X : Serological & Molecular Detection of Bacterial Infections
1/144
Earn XP
Description and Tags
Name | Mastery | Learn | Test | Matching | Spaced | Call with Kai |
|---|
No analytics yet
Send a link to your students to track their progress
145 Terms
d. release of lipid A from the bacterial cell.
All of the following are protective mechanisms against bacteria except
a. production of antimicrobial defense peptides.
b. phagocytosis.
c. activation of complement.
d. release of lipid A from the bacterial cell.
c. antibodies to one serotype protect against other serotypes.
All of the following are characteristics of streptococcal M proteins except
a. it is the chief virulence factor of Group A streptococci.
b. it provokes an immune response.
c. antibodies to one serotype protect against other serotypes.
d. it limits phagocytosis of the organism.
b. The patient has an antibody to a streptococcal exoenzyme other than streptolysin O.
An ASO titer and a streptozyme test are performed on a patient's serum. The ASO titer is negative, the streptozyme test is positive, and both the positive and negative controls react appropriately. What can you conclude from these test results?
a. The ASO is falsely negative.
b. The patient has an antibody to a streptococcal exoenzyme other than streptolysin O.
c. The patient has not had a previous streptococcal
infection.
d. The patient has scarlet fever.
b. Antibodies to Group A streptococci are believed to cross-react with heart tissue.
Which of the following applies to acute rheumatic fever?
a. Symptoms begin after S. pyogenes infection of the throat or the skin.
b. Antibodies to Group A streptococci are believed to cross-react with heart tissue.
c. Diagnosis is usually made by culture of the organism.
d. All patients suffer permanent disability.
a. Reduction of methyl green from green to colorless
Which of the following indicates the presence of anti- DNase B activity in serum?
a. Reduction of methyl green from green to colorless
b. Clot formation when acetic acid is added
c. Inhibition of red blood cell hemolysis
d. Lack of change in the color indicator
a. Acute rheumatic fever
Which of the following is considered to be a nonsuppurative complication of streptococcal infection?
a. Acute rheumatic fever
b. Scarlet fever
c. Impetigo
d. Pharyngitis
b. stimulation of chemotaxis.
All of the following are ways that bacteria can evade host defenses except
a. presence of a capsule.
b. stimulation of chemotaxis.
c. production of toxins.
d. lack of adhesion to phagocytic cells.
d. Antibody production takes at least a week before detection.
Antibody testing for Rocky Mountain spotted fever may not be helpful for which reason?
a. It is not specific.
b. It is too complicated to perform.
c. It is difficult to obtain a blood specimen.
d. Antibody production takes at least a week before detection.
c. Urease
Which of the following enzymes is used to detect the
presence of H pylori infections?
a. DNase
b. Hyaluronidase
c. Urease
d. Peptidase
c. Antibodies remain after initial treatment.
Which of the following reasons make serological identification of a current infection with Helicobacter pylori difficult?
a. No antibodies appear in the blood.
b. Only IgM is produced.
c. Antibodies remain after initial treatment.
d. No ELISA tests have been developed.
a. Cold agglutinins
M pneumoniae infections are associated with the production of which antibodies?
a. Cold agglutinins
b. Antibodies to ATPase
c. Antibodies to DNase
d. Antibodies to Proteus bacteria
b. Specific antibodies in the serum sample attach to the antigens fixed to a microscope slide. In a second step, the attached antibodies are stained with fluorescein-labeled anti-human immunoglobulin and visualized with the fluorescence microscope.
Which of the following best describes the principle of the IFA test for detection of antibodies produced in Rocky Mountain spotted fever?
a. Patient serum is applied to a microtiter plate coated with a monoclonal antibody directed against the target antigen. A detection antibody labeled with biotin and directed against the target antigen is added. After addition of a substrate, a color reaction develops indicating presence of the antigen.
b. Specific antibodies in the serum sample attach to the antigens fixed to a microscope slide. In a second step, the attached antibodies are stained with fluorescein-labeled anti-human immunoglobulin and visualized with the fluorescence microscope.
c. The serum sample is treated chemically to link the target antibodies to a fluorophore. The labeled sample is applied to a microscope slide to which the antigen has been attached. Following a wash step, the slide is examined for fluorescence.
d. Patient serum is applied to a slide to which a specific antigen is bound. Following a wash step, a chromogenic dye is applied that binds to the Fc region of IgG and IgM antibodies. After a second wash step, the slide is examined for fluorescence.
c. Endotoxin is released from the cell wall of dead bacteria, whereas exotoxin is released from live bacteria.
