intro to electrotherapy: electrical currents, activation of excitable tissues and instrumentation
1/85
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
86 Terms
what is electrotherapy
he induction of electrical currents in biological tissue to achieve or facilitate a therapeutic outcome (the resolution of impairment and the restoration of function)
– Electrical stimulation for pain control
– Electrical stimulation for muscle weakness (strengthening)
– Electrical stimulation for wound healing
Impairment oriented interventions
what is electrical current?
the movement of electrically charged particles (mainly ions in humans)
How do electrodes become polarized?
plug it in the wall and stick a battery
What are the ions in human tissues?
POS.: sodium
NEG.: hydrogen and hydroxide
what produces electrical current?
voltage (V)
Current (I)
he driving force for moving charged particles
– a.k.a.: electromotive force (EMF) or electrical potential difference
– EMF is created by electrodes of opposite charge or polarity
Voltage (V)
is proportional to the applied voltage
current (I)
What produces the voltages that separate electrically charged particles?
– Batteries or stimulators and subsequently the surface electrodes
Current is limited by Resistance of tissue to current flow
V = I x R
direct current
alternating current
pulsed current
types of therapeutic currents
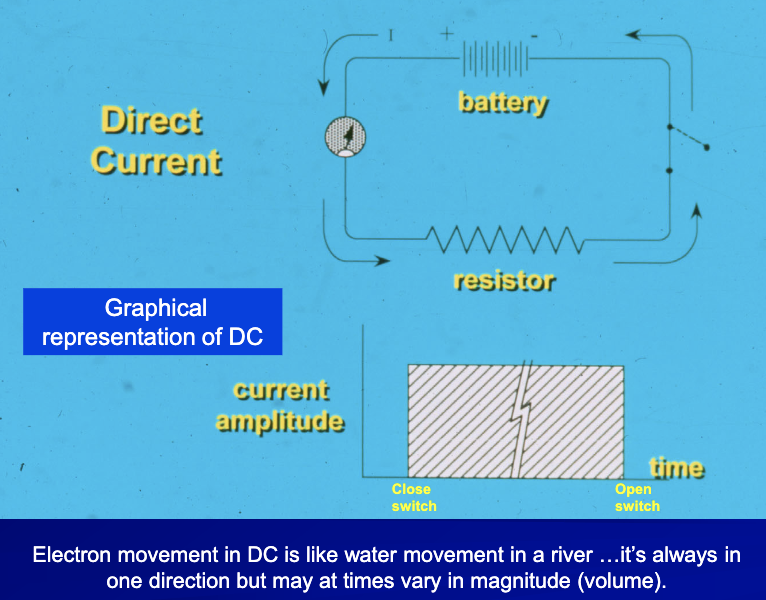
– Continuous (uninterrupted) unidirectional movement of charged particles
– For biological tissues: Anions in one direction, cations in the other
pH changes
moving in one direction and back stop
direct current
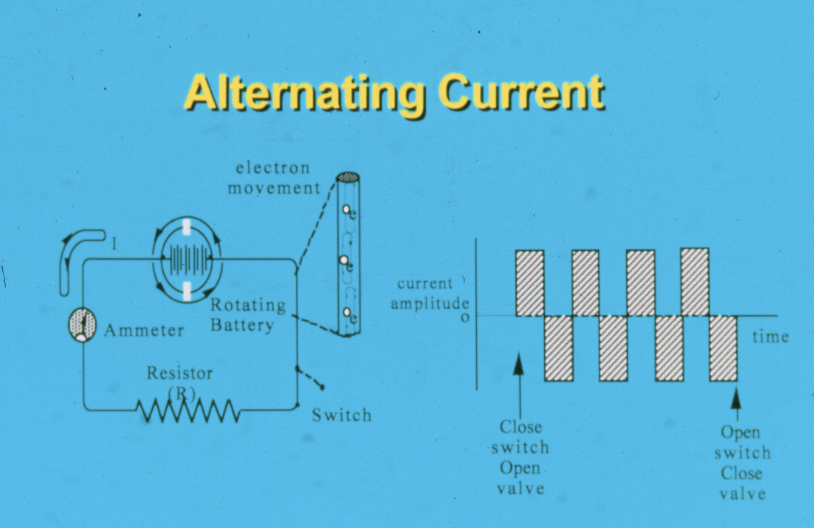
– Uninterrupted (continuous) bidirectional movement of charged particles
– Oscillation of anions and cations back and forth
DC plug it in the wall its AC
