Neuroanatomy & Psychiatric Disorders - prereading
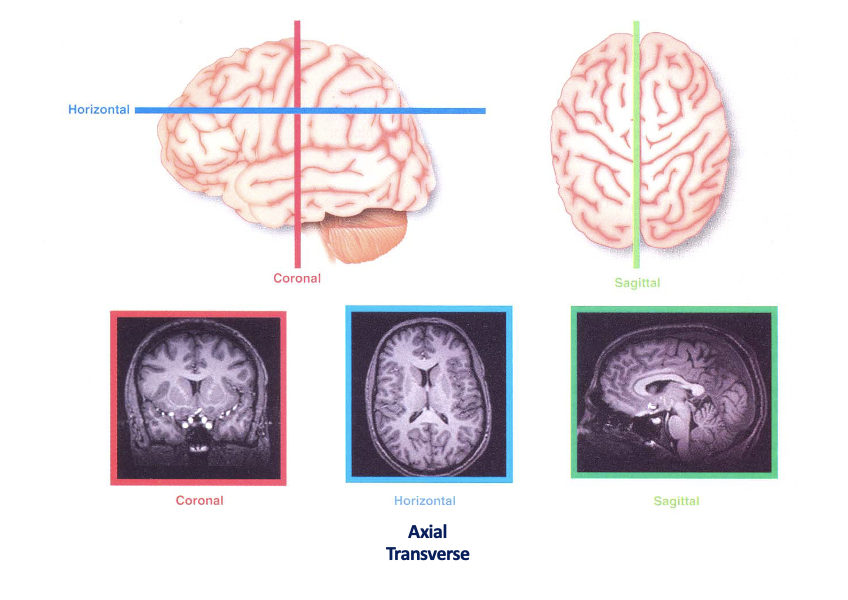
<<Planes of the brain<<
- White matter": Mainly axons due to myelination (lipid/ fatty sheath)
- Grey matter: neuronal cell bodies
}}Main regions of the brian}}
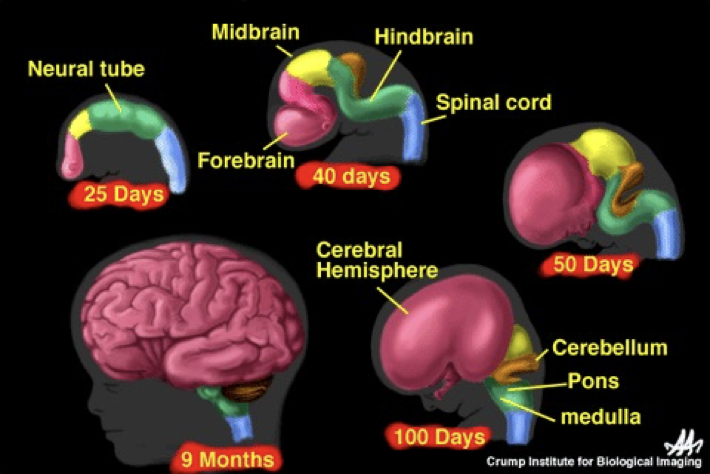
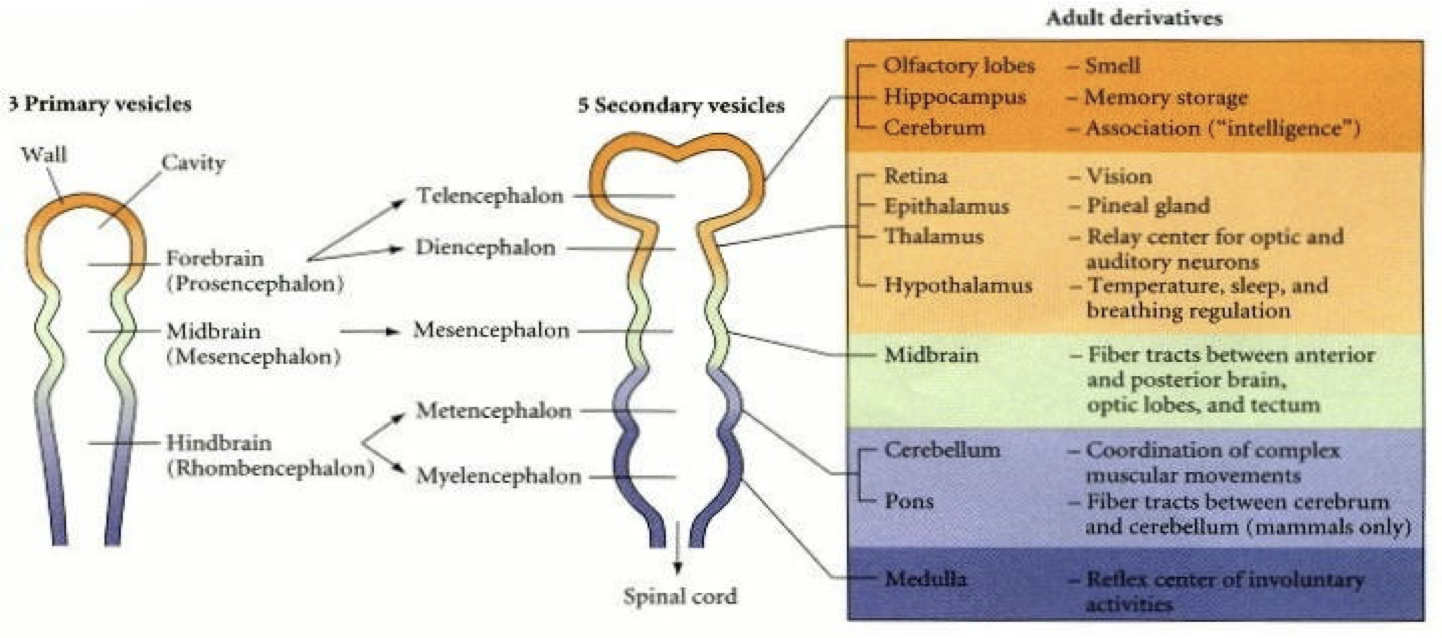
]]Embryology]]
Refer back to case 7 embryology on the formation of the spinal cord
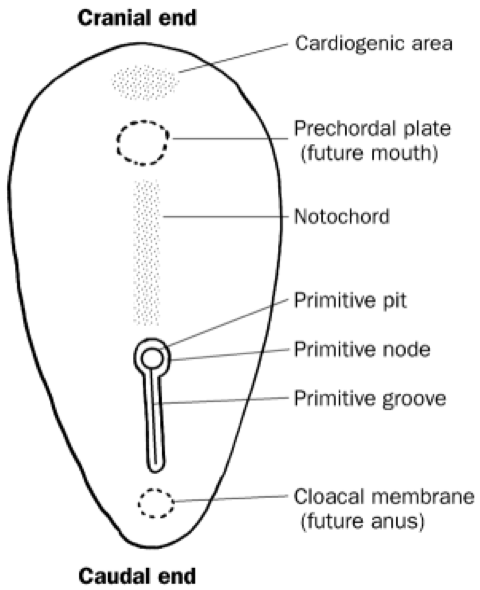
The neural tube then splits into the main parts of the brain
]]Rhombencephalon]]
- Brain stem
- Cranial nerves + normal nerves run from the medulla
- The cerebellum + pons are important in co-ordinating movements + responding to external stimuli
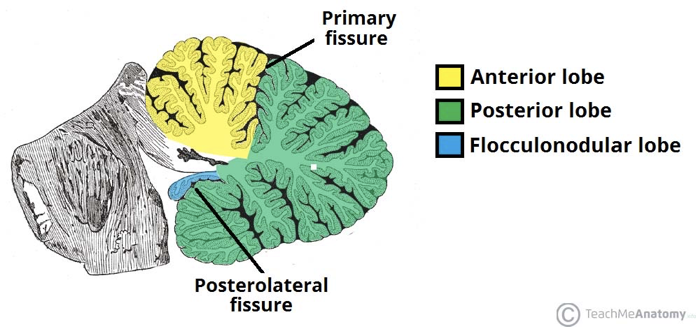
{{Cerebellum - divided i nto 3 lobes:{{
Flocculonodular lobe
- Vestibulocerebellum/ archicerebellum
- Regulates balance + co-ordination (oldest)
Posterior lobe
Anterior lobe
Contains Purkinjie + granule cells
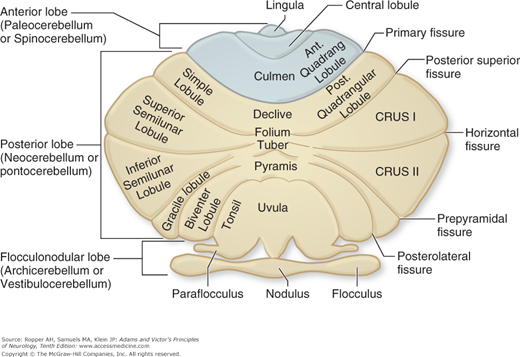
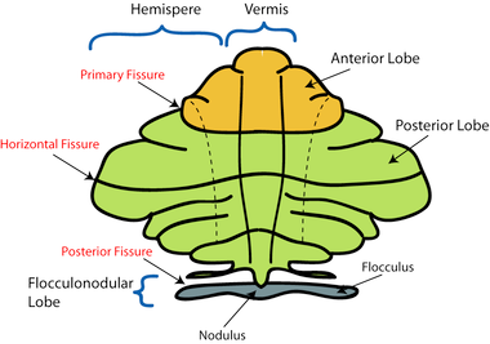