Which of the following is true regarding exotoxins and endotoxins?
a. Both endotoxin and exotoxins are highly immunogenic allowing for the development of protective antibodies and vaccines.
b. Endotoxin has targeted activity whereas exotoxins have systemic effects when released.
c. Endotoxin is released from the cell wall of dead bacteria, whereas exotoxin is released from live bacteria.
d. Both endotoxin and exotoxins bind to specific receptors on a bacterial cell leading to cell lysis.
c. It is an important mechanism for protecting a bacterium against ingestion by PMNs.
Characteristics of a bacterial capsule include which of the following?
a. It cannot be used for vaccine development.
b. It is composed of peptidoglycan.
c. It is an important mechanism for protecting a bacterium against ingestion by PMNs.
d. It is what causes bacteria to stain as gram-negative.
b. It is the cause of most cases of acute food poisoning in the United States.
Which of the following statements regarding Helicobacter pylori is not true?
a. It is associated with an increased risk of gastric carcinoma.
b. It is the cause of most cases of acute food poisoning in the United States.
c. It is a major cause of peptic ulcers in the United States.
d. It is positive for urease.
Symbiotic
- Host & microbes live together long term.
Symbiotic
- Indigenous microbiota.
Mutualistic
- Both host & microbe’s benefit.
Parasitic
- Microbes cause harm to the host.
Infectivity
- Organism’s ability to establish an infection.
Pathogenicity
