Topic 1: Neuroanatomy
1/101
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
102 Terms
Neurogenic Communication Disorders
• Consequence of nervous system damage.
• Location + size = severity and outcome —> closer to the language centers - worse outcomes
• Disorders:
-Aphasia
-Motor speech disorders (dysarthria, apraxia)
-Right Hemisphere Syndrome
-Dementia
-TBI
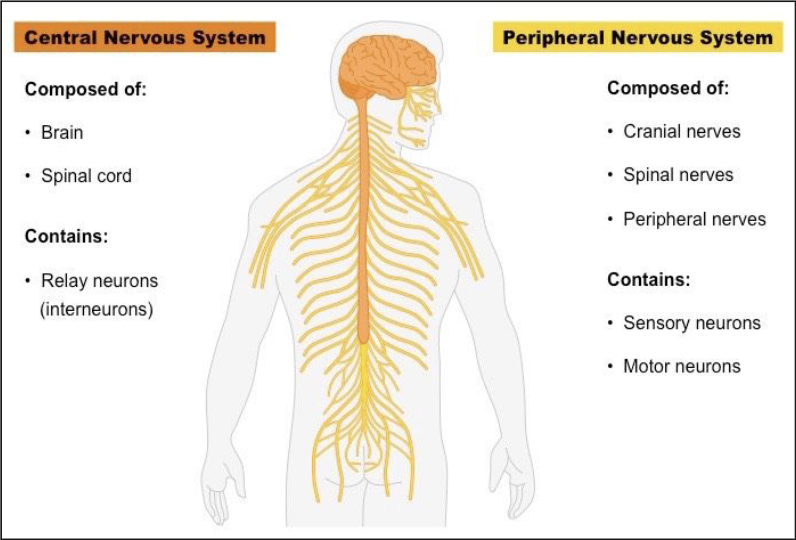
Nervous System
Central Nervous System
+Brain (cerebrum,
brainstem, cerebellum)
+Spinal cord
Peripheral Nervous System
+Spinal nerves (31 pairs)
+Cranial Nerves (12 pairs)
Language Centers are in the Cerebrum!
BS more swallowing problems
Cells of the Nervous System
1) Neurons (Nerve cells)
conduct and receive electrical impulses
responsible for actions of muscles, organs, glands
sensory & motor
Types:
sensory —> light sound touch taste temperature smell
motor —> muscles/body parts move
interneurons
100 Billion Neurons
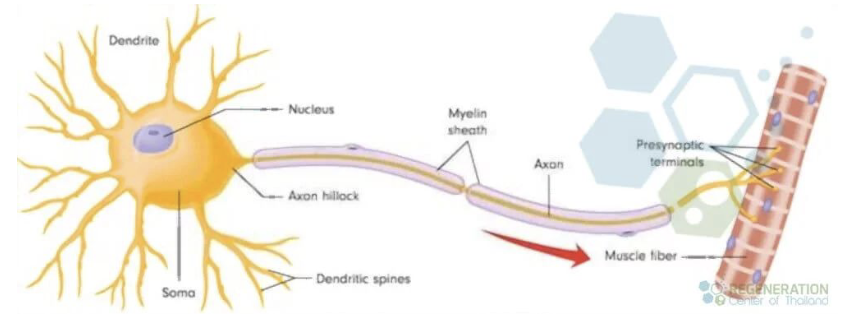
Each neuron has:
cell body (soma) —> processes informatino that is sent in
dendrites RECEIVE —> fingerlike — receive electrical impulses/info from other cells and give it to the cell body
axon SEND —> extends from cell body sends nerve signals away to other parts of the nervous system (connect to muscle)
Synapse = from cell to cell where axons meet (receptor site)
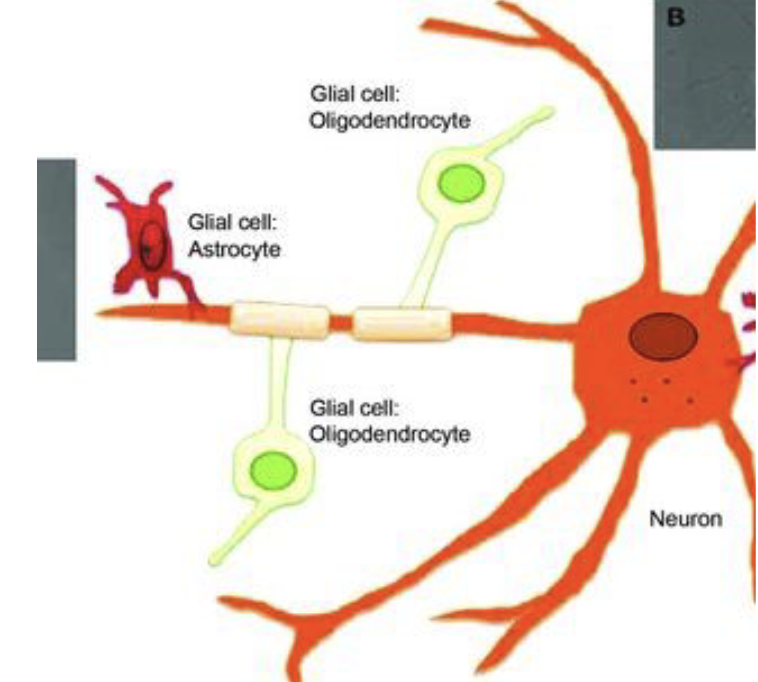
2) Glial cells (helper cells)
GLIAL= glue
connective tissue
support neurons
NO electrical impulses
Job : regulate fluid, remove foreign substances, metabolism
excessive alcohol abuse
(connections damaged - metabolism isn’t what it used to be)
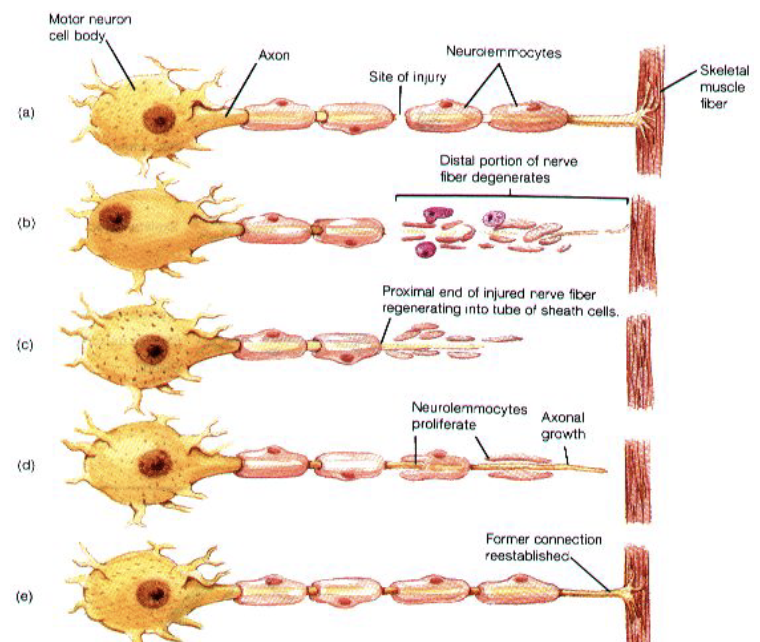
Damage to nerves
● Once axons are injured or destroyed
by disease/damage, do NOT
regenerate to the same extent
● Regeneration depends on type and
location of injury
● Peripheral nerves have better ability
to regenerate than central nerves
Severity, age, how long it took to get TX, underlying conditions (alzheimers + stroke), strokes prior?
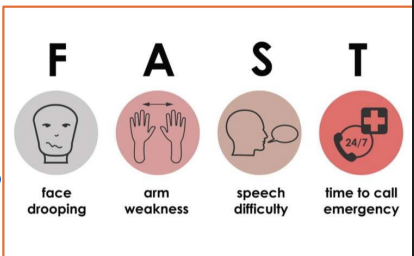
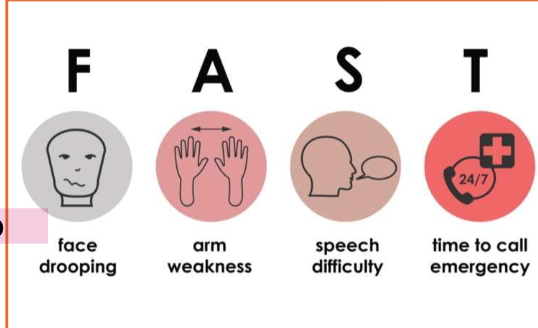
FAST - face arm speech time
Peripheral nerves have better chance at recovering
Axon is thinner after connection is reestablished (weaker, more likely to be damaged, electrical impulse doesn’t travel as smoothly -
ex) delayed or related example saying dog instead of cat
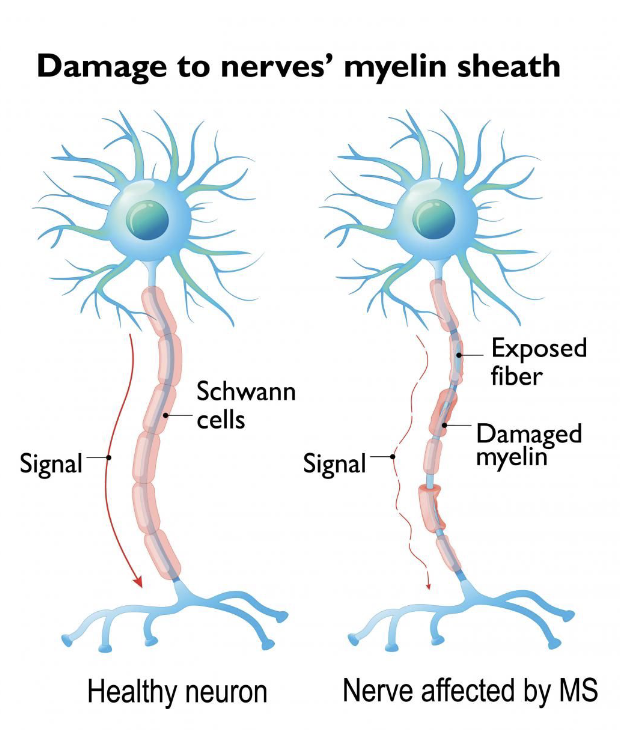
Myelin
thin layer of white, fatty substance
provides electrical insulation for nerve axons
some disease characterized by loss of myelin, which slows connection = weakness, impaired muscle control
IMPORTANT DEF —> keeps electrical signal functioning and in the right spot (fast too)
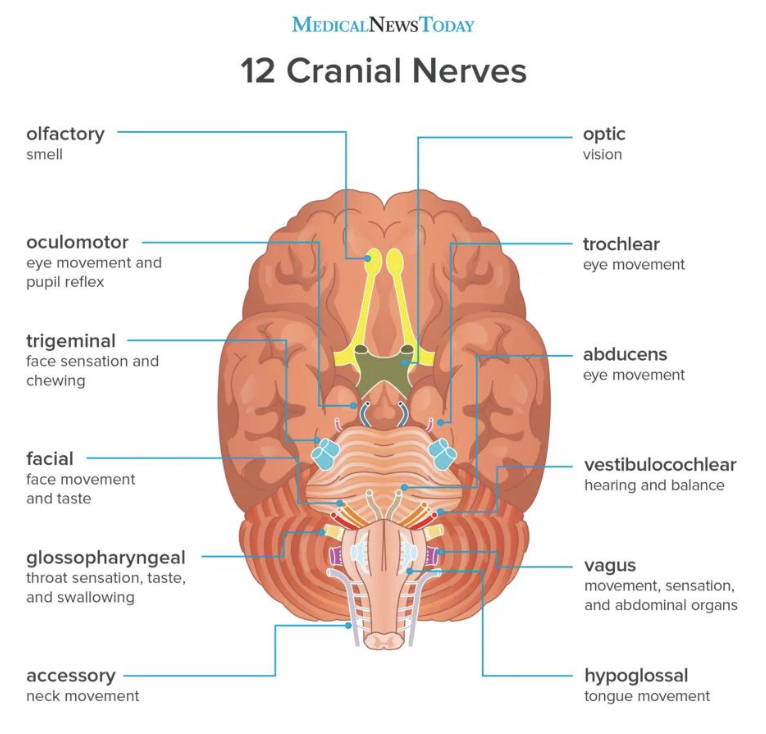
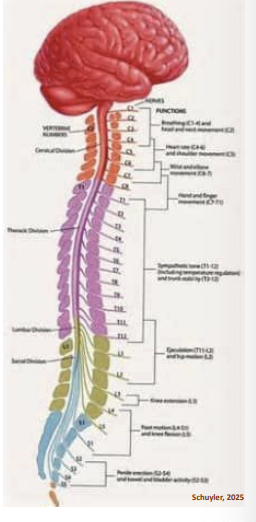
Peripheral Nervous System: Cranial & Spinal nerves
• Cranial nerves (12 pairs) = control muscles in head and neck
BOTH sensory and motor function
• Spinal nerves (31 pairs) = serve structures in the torso and limbs.