- Areas closest to the vermis- spinocerebellum/ paleocerebellum
- Spinocerebellum: regulates body temperature + limb movement
- Laterally- neocerebellum
- Neocerebellum:
regulates planning,
sensory movement for action
]]Cerebellar Disorders]]
Damage of the neocerebellum causes ataxic gait e.g. stroke or alcohol-related
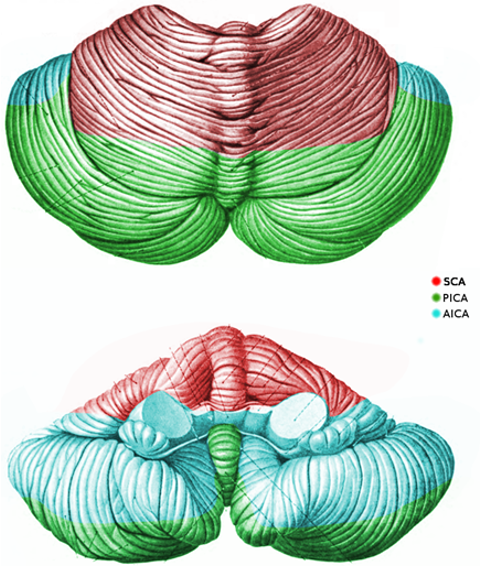
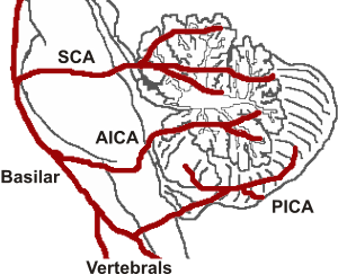
Cerebellum has a complex arterial supply
Therefore, it is important in cases of stroke or vertebral/ basilar artery dissection (present with cerebellar signs
]]Pontine disorders]]
- locked-in syndrome
- Central pontine myelinolysis
- Progressive Supranuclear Palsy (Steele-Richardson-Olszewski):
- Supranuclear ophthalmoplegia
- Neck dystonia
- Parkinsonism
- Pseudobulbar palsy
- Behavioural impairment
- Imbalance
- Frequently falls
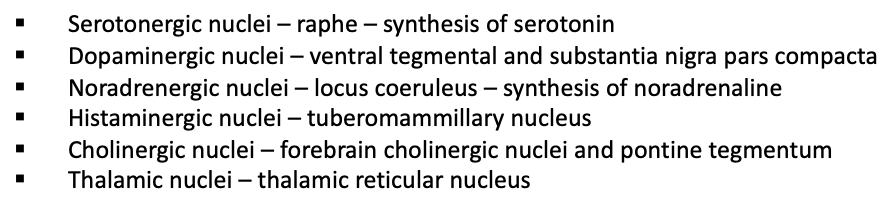
]]Reticular formation]]
Allows for communication of the brain to the rest of the body
A hub for the synthesis of neurotransmitters and wake/sleep state