- Ability of an organism to cause dx.
Virulence
Extent of pathology caused by an organism when it infects a host
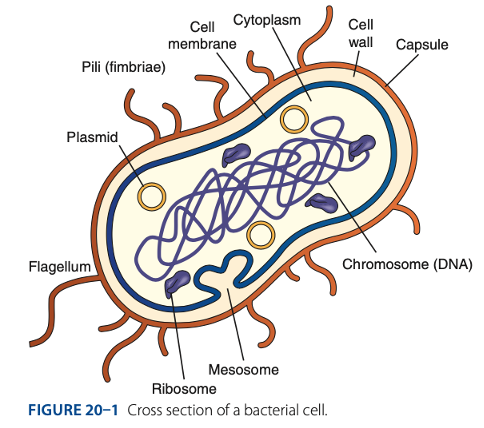
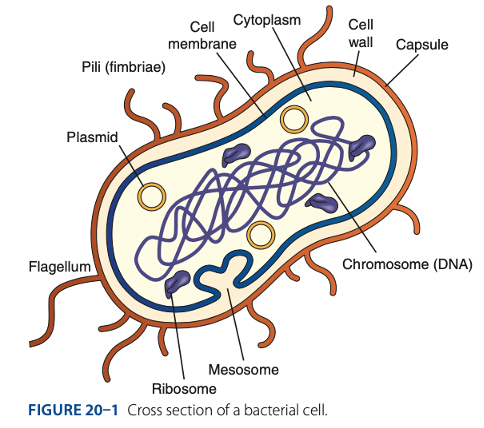
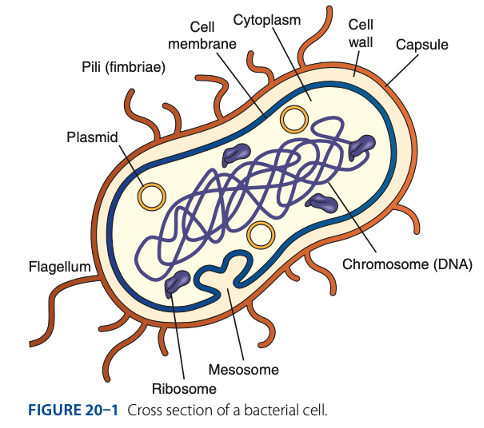
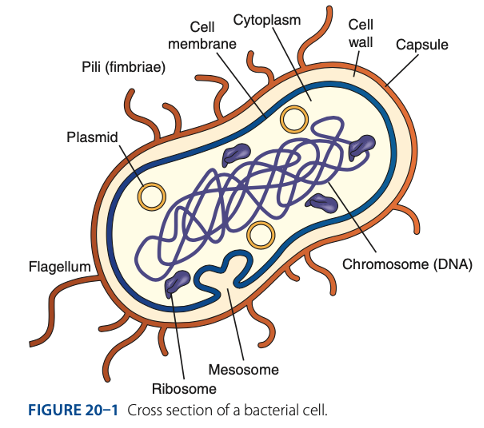
Endotoxin
Pili
Flagella
Capsule
Exotoxins
Bacterial Virulence Factors
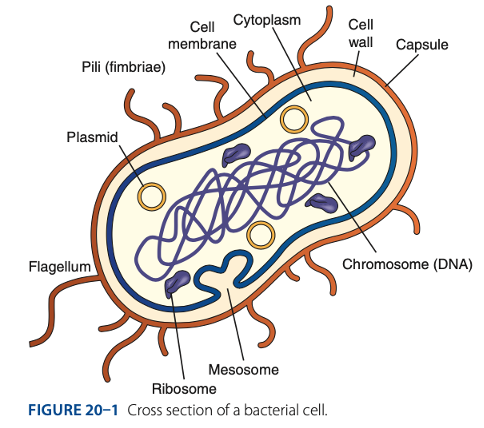
Endotoxin
- The lipid A portion of LPS in gram – cell walls
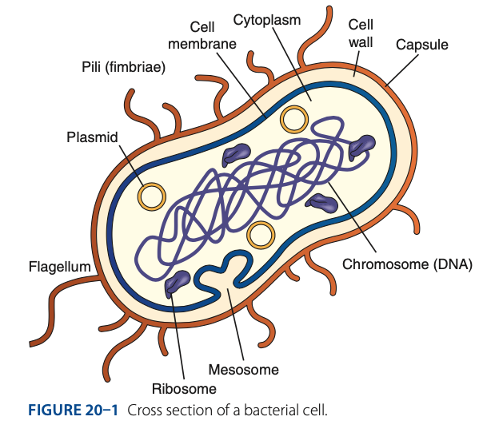
Endotoxin
- Powerful stimulator of cytokine release
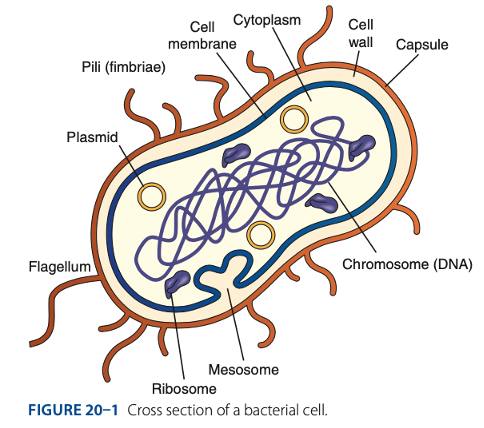
Pili
- Adherence to host cells
- Resistance to phagocytosis
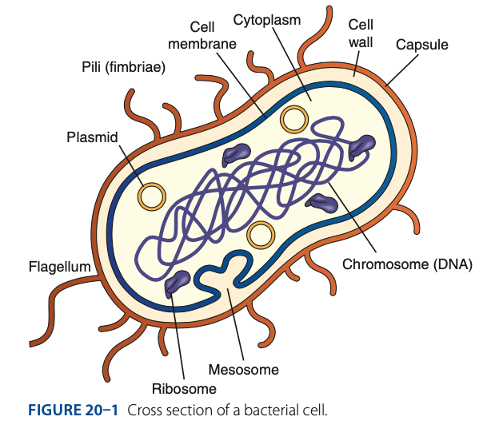
Pili
- Conjugation – process of Horizontal gene transfer
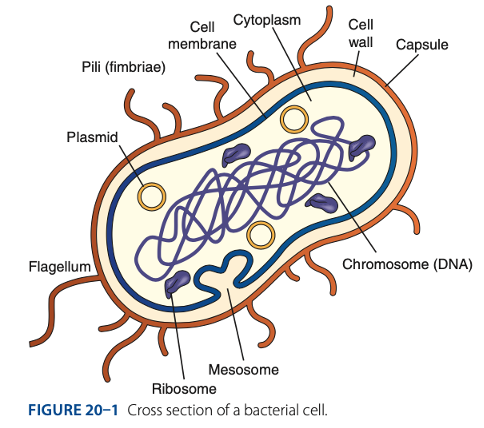
Flagella
- Adherence to host cells
- Motility
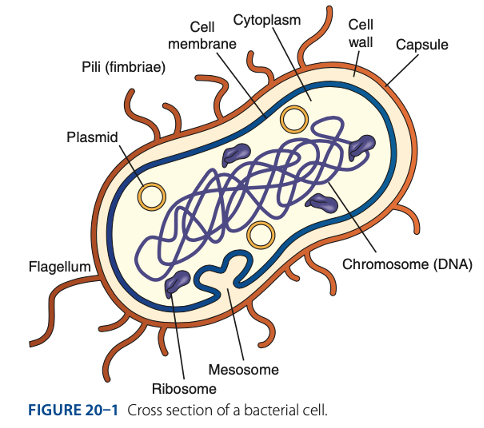
Capsule
Blocks phagocytosis
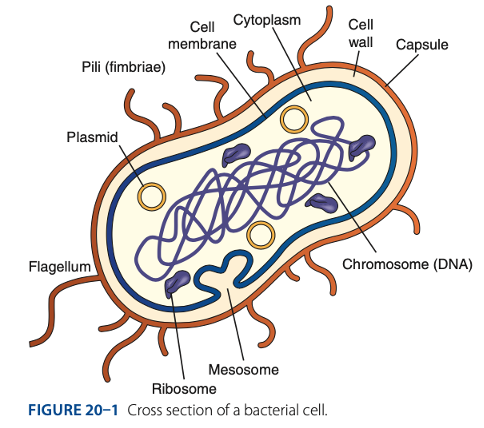
Capsule
antibody attachment
Exotoxins
- Potent toxic proteins released from living bacteria
Exotoxins
- Neurotoxins, cytotoxins, enterotoxins
Exotoxins
- G –& +
Innate Defenses
Immune Defenses Against Bacteria
Identify if Innate or Adaptive Defense:
• Intact skin & mucosal surfaces (barriers to entry)
Innate Defenses
Immune Defenses Against Bacteria
Identify if Innate or Adaptive Defense:
• Complement proteins, cytokines, acute-phase reactants
Innate Defenses
Immune Defenses Against Bacteria
Identify if Innate or Adaptive Defense:
• Recognition of PAMPs by PRRs such as TLRs
Adaptive Defenses