• PNS serves as a channel for sensory information from the body’s
sensory receptors to CNS, and for motor commands from CNS to the
muscles.
• Sensory fibers in cranial nerves transmit information from sensory
receptors in the head and neck to the CNS.
• Most cranial nerves connect with the CNS in the midbrain, pons, and
medulla.
PNS: 2 functional systems
-Somatic nervous system-enables us to perceive sensory
stimuli and carry on volitional motor activity.
-Autonomic nervous system-self-regulating system that
controls the glands and vital functions such as breathing,
heartbeat, and blood pressure.
digestion, toxins, blood pressure
Cranial Nerve Review
Label the cranial nerves by #
1 Olfactory —> smell
2 Optic —> vision
3 Oculomotor —> eye movement & pupil reflex
4 Trochlear —> eye movement
5 Trigeminal —> face sensation & chewing
6 Abducens —> eye movement
7 Facial —> face movement and taste
8 Vestibulocochlear —> hearing and balance
9 Glossopharyngeal —> throat sensation, taste/swallow
10 Vagus —> movement, sensation, abdominal organs
MOTOR ONLY
11 Accessory —> neck movement
12 Hypoglossal —> tongue movement
Oh once one takes the anatomy final very good vacations are heavenly
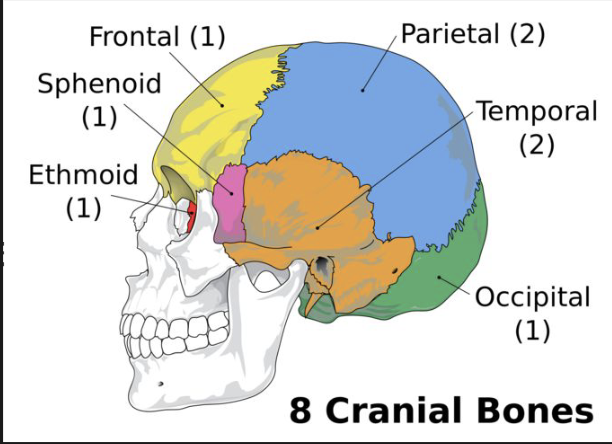
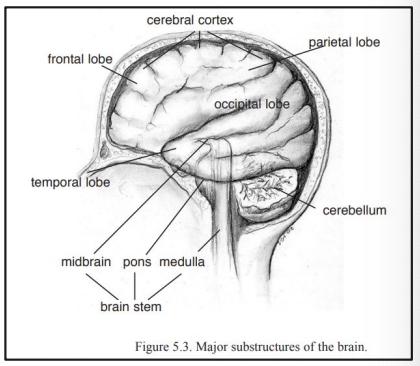
Central Nervous System
Includes: brain (cerebrum), brainstem, cerebellum, spinal cord
Supports perception and discrimination of sensory stimuli and expression of emotion.
Keeps processes like respiration and heartbeat going.
Organizes and regulates behavior.
Enables us to engage in mental processes such as thinking, remembering, and understanding information.
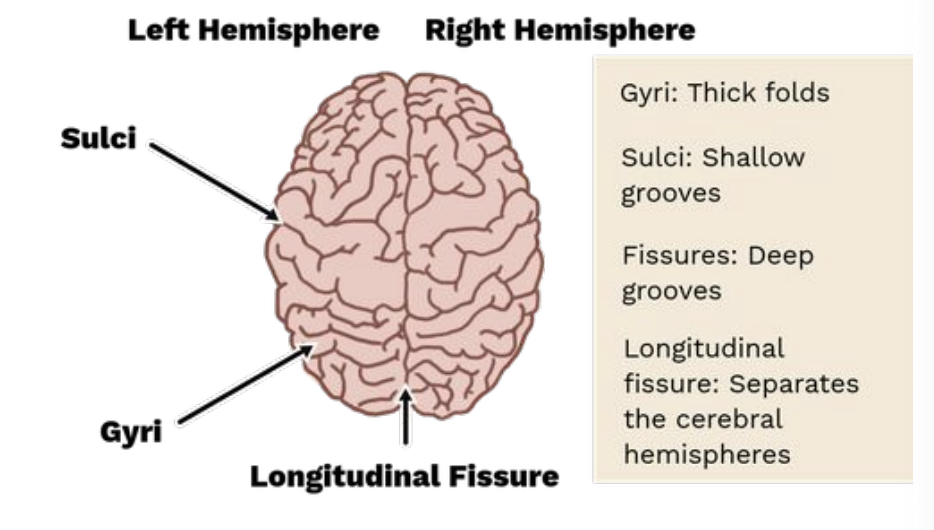
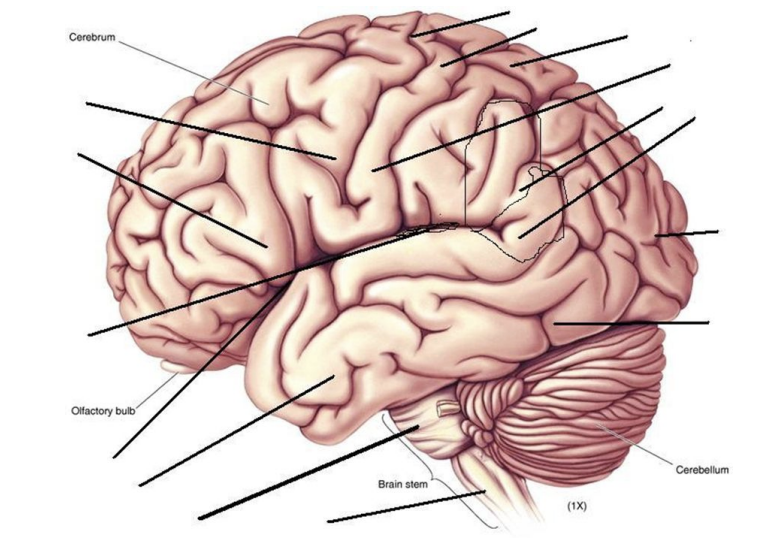
Brain
Mass of nerve cells and supportive tissue in CSF [ Cerebrospinal fluid]
Brain is completely dependent on a constant supply of oxygen and nutrients.
Cerebrum: 2 hemispheres (L & R) sit atop brain stem
Longitudinal cerebral fissure divides two hemispheres
Hemispheres communicate via corpus callosum
Receive sensory information from contralateral side of body and movement is affected on contralateral side of body
corpus callosum connect 2 sides of the brain —> contralateral issues
10 sec lose consciousness, 20 electrical currents stop, 2+ min permanent brain damage
Language in the LEFT
RIGHT —> emotions, music cognitive (memory/planning, pragmatics)
![<ul><li><p>Mass of nerve cells and supportive tissue in CSF [ Cerebrospinal fluid]</p></li><li><p>Brain is completely dependent on a constant supply of oxygen and nutrients.</p></li><li><p>Cerebrum: 2 hemispheres (L & R) sit atop brain stem</p></li><li><p>Longitudinal cerebral fissure divides two hemispheres</p></li><li><p>Hemispheres communicate via corpus callosum</p></li><li><p>Receive sensory information from contralateral side of body and movement is affected on contralateral side of body</p></li></ul><p></p><p>corpus callosum connect 2 sides of the brain —> contralateral issues</p><p>10 sec lose consciousness, 20 electrical currents stop, 2+ min permanent brain damage </p><p>Language in the LEFT</p><p>RIGHT —> emotions, music cognitive (memory/planning, pragmatics)</p>](https://knowt-user-attachments.s3.amazonaws.com/3e0bec85-bbea-40d9-aee6-da0766255d26.png)