Ascending/ descending through the brainstem
Includes ascending reticular activating system- role in arousal
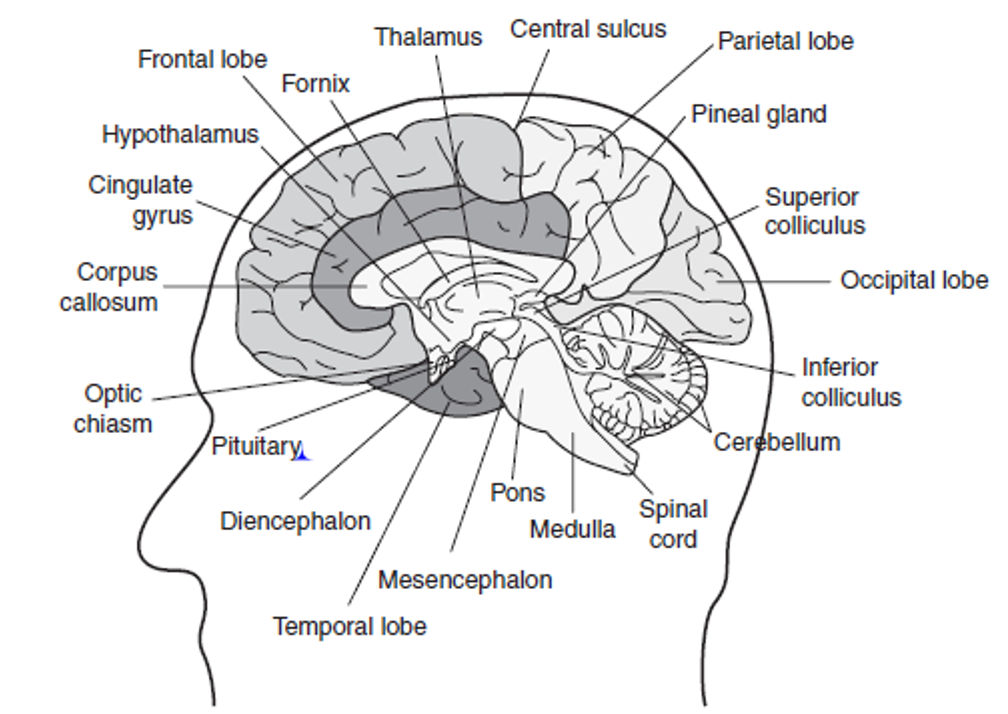
<<Mesencephalon<<
- Midbrain
- Acts as a connector between different parts of the brain
- links everything together
- Don’t worry too much about the next info
Parts of the midbrain
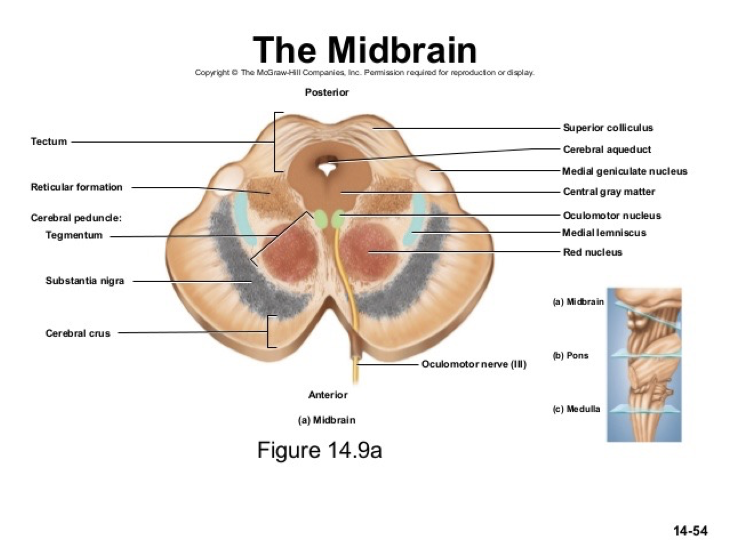
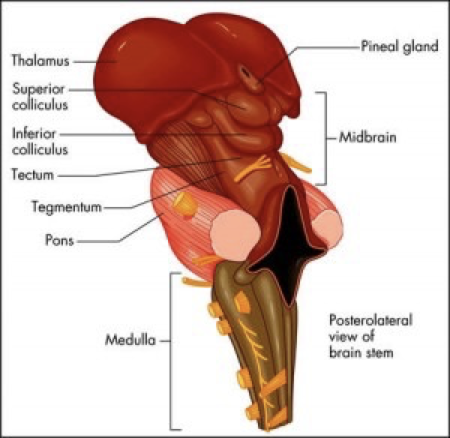
Tectum (dorsal part) splits into:
Superior colliculus- visual processing + eye movement control
Inferior colliculus- auditory processing
]]Disorders of the mesencephalon]]
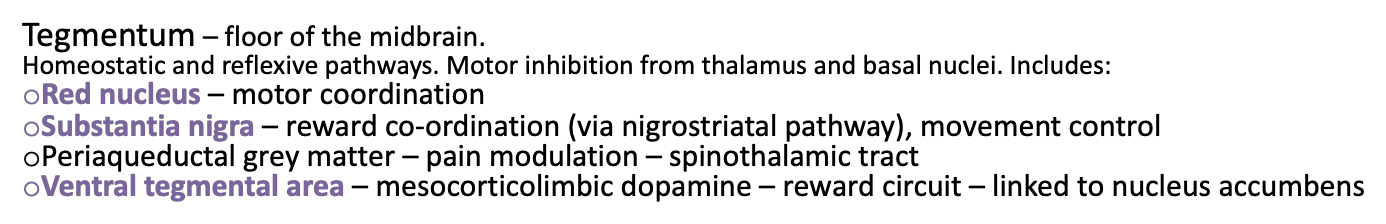
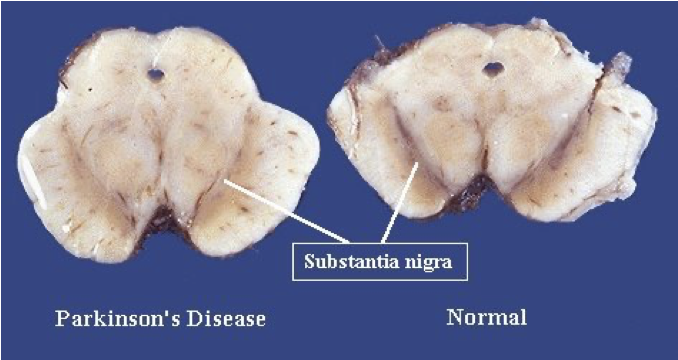
- Parkinson’s - reduction in dopaminergic neurones in substantia nigra
- Schizophrenia- increased dopamine in substantia nigra
- Multi-system atrophy- degeneration of striatum and substantia nigra
- Ventral tegmental area- primary sites of addictive drugs (heroin, cocaine, alcohol, nicotine)
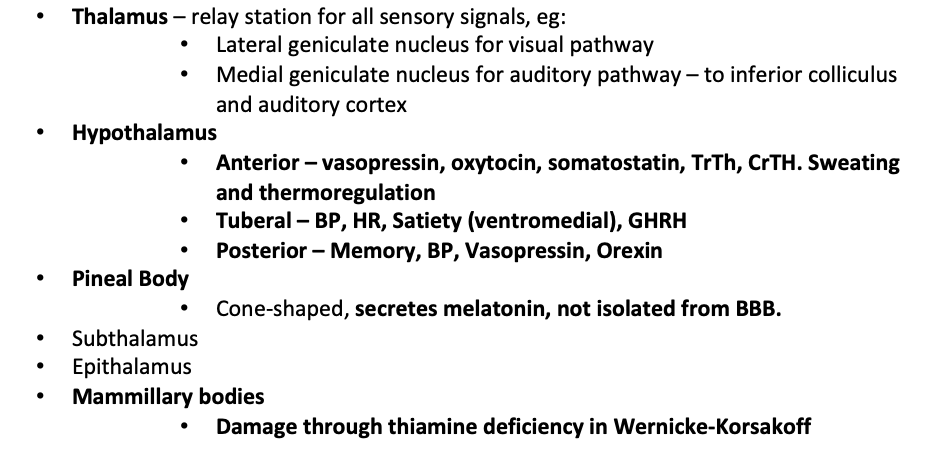