Immune Defenses Against Bacteria
Identify if Innate or Adaptive Defense:
• Antibody Production
Binding of Complement components, opsonization, neutralization of bacteria toxins
Adaptive Defenses
Immune Defenses Against Bacteria
Identify if Innate or Adaptive Defense:
• Cell-mediated immunity
CD4 T cells produce cytokines that induce inflammation; cytotoxic T lymphocytes attack host cells that contain intracellular bacteria.
Culture of the Causative Agent
Laboratory Detection of Bacterial Infections
• Growth on broth / solid media.
Culture of the Causative Agent
Laboratory Detection of Bacterial Infections
• Major means of diagnosis, but may take time or may not be possible.
Microscopic Examination
Laboratory Detection of Bacterial Infections
Gram / special stains
Detection of Bacterial Antigens
Laboratory Detection of Bacterial Infections
Rapid testing by ELISA, LFA, or LA.
Molecular Detection of Bacterial DNA / RNA
Laboratory Detection of Bacterial Infections
Can obtain results in a few hours with PCR.
Serology
Laboratory Detection of Bacterial Infections
Detects antibodies to bacterial antigens
Culture of the Causative Agent
Microscopic Examination
Detection of Bacterial Antigens
Molecular Detection of Bacterial DNA / RNA
Serology
Laboratory Detection of Bacterial Infections
T
Uses of Laboratory Detection of Bacterial Infections
• To detect & confirm infections for which other laboratory methods are not available.
(t/f)
F
• To diagnose infections for which clinical symptoms are nonspecific.