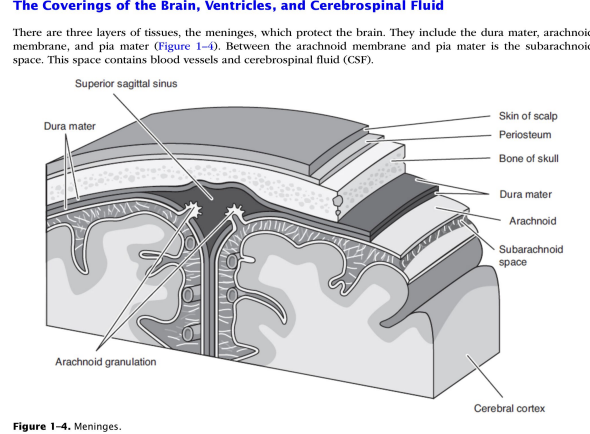
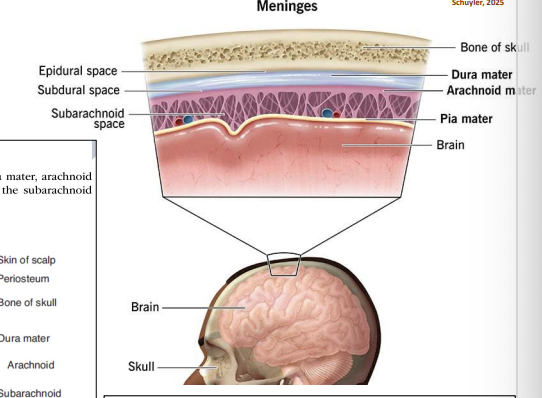
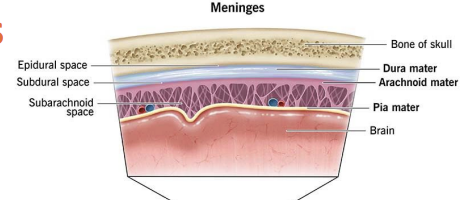
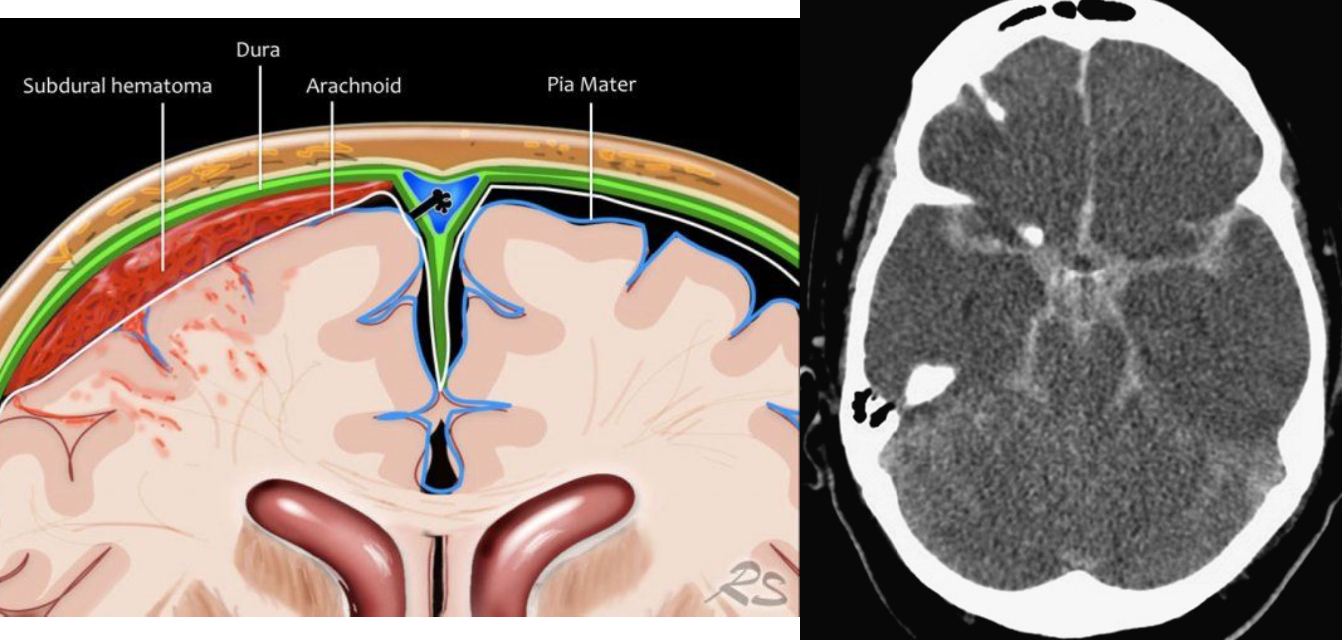
Brain Layers
dura —> thickest and most durable
arachnoid —> thinner than the dura
subdural —> below the dura
subarachnoid —> CSF
pia mater — >adheres to the surface of the brain (soft and fragile) blood supply to the brain
CLOSER TO BRAIN - WORSE DAMAGE
Cerebral Ventricles
● 4 ventricles: 2 lateral, 3rd ventricle, 4th ventricle
● Each contain choroid plexus (produces CSF)
CSF: cerebrospinal fluid [plasma] provides nourishment, shock absorber, protection/waste removal
● Blockage in any of these can result in pressure on brain
![<p>● 4 ventricles: 2 lateral, 3rd ventricle, 4th ventricle</p><p>● Each contain choroid plexus (produces CSF)</p><ul><li><p>CSF: cerebrospinal fluid [plasma] provides nourishment, shock absorber, protection/waste removal </p></li></ul><p>● Blockage in any of these can result in pressure on brain</p>](https://knowt-user-attachments.s3.amazonaws.com/882b699c-e42b-4cae-bde5-c041d56fe7f9.png)
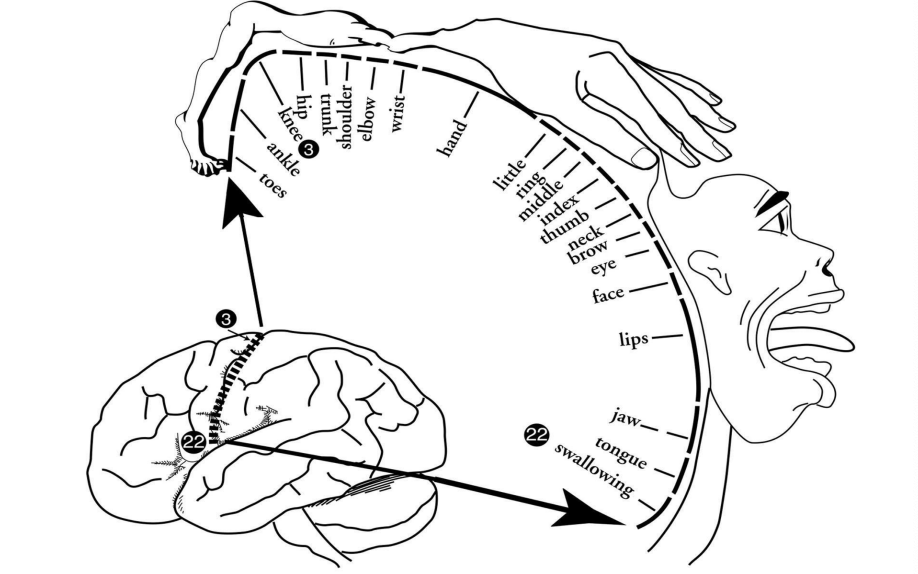
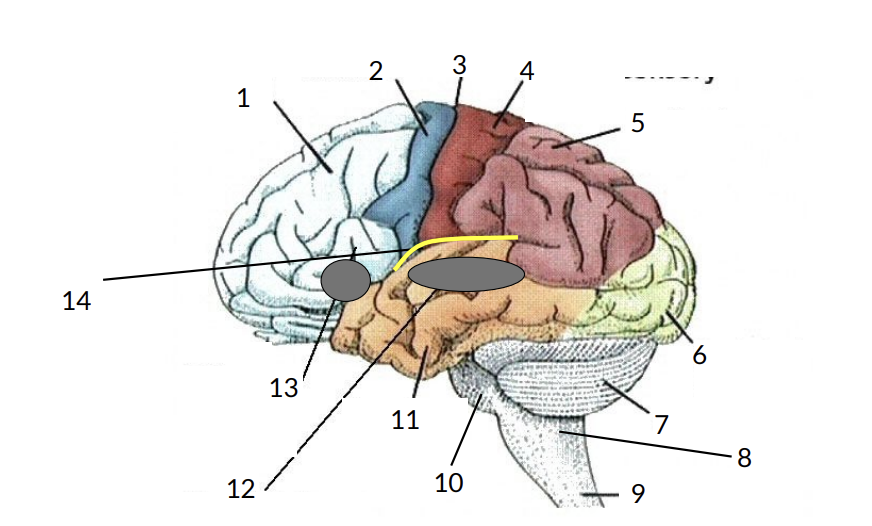
Major Gyri of Cerebral Hemispheres
Gyri thick folds of the brain (gray matter) —> nerve cells here
Hemispheres
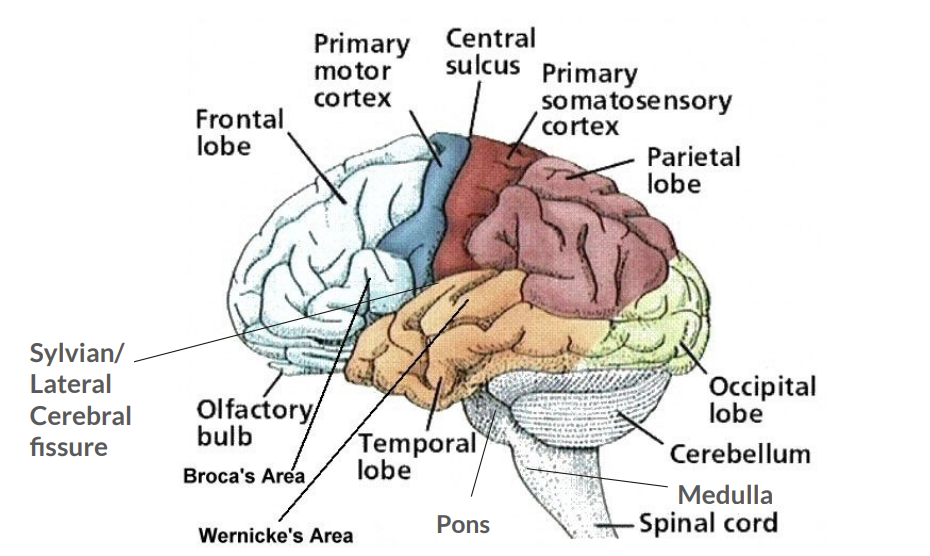
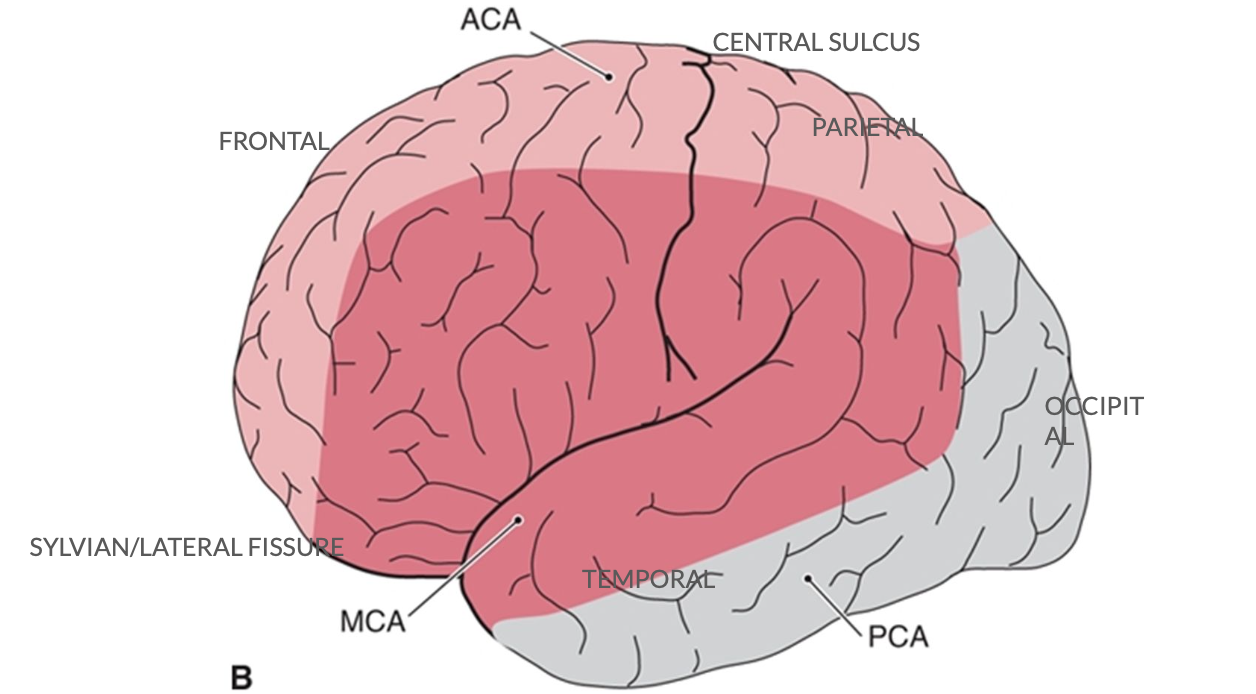
Each hemisphere is divided into 4 lobes:
1. Frontal lobe [EF, personality, emotion]
2. Parietal [perception, sensory awareness]
3. Occipital [vision]
4. Temporal [receptive language, hearing]
![<p>Each hemisphere is divided into 4 lobes:</p><p>1. Frontal lobe [EF, personality, emotion]</p><p>2. Parietal [perception, sensory awareness]</p><p>3. Occipital [vision]</p><p>4. Temporal [receptive language, hearing]</p>](https://knowt-user-attachments.s3.amazonaws.com/be6bbeaa-f345-4daf-837d-014c37e7540c.png)
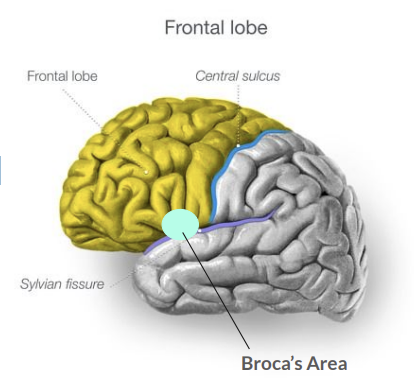
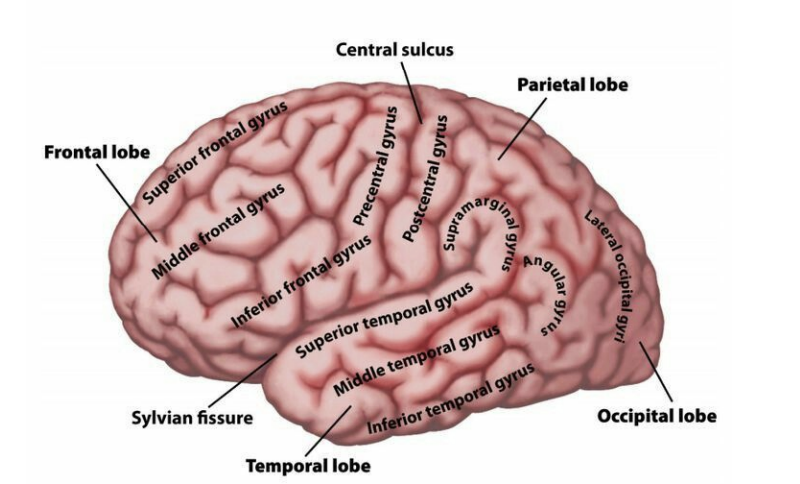
Frontal Lobes
● Lateral cerebral fissure (Sylvian): lower boundary for frontal lobe
● Central sulcus: posterior boundary
● Regulate general activity levels, formulating intentions, plans, and patterns for volitional behavior responsible for planning and executive function
● Expressive Language
● Cognition
● Damage: Difficulty expressing communication, irregular behaviors, personality changes, attention, loss of flexible thinking, decision making, mood changes
sylvian fissure = lateral cerebral
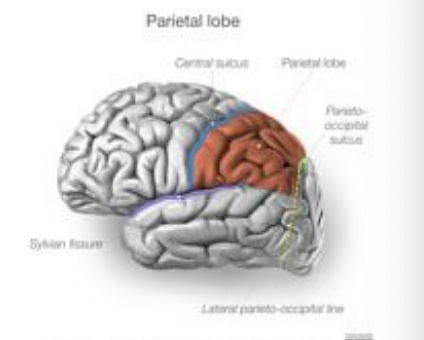
Parietal Lobes
● Lies behind the central sulcus and above the lateral fissure in each hemisphere.
● Important for perception, integration, mediation of sensory information (ie., touch, body awareness, and visuospatial information)
damage: don’t know where they are in space, reading, writing, visual, neglect, perception of touch
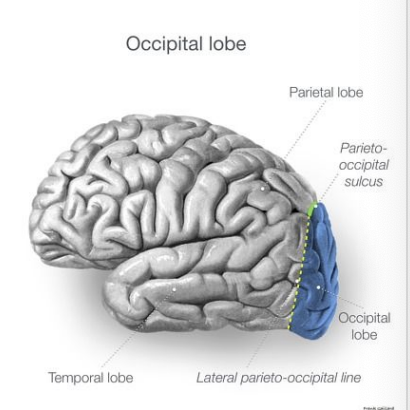
Occipital Lobes - perception (receive and process)
● Posterior part of each hemisphere.