]]Diencephalon]]
Contains:
Thalamus
Hypothalamus
Pineal Body
Subthalamus
Epithalamus
Mammillary bodies
Limbic system:
- Connects cortical control to memory / sensory/ secretory areas
- Involved in motivation, visceral processes + rewards
- Systems of emotions
- Connects a group of structures surrounding the brainstem (cingulate gyrus, hippocampus, hypothalamus + anterior thalamic nuclei)
- Connecting these structures enables cortical control of emotion + plays a role in storing memory
]]Telencephalon]]
- higher functions such as smell, memory + Intelligence
Hippocampus
- Medial temporal lobe
- Short-term memory to long term memory
- Spatial memory
- Includes dentate gyrus + granule cells - formation of new episodic memories, site of neurogenesis, affected in depression
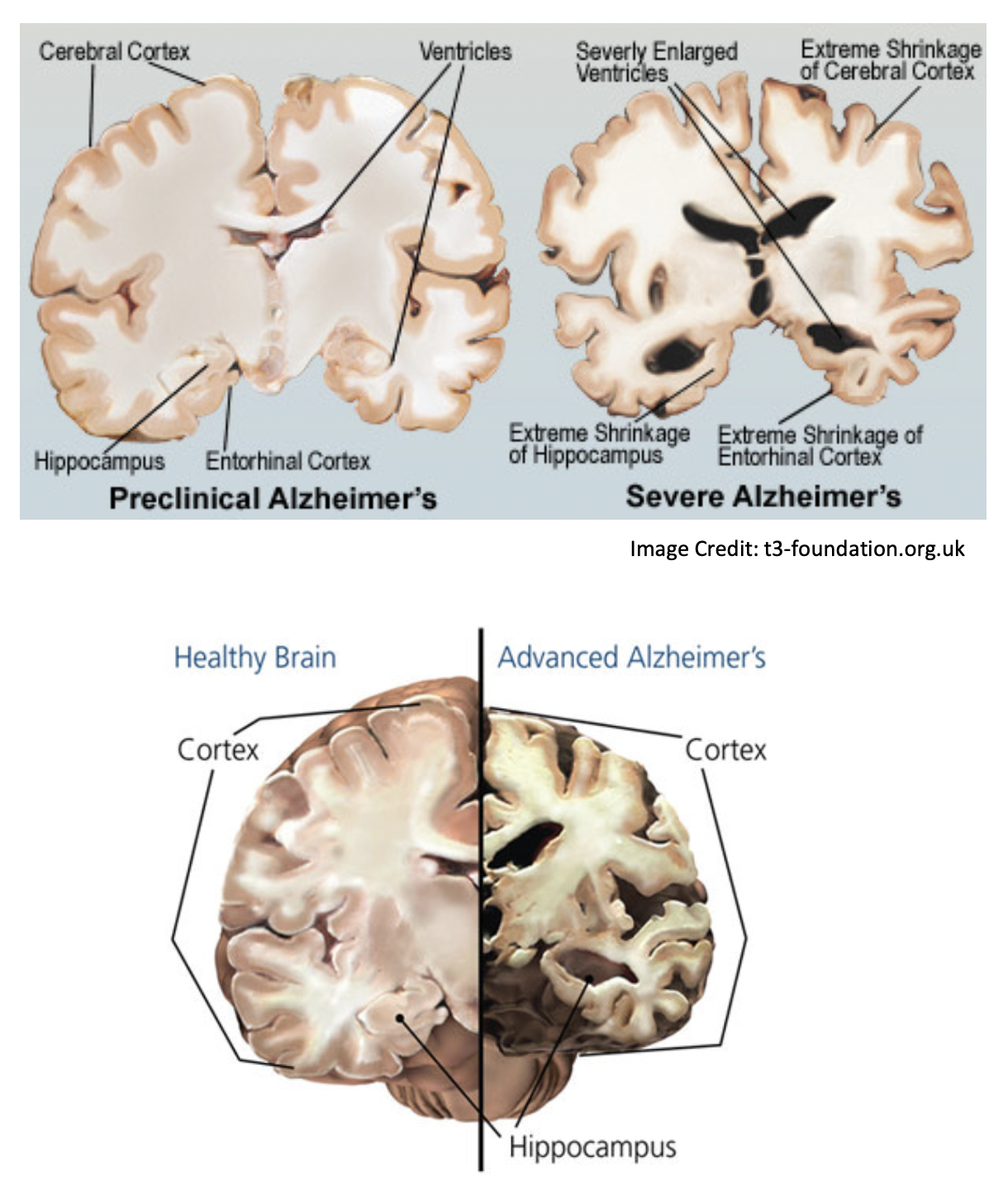
- Alzheimer’s + dementia → hippocampal atrophy → memory symptoms
Cortex
- Memory
- attention
- Cognition
- awareness
- thought
- language
- consciousness
- 4 lobes, gyrus (fold) + sulcus
Frontal lobe
- Superior frontal gyrus = self-awareness/ laughter
- Middle frontal gyrus
- Inferior frontal gyrus = language processing, Broca’s area
- Medial frontal gyrus = executive mechanism
- Paraolfactory area= limbic
- Orbitofrontal cortex= stimulus-reward, stimulus/outcome, addiction
- Ventromedial prefrontal cortex- decision making, emotion regulation, addiction
- frontotemporal dementia/ Pick’s disease = genetic + accumulation of tau + frontal symptoms
Prefrontal cortex
- Planning + executing actions
- One of the last to develop
- lesions:
- Dramatic changes in personality
- Loss of spontaneity/ problems with initiating speech/ movements
- inability to make + carry out sequences of actions/plans
Parietal lobe
Integrates sensory information
Dominant hemisphere lesions:
- Dysphasia, aphasia
- Dyscalculia- difficulty learning, doing calculations
- Dyslexia
- Apraxia- ability to execute or carry out skilled movements and gestures, despite having the desire and the physical ability to perform them.