Uses of Laboratory Detection of Bacterial Infections
• To diagnose infections for which clinical symptoms are specific. (t/f)
F
• Current infection indicated by presence of IgM, a high IgG titer, or a fourfold rise in antibody titer between acute & convalescent samples
Uses of Laboratory Detection of Bacterial Infections
• Current infection indicated by presence of IgM, a low IgG titer, or a twofold rise in antibody titer between acute & convalescent samples (t/f)
T
Uses of Laboratory Detection of Bacterial Infections
• To determine a past exposure to & organism (IgM-. IgG+) (t/f)
T
Uses of Laboratory Detection of Bacterial Infections
• To assess reactivation of re-exposure. (t/f)
• Delay between start of infection & production of antibodies.
• Low antibody production by immunosuppressed patients.
Disadvantages of Laboratory Detection of Bacterial Infections

Group A Streptococci
- Gram + cocci arranged in pairs / chains.

Person-to-person transmission.
Group A Streptococci MOT
• Pharyngitis / Strep Throat
• Pyoderma / Impetigo
• Scarlet Fever
• Toxic Shock Syndrome (TSS)
• Necrotizing Fasciitis
• Treated with Antibiotics
• Enanthem – rashes in mucosal
• Exanthem – rashes in the skin
Clinical Manifestations of Acute Group A Streptococcal Infection
Pharyngitis / Strep Throat
– most common clinical manifestations of Group A Streptococcal infection. Symptoms include fever, chills, severe sore throat, headache, tonsillar exudates, petechial rash on the soft palate, & anterior cervical lymphadenopathy.
Pyoderma / Impetigo
– most common clinical manifestations. It is characterized by vesicular lesions on the extremities that become pustular & crusted which tend to occur in young children.
Enanthem
rashes in mucosal
Exanthem
rashes in the skin
Acute Rheumatic Fever / Arthritis
- Develops a sequelae 1–3 weeks after pharyngitis/tonsillitis in 2% – 3% of infected individuals.
Acute Rheumatic Fever / Arthritis
- Most likely caused by immune responses to streptococcal antigens that cross-react with human heart tissue.
• Fever
• Joint pain
• Inflammation of the heart
JIF
- Symptoms of Acute Rheumatic Fever / Arthritis
Poststreptococcal Glomerulonephritis
- May follow strep infection of the skin or pharynx
Poststreptococcal Glomerulonephritis
- Damages glomeruli in the kidney, producing hematuria, proteinuria, edema, hypertension, malaise, backache, abdominal discomfort, & impairment in renal function.
Poststreptococcal Glomerulonephritis
- Deposits of immune complexes containing streptococcal antigens in glomeruli.
• Culture on Sheep Blood Agar (SBA) – Small translucent colonies surrounded by clear zone of β hemolysis.
• Rapid assays to detect group A streptococcal antigens
Lateral Flow Immunochromatographic Assays(LFA)
Laboratory Diagnosis of Acute Group A Streptococcal Infections

Small translucent colonies surrounded by clear zone of β hemolysis.
Laboratory Diagnosis of Acute Group A Streptococcal Infections
Culture on Sheep Blood Agar (SBA) shows
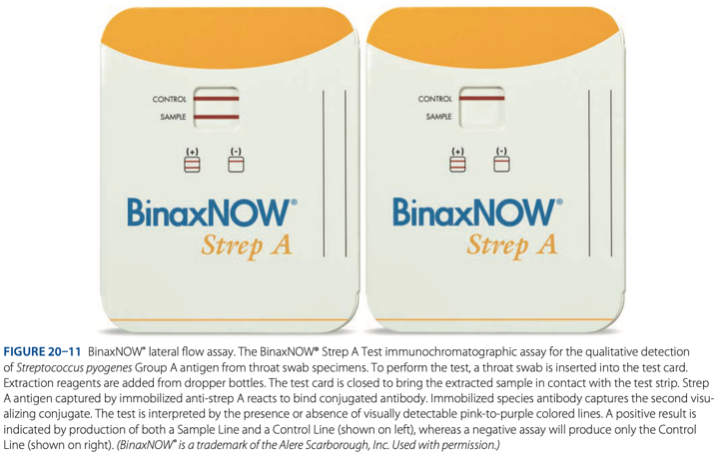
Lateral Flow Immunochromatographic Assays(LFA)
Laboratory Diagnosis of Acute Group A Streptococcal Infections
• Rapid assays to detect group A streptococcal antigens such as
Antistreptolysin O (ASO)
Serological Detection of Group A Streptococcal Sequelae
- Nephelometric methods currently used that measure light scatter produced by immune complexes containing streptolysin antigen.