● Extend from the posterior boundary of the parietal lobe to the longitudinal cerebral fissure
● Contain primary visual cortex and visual association areas
● Processes visual information
damage: vision reading/writing, visual neglect, ability to identify colors
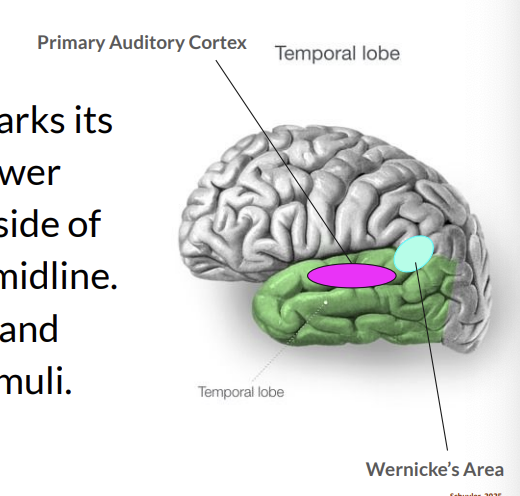
Temporal Lobes
● Lateral cerebral fissure marks its upper boundary and its lower boundary in on the underside of the hemisphere near the midline.
● Important for perception and processing of auditory stimuli.
● RECEPTIVE LANGUAGE
close to the ears, receptive, auditory stimuli (wernickes)
Damage: receptive language (difficulty understanding), looks like memory loss (can’t explain - looks like they forgot), attention
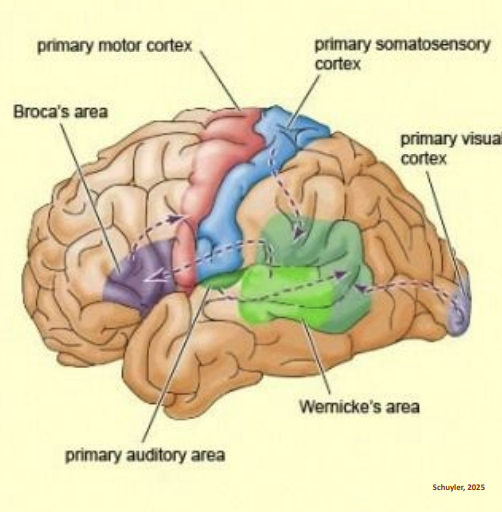
Brain-Cortex
▪ Cerebral cortex / Cerebrum: outer layer of cerebral hemispheres
▪ Major functional categories:
1) primary motor cortex
2) primary sensory cortex
3) primary auditory cortex
4) primary visual cortex
Brain Matter
● Grey Matter: brain cells
○ Outer surface containing nerve cells
○ Recall: responsible for directing motor/sensory stimuli
● White Matter: how FAST signals get sent b/w brain cells
○ Consists of axons
○ Damage to white matter:
■ Multiple sclerosis (MS): destroys myelin sheath
■ Alzheimer’s Disease: white matter changes result in plaque
Brain Stem
● Communicative and structural link between the brain and the spinal cord.
● Cranial nerves originate here*
● Pathway: motor nerve fibers from brain →spinal cord.
● Pathway: Sensory nerve fibers from periphery →brain.
● Damage to brain stem has effects both on motor and sensory functions.
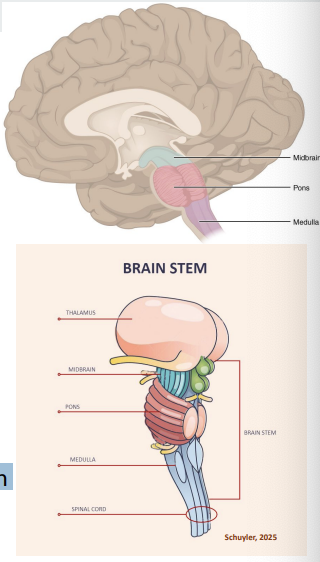
Brain Stem
Divided into 3 parts:
1. Midbrain-connects the brain stem with the cerebral hemispheres
a. Cranial nerves III & IV (vision, hearing, movement)
b. Common disorder: Parkinson’s
2. Pons (middle)-contain several nuclei involved in hearing and balance plus the nuclei CNV, CN VI, CN VII.
3. Medulla (lower)-connects the pons and the spinal cord.
a. Contains nuclei for five cranial nerves (CN VIII-CN XII): Speech motor control, phonation, articulation, VP closure, swallowing, alertness, sleep
b. Damage: vertigo (dizziness), paralysis of muscles of the throat and larynx, and various combinations of sensory loss in limbs and sometimes face.
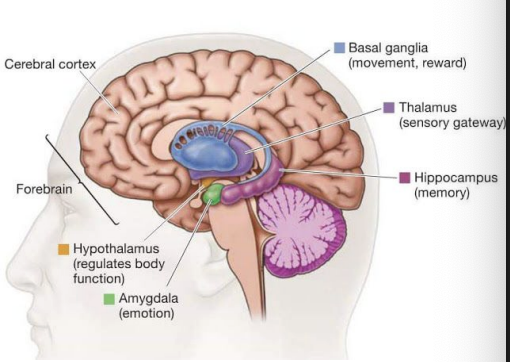
Diencephalon
● Regulation & integration of motor/sensory input
● Contain:
○ Thalamus
■ Receives motor input from cerebellum, basal ganglia, brainstem
■ Relays sensory input
■ Important in maintaining consciousness, alertness, attention
○ Basal ganglia [PD, huntingtons, CP, tardive dyskinesia]
■ Receives input from cortex (frontal lobe) and send to cortex
■ Reflex, posture, complex movements
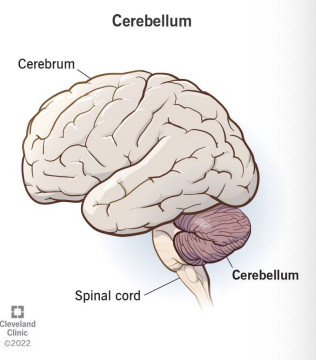
Cerebellum
Lies beneath the posterior temporal lobes.
Does not initiate movements, but coordinates and modulates planned motor movements initiated elsewhere (primarily motor cortex).
Regulates rate, range, direction, and force of movements.
Cerebellar damage causes ataxia [without coordination]
infection common, alcohol, drug use medication use
Spinal Cord
• 18 inches long in normal adult
• Extends from the first cervical vertebra to the first lumbar vertebra and then continues downward as a fine bundle of nerve fibers.
• Spinal cord connected to muscles and sensory receptors by spinal nerves.
• Functions:
1. Reflex arc: urgent messages (ie., pain + motor movement)
2. Sensory: upward to brain
3. Motor: from brain outward
Neurons/Nerve Tracts
1) Projection fibers-long distance carriers of CNS. Carry information from the brain to the brainstem and spinal cord or from periphery sensory nerves to the brain via spinal cord.
-Efferent (motor) projection fibers carry command and control signals from the brain to muscles and glands.
EXIT the brain (brain to body)
-Afferent (sensory) projection fibers carry sensory information from receptors in the periphery to CNS.
Affect=emotion
Sensory to CNS
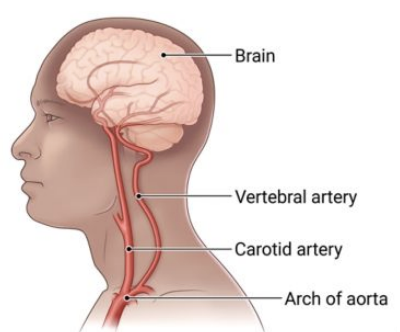
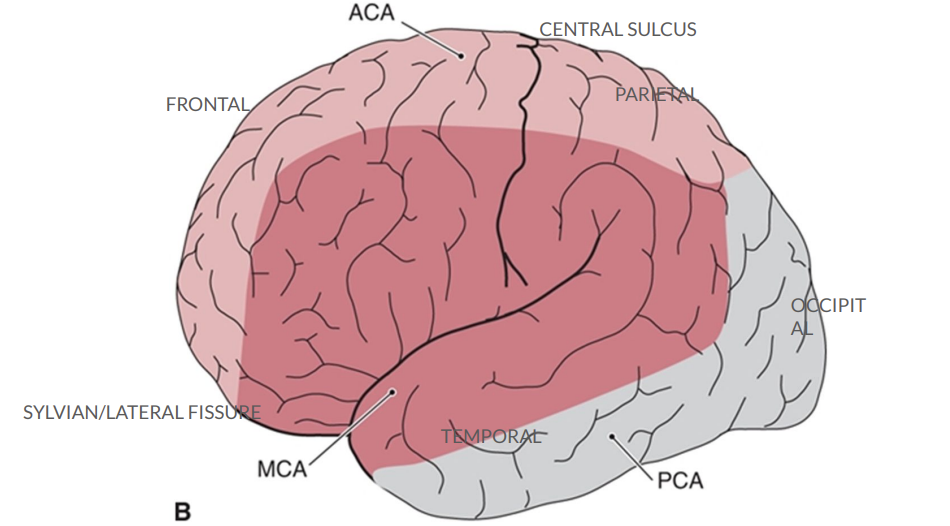
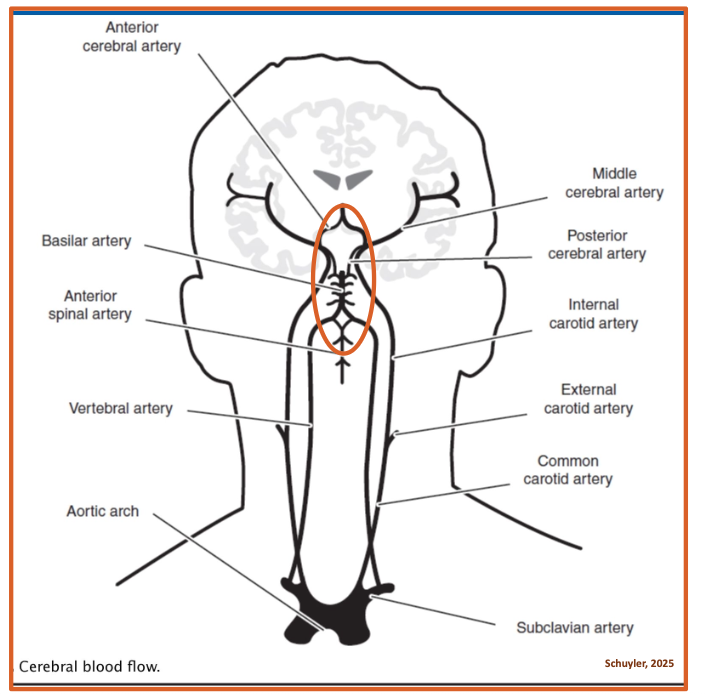
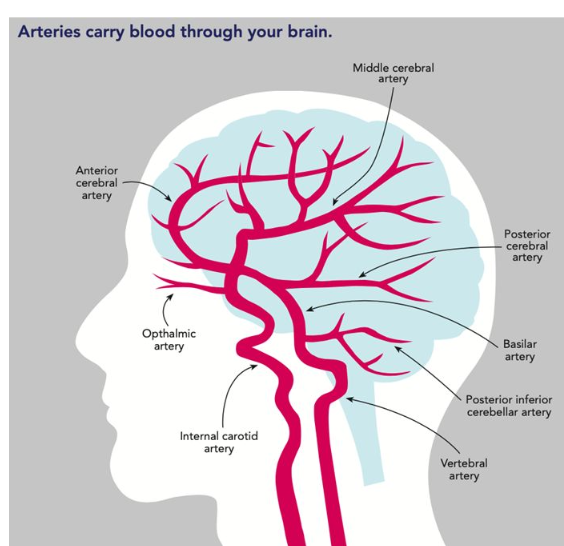
Blood Supply in Brain
⚫ At any given time about 25% of the blood in the body is in the brain.
⚫ Mechanical process of getting blood to the brain begins at the heart, where pumping pressure pushes blood through the arteries.
⚫ Heart pumps oxygenated blood into the aorta, major artery from the heart.