pH does not change and ions move back and fourth
alternating current
is alternating current pulse monophasic or biphasic
biphasic
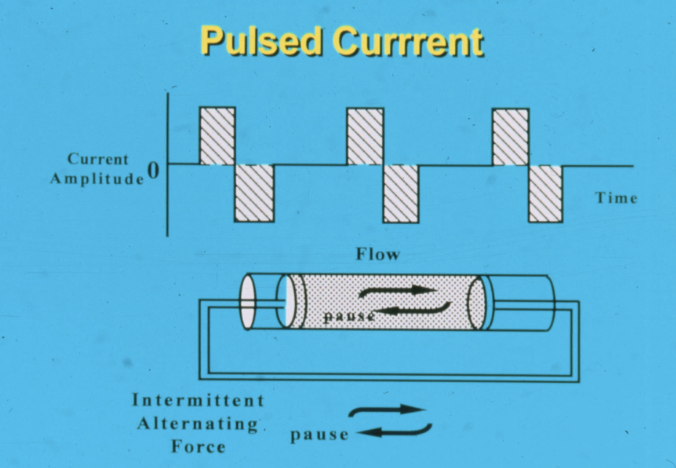
Interrupted, uni- or bidirectional movement of charged particles... ions move very briefly then stop and start
it would be stop, move, stop, move, etc.
often use pulse current
pulse current
is pulse current biphasic or monophasic
can be monophasic and biphasic
why does pulse current not alternate
because there is a pause/time in between
what is the common current PT’s use?
flow, flow, pause
the flow flow rate is frequency
what is the use of therapeutic currents direct current (DC)
– Delivery of medication...iontophoresis
– Enhance wound healing
– Denervated muscle
can use to stimulate and activate a denervated axon
what is the use of therapeutic currents pulsed current (PC) and alternating current (AC)
– Control pain
– Produce muscle contraction....
– Strengthen muscle
– Produce movement (FES)
– Improve blood flow
– Enhance wound healing
what are we stimulating?
we are stimulating the A-MN going to the muscle not the muscle itself
what type of current do we need to stimulate the muscle itself?
direct current (DC), skeletal muscle fibers have to be a DC
What tissues are directly affected by electrical currents in electrotherapy?
electrically excitable tissues:
peripheral nerve fibers
motor axons
sensory axons
autonomic axons
skeletal muscle fibers
cells tissues and bloods
to skeletal muscle fibers (A-alpha)
motor axons
from touch receptors and pain endings A-beta, A-delta, C
Sensory axons
to vascular smooth muscle
Autonomic axons
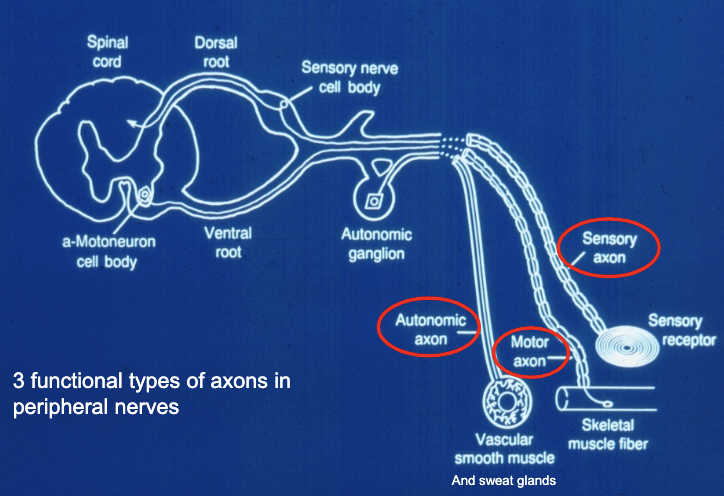
types of axons in peripheral nerves
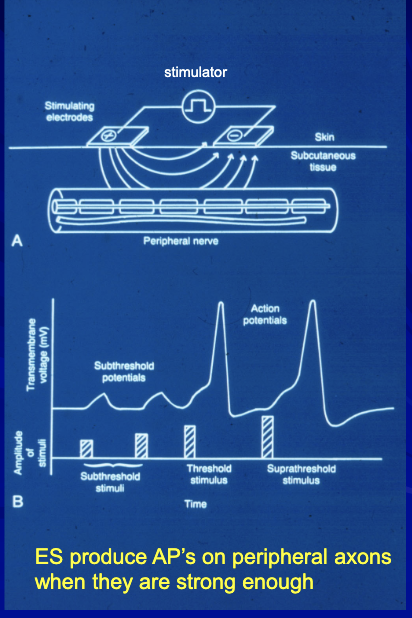
How does electrical stimulation activate peripheral nerve axons?