T
Serological Detection of Group A Streptococcal Sequelae (t/f)
Antistreptolysin O (ASO)
Titer elevated in 85% of patients with acute rheumatic fever
Antistreptolysin O (ASO)
Serological Detection of Group A Streptococcal Sequelae
- Does not increase in patients with skin infection.
Anti-DNase B
Serological Detection of Group A Streptococcal Sequelae
- Produced by both rheumatic fever & impetigo px.
EIA & nephelometric methods.
Serological Detection of Group A Streptococcal Sequelae
Anti-DNase B is tested by
Streptozyme Test
Serological Detection of Group A Streptococcal Sequelae
- Is a slide agglutination screening test for the detection of antibodies against streptococcal antigens.
• Antistreptolysin O (ASO)
• Anti-hyaluronidase (AHase)
Hyaluronidase
• Anti-streptokinase (ASKase)
• Anti-nicotinamide adenine dinucleotide (anti-NAD)
• Anti-DNase B – enzyme that degrades DNA
Serological Detection of Group A Streptococcal Sequelae
Streptozyme Test detect antibodies to 5 streptococcal products:
Antistreptolysin O (ASO)
Serological Detection of Group A Streptococcal Sequelae
– detect antibodies to the streptolysin O enzyme produced by Group A streptococcus.
Hyaluronidase
Serological Detection of Group A Streptococcal Sequelae
enzyme produced by gas that breaks hyaluronic acid
Anti-streptokinase (ASKase)
Serological Detection of Group A Streptococcal Sequelae
can dissolve blood clots
Anti-nicotinamide adenine dinucleotide (anti-NAD)
Serological Detection of Group A Streptococcal Sequelae
– break down
Anti-DNase B
Serological Detection of Group A Streptococcal Sequelae
enzyme that degrades DNA
F
Gram – microaerophilic spiral bacterium
Helicobacter pylori is a gram + microaerophilic rods bacterium (t/f)
fecal-oral route
Helicobacter pylori is transmitted by
gastric & duodenal ulcers
Helicobacter pylori’s major cause is
urease
Helicobacter pylori can survive in acid environment of stomach because of production of -, which provides a buffering zone around the bacteria.
Urease
provides a buffering zone around the bacteria.
antibiotics & anti-ulcer medications
Treatment of Helicobacter pylori
gastric carcinoma or mucosa-associated lymphoid tumors
If Helicobacter pylori is left untreated, it can lead to
• Detect urease in stomach biopsy (CLOtest)
• Urea Breath Test
• H pylori antigen
• H pylori Antibodies
ELISA is method of choice.
IgG in serum indicates an active infection.
Titers decrease AFTER successful treatment.
Detection of Helicobacter pylori Infection
T
Helicobacter pylori (t/f)
Titers decrease AFTER successful treatment
ELISA
method of choice for the detection of Helicobacter pylori Infection
IgG
what indicates in a serum an active infection
- Tiny bacteria that lack a cell wall
Mycoplasma pneumonia
- Leading cause of respiratory infections
Stevens-Johnson syndrome
Mycoplasma pneumonia causes what dx in minority of cases which is a condition in which the top layer of the skin dies & sheds
Fever, headache, malaise, & cough
Symptoms of Mycoplasma pneumonia
“Walking pneumonia”
Mycoplasma pneumonia is commonly known as
Raynaud Syndrome
transient vasospasm of the digits in which the fingers turn white when exposed to the cold.
Culture
Antibodies to M. pnuemoniae
Cold Agglutinins
Molecular Methods
Laboratory Diagnosis of M. pnuemoniae Infection
- Produces mulberry colonies with a “fried egg” appearance on specialized media
Culture of M. pnuemoniae Infection produces what colonies and appearance on specialized media
Culture
- Is gold standard for detection of M. pnuemoniae but rarely performed in clinical laboratories because organism is difficult to grow.
Antibodies to M. pnuemoniae
Most useful diagnostic assay of M. pnuemoniae