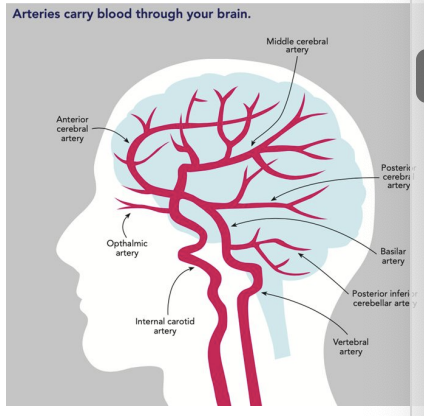
Blood Supply Arterial/Carotid System
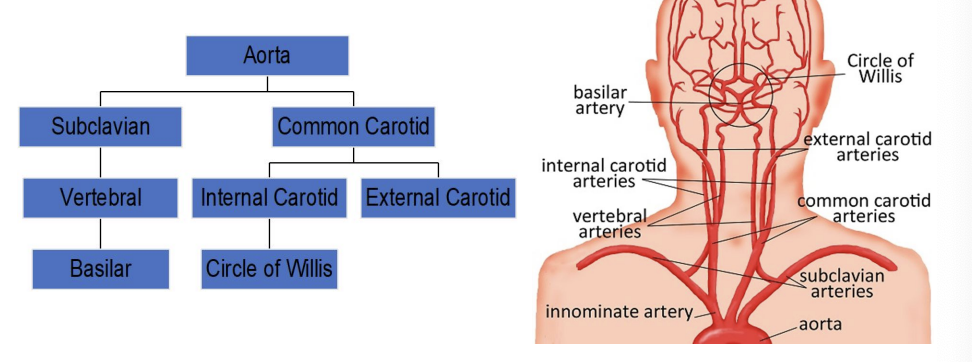
Blood Supply Vertebral System
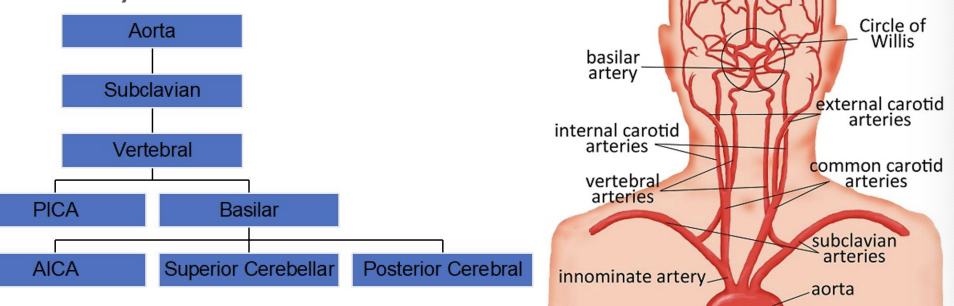
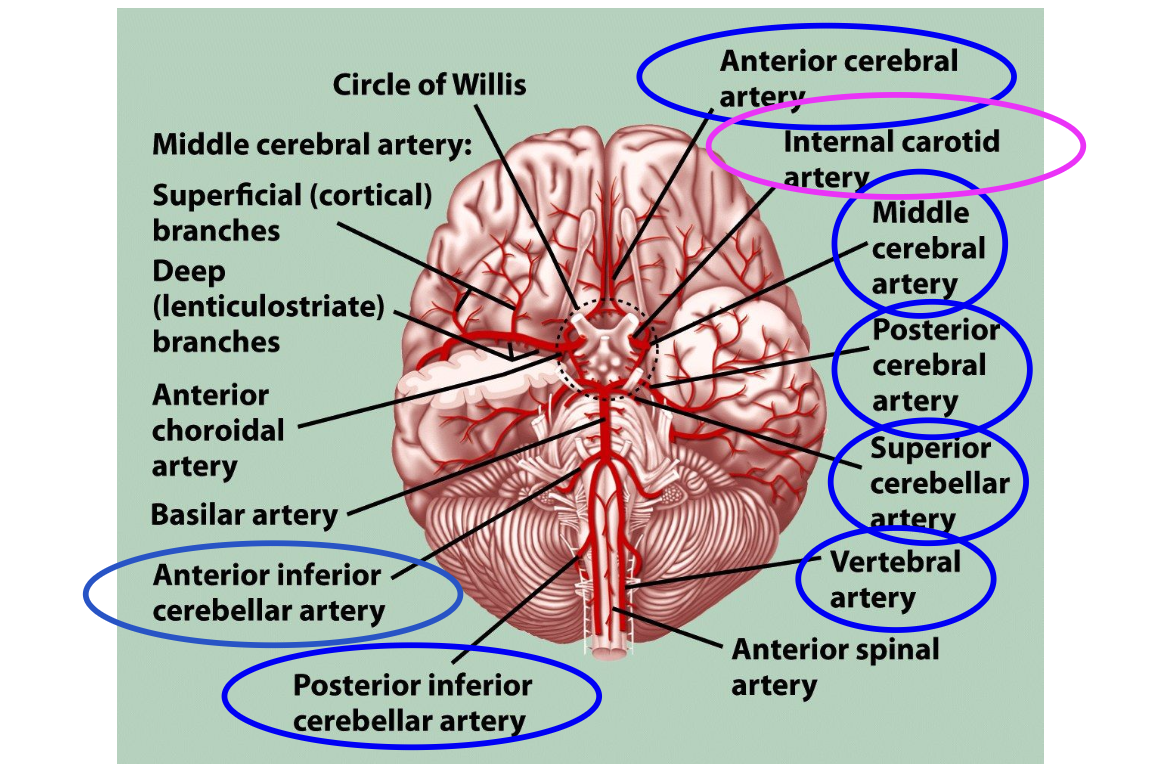
Cerebral Arteries
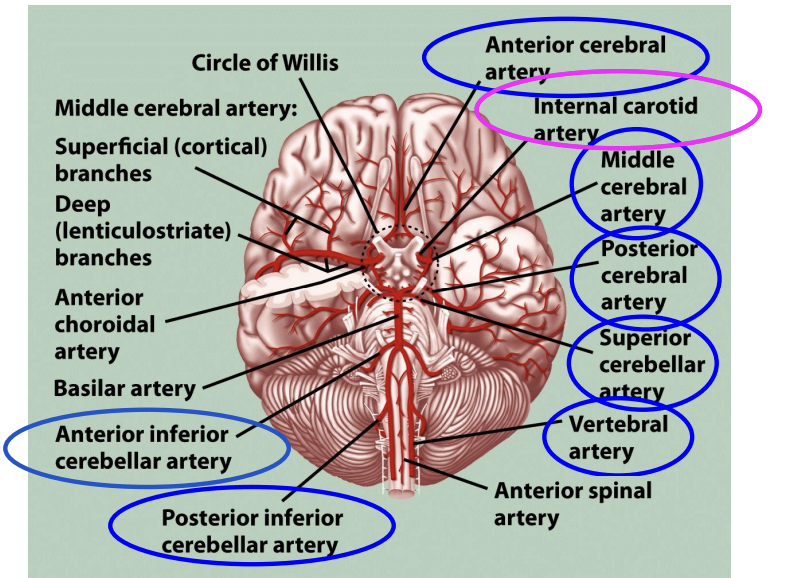
Circle of Willis provides blood supply to 3 paired cerebral arteries:
● 2-Anterior cerebral arteries supply the upper and anterior regions of the frontal lobes and anterior corpus callosum. - Broca only if medial
● 2-Middle cerebral arteries fan-shaped distribution and supply most of lateral surfaces of the brain hemispheres, plus thalamus and basal ganglia. —> most affected in stroke based on location (temporal/parietal) LANGUAGE CENTERS AFFECTED
● 2-Posterior cerebral arteries supply blood to the occipital lobes and lower parts of the temporal lobes.
Damage to Blood Supply
Amount of brain tissue affected by occlusion of an artery depends on the location of the occlusion in the artery.
Occlusions in the trunk or main branch of the cerebral artery affect large regions of the brain.
Occlusions in peripheral branches affect smaller regions.
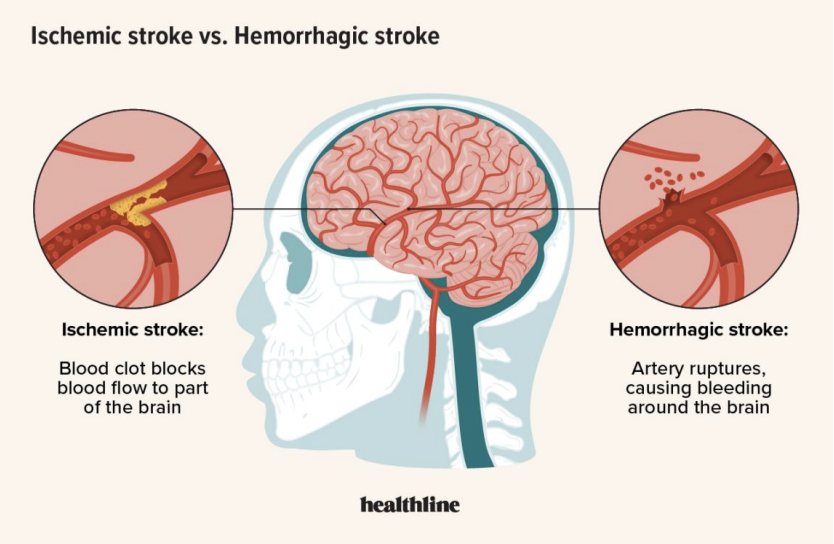
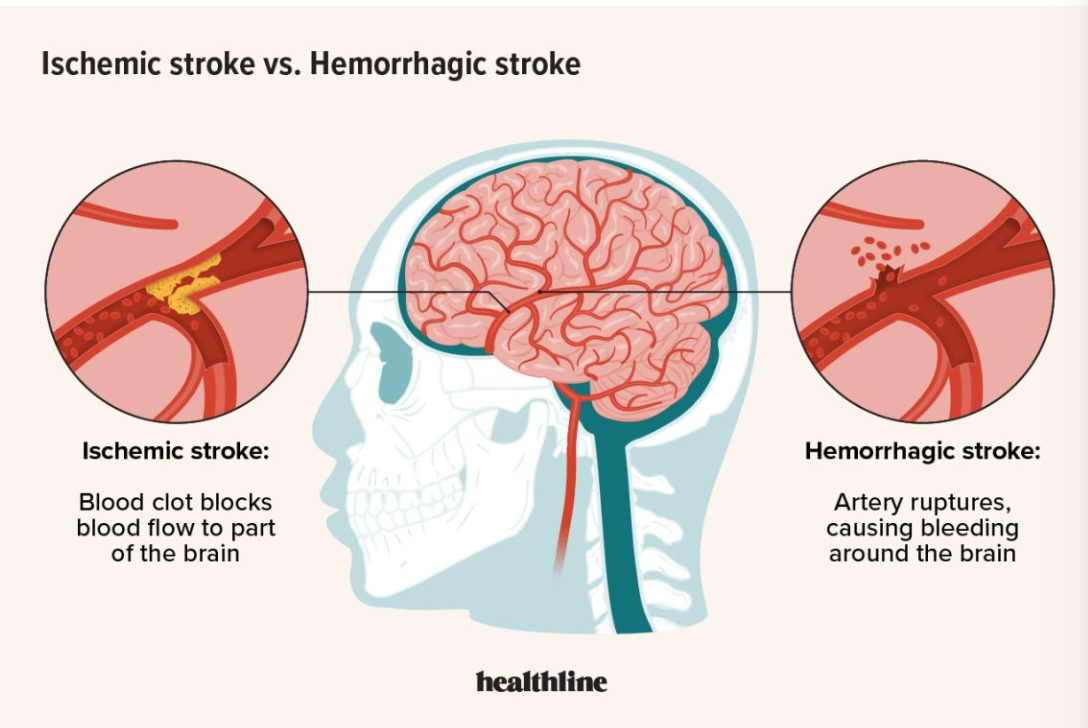
Stroke/CVA (blood supply to the brain) occluded or burst
● Brain damage caused by vascular disruptions such blockage of blood supply or bleeding.
Common Abrupt Symptoms: ▪weakness or numbness on one side of the body. ▪impairment of vision, especially in one eye.
▪difficulty speaking or understanding speech.
