “25,” but his chest radiograph was normal. The mother asks you what type of medication her boy should receive. Of the following, the MOST appropriate antituberculous agent to prescribe for this boy is
rifampin
A healthy term newborn has done well in the nursery and is ready for discharge. While speaking with the new mother, the attending physician learn that her brother (uncle) has a coughing illness accompanied by fever, weight loss, and hemoptysis. He often stays at his sister’s home. No other family members, including the infant’s mother, are ill. Of the following, the best management step for the newborn is to:
separate the infant from the uncle.
A 17-year-old boy has a positive interferon-γ release assay test (IGRA). He immigrated to the United States from India at 3 years of age. He received a Bacillus Calmette-Guérin (BCG) vaccine as an infant. All of his family in India and the United States are reportedly healthy, and his grandparents, who live in India, visited him 6 months ago. The BEST step in management of this patient is to
obtain a chest radiograph.

A 17-year-old adolescent girl presents with dyspnea. It is persistent and chronic for 3 months. She also elicits productive, cough, fever, and night sweats of a persistent, chronic nature; chronic bright red hemoptysis; pleuritic chest pain; and loss of appetite. On physical examination, chest crackles are appreciated in the right upper lobe, accentuated after a short cough. Chest radiography is performed as shown. Of the following, what is the most likely location for an anterior Chapman point in this patient?
On the right, 3rd intercostal space, medially
A 29-year-old man is admitted to the intensive care unit for respiratory failure. He has a past medical history of acquired immunodeficiency syndrome (AIDS). Vitals and initial ventilator settings confirm the additional diagnosis of acute respiratory distress syndrome. Computed tomography reveals hilar adenopathy and multiple calcifications within the parenchyma bilaterally in addition to severe bronchiectasis. Upon further workup, an interferon-γ release assay is positive, which confirms the suspected secondary infectious diagnosis leading to the calcifications. Once the patient is stabilized, biopsy of one of the lesions is performed. Of the following, the biopsy will MOST likely reveal
caseous necrosis