recruiting more axons to make it feel stronger
recruitment = treat bigger area (amplitude/duration)
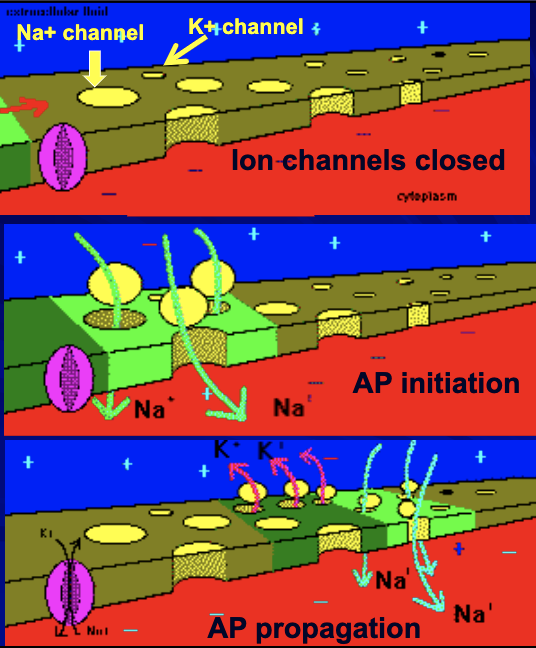
Axon Membrane at rest
what does stimulation open?
Stimulation opens sodium and potassium channels..........channels are “voltage gated”
where does depolarization spread to?
Depolarization spreads to adjacent membrane
What happens when AP’s are produced in peripheral axons with e-stimulation?
A-alpha motoneuron AP’s activate skeletal muscle and cause muscle contraction (motor response)
What happens when AP’s are produced in peripheral axons with e-stim?
A beta cutaneous touch axon AP’s pass into the CNS and produce a “tactile” or touch sensation
A Beta = sensory response (touch pressure)
A-delta or C fibers = pain
A-alpha is the biggest and more myelinated than A-delta
What happens when AP’s are produced in peripheral axons with e-stim?
A-delta and C sensory axon AP’s pass into the CNS and produce the sensations of sharp, fast pain and slow, achy pain respectively
What factors determine the order of activation of peripheral axons with ES?
Size (diameter) of peripheral axon
Location of axon
Stimulus amplitude and duration
– larger diameter axons activated before smaller with ES
Size (diameter) of peripheral axon
– Axons closer to the electrodes activated before those further away
– Why?..... Higher current density close to the
electrodes
Location of axon
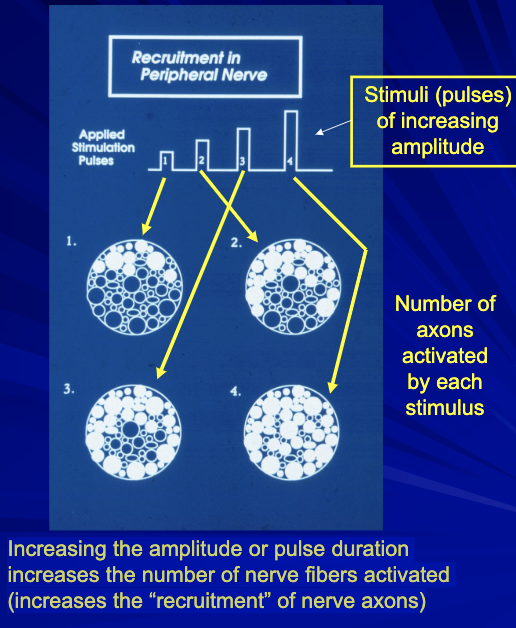
– As amplitude or duration are increased, more axons are activated in response to each stimulus .... called “recruitment
Stimulus amplitude and duration
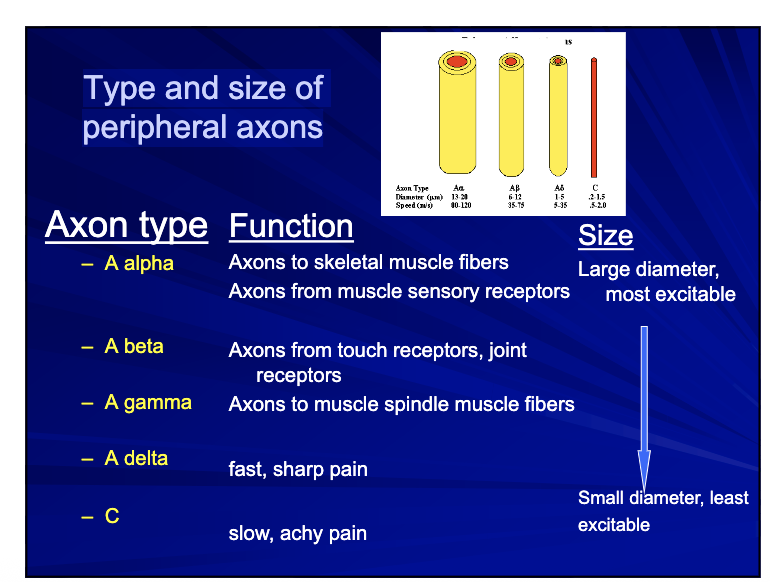
Type and size of peripheral axons