▪episodes of dizziness or falls. ▪severe headache, especially with any other symptoms
FAST —> one side
2 Types:
1. Ischemic (deprived of blood) blockage 80% —> circle of willis another way around it
2. Hemorrhagic (caused by rupture of artery) burst 20% —> more damage
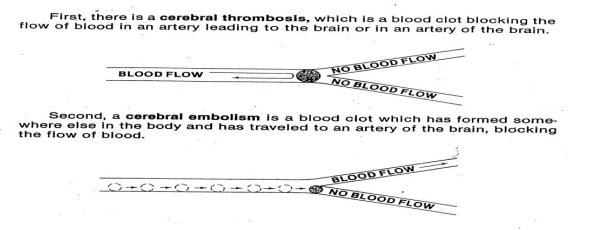
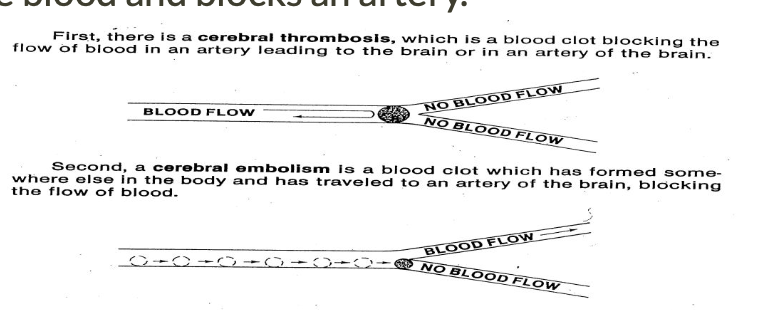
Ischemic Stroke
Occurs when an artery is blocked (occlusion) and part of the brain loses its blood supply
May be caused by:
1. Thrombosis: an artery is occluded by material accumulating at a fixed location
2. Embolus: an artery is abruptly occluded by material that moves through the blood and blocks an artery.
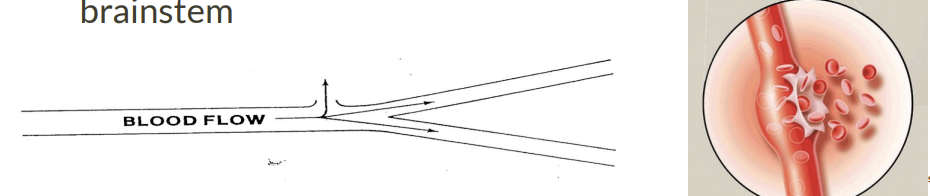
Hemorrhagic Stroke
▪ Caused by rupture or leakage of cerebral blood vessels.
▪ May be the result of weakness of a vessel wall or extreme fluctuations in blood pressure
1. Extracerebral hemorrhages-hemorrhages from blood vessels in the meninges or on the surface of the brain (bleeding outside brain).
2. Intracerebral hemorrhages-hemorrhages within brain or brainstem
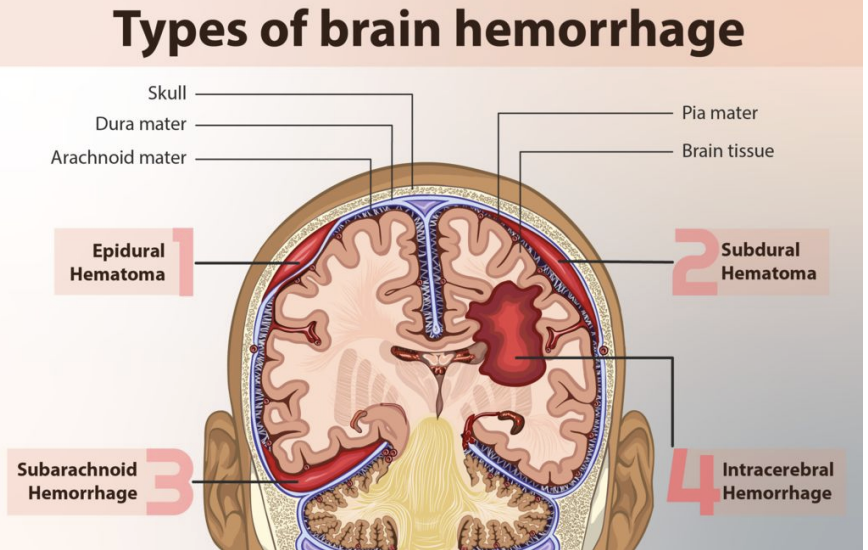
Types of brain hemorrhage
epidural hematoma
subdural hematoma
subarachnoid hemorrhage
intracebral hemorrhage
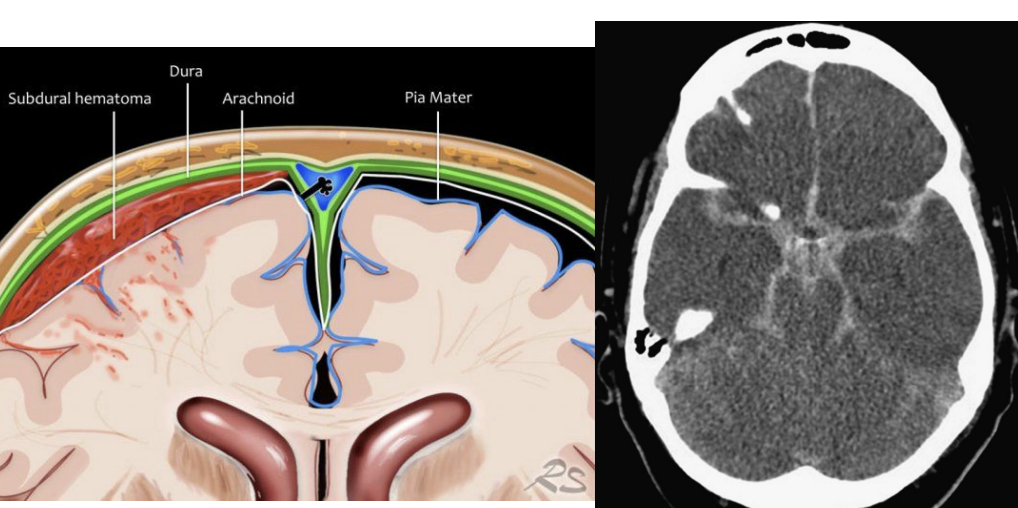
Extracerebral Hemorrhages
3 types depending on WHERE blood accumulates:
1. Subarachnoid hemorrhage-bleeding between arachnoid and pia. —> closest to the brain/blood supply
2. Subdural hemorrhage-bleeding beneath dura.
3. Epidural hemorrhage-bleeding between dura and skull.
● TBI usual cause of subdural and epidural hemorrhages
● After bleeding stops, left with a hematoma/bruise (subarachnoid, subdural, or epidural)--accumulation of clotted or partially clotted blood in the space created by the hemorrhage.
hematoma causing pressure on the brain temporary
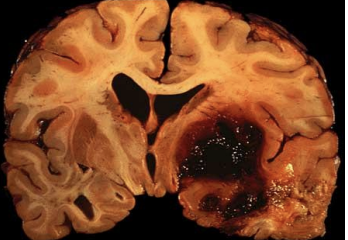
Intracerebral Hemorrhage
Hemorrhage into the brain and brainstem (bleeding in brain tissues).
Most common sites are the thalamus and basal ganglia
Also possible: Brainstem (especially pons) and cerebellum
May be caused by aneurysm: pouch formed in weakened arterial walls
If aneurysm in cerebral artery bursts, severe aphasia is likely (big accumulation big burst)
high blood pressure (walls give out)
if super deep hard to evacuate the bleeding
Location of Stroke
● Directly determines areas affected
● Anterior Cerebral Artery Stroke:
○ Supplies Frontal lobe
○ Confusion, coordination, sensory function, personality, contralateral paralysis/paresis
● Middle Cerebral Artery Stroke:
○ Supplies Temporal lobe, anterolateral frontal lobe, parietal lobe
○ Aphasia, motor speech, visual field deficits, contralateral paralysis/paresis
● Posterior Cerebral Artery Stroke:
○ Supplies Occipital Lobe, inferior Temporal lobe
○ Visual field, vision, sensory impairment, agnosia, memory
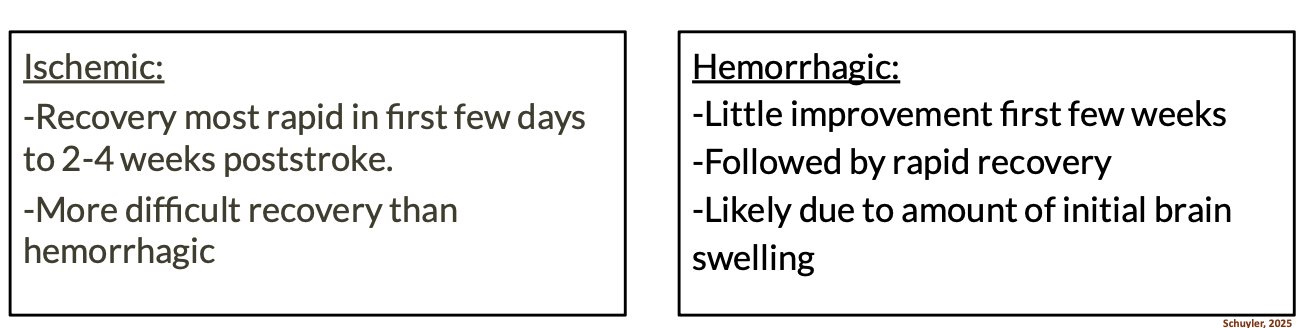
Stroke Recovery
Different rates of recovery
Recovery depends on:
1. Type of stroke
2. Severity (How much brain tissue destroyed)
3. Location of the destruction
Ischemic - blockage
recovery most rapid in first few days 2-4 weeks poststroke
more difficult recovery than hemorrhagic ( depending on how long the blockage occurred)
Destroys the WHITE matter (connections)
Hemorrhagic: treat most severe first (bleed NOT connections)
little improvement first few weeks (brain trying to recover reabsorb the blood, repair artery wall) (WAY LATER ON RECOVERY)
followed by rapid recovery
likely due to amount of initial brain swelling
moderate best recovery
mild —> not much to recover
FIRST FEW DAYS NOT RELIABLE!
![<p>Transient Ischemic Attacks TIA's [mini stroke] temporary </p>](https://knowt-user-attachments.s3.amazonaws.com/2e20dc6a-7835-41c6-b088-163eb586db85.png)
Transient Ischemic Attacks TIA's [mini stroke] temporary
Temporary disruptions of cerebral circulation accompanied by rapidly developing symptoms including:
sensory disturbance, limb weakness, slurred speech, visual anomalies, dizziness, confusion, mild aphasia, or other symptoms which resolve completely within 24 hours.
Interruptions of blood supply to the brain that last more than 24 hours but leave minor deficits after few days.