- Agnosia- inability to recognize and identify objects or persons.
- Gerstmann syndrome- Dyscalculia, Dysphasia, finger agnosia, LR disorientation
Non- dominant hemisphere lesions:
- Spatial disorientation
- Constructional apraxia
- Dressing apraxia
- anosognosia- unaware of their own health problems
Temporal lobe
- Transeverse temporal gyri - Heschl’s gyri
- Superior temporal gyrus= auditory context with TTG. Pricess perception of sound + apply comprehension.
- Posterior STG = wernicke’s area
- Middle temporal gyrus
- Fusiform gyrus = FACIAL RECOGNITION, synaesthesia, dyslexia, prosopagnosia
- Inferior temporal gyrus= visual object recognition
Occipital lobe
- Lingual gyrus
- role in vision + dreaming
- Visuo-limbic integration
- encoding complex images
- word processing
- Cuneus - basic visual processing
- Calcarine sulcus/fissure
- primary visual cortex
- takes signals from geniculate nucleus via thalamus
Tracts- only for reference
Arcuate fasciculus- links Broca’s + Wernicks area
Uncinate fasciculus
- Links temporal inferior frontal gyrus + frontal lobe
- Hippocampus + amygdala with orbitofrontal cortex
- implicated in several psych conditions
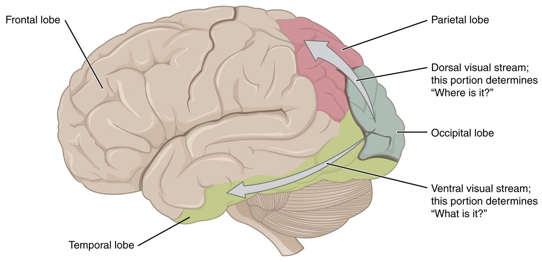
2 visual streams hypothesis:
- dorsal - where?
- ventral- what?
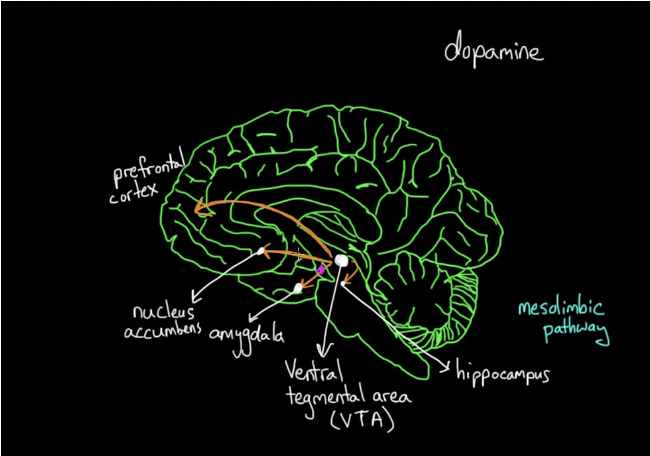
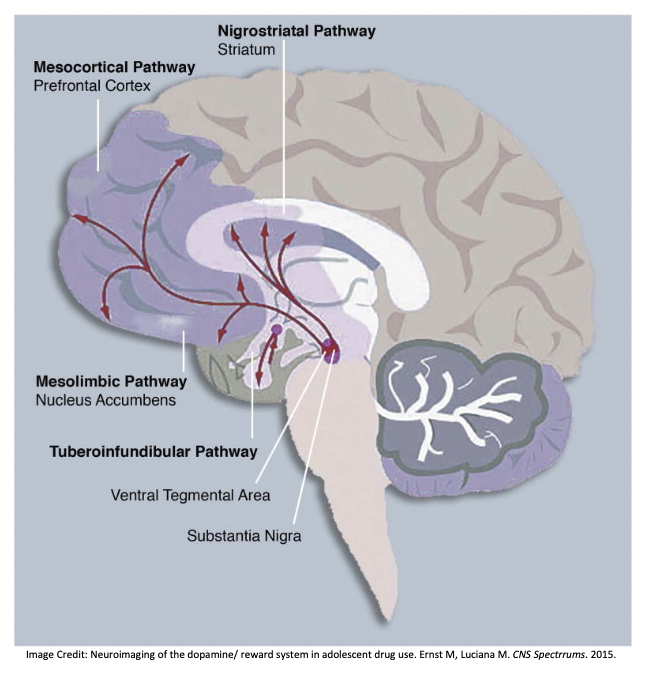
Central dopamine hypothesis
- Meso-cortical pathway
- Meso-limbic pathway
- Nigrostriatal pathway
- Affected in schizophrenia + other psych disorders
- Medications for scz work on this pathway
- Side effects of these meds are linked to these pathways (e.g. cog-wheel rigidity like that seen in parkinson’s/ galactorrhea due to pituitary stimulation)
]]Alzheimer’s Dementia]]
- Microscopic accumulations of peptide amyloid-β – plaques → cause loss of synapses, then neurons.
