Heart failure, strucuture, and MI complications lecture ❤️
1/126
There's no tags or description
Looks like no tags are added yet.
Name | Mastery | Learn | Test | Matching | Spaced |
|---|
No study sessions yet.
127 Terms
Atherosclerosis
abnormal accumulation of lipid deposits and fibrous tissue within arterial walls and lumen
Blockages and narrowing of the coronary vessels reduce blood flow to the
myocardium
high levels of hs-CRP are indicative of what
early indicator of CVD and athereosclerosis
clinical manifestations of myocardial ischemia
Angina pectoris (most common)
Other symptoms: epigastric distress, pain that radiates to jaw or left arm, SOB, atypical symptoms in women
Myocardial infarction
Heart failure
Cardiac arrest
what is angina pectoris
chest pain caused by insuffiecent coronary blood flow
stable angina pectoris
stable means there is some narrowing in vessels but patient can do what they need to do. pain on exertion. resting makes it go away
Unstable angina pectoris
unstable means you cant get pain to go away. usually means pre-infarct
variant angina pectoris (aka Prinzmetal’s)
coronary artery spasm as propsed to embolism.
What are the two main angina precipitating events
Decreased oxegyn supply (ex asthma, anemia, thrombosis) or increased demand (ex exercise, HTN, stress)
when assesing someone with anina what 4 things should you ask about
Discomfort?
Precipitation?
Relief?
Duration?
what does an elevated ST segment mean
heart attack
unstable angina characteristics
Non occlusive thrombus
Non specific ECG changes
Normal cardiac enzymes
NSTEMI characteristics
Non-occlusive thrombus sufficient to cause tissue damage & mild necrosis
ST depression/T wave inversion on ECG
Elevated cardiac enzymes
STEMI characteristics
Complete thrombus occlusion
ST elevations on ECG
Elevated cardiac enzymes
More severe symptoms
MI interventions include increasing supply and decreasing demand. How can you increase supply
applying oxygen,
vasodilations like nitroglycerin,
break up clot (TPA is clot buster. most with MI dont qualify for TPA bc there is a short window to give it (3-6 hrs) and most patients do not present to ED until later)
anticoagulant therapy is heparin because it prevents clot from getting bigger),
antiplatelet therapy (asprin, clavix), angioplasty/stenting
MI interventions include increasing supply and decreasing demand. How can you decrease demand
limit activity, beta blockers (decrease force of contraction. reduces strain on heart. lets heart rest), ACEi (decrease resistance), stool softeners
immediate treatment of a MI
MONA B!!!!
Morphine* not always nessesary. reseved for last if other interventions are not enough
Oxygen
Nitroglycerin*can be problematic if client has right sided MI
Aspirin
Heparin
Beta Blockers
Obtain EKG* delegate and get this done ASAP
*you do not have to go in that order
MI diagnostics
cardiac enzymes, EKG, cardiac stress test, cardiac cath
when do you draw cardiac enzyme labs
draw them three times to see if damage is worsening or improving
draw every 4-8 hrs
ST depression and/or T‑wave inversion indicates
presence of ischemia.
ST‑segment elevation indicates
injury
abnormal Q‑wave indicates
necrosis.
inferior infarct is problem in the
Right Coronary Artery
anterior and/or septal infarct is problem in the
Left Main or Left Anterior Descending artery
lateral infarct is problem in the
Left Main or Circumflex artery
severe ST elevations indicates
terrible tissue death
Core Measures: MI (as outlined by joint commision)
Aspirin at arrival
PCI accomplished within 90 minutes for STEMI patients**
PCI is same as angioplasty
ASA prescribed at discharge
ACE or ARB for LVSD
BB prescribed at discharge
Statin prescribed prior to discharge
if you cant fix obstruction with stents, you have to
bypass that obstruction with a vein bypass
are veins or arteries better for a vein bypass
veins more commonly used but we prefer artery. swap artery for an artery
veins easier to use.
veins cant withstand pressure of artery so it doesnt last as long
three things you always monitor for post op
infection, clotting, bleeding
it is really important for cardiac surgery post op paitents to
restrict activity and movement and monitor respirotry function
what is ectopy
ectopy are cranky cells. extra beats. beats that aren't right (PVC and PAC)
usually as a result of right MI
causes of PVC-
tissue damage, potassium, electrolyte disturbances,
bradycardia and heart blocks are
A “block” or delay in conduction from SA node to AV node
bradycardia physical assessment-
poor perfusion, cyanosis, dizziness syncope, tachypnea
bradycardia medications-
atropine, dopamine
bradycardia procedure-
pacemaker
Heart Block: Interventions
meds- atropine, epinipehrine
procedures- pacemaker
Atrial finbrilation phisiology
increased irritability in cells
atria not completely depolarized witheach impulse so the atria quiver, rather than contract forecfully
pulse deficit equation
Apical pulse – peripheral pulse
Manifestations of atrial dysrhythmias, such as atrial fibrillation, include
a sensation of palpitations (a racing, fluttering, or pounding heart), shortness of breath, dizziness or lightheadedness, and extreme fatigue
ventricular tachycardia pathophysilogy
SA node, other atrial pacemaker sites, AV junction all fail to initiate an electrical impulse 🡪 ventricles take over
Rate of 101 to 250 electrical impulses/minute
CAN BE LIFE THREATEING
Ventricular fibriliation pathophysilogy
Ventricles make ineffective quivering movements, not actual contractions.