Typically, predecessor to a full blown stroke
embolus broken up into pieces
pressure on wall —> hemorrhagic
Other causes of neurological damage
● Traumatic brain injury
● Intracranial tumors
● Hydrocephalus [fluid on brain]
● Infections/toxins/substance abuse
● Nutritional and metabolic disorders
Language and Cerebral Dominance
most adults, regardless of handedness, depend on the left hemisphere for language
left hemisphere dominant for speech and language in 85-90% of adults
Cerebral plasticity or Neuroplasticity: brain’s ability to reassign to different brain regions functions that are lost when brain tissue is damaged
diminishes with age and other factors
neuroplasticity: brain rewiring neural connections to go around the damage - reestablish connection (age, neurodegenerative disease/disorder, # of strokes/brain injury, cognition level — education level, motivation level)
L side embolism in MCA LEFT & MCA
= ischemic, Aphasia, visuospatial awareness, reading/writing (vision)
Subarachnoid hemorrhage (fell onto head) frontal
b/w arachnoid & pia mater (extracerebral)
cognitive (memory, problem solving, personality, emotions)
if it was dura —> less severe not as close to the brain
clot of blot after = hematoma
patient falls backward off bike without a helmet with resulting subdural hemorrhage
reading/writing (vision/occipital)
cognition (see and process what we are doing) functional ADL
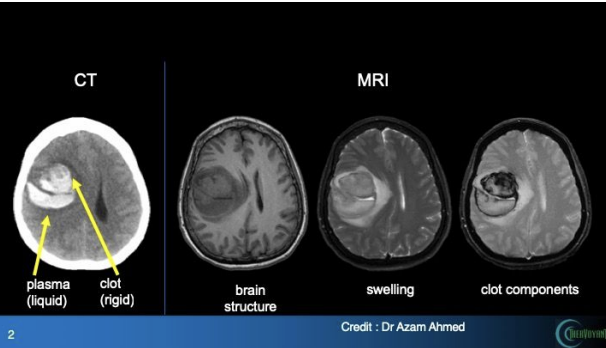
Imaging Procedures
● Identifies lesion site
● X-rays
● CT (first - least invasive) or CAT scans
● MRI–Magnetic Resonance Imaging
● Carotid ultrasound
● Cerebral angiography
● Doppler ultrasound
Full blown = CT/MRI
brain swells post injury
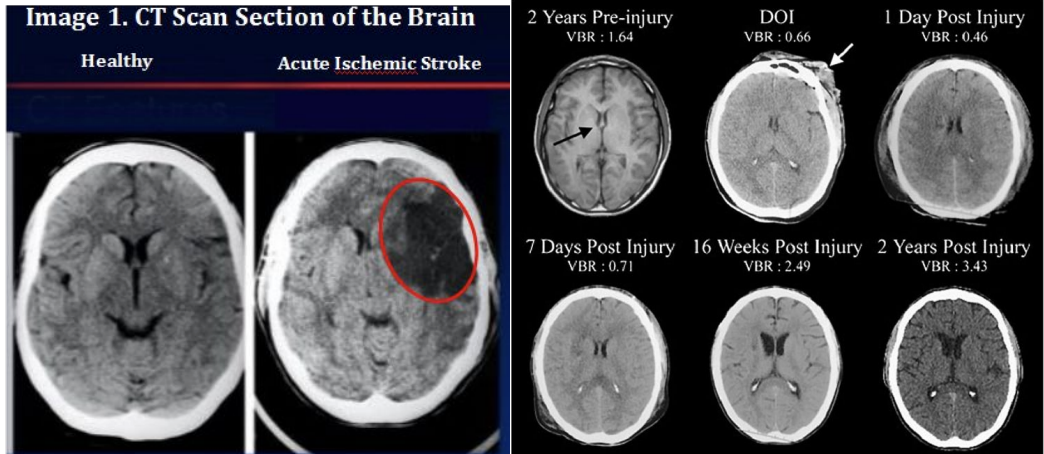
Brain Atrophy
stroke —> dementia type symptoms bc of more grey matter - atrophy
grey and white matter disintegrating (lang. cognition, memory body voluntary functions impaired)
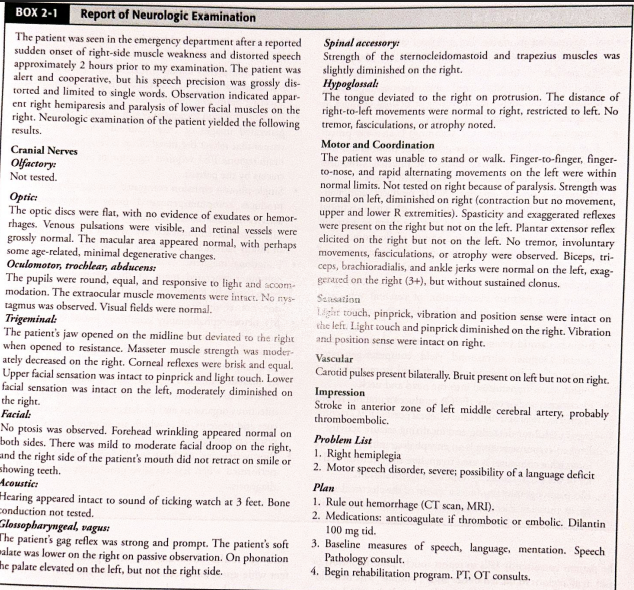
Vastly oversimplified but concise overview of major stroke syndromes
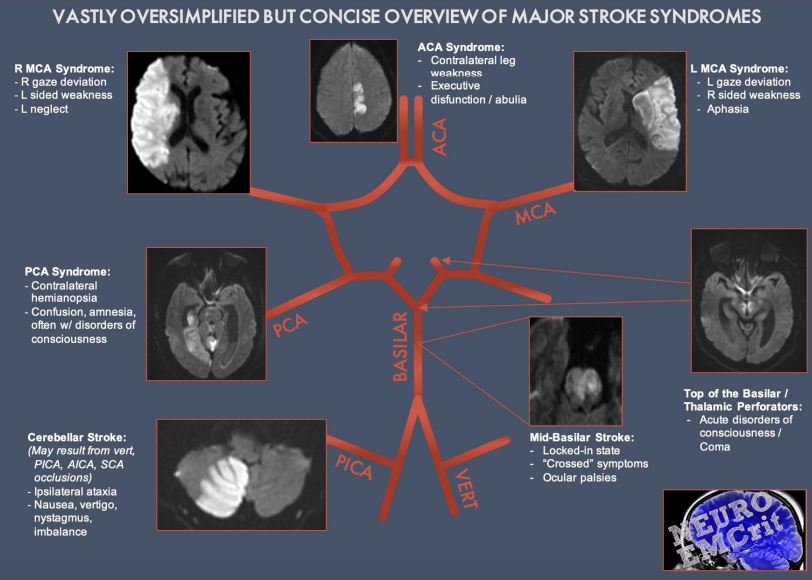
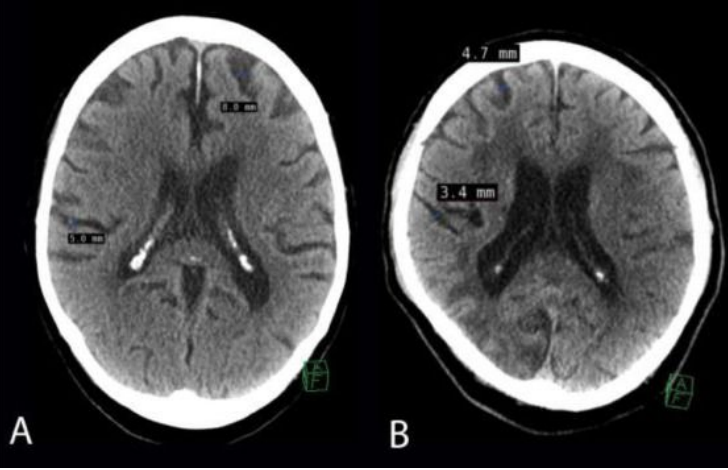
Neurologist Assessment includes
● Patient and family interview
● Symptoms (initial and over time)
● Evaluation of motor systems:
○ Assess movement, reflexes, muscle tone, ROM, strength, voluntary movement
○ Nystagmus
● Evaluation of sensory systems
○ Body sensation
○ ℅ pain, numbness, or abnormal sensations
● Evaluation of mental status ● Cranial nerve assessment
Mental Status Exam
Provides information on:
● Level of consciousness
● Attention and concentration
● Orientation
● Memory
● Mood and behavior
● Thought, content, language and speech
Screeners
● Mini Mental Status Examination (MMSE) ● Modified Mini Mental Status Examination (3MS) ● Cognitive Abilities Screening Instrument (CASI) ● Brief Cognitive Rating Scale (BCRS) ● Brief Interview of Mental Status (BIMS) ● Montreal Cognitive Assessment (MoCA) ● Mini-Cog ● St Louis University Mental Status Exam (SLUMS) ● Cognitive Assessment Screening Test (CAST)
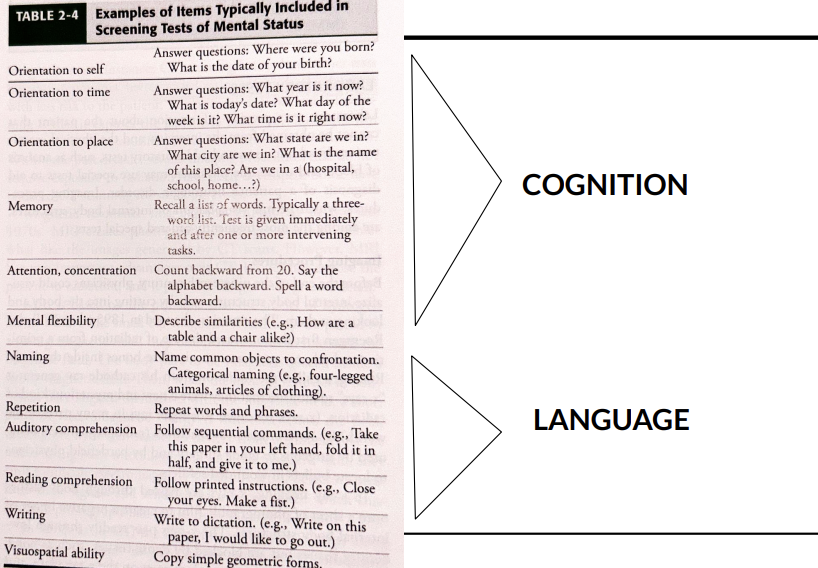
Cognition
orientation to
self
time
place
memory
attention, concentration
mental flexibility
language (exp/receptive)
naming
repetition
auditory comprehension
reading comprehension
writing
visuospatial ability
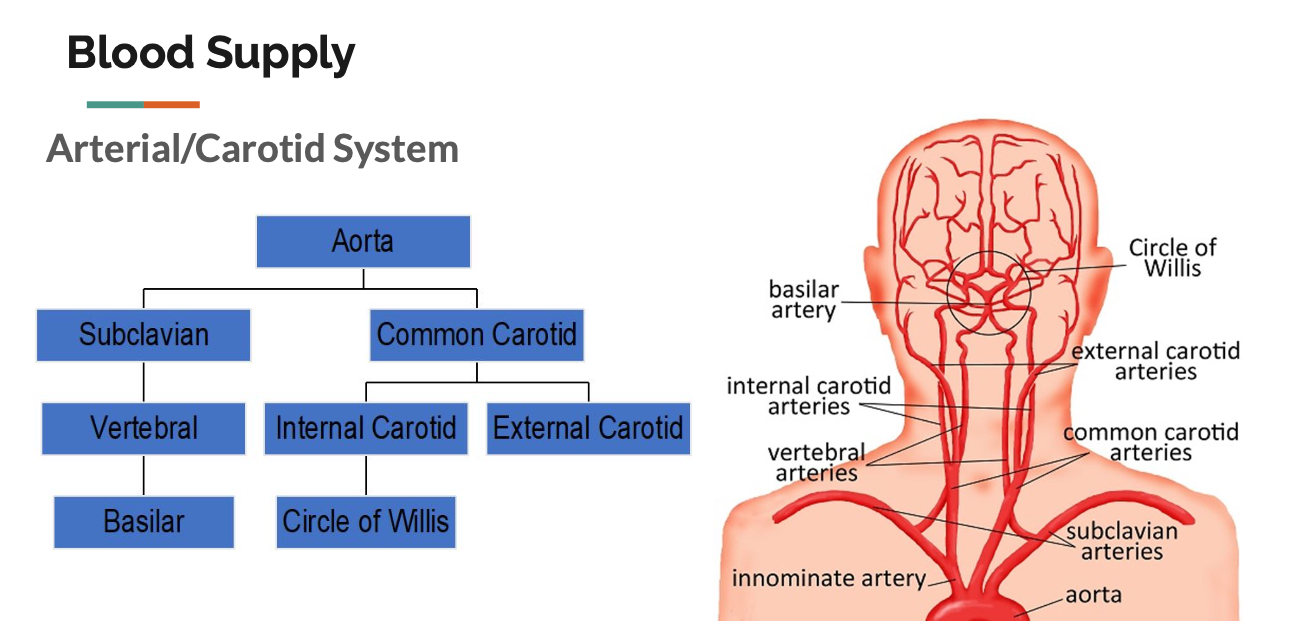
Blood Supply in the Brain
⚫ At any given time about 25% of the blood in
the body is in the brain.
⚫ Mechanical process of getting blood to the
brain begins at the heart, where pumping
pressure pushes blood through the arteries.
⚫ Heart pumps oxygenated blood into the
aorta, major artery from the heart.
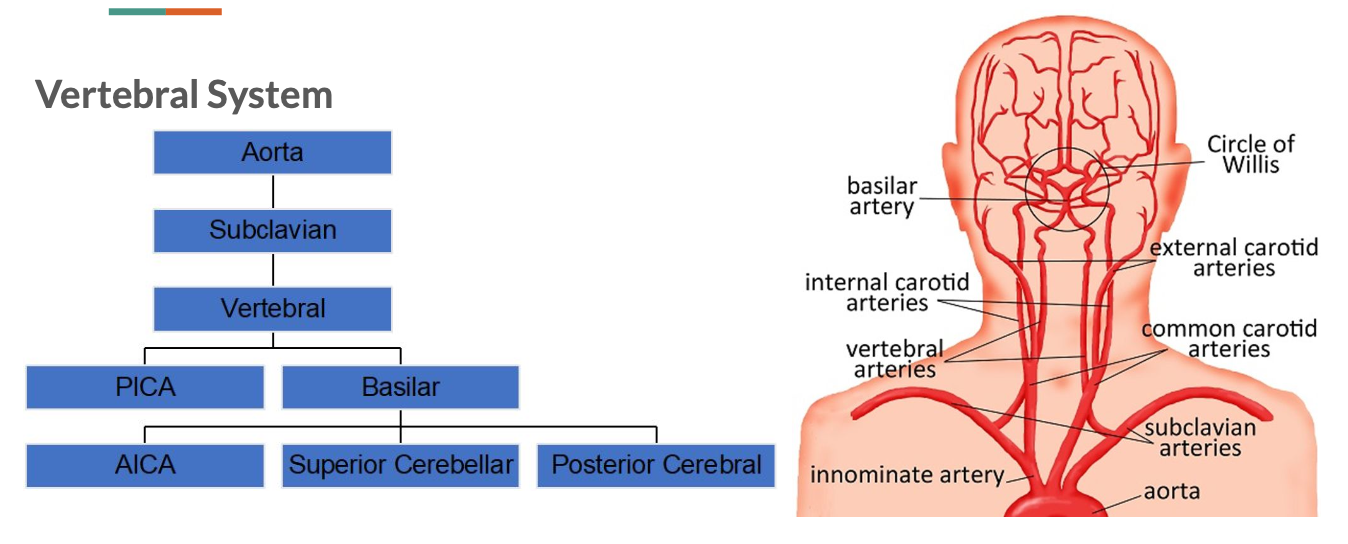
Cerebral Arteries
Circle of Willis provides blood supply to 3
paired cerebral arteries:
● 2-Anterior cerebral arteries supply
the upper and anterior regions of
the frontal lobes and anterior
corpus callosum.