Axons to skeletal muscle fibers Axons from muscle sensory receptors
A alpha
Axons from touch receptors, joint receptors
A beta
Axons to muscle spindle muscle fibers
A gamma
fast, sharp pain
A delta
slow, achy pain
C fibers
Axon size determines the ___ of peripheral axons
“inherent excitability”
as the stimulus is increased
larger axons are activated before smaller
muscle contraction 1st, cutaneous sensation 2nd and pain response 3 rd
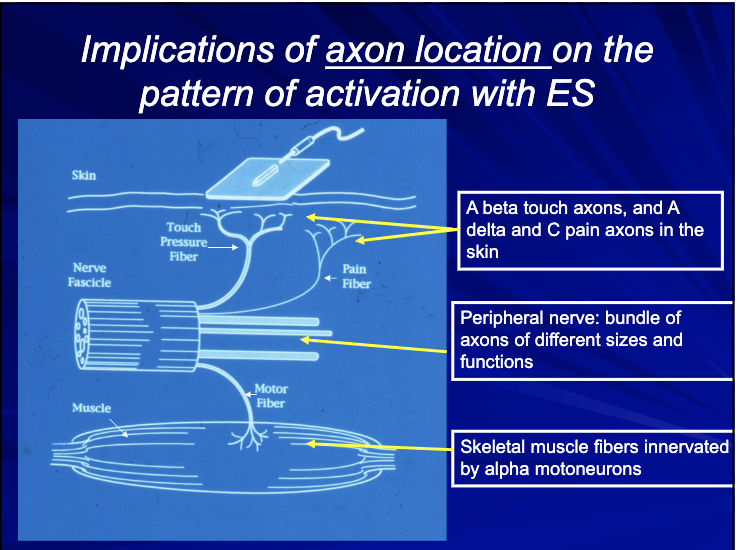
Implications of axon location on the pattern of activation with ES
A beta touch axons, and A delta and C pain axons in the __
skin
bundle of axons of different sizes and functions
peripheral nerve
Skeletal muscle fibers innervated by
alpha motoneurons
The closer the nerve fibers to the electrodes the more likely
they will be activated
__ afferents beneath electrodes first to be activated followed by superficial pain afferents and last motor neurons to muscle fibers... not always the case!
cutaneous touch
Pattern of activation depends on what specific tissues are actually near the electrodes
– e.g. electrode over a superficial nerve bundle vs. over a bony area
By your choice of electrode placement, you may determine which nerve fibers may be activated
– True sometimes but not in every stimulation application
– You must know the anatomy of the area where you are placing electrodes!
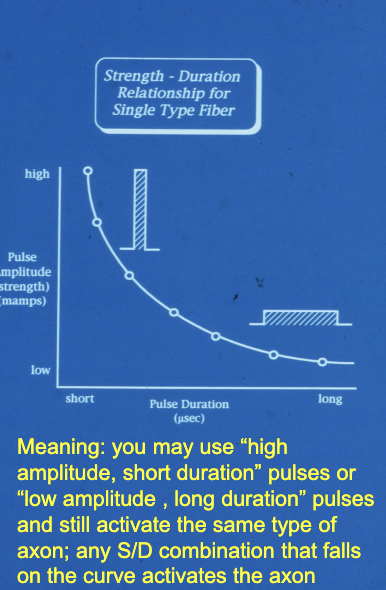
The SD curve is a plot of all of the stimulus amplitude and duration combinations that activate a particular axon
Strength-duration curve
How does the amplitude/or pulse duration of stimulus effect the pattern of axon activation with ES?