- Progressive degeneration
- Early changes in the hippocampus (first to be damaged)
Generalised shrinking and enlarged ventricles follow
- In severe depression, the dentate gyrus don’t light up in the scans which means they don’t form many memories.
]]Drug misuse]]
The reward system is based on dopamine.
It activates all dopamine pathways, particularly the mesolimbic pathway.
Dopamine is produced in the Vental Tegmental Area (VTA).
The mesolimbic pathway links this to the Nucleus Accumbens (motivation/ reward).
If we do something good, or use an addictive drug, this pathway is stimulated.
The mesocortical pathway is also activated.
This links to the Prefrontal Cortex (PFC).
This changes how you prioritise and plan.
]]Disorders]]
Case 1- depression after frontal tumour
56 year old female
Progressive apathy
Social withdrawal
Poor self-care for part 3 years
Admitted to a psychiatric facility for depression
unresponsive to antidepressants so CT was conducted
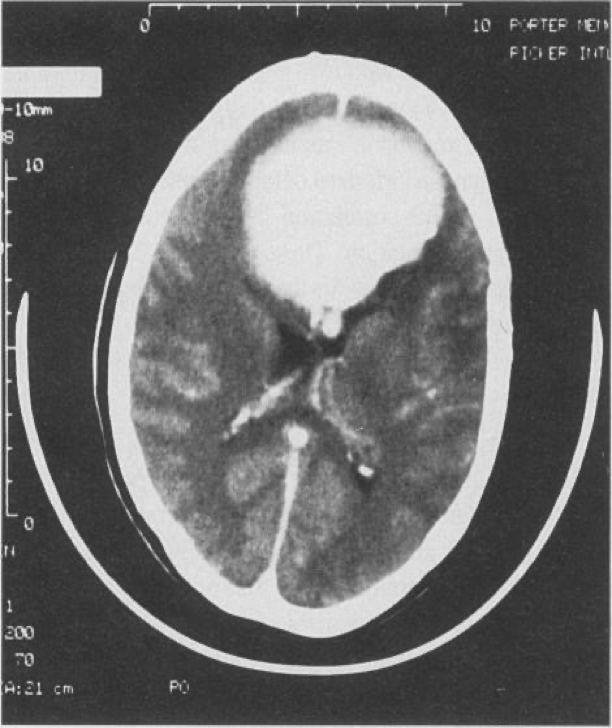
8cm medial bifrontal mass
Total excision benign transitional-type meningioma → rapid improvement
4 months after the operation was cheerful + motivated
Case 2- Psychosis after temporal tumour
18-year-old female
Referred form school to a psychosis clinic (high risk)
2 years of withdrawal from social activities + resent from work groups or talking in public
1 year later became concerned about unknown people stating + laughing at her for no reason
Feeling the world around her has changed
She is concerned that people are intimidating her + that there are special messages in TV for her