Blood is not pumped throughout body.
Patient does not have a pulse.
CPR should begin immediately
Death will occur if treatment does not begin!
cardioversion and defibrillation are both used to
Treat tachydysrhythmias by delivering electrical current that depolarizes critical mass of myocardial cells
When cells repolarize, sinus node is usually able to recapture role as heart pacemaker
cardioversion is different from defibrillation because
In cardioversion, current delivery is synchronized with patient’s ECG
cardioversion is used when paitent has a pulse
defibrillation is different from cardioversion because
In defibrillation, current delivery is unsynchronized
used if paitent does not have a pulse
pacemakers are often used for clients with what condition
good for those with bradycardia bc it gives chambers impulse to contract
risks of pacemakers
cant do MRI’s with most
activity restrictions
uncontrollable hiccups is sign of pacemaker displacement
risks- infection, bleeding, displacement, pneumothorax
procedure can be risky bc surgeon can clip lung during insertion
if a client is in complete heart block what should you do first
- administer atropine
if you know they are in heart block EKG prolly already done. if you already know rhythm give atropine to increase HR
client with AFIB comes in. they are there for 48 hours and dysrythmia persists. what do you give first
- warfarin
heparin doesnt give as systemic of effects as warfarin. warfarin more widespread
heart failure definition
An inability of the heart to provide sufficient blood flow to meet the needs of the body for oxygenated blood
heart failure is characterized by
Volume overload
Dyspnea
Activity intolerance
what peptides are released early in heart failure?
Atrial Natrieurtic peptide (ANP)
secreted in response to atrial stretch
results in salt loss, diuresis, vasodilation, inhibits norepinephrine
Brain Natriuetric peptide (BNP)
gold standard
ventricular stretch
salt and water retention short term and long term effects
short- augments preload
long- pulmonary congestion, ansarca
vasoconstriction short term and long term effects
short- maintain BP for perfusion of vital organs
long- exacerbates pump dysfunction (excessive afterload), increases cardiac energy expendeture
sympathetic stimulation short term and long term effects
short -increase HR and ejection
long- increase energy expenditure
neurohormones (ANP and BNP) short term and long term effects
short- vasodilation, naturiesis, inhibition of RAAS
long- decreased BP, dehydration
a BNP above what level indicated there is HF
anything over 100
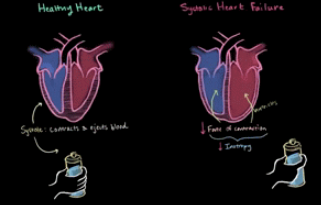
systolic dysfunction is
HF with reduced EF
Occurs when the left ventricle is unable to contract well against volume and unable to eject blood volume into the aorta
(impaired contractility and ejection)
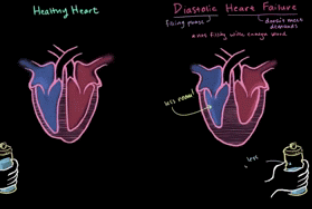
diastolic dysfunction is
HF with preserved EF
Inability of the left ventricle to accommodate blood volume during diastole at low to normal filling pressures.
(impaired filling and relaxtion)
normal ejection fraction
50-70%
clinical manifestations of LEFT ventricular dysfunction
dyspnea, orthopnea
fatigue
s3 gallop
pulomonary congestion (cough, crackles)
frothy sputnum (can be blood tinged)
altered mental status
manifestations of organ failure ex oliguria
clinical manifestations of RIGHT ventricular dysfunction
jugular vein distention
edema
abdominal distention, ascites
fatigue weakness
nausea and anorexia
polyuria/nocturia
liver enlargement and tenderness
weight gain
what medications improve symptoms of HF?
diuretics, digoxin, vasodilators, morphine
do diuretics treat systolic or diastolic HF?
both! diuretics appropriate for systolic and diastolic HF. used most often in systolic HF. acute exacerbation of diastolic HF can use diuretics, but dont tolerate as well. give diuretic if symptomatic in diastolic
is digoxin used to treat systolic or diastolic HF?
digoxin helps heart pump more effectively. best for systolic. positive inotrope to increase contractility.
do vasodiators treat systolic or diastolic HF?
vasodilators used in systolic dysfunction. decreases preload
is morphine used to treat systolic or diastolic HF?
used for both. slows heart and helps pain. improves respirtroy symptoms
what medications can help to increase survival rate in HF?
beta blockers, ACEi, spironolactone, ARBs, entresto(sacubitril/valsartan)
do beta blockers treat systolic or diastolic HF?
beta for diastolic HF. decrease contractility
do ACEi treat systolic or diastolic HF?