A 36-year-old man presents to the outpatient clinic with a chief complaint of cough for 4 months. He states that he immigrated to the United States 15 years ago and lived in a crowded resettlement camp before arriving. He admits to weight loss of 10 kilograms. Upon further workup, an interferon-γ release assay is positive, and plain chest radiography reveals hilar adenopathy and a few pulmonary calcifications, which confirms the suspected diagnosis. Of the following, the factor MOST likely triggering the clinical finding noted on radiography would be
cord factor
A 30-month-old boy has a positive tuberculin skin test (TST) that measures 12 mm. It was placed during a routine well child check in the outpatient clinic. He is well, without fever, chills, cough, weight loss, or night sweats. No known tuberculosis (TB) contacts are identified. Of the following, the MOST likely statement regarding management to be true, based on the suspected diagnosis in this patient, is that
plain chest radiography should be ordered because the TST is positive
A medical student has been exposed to a patient with tuberculosis and developed a positive purified protein derivative (PPD) intradermal skin test. His plain chest radiography is negative. He is placed on a 6-month course of prophylactic treatment, but subsequently develops peripheral neuropathies. Of the following, the vitamin MOST likely to treat the neurotoxicity in this patient would be
vitamin B6 (pyridoxine)
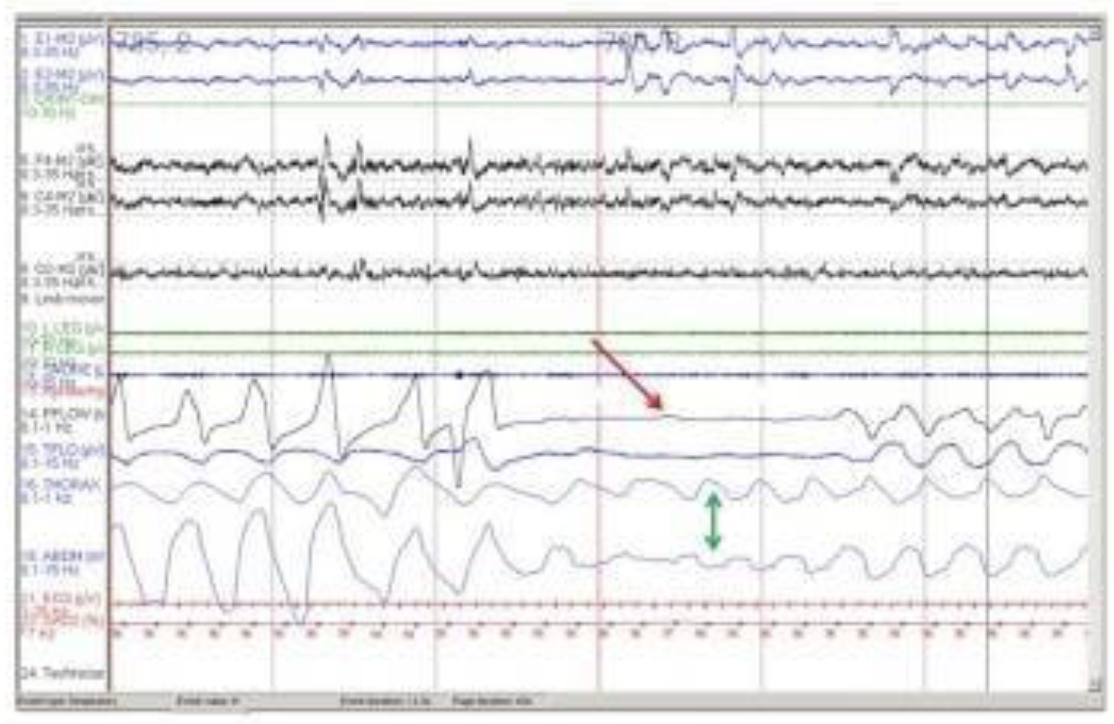
A 50-year-old patient presents to their provider with complaints of excessive daytime sleepiness, fatigue and morning headache. Their partner reports loud snoring with witnesses pauses in breathing. Past medical history is significant for hypertension and a 30 pack-year history of smoking. On physical exam BP is 150/90 and BMI is 40. Polysomnography findings are as shown in the attached image. What is the most likely diagnosis?
Obstructive sleep apnea (OSA)
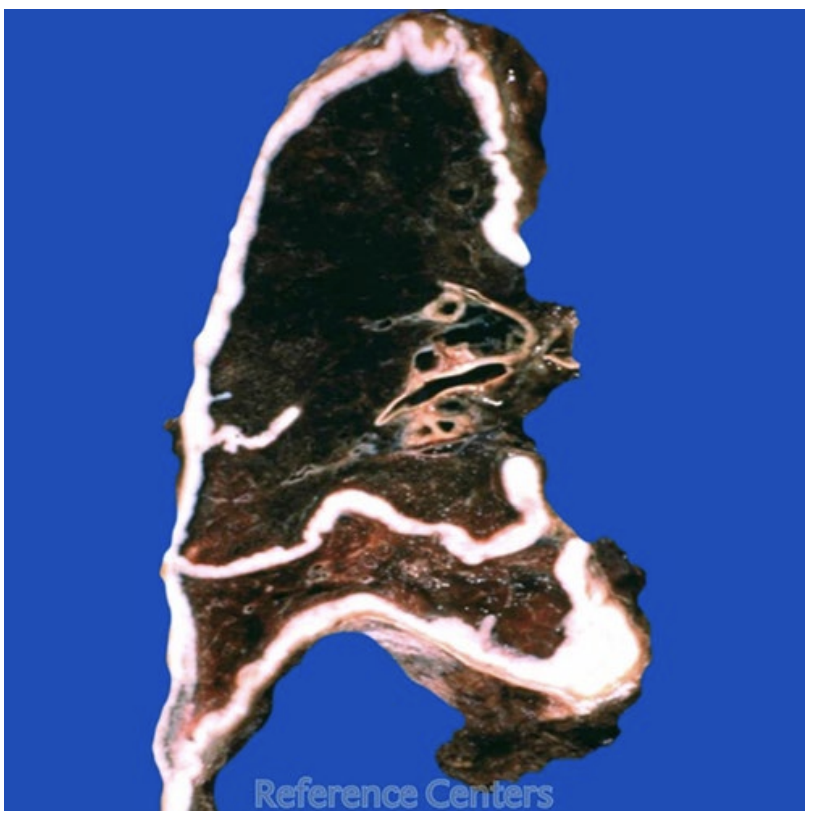
A 72-year-old male has had increasing dyspnea for the past year. Decreased breath sounds are heard on auscultation of the right side of the chest. A chest radiograph shows a large pleural mass that nearly encases the right lung. The representative gross appearance of his lung is shown in the attached figure. A pleural biopsy specimen shows a malignant neoplasm. Exposure to which of the following is associated with these findings?
Asbestos