Increasing the amplitude or pulse duration increases the number of nerve fibers activated (increases the “recruitment” of nerve axons)
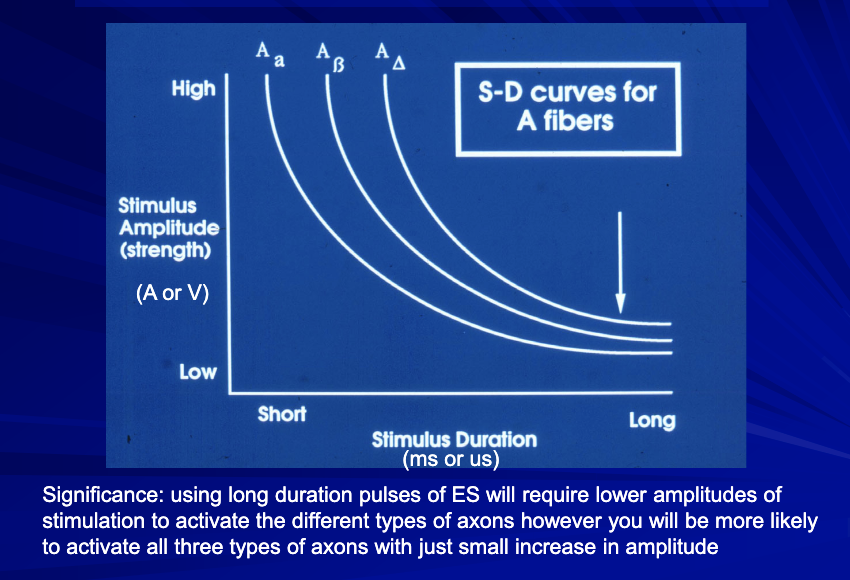
S-D curve based on axon size alone
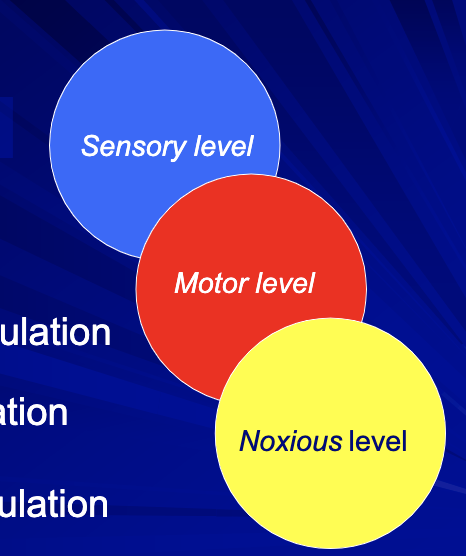
sensory level stimulation
motor level stimulation
noxious level stimulation
Clinical Levels of Stimulation
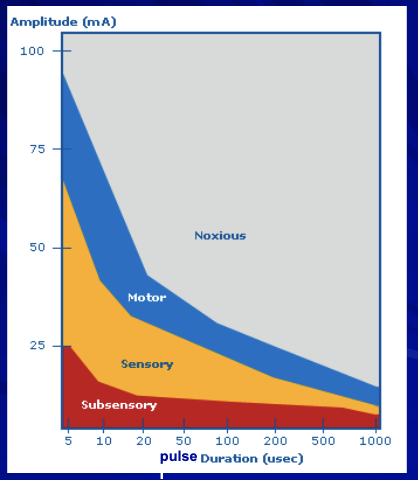
This is the graph that you need to keep in mind whenever you are using ES in a clinical application
when you get to motor, sensory does not stop
Typical S-D curves in electrotherapy based on both axon size and proximity of axons (location) to surface electrodes
Activates (produces AP’s in) superficial A beta cutaneous touch-pressure axons
Produces a tapping sensation with low frequency stimulation (< 5 pps)
Produces a tingling or “pins-and-needles” sensation with higher frequency stimulation (>20 pps)
Tingling may diminish with fixed amplitude stimulation......this is called “accommodation
Sensory level stimulation
Activates (produces AP’s in) A alpha motor neuron axons to skeletal muscle
– Be prepared to describe physiologic sequence of steps leading to muscle contraction
Produces weak,“twitch” contractions with low frequency (< 5 pps) of stimulation and a “tapping” sensation
Produces “unfused” tetanic contractions (“tremor”) at frequencies of 5 15 pps
Produces stronger, “smooth (fused) tetanic” contractions with higher frequency (>20 pps) stimulation with “tingling” sensation
Motor level stimulation
what is being activated at motor level?