● 2-Middle cerebral arteries
fan-shaped distribution and supply
most of lateral surfaces of the brain
hemispheres, plus thalamus and
basal ganglia.
● 2-Posterior cerebral arteries supply
blood to the occipital lobes and
lower parts of the temporal lobes.
Arteries Label
Damage to blood supply
⚫ Amount of brain tissue affected by
occlusion of an artery depends on
the location of the occlusion in the
artery.
⚫ Occlusions in the trunk or main
branch of the cerebral artery affect
large regions of the brain.
⚫ Occlusions in peripheral branches
affect smaller regions.
Stroke CVA
● Brain damage caused by vascular disruptions such blockage of blood
supply or bleeding.
Common Abrupt Symptoms:
▪weakness or numbness on one side of the body.
▪impairment of vision, especially in one eye.
▪difficulty speaking or understanding speech.
▪episodes of dizziness or falls.
▪severe headache, especially with any other symptoms
2 Types:
1. Ischemic (deprived of blood)
2. Hemorrhagic (caused by rupture of artery)
Ischemic Stroke
Occurs when an artery is blocked (occlusion) and part of the brain
loses its blood supply
May be caused by:
1. Thrombosis: an artery is occluded by material accumulating at a
fixed location
2. Embolus: an artery is abruptly occluded by material that moves
through the blood and blocks an artery.
Hemorrhagic Stroke
▪ Caused by rupture or leakage of cerebral blood vessels.
▪ May be the result of weakness of a vessel wall or extreme
fluctuations in blood pressure
1. Extracerebral hemorrhages-hemorrhages from blood
vessels in the meninges or on the surface of the brain
(bleeding outside brain).
2. Intracerebral hemorrhages-hemorrhages within brain or
brainstem
Types of Brain Hemorrhage
epidural hematoma
subdural hematoma
subarachnoid hemorrhage
intracerebral hemorrhage
Extracerebral Hemorrhages
3 types depending on WHERE
blood accumulates:
1. Subarachnoid hemorrhage-bleeding between arachnoid
and pia.
2. Subdural hemorrhage-bleeding beneath dura.
3. Epidural hemorrhage-bleeding between dura and skull.
● TBI usual cause of subdural and epidural hemorrhages
● After bleeding stops, left with a hematoma
(subarachnoid, subdural, or epidural)--accumulation of
clotted or partially clotted blood in the space created
by the hemorrhage
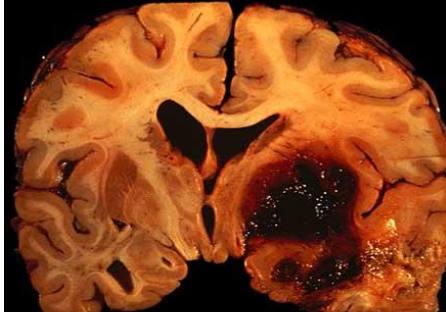
Intracerebral Hemorrhage
Intracerebral Hemorrhage
Hemorrhage into the brain and
brainstem (bleeding in brain tissues).
Most common sites are the
thalamus and basal ganglia
Also possible: Brainstem (especially pons) and cerebellum
May be caused by aneurysm: pouch formed in weakened
arterial walls
If aneurysm in cerebral artery bursts, severe aphasia is likely
Location of Stroke
● Directly determines areas affected
● Anterior Cerebral Artery Stroke:
○ Supplies Frontal lobe
○ Confusion, coordination, sensory function, personality, contralateral
paralysis/paresis
● Middle Cerebral Artery Stroke:
○ Supplies Temporal lobe, anterolateral frontal lobe, parietal lobe
○ Aphasia, motor speech, visual field deficits, contralateral
paralysis/paresis
● Posterior Cerebral Artery Stroke:
○ Supplies Occipital Lobe, inferior Temporal lobe
○ Visual field, vision, sensory impairment, agnosia, memory
Stroke Recovery
⚫ Different rates of recovery
⚫ Recovery depends on:
1. Type of stroke
2. Severity (How much brain tissue destroyed)
3. Location of the destruction
Transient Ischemic Attacks
⚫ Temporary disruptions of cerebral circulation
accompanied by rapidly developing symptoms
including:
sensory disturbance, limb weakness, slurred
speech, visual anomalies, dizziness,
confusion, mild aphasia, or other symptoms
which resolve completely within 24 hours.
⚫ Interruptions of blood supply to the brain that
last more than 24 hours but leave minor deficits
after few days.
⚫ Typically, predecessor to a full blown stroke
Acute care [hospitals]
typically a short period of time
Focused on evaluating, informing and monitoring in preparation for next level of care
Frequency: everyday, short period of time
Rehabilitation
focused on recovery of patient function in more intensive setting (intensive therapy)
treatment is the focus
ex) wing in the hospital, rehab center SNF
Frequency: every day or twice a day, longer periods of time
Home Care
referral —> assessment —> submit POC —> TX —> discharge & carryover
family/caregiver training is focus
QOL and least cost
Frequency: once a week at MOST
Outpatient (once a month)
time to achieve goals is typically more limited than other settings
focus on carryover and maintenance of skills achieved during tx
private practice (hospital)
INSURANCE - goals/progress/data
Frequency: once a week/month
Long-Term care (SNF)
typically involves frequent reassessment due to patient changing over time
focus on maximizing function, interdisciplinary care
Frequency: depends on needs, insurance 3-5 times a week
Cognition
attention/concentration
memory
orientation (where we are, who you are, time, why)
mental flexibility
executive function (reasoning & problem solving)
safety/judgement
visuospatial skills
Communication
expressive/receptive lang
reading
writing
speech intelligibility
pragmatics
NEEDS TO BE A DEFICIT FOR SLP TX
Cognitive-Communicative impairments
infinite number of signs, symptoms and syndromes associated with neurogenic cognitive-communicative impairments
Challenge for clinician = organize, refine, interpret and draw conclusions from confusing and sometimes contradictory information to diagnose and deveop plan of care for your patient
behavioral, cognitive, and emotional consequences of brain injury may affect how patient responds to different situations [frontal lobe]
Assessment of Cognitive-Communicative disorders
use of clinical knowledge
use clinical training
use experiences
be familiar with signs and symptoms of many cognitive communicative disorders
flexibility is key
Purpose of Assessment
determine if language disorder and classify symptoms
determine level of severity (change frequency of therapy, prognosis, discharge planning, insurance reimbursement)
determine which skills/strategies are used to communicate successfully
develop treatment plan
provide functional prognosis
establish baseline to measure progress from (skilled service, provide progress to patient)
educate patient and family about language skills and communication strategies and counsel about therapy expectations and outcomes
Collecting case history
DX and date of onset & chief complaint (relate to speech)
past medical history PMH [high blood pressure, past neurological injuries, age]
past surgical history
family history [dementia, alzheimer]
psychosocial history [drug, alcohol, smoke, depression]
work and educational history [stay at home, or super social] [baseline diff with schooling]
current medications
prior communication level [wanna know baseline]
current communication difficulties
Interviewing the patient
provides the first direct look at patient’s
cognitive-communication abilities
physical condition
orientation
attention
visual
hearing acuity
alertness (awake/asleep)
mood
other characteristics that may impact assessment
during interview clinician may support, inform, counsel, and educate the patient and family regarding the nature of the patient’s communicative impairments
Interviewing the patient
1) do your hw before the interview
2) conduct the interview in a quiet place free of distractions
3) tell patient who you are and your role in the case
4) make them comfortable
5) get the patient’s story
6) be a patient, concerned, and understanding listener
7) treat the patient as an adult who merits respect
8) Prepare the patient for what comes next
9) reassure the patient
10) include family members or significant others in the interview
Testing adults with brain injuries
do your homework
choose appropriate place for testing
schedule testing to maximize patient’s performance
collaborative effort testing patient
select appropriate test for patient [language vs. cognition]
let the patient’s performance guide what and how you test
use standardized tests and procedures purposefully
consider validity of standardized tests
consider adequacy of norms of standardized tests
evaluative normative sample
obtain a large enough sample of patient’s behavior to ensure test-retest stability
Standardized testing
stroke is always evolving, NOT GOOD FOR ACUTE setting
Setting: outpatient, rehab, home care, long term skilled nursing setting (10 years)
could do over multiple sessions (subtests too)
Purposes of testing
determining nature and severity of cognitive-communication impairment usually has implication for the diagnosis, the prognosis, and decisions about treatment
Diagnosis: attaching a label to the cognitive-communication disorder
differential diagnosis
arrive at a more specific diagnosis
often suggests the location of brain injury based on symptoms (wernickes aphasia)
SLP responsibility
diagnose cognitive/communication disorder
determine the nature and severity of the patient’s impairment
form a tx plan
ICD 10
I 69 = CVA
R41.84 = TBI
R48.8= epilepsy, brain cancer, autism, ND disease
F80 ONLY LANG no medical
Prognosis
prediction about the course and the eventual outcome of a disease or condition
more objective probability statement based on clinical experience and intuition based on studies of individuals who have had the disease or condition (prospective or retrospective prognostic studies)
Prognostic Variables for Recovery
Neurologic findings
DX
location and extent of the damage
presence and duration of coma (without brain activity dec. prognosis)
Associated conditions
medical conditions or physical findings
general health
associated sensory and motor impairments
Patient Characteristics
age, gender education, occuptation, premorbid intelligence, handedness, personality, emotional state
overall severity of patient’s cognitive communicative impairment
Measuring recovery and response to tx
measuring patient’s performance over time
define baseline measures (tests)
measure responses to tx (formal/informal assessment)
change tx procedures as needed based on response
Efficacy
existence of measurable change as a result of tx (research or clinical practice)
- treatment that is efficacious does not necessarily mean it is effective
standardized assessment
Effectiveness
effects of tx on a patient’s daily life and well being
typically measured by subjective reports of patient and family or by observation
self-report (REAL WORLD)
Functional communication
functional = affecting patient’s daily life competence or well being
Ex) ordering at a restaurant (scripting), remembering what day it is/ what time appointments are, object naming relevant, functional conversations - give them a quote, recognizing family members
Standardized Assessments Cognitive linguistic (Occipital right hemisphere!)
Global deterioration sccale (GDS)
Cognitive linguistic test plus (CLQT+)
Scales of Cognitive Ability for TBI (SCATBI)
Standardized tests Language (LEFT FRONTAL TEMPORAL)
Western Aphasia Battery (WAB)
Kentucky Aphasia test
Boston diagnostic aphasia examination BDAE-3
Informal assessment
conversation
auditory comprehension
behavior
general appearance: gait, posture, symmetry, involuntary movements, CN function
Communication modality (verbal, gesture)
interest and motivation
family/caregiver comments
visuospatioal (look where they are looking)
Informal assessment
impairment: identify cognitive-communication deficits, design an intervention program considering strengths, weaknesses and needs
activities: assess daily life cognitive-communicative strengths and weaknesses
participation: assess effects of impairments on person’s social psychological and emotional well being and QOL
Functional Tasks
express ideas, start conversations, discuss feelings
use the phone/internet to make appointments
understand the concepts
design and follow a schedule
manage finances, write checks and bank
shop, make purchases, use coupons
plan a menu, prepare meals
read/understand signs, symbols maps
follow written directions
engage in leisure activities
conduct work related tasks as needed
Examples of informal assessment
introduce yourself to the patient, names can be used to assess memory later
check reading by having the patient attempt to read get well cards to you and any signs in the room
check the relationship of the person who sent the cards by asking the patinet who that person is along with a description
ask the patient to complete a hospital menu and read what was selected
ask the patient to write a few words such as the names of family or friends for word retrieval and writing
ask him or her to name a few objects around the room, listening to speech and naming ability
have the patient attempt to follow commands and answer yes/no questions
track higher level comprehension by assessing the patient’s ability to engage in conversation with you
Setting goals
goals should be based on patient’s needs and preferences while also considering level of impairment and functional abilities
promote function
promote effective communication
provide compensatory strategies
reduce interfering behaviors
provide education and counseling for patient and family
provide relevant home program to patient and family (if applicable) (outpatient) (home care), depending rehab