She is neurologically normal + an average IQ
Initial diagnosis: prodromal syndrome of schizophrenia but symptoms became more rapidly severe
Routine MRI conducted
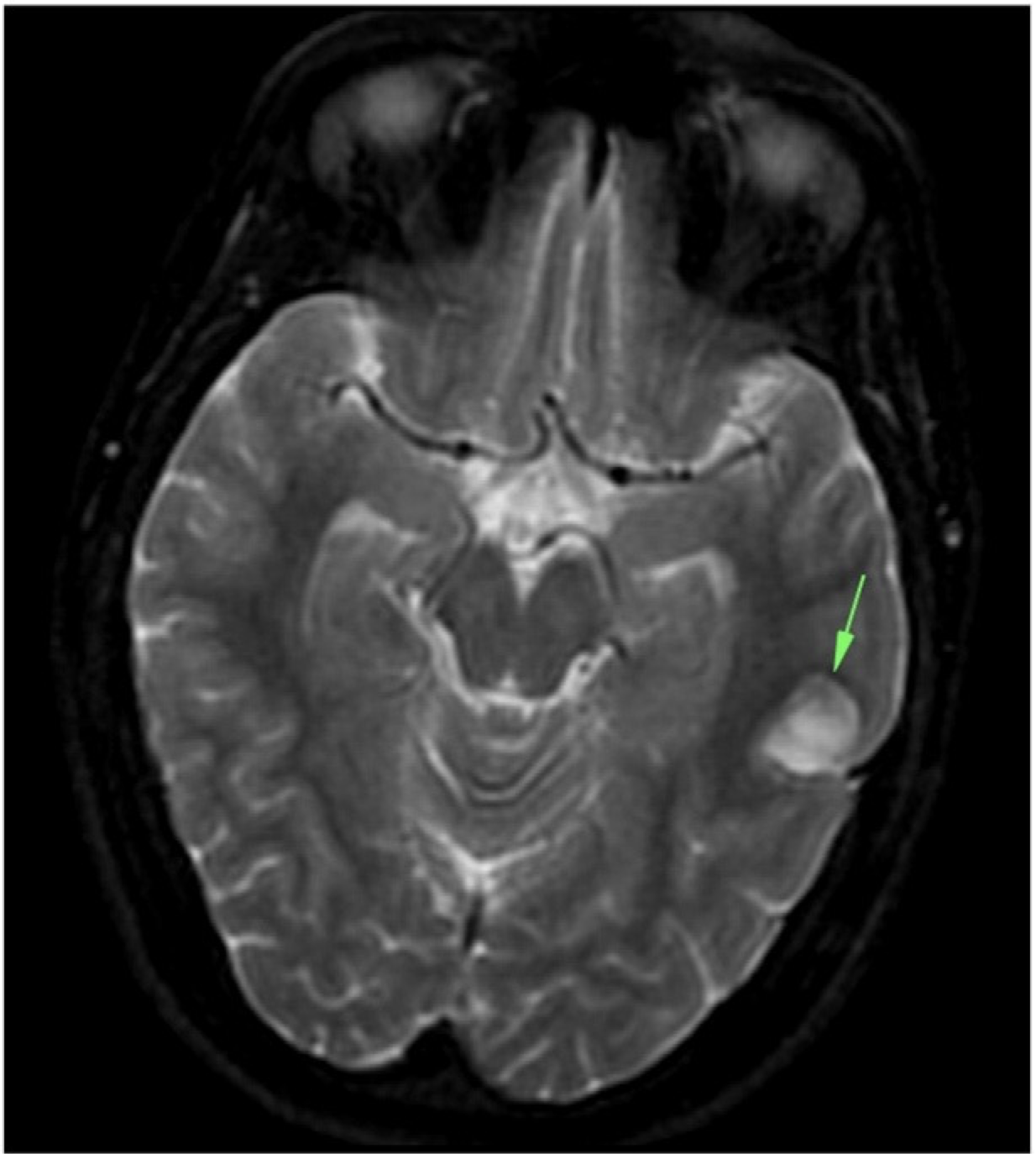
Tumour in the left temporal lobe - dysembryoplastic neuroepithelial tumour (DNET)- usually benign glial neural neoplasm
Surgically remove
Psychotic symptoms improved with the help of other treatments- risperidone + CBT
However, remained socially withdrawn
Case 3- bipolar effective disorder due to Wilsons disease
Middle aged female
Detained + admitted under section 2 of the Mental Health Act (MHA) 2007- decline in her mental state
Initially aggressive behaviour + required restrain by the Emergency Department security + police
Quietly spoken
voicing paranoid persecutory delusions
euthymic with labile affect
alternating between anger
tearfulness
displaying disinhibited affection
Doesn’t know why she was presented
CT

Hypodensity in the putamen, worse on the left
No mass, infarct or infectious process to explain the lesions
Consistent with the MRI from a couple of months ago which demonstrates hyperintensity of both putamina
Associated with Wilson’s disease
final diagnosis: psychosis secondary to neurological Wilson’s Disease
Case 4- Psychiatric syndromes associated with neurological disease
63-year-old male
paranoia
impaired anterograde memory + fatigue
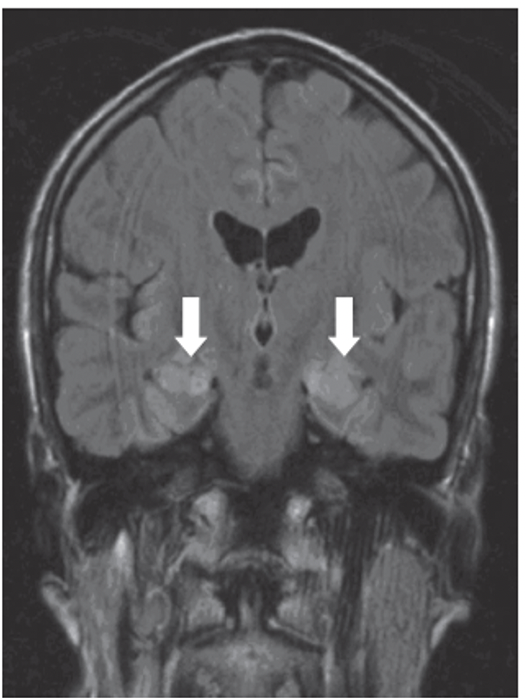
FLAIR scan shows bilateral hyperintensities in the hippocampus (arrows) → shows inflammatory process
Blood tests revealed anti-voltage gated potassium channel antibodies