A-alphas
if you want fused titanic you want?
frequency (rate coding)
Produces a “pain” response
– due to A delta and/or C fiber axon activation
Cutaneous sensations and contraction persist as stimulation “intensity” is increased from motor to noxious level – Why?
A level of stimulation to be avoided in some clinical applications...Why?
Noxious level stimulation
Traditional designations
Commercial designations
Contemporary designations
Types of currents in electrotherapy
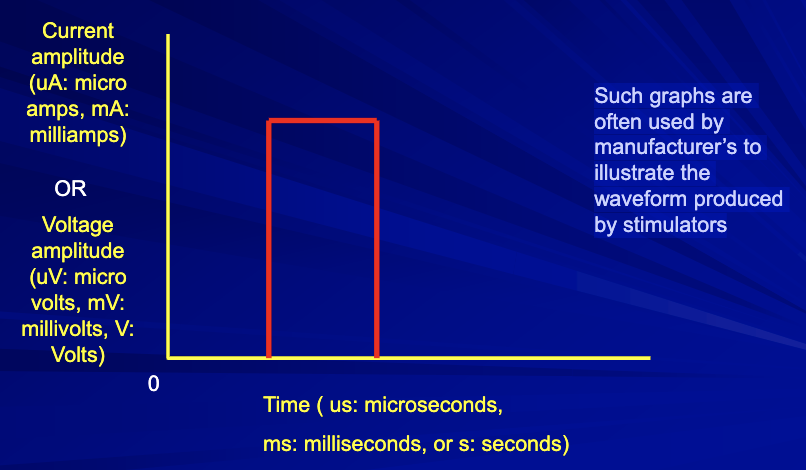
How are electrical currents displayed?...in graphs
Such graphs are often used by manufacturer’s to illustrate the waveform produced by stimulators
Direct Current
Alternating Current
Pulsed Current
Differences between various types of AC and PC clarified by identifying defined quantitative characteristics (parameters) and qualitative characteristics using diagrams of the current or voltage waveforms
Contemporary Designations for Therapeutic Currents
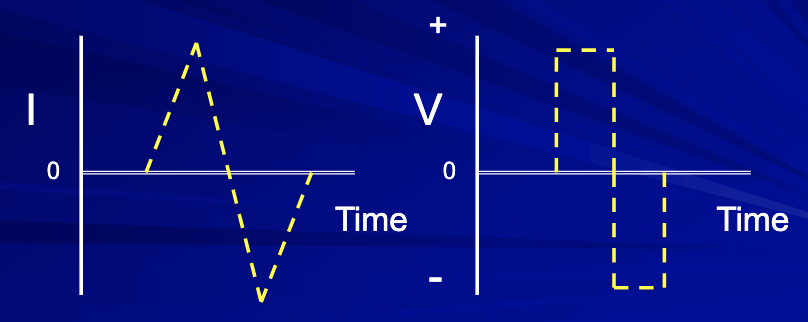
What is a “Waveform”
A visual representation in a graph of the changes in amplitude of current or voltage over time
both are pulsed current
both are biphasic
For individual waveforms or pulses
– Amplitude
– Pulse or phase duration
For a series of waveforms
– Frequency
Pulses/second (pps) for PC