ACEi used for both.
everyone on ACEi at discharge. gold standard
is spironolactone used to treat systolic or diastolic HF?
both
what are some complications of HF?
hypertrophy
pleural effusion
thromboembolism
dysrrythmias
liver enlargment
kidney failure
electrolyte imbalances
cardiogenic shock
sytolic dysfunction occurs when
Occurs when the left ventricle is unable to contract well against volume and unable to eject blood volume into the aorta
diastolic dysfunction occurs when
Inability of the left ventricle to accommodate blood volume during diastole at low to normal filling pressures.
this can occur from the ventricles working too hard and the muscles becoming too large, making the chamber smaller and not able to fill as much
what is cardiomyopathy and what can it lead to
diseased heart muscles causing impaired CO
can lead to heart failure, sudden death, or dysrhythmias.
idiopathic cardiomyopathy
idiopathic= we dont know why it happened
Dilated Cardiomyopathy
Left Ventricle becomes dilated and “floppy”
Cannot contract well
common in ppl with MI
Hypertrophic Cardiomyopathy
Heart muscle thickening
Decreased size of ventricles
Decreased volume = decreased CO
Restrictive Cardiomyopathy
Least Common
Fibrosis/Scarring of heart tissue
Ventricular stiffness results in unable to relax and fill
Takotsubo Cardiomyopathy
Temporary weakening of left ventricle brought on by extreme stress
The ”broken heart” syndrome (can be seen after death of loved one or other periods of extreme stress)
Presents like MI with chest pain
has EKG and enzymes of MI but there is no blockage
reversible
treated by reducing stress on heart (ex beta blockers)
downsides of artifical hearts
bridge therapy (buys time, but not permanent for life). expensive and risky
what is an LVAD? what are the downsides
mechanically implant pump to pump for pt
bridge therapy. buys us time but not meant to last forever . does not solve problem
heart transplantation pros,cons, and important considerations
best solution for failing heart
low supply of hearts
key considerations
anti rejection medications and regiment must be adhered to
no nerve connection in transplanted heart
poor innervation to heart means they cant feel pain in heart if MI occurs. look for symptoms besides pain
vagus nerve severed so meds that work on vagus nerve (ex atropine) dont work
heart transplant maybe last 10-20 years
s1 heart sounds are caused by
mitral & tricuspid valves closing
s2 heart sounds are caused by
aortic & pulmonic vlaves closing
heart sounds are the sound of
valves closing
when someone has stenosis you will hear
clicking or extra sound
when someone has regurgitation you will hear
whooshing
regurgitation
The valve does not close properly, and blood backflows through the valve
stenosis
The valve does not open completely, and blood flow through the valve is reduced
valve prolapse
The stretching of an atrioventricular valve leaflet into the atrium during diastole
pretty similar to regurgitation
should aortic and pulmonic valves be open or closed during systole? what does it mean if they are not?
OPEN in systole. if hard to do=stenosis
should mitral and tricuspid valves be open or closed during systole? what does it mean if they are not?
CLOSED. if they dont=regurgitation
should aortic and pulmonic valves be open or closed during diastole? what does it mean if they are not?
CLOSED. if they arent = regurgitiation
should mitral and tricuspid valves be open or closed during diastole? what does it mean if they are not?
OPEN. if this is hard to do= stenosis
mitral valve prolapse. what causes it? what are symptoms? what type of murmur is this?
Leaflet(s) buckle back into the left atrium during ventricular systole
systolic murmur often asymptomatic
can be inherited or from endocarditis
mitral regurgitation. what causes it? what type of murmur? what are symptoms?
can be from MI, ruptured papillary muscles or endocarditis
Valve allows blood to return to left atrium from the left ventricle during systole
systolic murmur
risk for clots
mitral stenosis. what causes it? what type of murmur is it? what are symptoms
Obstruction of flow from left atrium to left ventricle
caused by endocarditis
SOB, DOE, pulmonary congestion
diastolic murmur
aortic stenosis. what causes it? what type of murmur? what are symptoms?
caused by malformations, age, or endocarditis
systolic murmur
can cause left ventricle muscle to thicken bc it has to work harder