Cycles/second (cps) or Hertz for AC
– On times/off times
seconds on/seconds off
Stimulation parameters that you select, adjust or set
– Amplitude
– Pulse or phase duration
For individual waveforms or pulses
– Frequency
Pulses/second (pps) for PC
Cycles/second (cps) or Hertz for AC
– On times/off times
seconds on/seconds off
For a series of waveforms
On Time/Off Time (secs)
Burst duration/interburst interval
Timing modulations
Automatic, systematic variations in one or more waveform parameters
Modulations:
electrodes
stimulators
Instrumentation in Electrotherapy
– Interface between the client and the “stimulator”
– 2 needed for each “channel” of
stimulator
electrodes
– Clinical models: line-powered
– Portable models: battery operated
– Produce the driving forces to induce currents in tissues
Stimulators
Electrodes size and shapes selected based upon the specific type of ES intervention selected and the requirements of that intervention
You do not use the same type and size of electrodes for all ES applications
Electrodes Sizes and Shapes
Electrodes are connected to the stimulator by electrode leads
An electrode lead is a wire with connectors that attached securely to both the electrode and the stimulator
Electrodes and Leads
Always securely attached to client
Always securely attached to the “leads” of the stimulator
Placement in a manner consistent with the particular impairment managed
Electrodes are not “forever”... all types need to
be regularly replaced– “hot spots” during use indicates electrode must be
discarded and replaced
Specify size and location of electrodes for each
clinical application using anatomical references
Electrode best practices
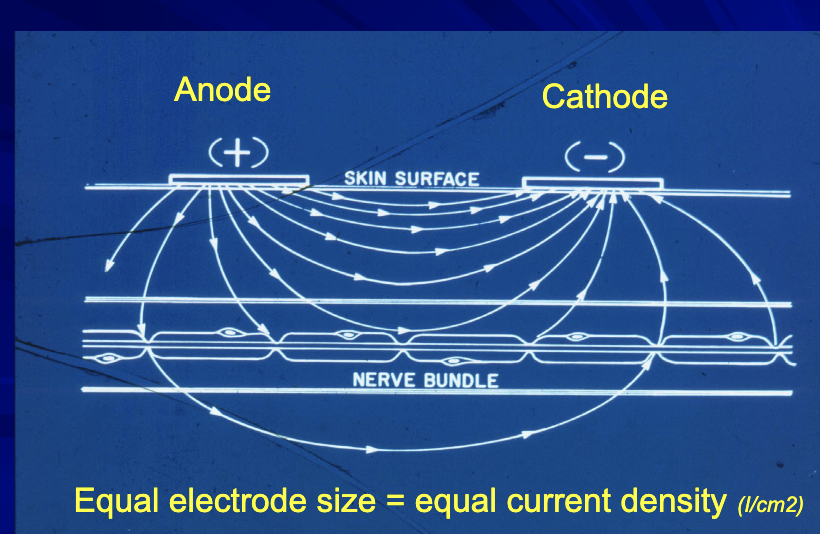
Electrode Size and Current Density
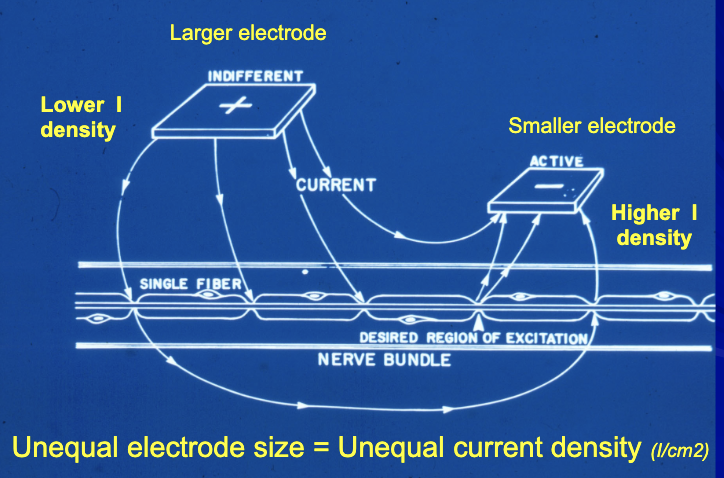
Effect of size and location
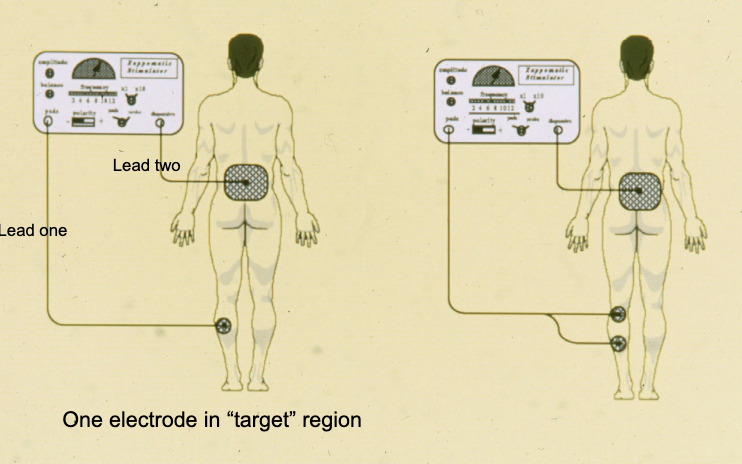
one electrode in target area is called a monopolar set up
two in the area is a bipolar set up
4 in the area is quadripolar
more placements = recruitment
use amplitude to increase
monopolar electrode placements
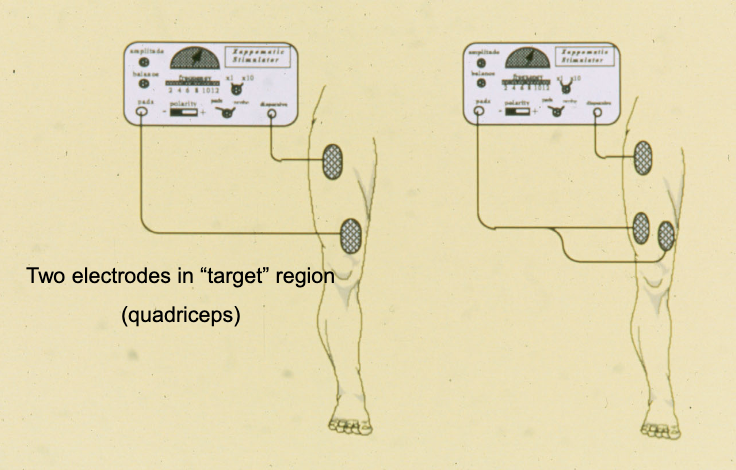
bipolar electrode orientation
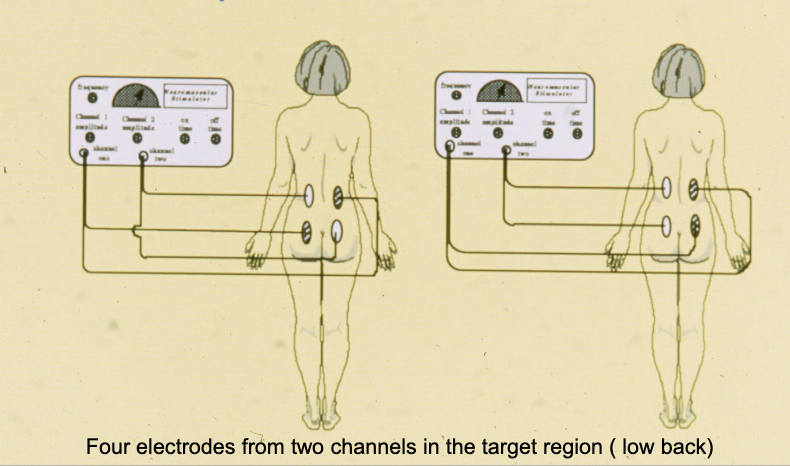
quadripolar electrode orientation
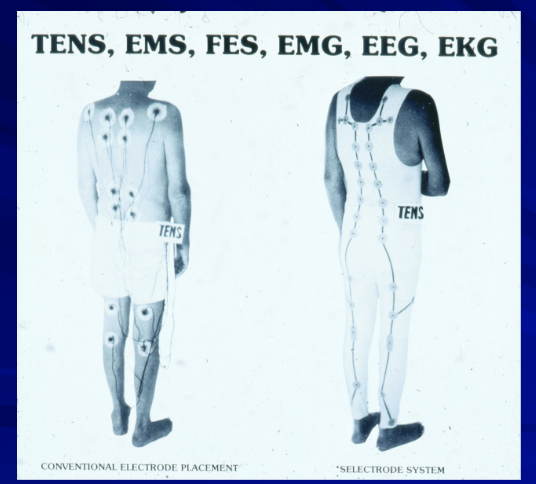
“Selectrode System”
Clinical and portable styles
Constant current vs. constant voltage
– Constant current may be safer
Analog design (rotating dials for controls) vs. digital design (pressure sensitive switches with electronic displays)
Commercial designations (not recommended)
– High volt
– Interferential
– TENS
– NMES
– MENS
– Russian
Types of Therapeutic Stimulators